Abstract
Purpose
To evaluate cross-sectional areas of conjunctivochalasis and tear meniscus using Fourier-Domain RTVue-100 optical coherence tomography (OCT) before and after conjunctival cauterization and to evaluate inter- and intraobserver reliability.
Design
Prospective, nonrandomized, consecutive case study.
Methods
A total of 12 eyes of 7 patients with conjunctivochalasis (aged 56 to 87) were evaluated. After topical anesthesia, conjunctival cauterization was performed on the inferior bulbar conjunctiva. All patients underwent anterior segment OCT (AS-OCT) imaging prior to and 4 weeks after the procedure. Cross-sectional tear meniscus and conjunctivochalasis areas at 3 locations (nasal, center, and temporal areas) were measured in all patients.
Results
Nonsignificant increases (P = .177) in cross-sectional tear meniscus area as a whole (3 locations combined) were observed following cauterization. Cross-sectional conjunctivochalasis area measurements significantly decreased in all 3 locations after cauterization (P < .001). Mean cross-sectional conjunctivochalasis area decreased from 0.247 ± 0.24 mm2 to 0.054 ± 0.79 mm2. For 2 measurements of cross-sectional tear meniscus area by examiner 1, intraclass correlation coefficients ranged from 0.998 to 0.999. Among 2 examiners, Cronbach's alpha reliability coefficients were as high as 0.993 and 0.997 before and after conjunctival cauterization. Regarding the cross-sectional conjunctivochalasis area measurements, intraclass correlation coefficient values were similar to those of the cross-sectional tear meniscus area, but Cronbach's alpha reliability coefficients were slightly less.
Conclusions
This study indicates the AS-OCT is a useful and reproducible instrument to measure the cross-sectional area of conjunctiva prolapsing into the tear meniscus of patients with conjunctivochalasis. The method can monitor effectiveness of thermoreduction of conjunctivochalasis.
Optical Coherence Tomography (OCT), Which was introduced in the early 1990s, is a noncontact imaging method that provides detailed cross-sectional images of biological tissues by measuring their optical reflections.1–3 OCT has been widely used clinically in ophthalmologic practice for a number of years. It has been a significant advance in diagnosis and monitoring treatment of vitreoretinal diseases such as age-related macular degeneration and macular edema, as well as glaucoma.4–6
In recent years, OCT technology has evaluated the incorporation of spectral-domain (SD) imaging that offers significant advantages over the traditional time-domain (TD) OCT techniques, which include faster imaging speed, higher resolution, and better visualization.7 Simultaneously with these improvements, the utility of OCT in the ophthalmic practice has become more extended. For example, anterior segment OCT (AS-OCT), which provides high-resolution cross-sectional images of anterior segment structures, including anterior chamber angle, cornea, conjunctiva, and tear meniscus, has recently gained popularity.8–13
AS-OCT has been reported to image conjunctival filtering blebs after trabeculectomy;12,13 however, there are no reports of using AS-OCT to diagnose conjunctivochalasis or monitor efficiency of surgical therapy for this condition. The goal of the present study was to evaluate cross-sectional conjunctivochalasis and tear meniscus areas using the Fourier-Domain RTVue-100 OCT before and after conjunctival cauterization in patients with moderate to severe conjunctival chalasis.
Material and Methods
Subjects
Twelve eyes of 7 patients (2 male and 5 female) with conjunctivochalasis who did not respond to conventional medical therapies were evaluated in this prospective study. Patients with a history of previous conjunctival or lid surgery or any lid abnormalities such as ectropion, entropion, and trichiasis; contact lens use; or use of any eye drop up to 2 hours before the imaging were not included in the study. All patients had a complete anterior segment examination at each visit.
Conjunctiva Cauterization
The procedure was performed by the same surgeon (S.C.P.) in all patients. After topical anesthesia (0.5% proparacaine ophthalmic solution [Accutome-Rx, Bausch & Lomb Incorporated, Tampa, Florida, USA] and 4.0% lidocaine hydrochloride solution [Roxane Laboratories Inc, Columbus, Ohio, USA]) was instilled, redundant inferior bulbar conjunctiva was cauterized using a low-temperature handheld fine-tip thermocautery (Bovie Aaron Medical, St. Petersburg, Florida, USA). The redundant bulbar conjunctiva was grasped between the blades of a curved tying forceps and the captured tissue was cauterized down to forceps surface. Cautery was performed in a line from the lateral to medial canthus approximately 5 mm below the inferior limbus. Postoperatively, eyes were treated with 1% prednisolone acetate ophthalmic suspension (Pred Forte; Allergan, Inc., Irvine, California, USA) 4 times daily for the first week and twice daily in the second week.
Patients were asked to return for follow-up examination 1 month after the procedure. At this visit, besides routine ophthalmologic examination and AS-OCT imaging, continuity of the fluorescein-stained inferior tear meniscus and relief of irritation symptoms were also noted.
Anterior Segment Optical Coherence Tomography Measurements
All patients underwent AS-OCT imaging prior to the procedure and 4 weeks after the procedure. AS-OCT images including lower tear meniscus and conjunctivochalasis were carried out using RTVue-100 (Ver. 4.0.7.5; Optovue Inc, Fremont, California, USA) with a corneal adaptor by the same person (K.G.).
