Quality of care for patients with cancer has received significant attention from a diverse array of stakeholders. Given the large numbers of patients diagnosed and treated annually, the toxicities associated with cancer therapies, and the substantial costs incurred, high-quality cancer care is a shared priority for policymakers, institutions, providers, and patients. Despite the seminal report by the National Cancer Policy Board1 that documents the substantial quality deficits in US cancer care delivery, little progress has been documented in standardizing the care experience for patients with cancer, particularly those who receive inpatient care.
Oncology nurses play a critical role in the delivery of care to hospitalized patients with cancer. Investigators have identified significant associations between adequate hospital nurse staffing and patient outcomes in both oncology2 and non-oncology settings.3–6 To date, there have been few studies that examine how staffing variations influence daily nursing care delivered to hospitalized patients with cancer. Variation in daily care quality likely influences the prevention, detection, and successful management of complications. One potential source of variation in daily care quality is missed nursing care, which is considered conceptually an error of omission7 and is defined operationally as any aspect of required patient care that is omitted (either in part on whole) or significantly delayed.8
A diverse group of investigators have confirmed a significant relationship between the quality of care and omitted nursing care. Sochalski9 identified a significant relationship between omitted care and perceived quality of care. Schubert and colleagues10 established significant relationships between care omitted due to poor staffing and adverse patient outcomes, including medication errors, patient falls, infections, and pressure ulcers. Kalisch and colleagues have completed several studies to quantify the patterns and correlates of missed care in inpatient units.11–13 In a qualitative inquiry, 9 areas of missed care (ambulation, turning, delayed or missed feedings, patient teaching, discharge planning, emotional support, hygiene, intake and output documentation, and surveillance) and 7 reasons for missed nursing care (too few staff, poor use of existing staff resources, time required for the nursing intervention, poor teamwork, ineffective delegation, habit, and denial) were identified.11 These areas and reasons for missed care have been distilled into the MISSCARE Survey, which has been validated previously.12 In a completed study of inpatient medical-surgical units, increased missed care has been associated significantly with poor staffing, either by a measure of nurse perception or by empirical staffing data.13,14
Our understanding of missed nursing care in inpatient oncology settings is limited, largely by the absence of multi-site studies with sufficient numbers of oncology units and personnel to report on the phenomena. Hence, this study attempts to bridge the knowledge gap by describing the patterns and correlates of missed nursing care in this high-risk, understudied setting.
Conceptual Framework
Informed by the seminal work of Donabedian,15 Kalisch’s Missed Nursing Care Model guided this analysis (see Figure 1).8 Structural antecedents to missed care include hospital (ie., Magnet hospital status) and unit characteristics (e.g., nurse staffing, clinical specialty). Missed care may occur along recognized dimensions of nursing process, from assessment/diagnosis (i.e., assessment for pressure ulcer risk) through implementation (i.e., perineal skin care), and evaluation (i.e., assessment of skin integrity at discharge). Outcomes may be patient- or staff- focused. In the current analysis, we examined those factors related to the structure and process that have been shown previously to correlate significantly with missed nursing care. These include characteristics of both unit personnel (role type, education, years of experience) and of nursing units (oncology specialization versus no oncology specialization, skill mix, and unit-level staffing).
Figure 1.
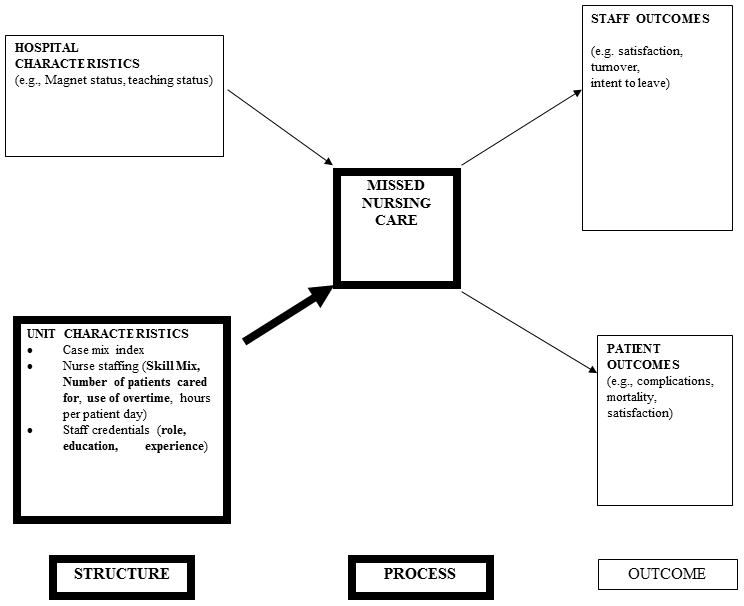
The Missed Care Model and variables examined in the current study are shown. Bolded sections indicate variables studied in the current analyses.
