Abstract
Background
Viral suppression and viral breakthrough impact the humoral immune response to HIV infection. We evaluated the impact of viral suppression and viral breakthrough on results obtained with two cross-sectional HIV incidence assays.
Methods
All samples were collected from adults in the US who were HIV infected for >2 years. Samples were tested with the BED capture enzyme immunoassay (BED-CEIA) which measures the proportion of IgG that is HIV-specific, and with an antibody avidity assay based on the Genetic Systems 1/2+ O ELISA. We tested 281 samples: (1) 30 samples from 18 patients with natural control of HIV-1 infection known as elite controllers or suppressors (2) 72 samples from 18 adults on antiretroviral therapy (ART), with 1 sample before and 2–6 samples after ART initiation, and (3) 179 samples from 20 virally-suppressed adults who had evidence of viral breakthrough receiving ART (>400 copies/ml HIV RNA) and with subsequent viral suppression.
Results
For elite suppressors, 10/18 had BED-CEIA values <0.8 normalized optical density units (OD-n) and these values did not change significantly over time. For patients receiving ART, 14/18 had BED-CEIA values that decreased over time, with a median decrease of 0.42 OD-n (range 0.10 to 0.63)/time point receiving ART. Three patterns of BED-CEIA values were observed during viral breakthrough: (1) values that increased then returned to pre-breakthrough values when viral suppression was re-established, (2) values that increased after viral breakthrough, and (3) values that did not change with viral breakthrough.
Conclusions
Viral suppression and viral breakthrough were associated with changes in BED-CEIA values, reflecting changes in the proportion of HIV-specific IgG. These changes can result in misclassification of patients with long-term HIV infection as recently infected using the BED-CEIA, thereby influencing a falsely high value for cross-sectional incidence estimates.
Introduction
HIV incidence estimates are used to monitor the current state of the epidemic and determine the impact of prevention efforts and treatment policy. Longitudinal cohorts can be used to determine HIV incidence [1]; yet, longitudinal cohort studies are expensive and suffer from selection and follow-up biases [2], [3]. Cross-sectional surveys have been used to identify recently-infected patients and estimate population incidence [3]. However, most laboratory methods used for cross-sectional HIV incidence determination misclassify some patients with long-term infection as recently infected, causing inaccurate incidence estimates [4]. One key factor associated with misclassification by cross-sectional incidence assays is viral suppression, both natural and antiretroviral (ARV) drug induced [5]. Self-report of ARV treatment (ART) has been used to exclude patients from being considered recently infected; however, self-report of ART is inaccurate [6]. Some patients who are receiving ART report that they are not on treatment.[7] Other patients receiving ART are not virally suppressed, due to viral resistance or lack of adherence [6]. Furthermore, detection of ARVs in blood can be difficult because of the short half-life of some ARV drugs [6], [8]. In addition, viral breakthrough is another important component that could be affecting cross-section incidence estimates. Viral breakthrough is defined as the reemergence of virus, while receiving ART, to >1000 copies/mL [9]. A summary on these and other issues associated with cross sectional incidence testing can be found in recent reviews.[10], [11], [12] We evaluated the impact of viral suppression and viral breakthrough on results obtained from cross-sectional incidence testing assays.
In this report, we evaluated the impact of viral suppression on the anti-HIV antibody response, measured using two different cross-sectional incidence assays: (1) the proportion of IgG that is HIV specific (measured using the BED capture immunoassay [13] (BED-CEIA), and (2) antibody avidity (measured using a modified enzyme immunoassay). The avidity immunoassay measures the strength of the HIV antibody response [14]. It has been recorded that the avidity response directly correlates with the amount of time an patient has been infected [14]. We evaluated these effects in patients with both natural and ARV-induced viral suppression. We also evaluated the effect of duration of viral suppression and the impact of viral breakthrough on these immune responses.
Methods
Samples were collected from adults with likely HIV-1 subtype B infection, from the Johns Hopkins HIV Clinical Practice Cohort [15] in Baltimore Maryland, who were infected for at least two years. A study of HIV infected subjects determined that >98% of patients from inner city Baltimore were infected with HIV-1 subtype B virus [16]. All subjects from the elite suppressor cohort at Johns Hopkins University are infected with HIV-1 subtype B virus [17], [18], [19]. This included: (1) 18 patients who were identified as elite suppressors [17] (30 samples); (2) 18 patients receiving ART with one sample before and 2–6 samples (one/year) after ART initiation (72 samples); and (3) 20 virally-suppressed patients who had evidence of viral breakthrough while receiving ART (>400 copies/ml) with subsequent viral suppression (179 samples). All participants provided written informed consent and the study was approved by the Institutional Review Board of the Johns Hopkins University.