Two parameters were measured in all images: cross-sectional area of inferior tear meniscus and conjunctivochalasis.
Measurement of the cross-sectional area of lower tear meniscus and conjunctivochalasis
The lower tear meniscus and conjunctiva in each eye was imaged by vertical scans centered on the inferior cornea and the lower eyelid. The system takes 26 000 axial scans per second and has a 5-μm axial resolution and transverse resolution of 15 μm. The Cornea–Anterior Module (CAM) is additional software on the device, for anterior segment imaging. Two lens adapters with short-CAM (10 mm, higher magnitude) and long-CAM (13 mm, wide field) are available for corneal and anterior segment examination. In the current study, the images were taken after connecting the long-CAM lens to the RTVue.
Examination was performed by positioning the patient's chin on the chin rest and the forehead against the headrest, asking the patient to look straight ahead after turning off the room light as recommended. No topical anesthesia or lubricating drops were used. The red external fixation light on the headrest was used to illuminate the lower lid margin. Based on the alignment of the arrow, the image of the anterior segment was seen directly on the examination screen. The arrow that appeared in the screen was then changed from the horizontal position to vertical position. The scans were taken 2 seconds after a blink. After the scanning was performed, the software automatically measured and reduced scans to a single image. If the images obtained after scanning were not of satisfactory nature because of eye movement, the scan was repeated.
The lower tear meniscus and conjunctiva were evaluated in central, temporal, and nasal segments of each eye with a digital caliper. Prior to the measurements of tear meniscus and conjunctivochalasis areas, these images were digitally magnified 3 times to improve accuracy of defining borders of the tear meniscus and adjacent structures including conjunctiva, lower lid, and cornea (Figure 1). A tear meniscus was defined as the triangular-shaped wedge of tear film between the lower lid margin and ocular surface (cornea/conjunctiva) (Figure 1).
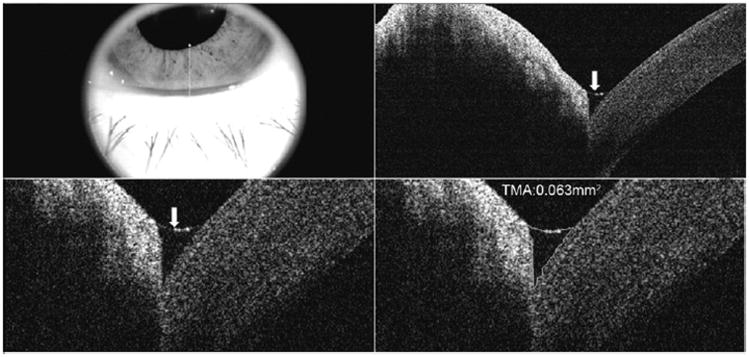
Figure 1.
Appearance of lower tear meniscus using RTVue-100. (Top left) Appearance of inferior eye lid and cornea where the vertical scans were taken. (Top right) After scanning, triangular-shaped tear meniscus (white arrow) is seen between the lower cornea and lower lid. (Bottom left) Appearance of tear meniscus (white arrow) after the image was digitally magnified 3 times. (Bottom right) After magnification, cross-sectional tear meniscus area (TMA) was measured with the instrument's software by outlining the tear meniscus.
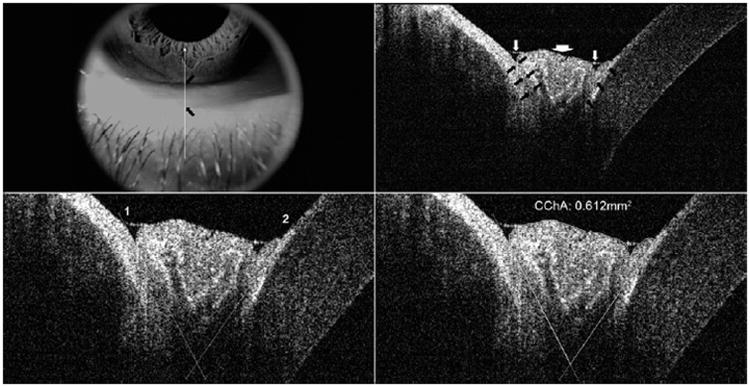
The method used to measure the cross-sectional area in images taken by the RTVue-100 is provided in Figure 2. To measure the cross-sectional area of conjunctivochalasis, the images were digitally magnified, tissue landmarks were identified by differences in brightness between tissues, and visual clues such as spaces under the conjunctiva were used to identify the starting point of prolapsing. After evaluating these landmarks, 2 lines were placed pointing to the intersection of the inferior cornea/bulbar conjunctiva and lower lid margin. Finally, the surface of the prolapsed conjunctiva was outlined with the software and the area of the conjunctiva protruding into the angle formed by these 2 lines was measured in mm2 using the instrument's software. The distance between points on the peripheral cornea and lower lid margin was measured before and after treatment in 4 patients with central conjunctivochalasis.
Figure 2.