Research Questions
The purpose of the study was to quantify the degree of missed nursing care in oncology units, compare missed nursing care between oncology and non-oncology medical surgical units, and identify correlates of missed nursing care in oncology units. The specific study questions included:
What elements of nursing care are missed frequently or always on oncology units?
Does missed nursing care vary significantly between oncology units and other non-oncology, medical-surgical units?
Is unit staffing significantly associated with missed nursing care on oncology units?
Methods
Settings and Participants
This secondary analysis examined survey data obtained from nursing assistants and nurses (both registered and licensed practical) who provided direct patient care in medical-surgical units across 9 hospitals in one Midwestern state. Given institutional differences in the care delivery models across settings, nurses and nursing assistants were invited to participate in the study. Data were collected following institution-specific human subjects and administrative approval between November 2008 and April 2009, with an overall response rate of 59.8 percent.
Instrument
The MISSCARE Survey was administered to study participants on the nursing units. Responses were anonymous with the exception that questionnaires were coded with unit identifiers to enable aggregation of responses to specific nursing units. The MISSCARE Survey examined staff perceptions of the frequency of missed nursing care and the reasons for missed care on their unit. The total number of items is 38 for Parts A (elements of missed care) and B (reasons for missed care). The current analysis focuses solely on the frequency of missed nursing care. Additional data collected from the survey included respondent characteristics (years of experience, gender, role, education), work schedules (shift and hours worked) and staffing (absenteeism, reported workloads, and perceived staffing adequacy). Favorable factor analysis results and a test-retest coefficient of 0.87 (p < .05) were published previously in a sample of nurses and nursing assistants.16 The average completion time is 10 minutes.
Study Procedures
We obtained Institutional Review Board from our university and from each participating hospital. Eligible respondents (nursing assistants, registered nurses, and licensed practical nurses who worked 30 or more hours per week on a medical surgical unit) were provided with a study packet that included the MISSCARE Survey, a return envelope, and a candy bar incentive. Nursing units who achieved ≥ 50 percent response rates received an additional incentive of a staff pizza party. Each unit received a locked box for questionnaire returns, with an average timeframe of survey administration across study units of 2 weeks.
Data Analysis
This secondary analysis used an analytic dataset of responses from registered nurses, licensed practical nurses and nursing assistants who worked in medical-surgical units. For the secondary analysis, units were further classified into serving oncology or non-oncology patient populations. Nursing unit specialization was selected as an independent variable given the differences in work environment, job satisfaction, and perceived quality of care reported in previous studies.17, 18 Consistent with the previously-reported primary study, after we examined demographics of the analytic sample, we quantified the degree to which the 24 identified items of nursing care (as measured by the MISSCARE Survey) were reported as missed rarely, occasionally, frequently, or always. Next, we used the total score of the MISSCARE Survey, which is the average amount of missed care reported by a respondent. The total score is based on a four-point Likert scale, where 1= rarely missed and 4 = always missed. We compared the total missed care score between nursing personnel employed in oncology versus non-oncology units by student’s t-test. Finally, with our restricted sample of 352 nursing personnel employed on oncology units in this secondary analysis, we used linear regression to estimate the correlates of increased missed nursing care based on the total missed nursing care score. The linear regression included respondent characteristics (age, job title, education, years of experience, overtime worked) and unit characteristics (number of patients care for on the last shift). We used robust cluster methods to adjust the standard errors for respondent clustering in nursing units.
Results
This secondary analysis included 9 hospitals and 62 nursing units: 12 identified as oncology units (352 total respondents) and the remaining 50 identified as non-oncology, medical/surgical units (1,966 total respondents). Few significant differences were observed in respondent characteristics between groups (see Table 1). However when compared with non-oncology units, oncology units had significantly higher proportions of nursing personnel with 2 or more years of role experience (chi-square 20.83, p < .001) and longer tenures on their current unit (chi-square 15.21, p < .01). Oncology unit personnel also worked significantly more overtime than non-oncology unit personnel (chi-square 6.77, p < .05).
Table 1.