The BED-CEIA [20] was performed according to the manufacturer's instructions (Sedia Biosciences Corporation, Portland, OR); with the exception that all samples were run in duplicate. The average normalized optical density (OD-n) was used for the analysis. Since all of patients had documented HIV infection for a minimum of two years, any sample with an OD-n ≤0.8 was considered misclassified. The avidity assay was based on the Genetic Systems HIV-1/HIV-2 EIA +O (enzyme linked immunoassay, BioRad Laboratories, Redmond, WA)[21]. In short, samples were diluted 1:10 in duplicate, and were incubated at 4°C for 30 minutes (initial antibody-binding step). Samples were then incubated for 30 minutes at 37°C with or without the chaotropic agent, diethylamine (antibody disassociation step). For each sample, the avidity index was calculated as: [optical density of the diethylamine-treated well]/[optical density of the non-treated well] ×100. For both the BED-CEIA and avidity assays, all samples from a given patient were run on the same plate to minimize the effect of plate-to-plate variation.
Results
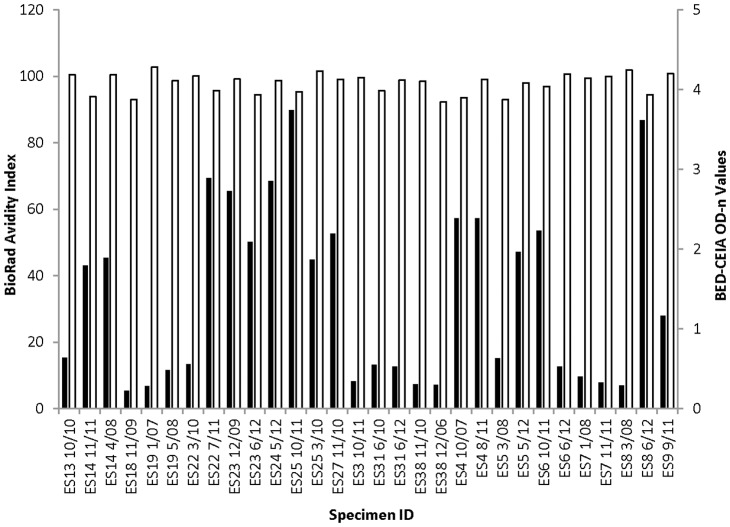
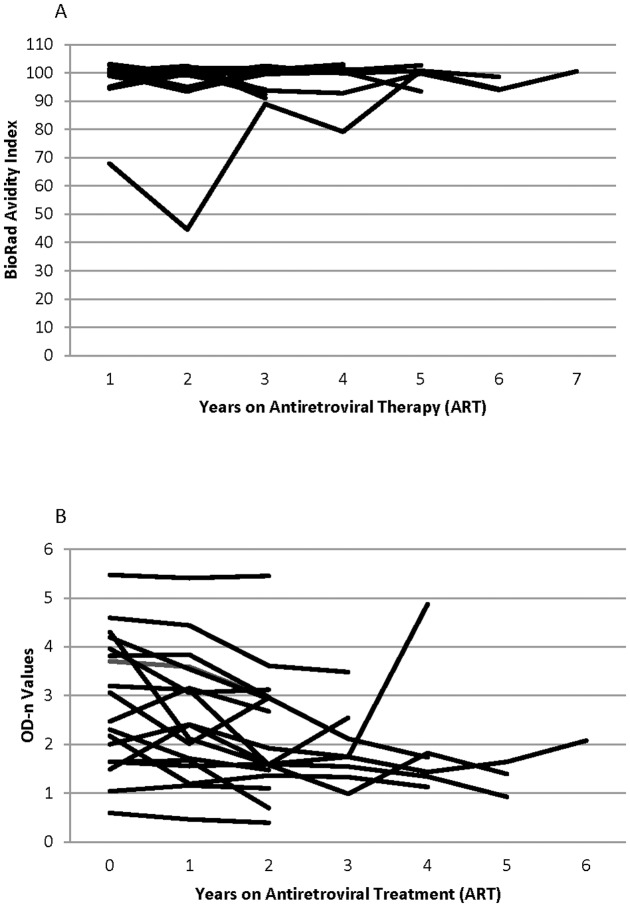
For the elite suppressors, the avidity index ranged from 92% to 101% and was well above the threshold of 40% for recent infection [21] (Figure 1). The avidity index was also not affected by longer duration of ART or viral breakthrough (Figure 2B). Of the all 38 patients receiving ART, 26 consistently had avidity index values above 80% for all time points tested. One subject had an avidity index of 70% prior to ART initiation that decreased during the first year of treatment and then increased to and remained above 80% at two years receiving ART (Figure 2B). The second subject had an avidity index of 35% at the first time point (consistent with recent HIV infection) that slowly climbed to above 80% by the last time that the last sample was collected (after 9 years receiving ART). Viral suppression had no detectable impact on antibody avidity.