Measurement of cross-sectional conjunctivochalasis are a (CChA) using RTVue-100. (Top left) Appearance of inferior eyelid and cornea where the vertical scans were taken. Black arrows mark the upper and lower margins of conjunctivochalasis protruding over the lid margin. (Top right) Uniform triangular-shaped tear meniscus between the cornea and lower lid is not visualized in this image; rather, 2 separate small tear menisci on either side of the chalasis are noted (white arrows). The white arrowhead points to the conjunctivochalasis. After the image was digitally magnified 3 times, tissue boundaries (black arrows) among the lower lid, prolapsed conjunctiva, and bulbar conjunctiva/inferior part of the cornea were discriminated from each based on the different levels of the brightness between tissues. (Bottom left) Based on previous determined boundaries, intersecting lines (numbered 1 and 2) were placed to outline the conjunctiva protruding into the junction of the lower lid margin and cornea. (Bottom right) Cross-sectional area of the outlined conjunctivochalasis was measured as 0.612 mm2 using the instrument's software.
In order to evaluate inter- and intraobserver variability, measurements were initially made twice by the first examiner (K.G.) at different times. Next, a second examiner (C.H.), previously informed about the nature of the study, took the same measurements from the same images obtained, with no knowledge of the first examiner's measurements. Finally, the mean of the repeated measurements taken by the first examiner was used for statistical analysis.
Statistical Analysis
The data were analyzed using SPSS 15.0 for Windows (SPSS Inc, Chicago, Illinois, USA). Intraclass correlation coefficients and Cronbach's alpha coefficients were calculated for the intraindividual and intraobserver variation. The intraclass correlation coefficient is commonly used as a measure of reliability, with a value of 1 representing a perfect correlation. To compare the baseline and follow-up measurements, paired-samples t test was used. For correlations, Spearman rank correlation coefficient was used. A value of P ≤ .05 was considered to be statistically significant.
Results
The Mean Age Of Patients Was 69.0 Years, With A range of 56 to 87. There were no postoperative complications during the follow-up period. At the first month postoperatively, all patients reported improvement in irritation symptoms. The inferior tear meniscus, visualized after fluorescein staining that was noted to be interrupted by chalasis preoperatively, was found to be continuous in all patients postoperatively.
Intraobserver and Interobserver Variability
Repeated measurements of cross-sectional tear meniscus and conjunctivochalasis areas obtained by the first examiner were analyzed and no statistically significant difference was found between these 2 different measurements (all P values > .05). Intraclass correlation coefficient values for intraobserver and interobserver agreement between the baseline and follow-up measurements of cross-sectional tear meniscus and conjunctivochalasis areas are provided in the Table. The correlation coefficients ranged from 0.938 to 0.976, indicating good agreement between measurements made by the 2 examiners. Intraobserver and interobserver correlation plots are provided in Figures 3 and 4.
Table. Intraobserver and Interobserver Repeatability of Cross-Sectional Tear Meniscus and Conjunctivochalasis Area Measurements.
| Variables | Intraobserver/Intraclass Correlation Coefficient (95% CI) | |
|---|---|---|
|
| ||
| Before (n = 36) | After (n = 36) | |
| TMA (mm2) | 0.998 (0.995–0.999) | 0.999 (0.998–1.000) |
| CChA (mm2) | 0.998 (0.996–0.999) | 0.994 (0.988–0.997) |
|
| ||
| Variables | Interobserver/Cronbach's Alpha Coefficient (95% CI) | |
|
| ||
| Before (n = 36) | After (n = 36) | |
|
| ||
| TMA (mm2) | 0.993 (0.971–0.992) | 0.997 (0.988–0.997) |
| CChA (mm2) | 0.987 (0.974–0.993) | 0.988 (0.977–0.994) |
CChA = conjunctivochalasis cross-sectional area; CI = confidence interval; TMA = tear meniscus cross-sectional area.
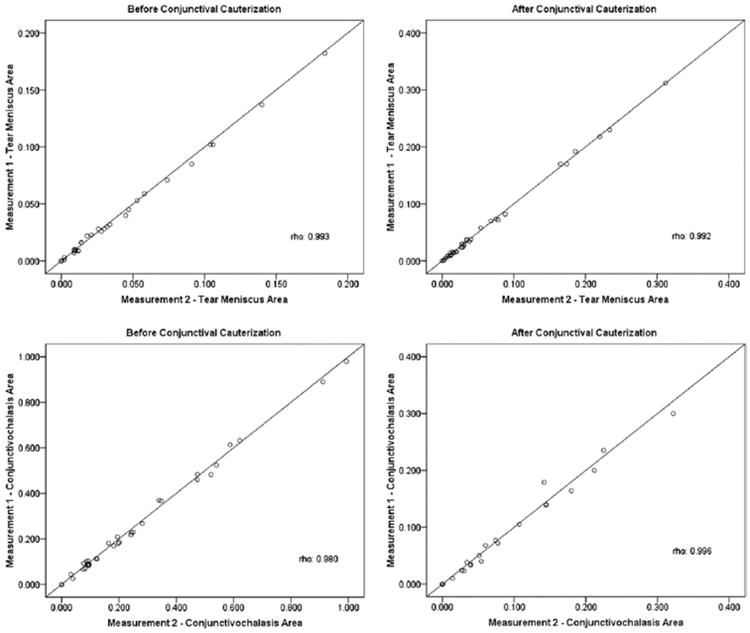
Figure 3.