Sample Characteristics by Nursing Unit Type
| Variables | Description | Non-oncologya n=1,966 |
Oncologya N=352 |
|---|---|---|---|
| Gender | Male | 173 (8.9) | 29 (8.4) |
| Female | 1761 (91.1) | 316 (91.6) | |
| Age | Under 25 years | 344 (17.5) | 52 (14.8) |
| 26–34 | 617 (31.5) | 105 (29.9) | |
| 35–44 | 473 (24.1) | 88 (25.1) | |
| Over 45 | 527 (26.9) | 106 (30.2) | |
| Highest education | Grade | 11 (0.6) | 6 (1.7) |
| High School or GED | 326 (16.7) | 53 (15.4) | |
| Associates degree | 772 (39.7) | 130 (37.7) | |
| Bachelors degree | 779 (40.0) | 145 (42.0) | |
| Graduate degree | 59 (3.0) | 11 (3.2) | |
| Nursing education | Licensed Practice Nurse Diploma | 36 (2.4%) | 6 (2.2) |
| Registered Nurse Diploma | 101 (6.8%) | 20 (7.4) | |
| Associate degree | 661 (44.2) | 110 (40.6) | |
| Bachelors degree | 664 (44.4) | 130 (48.0) | |
| Masters degree | 34 (2.3) | 5 (1.8) | |
| Job title | Registered Nurse | 1443 (73.4) | 261 (74.1) |
| Licensed Practical Nurse | 32 (1.6) | 8 (2.3) | |
| Nursing Assistant | 491 (25.0) | 83 (23.6) | |
| Hours Worked | Less than 30 hours | 398 (20.3) | 73 (20.9) |
| 30 hours or more | 1564 (79.7) | 277 (79.1) | |
| Shift | Day | 986 (50.3) | 161 (46.0) |
| Evening | 184 (9.4) | 42 (12.0) | |
| Night | 659 (33.6) | 122 (34.9) | |
| Rotates | 132 (6.7) | 25 (7.1) | |
| Role Experience | Up to 6 months | 98 (5.0) | 22 (6.3)b |
| 6 months to 2 years | 533 (27.3) | 61 (17.4) | |
| 2 years to 5 years | 388 (19.9) | 97 (27.7) | |
| 5 years to 10 years | 360 (18.5) | 65 (18.6) | |
| Greater than 10 years | 572 (29.3) | 105 (30.0) | |
| Current Unit Experience | Up to 6 months | 147 (7.5) | 30 (8.6)b |
| 6 months to 2 years | 619 (31.7) | 79 (22.6) | |
| 2 years to 5 years | 468 (24.0) | 110 (31.5) | |
| 5 years to 10 years | 388 (19.9) | 71 (20.3) | |
| Greater than 10 years | 329 (16.9) | 59 (16.9) | |
| Shift Length | Less than 12 hours | 473 (24.1) | 97 (27.7) |
| 12 hours | 1389 (70.7) | 243 (69.4) | |
| Other | 102 (5.2) | 10 (2.9) | |
| Overtime | None | 625 (31.9) | 91 (26.1)c |
| 1–12 hours | 952 (48.6) | 173 (49.6) | |
| More than 12 hours | 383 (19.5) | 85 (24.4) |
Abbreviations: GED, General educational development.
Values given are n (%).
P < .05 (values compared between oncology and non-oncology units).
P < .01 (values compared between oncology and non-oncology units).
Differences in Missed Nursing Care between Oncology and Non-Oncology Units
First, we examined the elements of missed nursing care reported either frequently or always missed, as reported by oncology unit personnel (see Figure 2), with only the ten most frequently missed care items reported (out of the total 24 items on the questionnaire). Ambulation of patients three times a day or as ordered was the item most frequently reported as missed (total 39.1%, 37.0% frequently missed, 2.1% always missed), followed by attendance at interdisciplinary care conferences (total 31.3%, 25.3% frequently missed, 6% always missed). The third item most frequently missed was mouth care (total 23.9%, 23% frequently missed, 0.9% always missed). The top three most-frequently reported elements of missed nursing care were also the most-frequently reported elements in non-oncology units.13
Figure 2.