Figure 1. Elite suppressor BioRad avidity index and BED-CEIA OD-n values.
Results from 30 samples from 18 elite suppressors (patients who had viral load <50 copies/mL without antiretroviral therapy). The month and year of sample are listed. Black bars denote BED-CEIA OD-n values and white bars denote BioRad avidity index.
Figure 2. The effect of time after ART-induced viral suppression on antibody avidity and BED-CEIA results.
(A) BioRad avidity index values of 18 patients (72 samples) receiving ART with one sample before and 2–6 samples after ART initiation. (B) BED-CEIA normalized optical density (OD-n) values of 18 patients (72 samples) receiving ART, with one sample before and 2–6 samples after documented viral suppression.
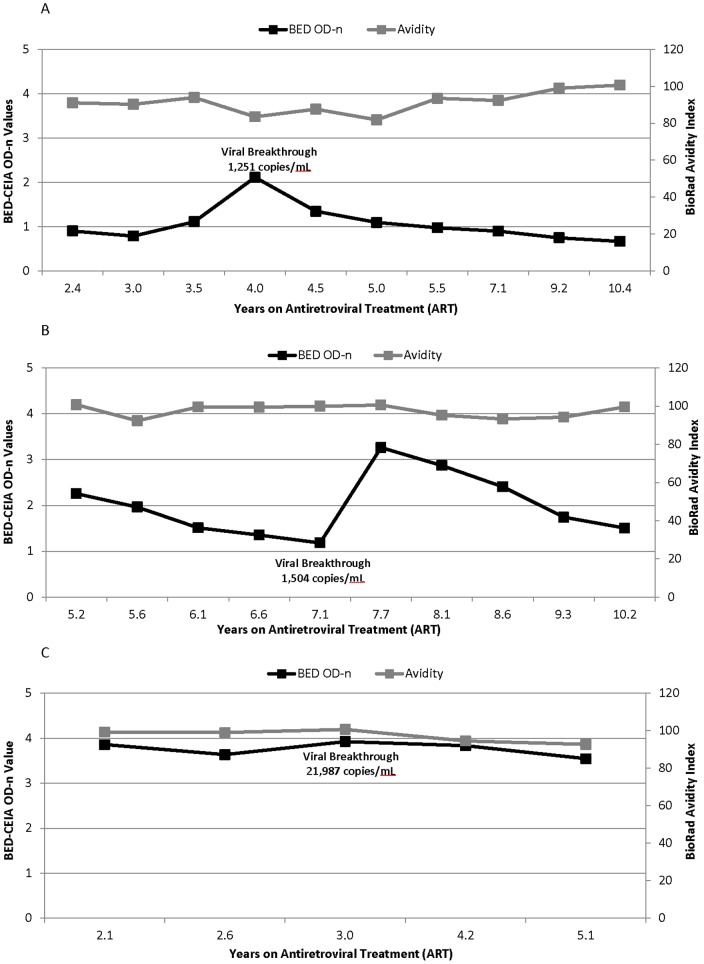
In contrast, viral suppression had a significant impact on results obtained with the BED-CEIA; this was observed for patients with both natural and ARV-induced viral suppression. Ten of 18 elite suppressors had BED-CEIA values ≤0.8 OD-n (Figure 1). After ART initiation, BED-CEIA values decreased in 14 of 18 patients, with a median decrease of 0.42 OD-n per year of treatment (range 0.10 to 0.63) (Figure 2A). In those with viral breakthrough, three patterns of BED-CEIA values were observed. In 9 of 20 patients, values increased at the time of viral breakthrough by a median of 0.52 OD-n, and returned to pre-breakthrough values when viral suppression was re-established (Figure 3A). In 8 of 20 patients, values increased at the visit after viral breakthrough (mean 322 days after breakthrough, range 0.8–2.8), with a median increase of 0.81 OD-n (Figure 3B). In the remaining three subjects, there was no change in BED-CEIA values with viral breakthrough (Figure 3C).