These correlation plots represent intraobserver repeatability of cross-sectional tear meniscus and conjunctivochalasis areas before and after conjunctival cauterization. All measurements are in mm2.
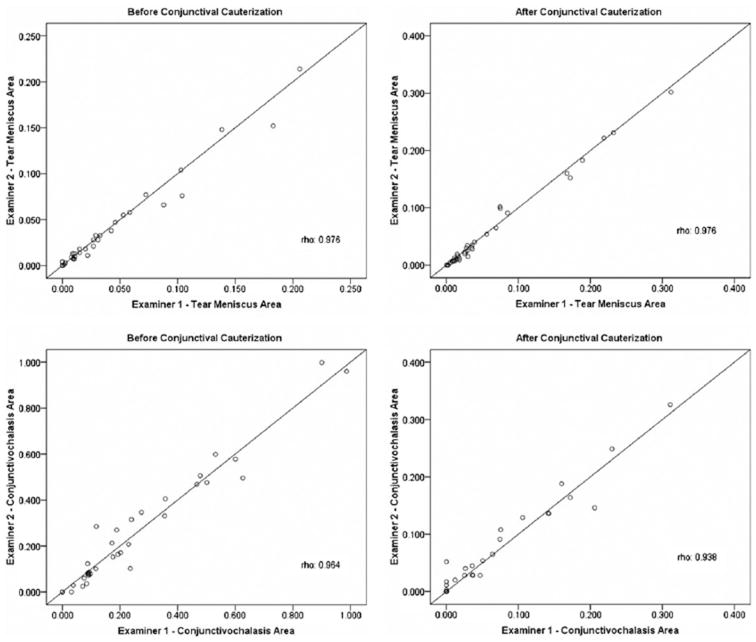
Figure 4.
These correlation plots represent interobserver agreement of cross-sectional tear meniscus and conjunctivochalasis areas between the examiner 1 and 2 before and after conjunctival cauterization. All measurements are in mm2.
Tear Meniscus Area And Conjunctivochalasis Area
Central, temporal, and nasal cross-sectional tear meniscus and conjunctivochalasis areas at baseline and after cauterization of conjunctivochalasis are provided in Figures 5 and 6. Digital image examples of biomicroscopy with fluorescein and cobalt blue filter and AS-OCT in the same patient with nasal and temporal conjunctivochalasis are provided in Figure 7.
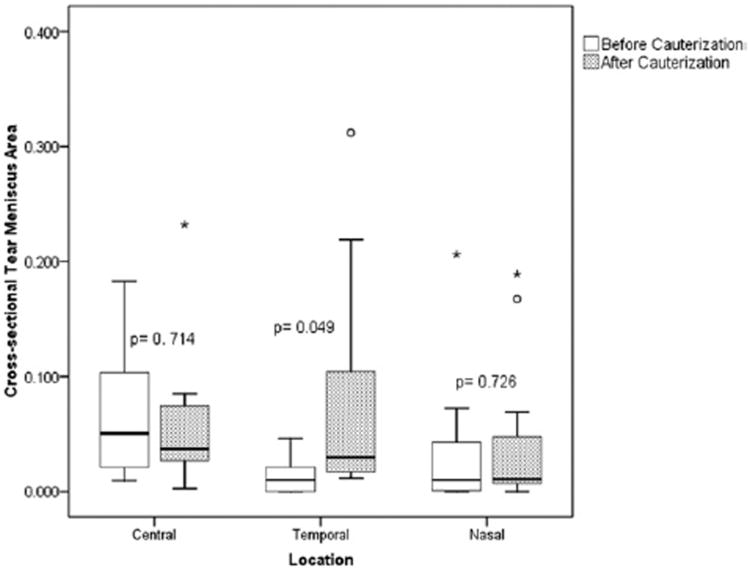
Figure 5.
Cross-sectional tear meniscus area in central, temporal, and nasal locations at baseline and following the cauterization. (The median of the data is represented by the line in the center of the rectangular box.) (* = extreme values; ° = outliers.)
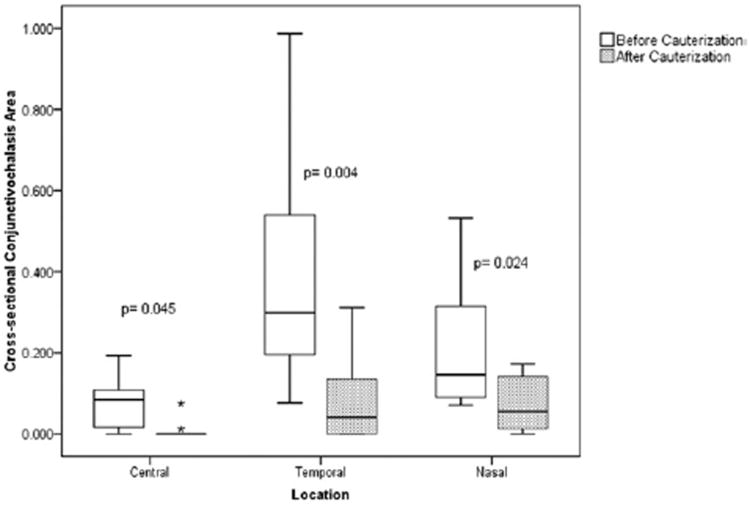
Figure 6.