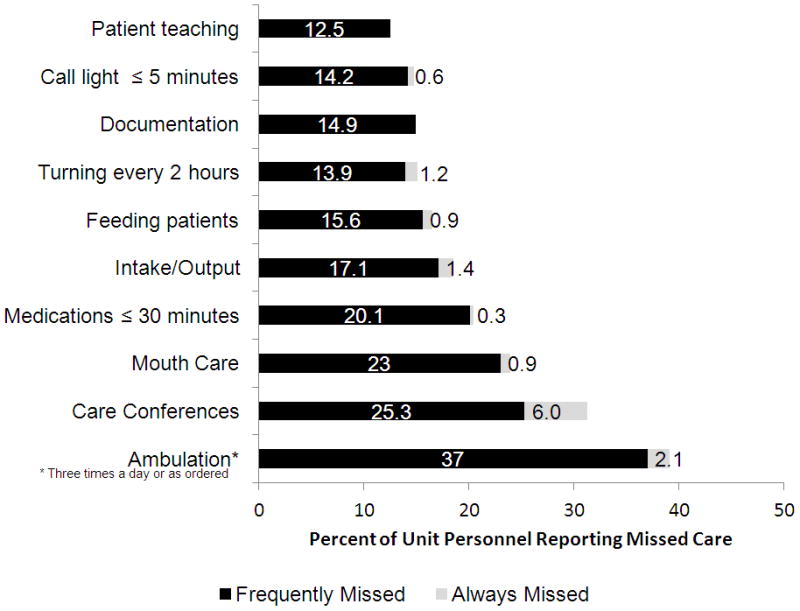
The proportion of respondents in oncology units who indicated care elements were frequently or always missed is shown.
Next, we compared differences in reported missed care between oncology and non-oncology units, as reflected by the mean scores on the total missed care score and the scores for the individual items. Compared with non-oncology units, the total overall score of the MISSCARE Survey was significantly lower on oncology units (t-test = 2.20, p < .05), reflecting that respondents from oncology units report less missed care than their counterparts from non-oncology units (see Table 2). In no instance did the frequency of missed nursing care for any item reported by oncology personnel exceed the average score by non-oncology personnel.
Table 2.
Differences in Missed Nursing Care between Oncology and Non-Oncology Units
| Variable | Oncologya n=352 |
Non-oncologya n=1,966 |
|---|---|---|
| Overall missed nursing care | 1.50±.21 | 1.57±.15b |
| Ambulation | 2.03±.36 | 2.13±.28 |
| Turning | 1.65±.31 | 1.77±.23b |
| Feeding | 1.65±.26 | 1.82±.30c |
| Meal set up | 1.35±.27 | 1.47±.22c |
| Timely medication administration | 1.76±.33 | 1.79±.24 |
| Vital signs | 1.27±.29 | 1.29±.17 |
| Monitoring intake and output | 1.59±.40 | 1.65±.38 |
| Full documentation | 1.60±.29 | 1.73±.24c |
| Patient teaching | 1.62±.25 | 1.72±.22b |
| Emotional support | 1.47±.25 | 1.53±.22 |
| Bathing | 1.50±.27 | 1.56±.22 |
| Mouth care | 1.81±.32 | 1.93±.31b |
| Hand washing | 1.27±27 | 1.35±.19 |
| Patient discharge planning | 1.29±.28 | 1.31±.14 |
| Glucose monitoring | 1.14±.32 | 1.17±.13 |
| Assessment each shift | 1.11±.29 | 1.12±.10 |
| Focused reassessments | 1.28±.27 | 1.29±.15 |
| Intravenous line /central line care | 1.32±.26 | 1.47±.18c |
| Call light response | 1.54±.31 | 1.67±.29b |
| PRN meds administration | 1.45±.25 | 1.52±.21 |
| Meds effectiveness assessment | 1.52±.25 | 1.63±.20c |
| Attend interdisciplinary care conferences | 1.99±.28 | 2.05±.50 |
| Assist with toileting | 1.54±.24 | 1.60±.23 |
| Skin/Wound care | 1.32±.26 | 1.39±.15b |
Abbreviations: PRN, as needed.
Values given are mean ± SD.
P < .05 (values compared between oncology and non-oncology units).
P < .01 (values compared between oncology and non-oncology units).
Unit Staffing and Missed Nursing Care in Oncology Units
Our final analyses considered the relationship between unit staffing and the total missed care score. These analyses were performed at the individual respondent level with an adjustment for respondent clustering within nursing units (see Table 3). After adjusting for respondent characteristics, including age, job title, education, years of experience, and overtime hours in the last week, the number of patients cared for on the last shift had a significant relationship to the total missed care score. A one-patient increase in the assignment of respondents was associated with a 2.1 percent increase in the total missed nursing care score (p < .05). In a secondary analysis (results not shown), similar relationships were found when a measure of perceived staffing adequacy was used in place of reported respondent workload on the last shift).