Figure 3. The effect viral breakthrough on BED-CEIA and avidity results.
20 virally-suppressed patients (179 samples) who had evidence of viral breakthrough while receiving ART (>400 copies/ml) with subsequent viral suppression. (A) Individual example of BED-CEIA OD-n values increase with viral breakthrough. Apart for time point listed, all other time points had viral loads <400 copies/ml. (B) Example of the increase in BED-CEIA OD-n values after viral breakthrough time point; results from one patient. Apart for time point listed, all other time points had viral loads <400 copies/ml. (C) Example of BED-CEIA OD-n values that showed no change with viral breakthrough. Apart for time point listed, all other time points have viral loads <400 copies/ml.
Discussion
In our study, we found that viral suppression impacts results obtained with the BED-CEIA, but does not impact results obtained with an antibody avidity assay. BED-CEIA values varied in patients experiencing viral suppression and viral breakthrough. Elite suppressors had naturally low BED-CEIA values; 10 of 18 elite suppressors were misclassified as recently-infected using this assay. ART use was also associated with decreasing OD-n values. The observed effect compromises use of the BED-CEIA for accurately assessing HIV incidence. As the number of HIV-infected patients accessing ART increases world-wide, and patients receiving ART survive longer, the frequency of long-term infected patients who are misclassified as recently infected by the BED-CEIA would be expected to increase over time.
The finding that ART-induced viral suppression is associated with BED-CEIA misclassification has been reported previously [4], [20], [22]. Our study defines a rate of decrease in BED-CEIA OD-n values after ART initiation, and demonstrates that BED-CEIA results do not change in some patients even after prolonged ART. We observe that the BED-CEIA values increase in the majority of patients with viral breakthrough, and that there is a temporal relationship between the increase of the BED-CEIA value and the increase in viral load. These findings support the use of viral load testing as a marker of ART use in combination with additional assay, including the BED-CEIA for analysis of cross-sectional incidence [5], [23], [24], [25].
Similar to results observed with the Vironostika-Less Sensitive enzyme immunoassay (Vir-LS), the BED-CEIA misclassifies a majority of samples from elite suppressors [22]. This finding supports previous results suggesting that the BED-CEIA and the Vironostika-Less Sensitive enzyme immunoassay (Vir-LS) were highly correlated in the context of other phases of infection, not just in elite controllers [26]. Additionally, results from 180 HAART-suppressed patients reveal a steady decrease in Vir-LS values for the twelve months after viremia became undetectable [27]. In contrast, the avidity assay used in our study did not misclassify elite suppressors as recently infected; this was confirmed using two assay platforms as the basis for the avidity assay (BioRad HIV-1/HIV-2 EIA and BioRad HIV-1/HIV-2+ O EIA). In a previous study, patients who initiated ART during the acute phase of HIV infection had muted serologic responses to HIV infection [28], which could potentially impact results obtained with an antibody avidity; we did not evaluate patients with early ART initiation in this study.
The changes we observed in BED-CEIA values with viral suppression are consistent with results from previous studies [29]. For example, in the Multicenter AIDS Cohort Study (MACS), men who initiated ART had an average decrease of 0.54 OD-n and that the longer patients are receiving ART the more likely they were to be misclassified as recent infection using the BED-CEIA. A recent study in South Africa found that the proportion of patients misclassified by the BED-CEIA increased with the duration of ART [30]. Our study observes that the ART-induced viral suppression results in decreased BED-CEIA OD-n values in most patients. Additionally in most patients, when the virus rebounds, our data suggests that the immune system responds by increasing the proportion of antibody that is specific for HIV. For other assays that identify recent HIV infection based on the quantity of anti-HIV antibodies (e.g. titer-based assays), the presence or absence of circulating virus may also impact the rate of false-recent misclassification.
Acknowledgments
The data in this report have not been published previously. Some related data will be presented at Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC), (San Francisco, California, September, 2012).