Cross-sectional conjunctivochalasis area in central, temporal, and nasal locations at baseline and following the cauterization. (The median of the data is represented by the line in the center of the rectangular box.) (* = extreme values.)
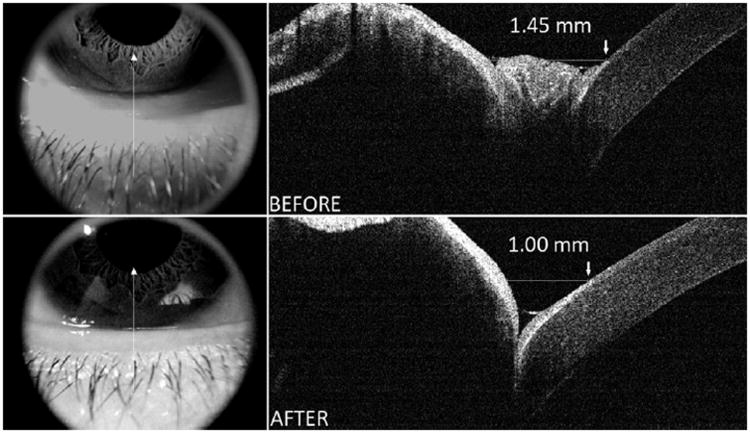
Figure 7.
An example of AS-OCT images of conjunctivochalasis located centrally before (Top right and left) and after (Bottom right and left) thermocauterization. Images show the conjunctivochalasis protruding into lower central tear meniscus shrunk after cauterization and a uniform tear meniscus was restored. The distance between landmarks on the lower cornea and lower lid was 1.45 mm prior to cauterization of severe conjunctivochalasis, decreasing to 1.00 mm after conjunctival cauterization.
Nonsignificant increases (P = .177) in cross-sectional tear meniscus area as a whole (central, temporal, and nasal locations combined) were observed following cauterization. When each location was analyzed individually, it was noted that while there was a slight decrease in the central meniscus, there was an increase in both temporal and nasal locations, reaching borderline statistical significance (P = .049) at the temporal site.
Regardless of location, overall cross-sectional conjunctivochalasis area measurements in all sites (central, temporal, and nasal) revealed a statistically significant decrease after cauterization (P < .001). Cross-sectional conjunctivochalasis area values were found to decrease from 0.247 ± 0.24 mm2 to 0.054 ± 0.79 mm2. Based on the individual analysis at each site, statistically significant differences were noted for the central, temporal, and nasal sites following cauterization. The greatest mean decrease was noted at the temporal site.
When the images before and after cauterization were analyzed, it was observed that the lower lid was pushed away by the prolapsed conjunctiva, particularly in severe conjunctivochalasis. Moreover, after removal of conjunctivochalasis by cauterization, the structures come closer and a uniform tear meniscus can be seen as a triangular shape (Figure 7). In 4 eyes with severe central conjunctivochalasis, prominent landmarks were identified on the lower cornea and lower lid, and the distance between these points was measured (Figure 7). The mean distance between these points before and after cauterization was 1.965 mm and 1.415 mm (mean difference: 0.55 mm).
Discussion
This study evaluated the ability of a novel instrument, the RTVue with anterior segment adaptor, for diagnosis of conjunctivochalasis and monitoring the area of conjunctival protrusion into the tear meniscus area in patients who underwent conjunctival cauterization to treat this condition. We mainly focused on 2 parameters, cross-sectional tear meniscus area and conjunctivochalasis area, a parameter that was described for the first time in this study. Even though slight variation was noted between a few measurements among 2 examiners, particularly in cross-sectional conjunctivochalasis area, overall the results demonstrated high intraobserver and interobserver reliability. In this pilot study, it was also documented that the cross-sectional conjunctivochalasis area was significantly reduced by conjunctival cauterization. In terms of cross-sectional tear meniscus area, even though there was no significant difference between baseline and postcauterization measurements except for the temporal location, central sequestration of tears that was observed in cases of prominent nasal or temporal conjunctivochalasis was noted to resolve with redistribution of tears along the entire length of the lower lid margin following cauterization.