Table 3.
Summary of Multiple Regression for Missed Nursing Care (n= 352)
| Independent Variable | B | Robust SE | t | p |
|---|---|---|---|---|
| Constant | 1.29 | 0.11 | 11.75 | <.01 |
| Age | 0.01 | 0.02 | 0.60 | .56 |
| Job title | ||||
| Registered nurse | - | - | - | - |
| Licensed practical nurse | −0.19 | 0.13 | −1.46 | .17 |
| Nursing assistant | −0.39 | 0.07 | −6.05 | <.01 |
| Education | ||||
| Grade, High School or GED | - | - | - | - |
| Associate degree | −0.09 | 0.04 | −2.12 | .06 |
| Bachelor’s degree or higher | 0.01 | 0.06 | 0.01 | .99 |
| Years of experience in the role | 0.04 | 0.03 | 1.44 | .18 |
| Overtime (yes versus no) | 0.04 | 0.05 | 0.81 | .43 |
| Number of patients cared for | 0.02 | 0.01 | 2.31 | .04 |
Note. R2 = .124, p < .000, F(8, 11) = 20.58
Discussion
This paper examined the phenomena of missed nursing care as a contributor to aberrant quality of care for hospitalized patients with cancer. Specifically, we hypothesized that poorer staffing of nursing personnel would be associated with missed nursing care. Several items of nursing care were frequently or always missed on oncology units. When compared with non-oncology units, overall missed care was lower on oncology units, although these absolute and relative differences were negligible. After adjusting for respondent clustering in nursing units and important covariates, we confirmed our hypothesis and identified a significant relationship between higher patient workloads and reported missed nursing care. These findings support the tenets of the Missed Care model that assert a relationship between structure (ie., unit-level staffing) and processes of care (missed nursing care).
Placed into the broader literature that examines differences in care quality across nursing units, our findings explain in part results from other investigators who have examined these phenomena. In two independent investigations, significantly higher job satisfaction and quality of care were reported by inpatient oncology nurses when compared with non-oncology nurses.17,18 The current study findings that identified less missed nursing care on oncology units may explain why oncology nursing staff perceive quality of care as higher than their medical-surgical counterparts. Perhaps more importantly, our findings may explain why hospital nurse staffing has been associated with complications, failure to rescue, and mortality in a diverse array of studies.2–6 If nurse staffing is associated with missed nursing care, it is likely that higher missed nursing care results in delayed detection or management of complications, which may in turn hasten mortality for at-risk patients.
Study Limitations
Our study has several limitations worthy of further discussion. First, this was a secondary analysis and the original study was not designed a priori to compare differences in missed care across types of nursing units. This results in an unbalanced proportion of respondents and units by oncology unit status. The source of all data for the study come from nurses and nursing assistants in the clinical setting and were not validated with external data sources, such as independent observation, patient report or correlation with clinical documentation. It is possible that nurses and nursing assistants perceive missed care differently, and this question should be evaluated in a future study that is adequately powered to detect differences by job category. The questionnaire in its current form is not specific to missed care omitted during a specific timeframe. Instead, it captures the general degree to which care is missed on a particular nursing unit. However, these limitations are presented alongside a multi-site study with large numbers of units and respondents and the use of previously-validated measures.
Implications
The issue of missed nursing care is of importance to both oncology and non-oncology settings. However, those items of missed nursing care reported by oncology personnel are prime targets for quality improvement efforts. Missed mouth care is especially concerning given the well-documented relationship between meticulous mouth care and reduced rates of debilitating oral mucositis for patients with cancer.18 Managers and clinicians can partner to assure patients receive appropriate mouth care to reduce preventable complications and debilitating symptoms. In addition, institutional leadership should pay heed to the significant relationship between staffing and missed nursing care as they set staffing levels for nursing units. Our results also provide additional insights into how nurse staffing may influence patient outcomes.4 To date, the MISSCARE Survey has been administered in adult nursing units, including oncology units. Further testing and validation in pediatric settings is warranted. Future research directions include a sampling strategy that includes diverse hospitals and nursing units with sufficient power to detect differences in missed care and outcomes across an array of independent variables. Such a study would enable researchers to examine all concepts in the model simultaneously. Finally, the MISSCARE Survey may be a useful way for nursing units to assess improvements in nursing care delivery over time.