Funding Statement
This work was supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH). Additional support was provided by the HIV Prevention Trials Network sponsored by NIAID, National Institutes of Child Health and Human Development, National Institute on Drug Abuse (NIDA), National Institute of Mental Health, and Office of AIDS Research, of the NIH, Department of Health and Human Services (UM1-AI068613). The Johns Hopkins HIV Clinical Practice Cohort was supported by NIDA (R01-DA-11602), National Institute on Alcohol Abuse and Alcoholism (R01-AA16893), NIAID (R01-AI-80328) and NIAID (R24-AI-067039). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Brookmeyer R (2010) Measuring the HIV/AIDS epidemic: approaches and challenges. Epidemiol Rev 32: 26–37. [DOI] [PubMed] [Google Scholar]
- 2. Nelson KE, Galai N, Safaeian M, Strathdee SA, Celentano DD, et al. (2002) Temporal trends in the incidence of human immunodeficiency virus infection and risk behavior among injection drug users in Baltimore, Maryland, 1988-1998. Am J Epidemiol 156: 641–653. [DOI] [PubMed] [Google Scholar]
- 3. Janssen RS, Satten GA, Stramer SL, Rawal BD, O'Brien TR, et al. (1998) New testing strategy to detect early HIV-1 infection for use in incidence estimates and for clinical and prevention purposes. JAMA 280: 42–48. [DOI] [PubMed] [Google Scholar]
- 4. Hallett TB, Ghys P, Barnighausen T, Yan P, Garnett GP (2009) Errors in 'BED'-derived estimates of HIV incidence will vary by place, time and age. PLoS One 4: e5720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laeyendecker O, Brookmeyer R, Oliver AE, Mullis CE, Eaton KP, et al.. (2011) Factors associated with incorrect identification of recent HIV infection using the BED capture immunoassay. AIDS Res Hum Retroviruses 27. [DOI] [PMC free article] [PubMed]
- 6. van der Straten A, Van Damme L, Haberer JE, Bangsberg DR (2012) Unraveling the divergent results of pre-exposure prophylaxis trials for HIV prevention. AIDS 26: F13–19. [DOI] [PubMed] [Google Scholar]
- 7.Kahle E, Kasuba A, Baeten J, Delany S, Donnell D, et al.. (2012) Unreported antiretroviral use by HIV-1 infected members of HIV-1 serodiscordant couples enrolling in an HIV-1 prevention clinical trial; 15-18 April; International Microbicides Conference, Sydney, Australia.
- 8. Zhang C, Denti P, Walt JS, Ren Y, Smith P, et al. (2012) Population pharmacokinetic model for adherence evaluation using lamivudine concentration monitoring. Ther Drug Monit. 34: 481–4. [DOI] [PubMed] [Google Scholar]
- 9. Orrell C, Kaplan R, Wood R, Bekker LG (2011) Virological breakthrough: a risk factor for loss to followup in a large community-based cohort on antiretroviral therapy. AIDS Res Treat 2011: 469127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Incidence Assay Critical Path Working Group (2011) More and Better Information to Tackle HIV Epidemics: Towards Improved HIV Incidence Assays. PLoS Med 8: e1001045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mastro TD, Kim AA, Hallett T, Rehle T, Welte A, et al. (2010) Estimating HIV incidence in populations using tests for recent infection: issues, challenges and the way forward. Journal of HIV/AIDS Surveillance and Epidemiology 2: 1–14. [PMC free article] [PubMed] [Google Scholar]
- 12. Busch MP, Pilcher CD, Mastro TD, Kaldor J, Vercauteren G, et al. (2010) Beyond detuning: 10 years of progress and new challenges in the development and application of assays for HIV incidence estimation. AIDS 24: 2763–2771. [DOI] [PubMed] [Google Scholar]
- 13. Parekh BS, Kennedy MS, Dobbs T, Pau CP, Byers R, et al. (2002) Quantitative detection of increasing HIV type 1 antibodies after seroconversion: a simple assay for detecting recent HIV infection and estimating incidence. AIDS Res Hum Retroviruses 18: 295–307. [DOI] [PubMed] [Google Scholar]
- 14. Murphy G, Parry JV (2008) Assays for the detection of recent infections with human immunodeficiency virus type 1. Euro Surveill 13: pii18966. [PubMed] [Google Scholar]