With the increasing popularity of anterior segment imaging by OCT, the numbers of studies that investigated both its repeatability and its ability to image the tear meniscus in ocular surface diseases such as dry eye have gradually increased.10,11,14,15 Even though there was an error margin in the measurement of tear meniscus height or its estimated volume using the digital images, most of these studies suggested that AS-OCT provided reliable results and good repeatability.10,16
While some OCT parameters have been defined in previous reported studies, there is still no consensus regarding the best measurement parameter and calculation method for imaging the tear meniscus by AS-OCT. For instance, Wang and associates used 6 parameters, including lower and upper tear meniscus curvature, height, and cross-sectional area.10,15 Moreover, it has been suggested that upper and lower tear meniscus volumes could be calculated by using the cross-sectional areas of tear menisci and eyelid lengths.17,18 This calculation assumed that the tear meniscus was uniform across the entire length of the eyelid margins. However, because of the increased prevalence of chronic dry eye disease, conjunctivochalasis, and lid margin disease in older individuals,19 and because of the fact that tear meniscus distribution throughout the lid margin might be altered because of loosening conjunctiva as documented in the current study, regional calculations are needed to more accurately assess tear dynamics. Our findings suggest that conjunctival changes should be considered as 1 of the important factors capable of disrupting tear meniscus continuity. We only used cross-sectional tear meniscus area in the current study, because a continuous lower tear meniscus could be visualized in only a few cases. In a majority of examinations in this population with conjunctivochalasis, either there were areas along the lower lid with no tear meniscus or the meniscus shapes were amorphous because of conjunctivochalasis. Therefore, we could not have used the previously reported parameters, such as tear meniscus curvature or height.
There are limited data in the literature regarding the evaluation of conjunctiva using AS-OCT, except for the studies that imaged trabeculectomy blebs.12,13 Most of these studies assessed the AS-OCT as a promising tool to image trabeculectomy blebs, with the ability to demonstrate features of bleb morphology that are not visible with the slit lamp.12,13,20
The current study is the first to evaluate the ability of AS-OCT imaging for diagnosis and monitoring of patients with conjunctivochalasis. Lower cross-sectional tear meniscus and conjunctivochalasis areas were estimated from the cross-sectional OCT images of lower lid margin. As noted previously, we could not use tear meniscus height or curvature because of the difficulty in obtaining uniform crescent-shaped tear meniscus in most of the conjunctivochalasis images. For cross-sectional tear meniscus area measurements, both intraobserver and interobserver repeatability were high. Between 2 measurements of examiner 1, intraclass correlation coefficients ranged from 0.998 to 0.999. Among 2 examiners, the Cronbach's alpha reliability coefficients were as high as 0.993 and 0.997 before and after conjunctival cauterization. Regarding the cross-sectional conjunctivochalasis area measurements, while intraclass correlation coefficient values were similar, Cronbach's alpha reliability coefficients were slightly less than those of the cross-sectional tear meniscus area. This was probably attributable to differences between the 2 examiners' interpretation of the slopes of the anatomic structures while placing the 2 lines to outline the cross-sectional conjunctivochalasis area. A slight difference in estimation of these slopes may lead to greater differences in cross-sectional conjunctivochalasis area measurements obtained by the 2 examiners. Nevertheless, overall results indicate a high level of reproducibility and reliability of these OCT parameters in conjunctivochalasis.
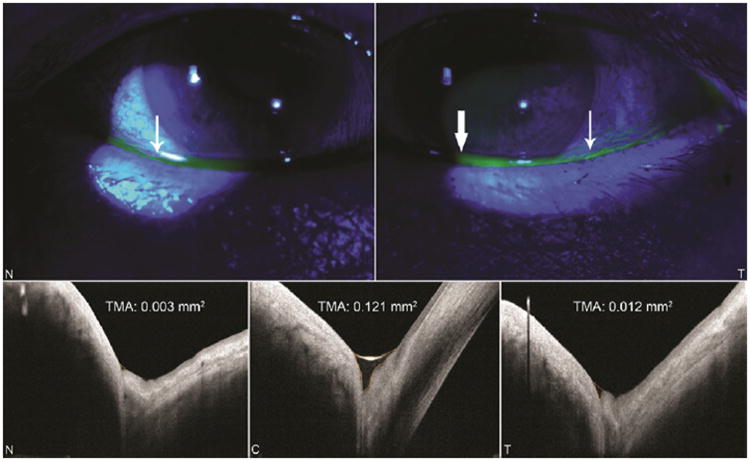
Theoretically, distribution of the inferior tear meniscus throughout the entire lid margin is expected to be affected by conjunctivochalasis. In this study, even though the difference in cross-sectional tear meniscus area before and after cauterization did not reach statistical significance, the patients who underwent conjunctival cauterization had significantly higher cross-sectional tear meniscus area values in the temporal location compared to baseline. This is consistent with the finding that cross-sectional conjunctivochalasis area was greatest temporally and was most likely to obstruct flow of tears along the lower lid in this region. Moreover, when we evaluated the cases individually, it was observed that the distribution of tear meniscus throughout the lid margin was more uniform and continuous after cauterization, as noted in Figure 8.
Figure 8.
Digital images of lid margin and ocular surface with fluorescein and cobalt blue filter (Top right and left) and anterior segment optical coherence tomography (AS-OCT) (Bottom right, left, and middle) in the same patient with nasal and temporal conjunctivochalasis. Thin white arrows in biomicroscopic images reveal nasal and temporal disruption of lower tear meniscus and thick white arrow points to central tear pooling. These biomicroscopic findings are consistent with the qualitative and quantitative AS-OCT data. Cross-sectional tear meniscus area (TMA) values are provided in AS-OCT images. (N, nasal; C, central; T, temporal.)