In summary, our findings suggest that a substantial amount of important nursing care is missed for patients with cancer and that missed care is associated with the staffing levels of nursing personnel. These findings may explain in part why outcomes for patients with cancer remain variable in the United States.1 Efforts to assure adequate staffing may reduce the variation in nursing care delivery, which may ultimately optimize outcomes for patients with cancer.
Acknowledgments
This research was supported by Pathway to Independence award (R00 NR10750) from the National Institute of Nursing Research, National Institutes of Health (Dr. Friese). Original data collection was supported by a grant from the Blue Cross Blue Shield of Michigan Foundation (Dr. Kalisch). This research was also supported in part by the National Institutes of Health through the University of Michigan’s Cancer Center Support Grant (5 P30 CA46592).
Footnotes
Conflict of interest: The authors have no conflicts of interest to disclose.
References
- 1.Hewitt ME, Simone JV National Cancer Policy Board. Ensuring Quality Cancer Care. Washington DC: National Academy of Sciences; 1999. [Google Scholar]
- 2.Friese CR, Lake ET, Aiken LH, Silber JH, Sochalski J. Hospital nurse practice environments and outcomes for surgical oncology patients. Health Serv Res. 2008;43(4):1145–63. doi: 10.1111/j.1475-6773.2007.00825.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aiken LH, Clarke SP, Sloane DM, et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 4.Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care. 2007;45(12):1195–204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- 5.Needleman J, Buerhaus P, Mattke S, et al. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346(22):1715–22. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 6.Needleman J, Buerhaus P, Pankratz VS, et al. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364(11):1037–1045. doi: 10.1056/NEJMsa1001025. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 8.Kalisch BJ, Landstrom G, Hinshaw AS. Missed nursing care: a concept analysis. J Adv Nurs. 2009;65(7):1509–1517. doi: 10.1111/j.1365-2648.2009.05027.x. [DOI] [PubMed] [Google Scholar]
- 9.Sochalski J. Is more better?: the relationship between nurse staffing and the quality of nursing care in hospitals. Med Care. 2004;42(2 Suppl):II 67–73. doi: 10.1097/01.mlr.0000109127.76128.aa. [DOI] [PubMed] [Google Scholar]
- 10.Schubert M, Glass TR, Clarke SP, et al. Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the International Hospital Outcomes Study. Int J Qual Health Care. 2008;20(4):227–237. doi: 10.1093/intqhc/mzn017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalisch BJ. Missed nursing care: a qualitative study. J Nurs Care Qual. 2006;21(4):306–313. doi: 10.1097/00001786-200610000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Kalisch BJ, Landstrom G, Williams R. Missed nursing care: errors of omission. Nurs Outlook. 2009;57(1):3–9. doi: 10.1016/j.outlook.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Kalisch BJ, Tschannen DJ, Lee H, et al. Hospital variation in missed nursing care. Am J Med Qual. 2011;26(4):291–299. doi: 10.1177/1062860610395929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kalisch BJ, Tschannen DJ, Lee KH. Do staffing levels predict missed nursing care? Int J Qual Health Care. 2011;23(3):1–7. doi: 10.1093/intqhc/mzr009. [DOI] [PubMed] [Google Scholar]
- 15.Donabedian A. Evaluating the quality of medical care. Milbank Q. 2005;83(4):691–729. doi: 10.1111/j.1468-0009.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalisch BJ, Williams R. Development and psychometric testing of a tool to measure missed nursing care (MISSCARE Survey) J Nurs Admin. 2009;39(5):211–219. doi: 10.1097/NNA.0b013e3181a23cf5. [DOI] [PubMed] [Google Scholar]
- 17.Shang J, Friese CR, Wu E, et al. Nursing practice environment and outcomes for oncology nursing. Cancer Nurs. 2012 doi: 10.1097/NCC.0b013e31825e4293. E-pub ahead of print, Jun 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friese CR. Nursing practice environments and outcomes: implications for oncology nursing. Oncol Nurs Forum. 2005;32(4):765–772. doi: 10.1188/05.ONF.765-772. [DOI] [PubMed] [Google Scholar]
- 19.McGuire DB, Correa ME, Johnson J, et al. The role of basic oral care and good clinical practice principles in the management of oral mucositis. Support Care Cancer. 2006;14(6):541–7. doi: 10.1007/s00520-006-0051-8. [DOI] [PubMed] [Google Scholar]