- 15. Moore RD (1998) Understanding the clinical and economic outcomes of HIV therapy: the Johns Hopkins HIV clinical practice cohort. J Acquir Immune Defic Syndr 17 Suppl 1S38–41. [DOI] [PubMed] [Google Scholar]
- 16. Carr JK, Osinusi A, Flynn CP, Gilliam BL, Maheshwari V, et al. (2010) Two independent epidemics of HIV in Maryland. J Acquir Immune Defic Syndr 54: 297–303. [DOI] [PubMed] [Google Scholar]
- 17. Bailey JR, Lassen KG, Yang HC, Quinn TC, Ray SC, et al. (2006) Neutralizing antibodies do not mediate suppression of human immunodeficiency virus type 1 in elite suppressors or selection of plasma virus variants in patients on highly active antiretroviral therapy. J Virol 80: 4758–4770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blankson JN, Bailey JR, Thayil S, Yang HC, Lassen K, et al. (2007) Isolation and characterization of replication-competent human immunodeficiency virus type 1 from a subset of elite suppressors. J Virol 81: 2508–2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bailey JR, Brennan TP, O'Connell KA, Siliciano RF, Blankson JN (2009) Evidence of CD8+ T-cell-mediated selective pressure on human immunodeficiency virus type 1 nef in HLA-B*57+ elite suppressors. J Virol 83: 88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dobbs T, Kennedy S, Pau CP, McDougal JS, Parekh BS (2004) Performance characteristics of the immunoglobulin G-capture BED-enzyme immunoassay, an assay to detect recent human immunodeficiency virus type 1 seroconversion. J Clin Microbiol 42: 2623–2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Masciotra S, Dobbs T, Candal D, Hanson D, Delaney K, et al.. (2010) Antibody Avidity-based Assay for Identifying Recent HIV-1 Infections Based on Genetic Systems TM 1 / 2 plus O EIA. 17th Conference on Retroviruses and Opportunistic Infections. San Francisco, CA.
- 22. Laeyendecker O, Rothman RE, Henson C, Horne BJ, Ketlogetswe KS, et al. (2008) The effect of viral suppression on cross-sectional incidence testing in the Johns Hopkins Hospital Emergency Department. J Acquir Immune Defic Syndr 48: 211–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Taha TE, James MM, Hoover DR, Sun J, Laeyendecker O, et al. (2011) Association of recent HIV infection and in-utero HIV-1 transmission. AIDS 25: 1357–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Welte A, McWalter TA, Laeyendecker O, Hallett TB (2010) Using tests for recent infection to estimate incidence: problems and prospects for HIV. Euro Surveill 15. [PMC free article] [PubMed]
- 25.Laeyendecker O, Oliver A, Astemborski J, Owen M, Kirk G, et al.. (2010) Improved Precision of Cross-sectional HIV Incidence Testing Using a Multi-assay Algorithm that Includes BED and an Avidity Assay with Modified Assay Cut-offs. 17th Conference on Retroviruses and Opportunistic Infections. San Francisco, CA.
- 26. Truong HM, Kellogg T, Louie B, Klausner J, Dilley J, et al. (2009) Recent HIV-1 infection detection: comparison of incidence estimates derived by laboratory assays and repeat testing data. J Acquir Immune Defic Syndr 51: 502–505. [DOI] [PubMed] [Google Scholar]
- 27. Hatano H, Delwart EL, Norris PJ, Lee TH, Neilands TB, et al. (2010) Evidence of persistent low-level viremia in long-term HAART-suppressed, HIV-infected individuals. AIDS 24: 2535–2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kassutto S, Johnston MN, Rosenberg ES (2005) Incomplete HIV type 1 antibody evolution and seroreversion in acutely infected individuals treated with early antiretroviral therapy. Clin Infect Dis 40: 868–873. [DOI] [PubMed] [Google Scholar]
- 29. Hayashida T, Gatanaga H, Tanuma J, Oka S (2008) Effects of low HIV type 1 load and antiretroviral treatment on IgG-capture BED-enzyme immunoassay. AIDS Res Hum Retroviruses 24: 495–498. [DOI] [PubMed] [Google Scholar]
- 30. Marinda ET, Hargrove J, Preiser W, Slabbert H, van Zyl G, et al. (2010) Significantly diminished long-term specificity of the BED capture enzyme immunoassay among patients with HIV-1 with very low CD4 counts and those on antiretroviral therapy. J Acquir Immune Defic Syndr 53: 496–499. [DOI] [PubMed] [Google Scholar]