In terms of cross-sectional conjunctivochalasis area, significant improvement was achieved in all locations after the conjunctival cauterization (Figure 8). Regardless of location, mean cross-sectional conjunctivochalasis area values declined from 0.247 ± 0.24 mm2 to 0.054 ± 0.79 mm2 following cauterization. When we evaluated each location separately, the most profound decrease in cross-sectional conjunctivochalasis area was found in the temporal site. Furthermore, a more uniform tear meniscus was established in most cases following the cauterization.
When the images before and after cauterization were analyzed carefully, it was observed that the inferior lid is pushed anteriorly, thus causing a subclinical ectropion, which is defined for the first time in this paper. After conjunctival cauterization, the lower lid moved back toward the cornea, with the mean distance between lower cornea and lower lid decreasing from 1.96 to 1.41 mm after conjunctival cauterization. Furthermore, a uniform tear meniscus was formed. This association between conjunctivochalasis and ectropion will require verification in future clinical studies.
According to our outcomes and observations during the trial, there are some pitfalls in measuring cross-sectional tear meniscus and conjunctivochalasis areas that should be addressed in future studies, including the gaze- and blink-dependent changes and calculation methods. Another limitation is the fact that although images were taken from 3 different locations, those images may not be representative of the tear meniscus across the entire lower lid. To minimize the first issue, we attempted to standardize our method by obtaining all images with the patient looking straight ahead and 2 seconds after the last blink. While there are some recent studies that investigated calculation methods for the tear meniscus, there are no published data about how to measure conjunctivochalasis area using AS-OCT. Consequently, we have proposed a new method to measure cross-sectional conjunctivochalasis area in this study. However, this measuring method should be considered as preliminary and subject to further refinement to increase accuracy.
AS-OCT has numerous advantages over other methods such as slit-lamp biomicroscopy, ultrasound biomicroscopy, and in vivo confocal microscopy for conjunctival imaging. For instance, AS-OCT is a completely noninvasive imaging method that allows high-resolution analysis and measurement of the anterior segment without the need for ocular anesthesia, a water bath, or instillation of drops such as fluorescein. It not only provides qualitative evaluation but also provides quantitative evaluation with detailed morphology not visible with the biomicroscope. Digital image storage and comparison features are other important advantages of AS-OCT.
In conclusion, AS-OCT can measure cross-sectional conjunctivochalasis area with high reproducibility and repeatability, and could be considered as an objective confirmatory clinical imaging method for the diagnosis and monitoring of patients with conjunctivochalasis. Moreover, AS-OCT could be very useful as a clinical research tool to study conjunctivochalasis objectively.
Acknowledgments
Publication of this article was Supported by grant #Ey11915 From National Institute Of Health, Bethesda, Maryland; an unrestricted grant from Research to Prevent Blindness (New York, New York); the Oshman Foundation (Houston, Texas); the William Stamps Farish Fund (Houston, Texas), Hamill Foundation (Houston, Texas) - all for S.C.P; and the Scientific and Technological Research Council of Turkey (Ankara, Turkey) (K.G.). The authors have no proprietary interest in any of the findings reported in this manuscript. Involved in design and conduct of the study (S.C.P., K.G.); collection of data (S.C.P., K.G., C.H.C.); management (K.G., S.C.P.), analysis (K.G., S.C.P.), and interpretation of the data (K.G., S.C.P.); and preparation, review, and approval of the manuscript (K.G., S.C.P.). This study was approved by the Baylor College of Medicine Institutional Review Board. The research protocol adhered to the tenets of the Declaration of Helsinki for clinical research. Written informed consent was obtained from all the participants after explanation of the purpose and possible consequences of the study. The authors have had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Biographies

Koray Gumus, MD, FEBO, received a medical degree with high honors from Hacettepe University Medical Faculty in Ankara, Turkey, and completed his residency there in Ophthalmology. He joined the faculty of the Department of Ophthalmology at Erciyes University Medical Faculty, Kayseri, Turkey. He is board certified by the European Board of Ophthalmology, Turkish Board of Ophthalmology and International Council of Ophthalmology. He currently works as a postdoc fellow in Ocular Surface Center at Baylor College of Medicine, Houston, Texas. His main research interests include corneal and ocular surface diseases, contact lens, cataract and refractive surgery.
Stephen C. Pflugfelder, MD, joined the faculty of the Cullen Eye Institute of Baylor College of Medicine as a Professor and Director of the Ocular Surface Center in July 2000. He has published over 200 peer-reviewed articles and over 45 book chapters and monographs, primarily in the field of cornea diseases and surgery. Dr Pflugfelder's research interests include the role of inflammation in dry eye and corneal bioengineering.
References
- 1.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254(5035):1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blumenthal EZ, Williams JM, Weinreb RN, et al. Reproducibility of nerve fiber layer thickness measurements by use of optical coherence tomography. Ophthalmology. 2000;107(12):2278–2282. doi: 10.1016/s0161-6420(00)00341-9. [DOI] [PubMed] [Google Scholar]
- 3.Chen TC, Cense B, Pierce MC, et al. Spectral-domain optical coherence tomography: ultra high-speed, ultra high-resolution ophthalmic imaging. Arch Ophthalmol. 2005;123(12):1715–1720. doi: 10.1001/archopht.123.12.1715. [DOI] [PubMed] [Google Scholar]
- 4.González-García AO, Vizzeri G, Bowd C, Medeiros FA, Zangwill LM, Weinreb RN. Reproducibility of RTVue retinal nerve fiber layer thickness and optic disc measurements and agreement with Stratus optical coherence tomography measurements. Am J Ophthalmol. 2009;147(6):1067–1074. doi: 10.1016/j.ajo.2008.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Menke MN, Dabov S, Knecht P, Sturm V. Reproducibility of retinal thickness measurements in patients with age-related macular degeneration using 3D Fourier-domain optical coherence tomography (OCT) (Topcon 3D-OCT 1000) Acta Ophthalmol. doi: 10.1111/j.1755-3768.2009.01692.x. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 6.Jittpoonkuson T, Garcia P, Rosen RB. Correlation between fluorescein angiography and spectral domain optical coherence tomography in the diagnosis of cystoid macular edema. Br J Ophthalmol. doi: 10.1136/bjo.2009.170589. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 7.Leitgeb R, Hitzenberger CK, Fercher AF. Performance of Fourier-domain vs. time-domain optical coherence tomography. Opt Express. 2003;11(8):889–894. doi: 10.1364/oe.11.000889. [DOI] [PubMed] [Google Scholar]
- 8.Sakata LM, Lavanya R, Friedman DS, et al. Comparison of gonioscopy and anterior segment ocular coherence tomography in detecting angle closure in different quadrants of the anterior chamber angle. Ophthalmology. 2008;115(5):769–774. doi: 10.1016/j.ophtha.2007.06.030. [DOI] [PubMed] [Google Scholar]
- 9.Doors M, Tahzib NG, Eggink FA, Berendschot TT, Webers CA, Nuijts RM. Use of anterior segment optical coherence tomography to study corneal changes after collagen cross-linking. Am J Ophthalmol. 2009;148(6):844–851. doi: 10.1016/j.ajo.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 10.Wang J, Aquavella J, Palakuru J, Chung S. Repeated measurements of dynamic tear distribution on the ocular surface after instillation of artificial tears. Invest Ophthalmol Vis Sci. 2006;47(8):3325–3329. doi: 10.1167/iovs.06-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen Q, Wang J, Shen M, et al. Lower volumes of tear menisci in contact lens wearers with dry eye symptoms. Invest Ophthalmol Vis Sci. 2009;50(7):3159–3163. doi: 10.1167/iovs.08-2794. [DOI] [PubMed] [Google Scholar]
- 12.Singh M, Aung T, Aquino MC, Chew PT. Utility of bleb imaging with anterior segment optical coherence tomography in clinical decision-making after trabeculectomy. J Glaucoma. 2009;18(6):492–495. doi: 10.1097/IJG.0b013e31818d38ab. [DOI] [PubMed] [Google Scholar]
- 13.Ciancaglini M, Carpineto P, Agnifili L, et al. Filtering bleb functionality: a clinical, anterior segment optical coherence tomography and in vivo confocal microscopy study. J Glaucoma. 2008;17(4):308–317. doi: 10.1097/IJG.0b013e31815c3a19. [DOI] [PubMed] [Google Scholar]
- 14.Wang J, Cox I, Reindel WT. Upper and lower tear menisci on contact lenses. Invest Ophthalmol Vis Sci. 2009;50(3):1106–1111. doi: 10.1167/iovs.08-2458. [DOI] [PubMed] [Google Scholar]
- 15.Wang J, Palakuru JR, Aquavella JV. Correlations among upper and lower tear menisci, noninvasive tear break-up time, and the Schirmer test. Am J Ophthalmol. 2008;145(5):795–800. doi: 10.1016/j.ajo.2007.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou S, Li Y, Lu AT, et al. Reproducibility of tear meniscus measurement by Fourier-domain optical coherence tomography: a pilot study. Ophthalmic Surg Lasers Imaging. 2009;40(5):442–447. doi: 10.3928/15428877-20090901-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mainstone JC, Bruce AS, Golding TR. Tear meniscus measurement in the diagnosis of dry eye. Curr Eye Res. 1996;15(6):653–661. doi: 10.3109/02713689609008906. [DOI] [PubMed] [Google Scholar]
- 18.Palakuru JR, Wang J, Aquavella JV. Effect of blinking on tear dynamics. Invest Ophthalmol Vis Sci. 2007;48(7):3032–3037. doi: 10.1167/iovs.06-1507. [DOI] [PubMed] [Google Scholar]
- 19.Di Pascuale MA, Espana EM, Kawakita T, Tseng SC. Clinical characteristics of conjunctivochalasis with or without aqueous tear deficiency. Br J Ophthalmol. 2004;88(3):388–392. doi: 10.1136/bjo.2003.025460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh M, Chew PT, Friedman DS, et al. Imaging of trabeculectomy blebs using anterior segment optical coherence tomography. Ophthalmology. 2007;114(1):47–53. doi: 10.1016/j.ophtha.2006.05.078. [DOI] [PubMed] [Google Scholar]