Abstract
The high prevalence of health conditions among U.S. women receiving Temporary Assistance for Needy Families (TANF, or `welfare') impedes the ability of many in this group to move from `welfare-to-work', and the economic recession has likely exacerbated this problem. Despite this, few interventions have been developed to improve employment outcomes by addressing the health needs of women receiving TANF, and little is known about the impact of economic downturns on the employment trajectory of this group. Using data from a recent randomized controlled trial (RCT) that tested the efficacy of a public health nursing (PHN) intervention to address the chronic health condition needs of 432 American women receiving TANF, we examine the effect of the intervention and of recession exposure on employment. We further explore whether intervention effects were modified by select sociodemographic and health characteristics. Both marginal and more robust intervention effects were noted for employment-entry outcomes (any employment, p=0.05 and time-to-employment, p=0.01). There were significant effects for recession exposure on employment-entry (any employment, p=0.002 and time-to-employment, p<0.001). Neither the intervention nor recession exposure influenced longer-term employment outcomes (employment rate or maximum continuous employment). Intervention effects were not modified by age, education, prior TANF receipt, functional status, or recession exposure, suggesting the intervention was equally effective in improving employment-entry across a fairly heterogeneous group both before and after the recession onset. These findings advance our understanding of the health and employment dynamics among this group of disadvantaged women under variable macroeconomic conditions, and have implications for guiding health and TANF-related policy.
Keywords: health disparities, welfare policy, Temporary Assistance for Needy Families (TANF), women's health, public health nursing, economic recession, U.S.A.
Introduction
In 1996, the U.S. welfare system changed dramatically when Congress created the Temporary Assistance for Needy Families (TANF) program. Commonly referred to as “welfare reform”, a major aim of this legislation was to “end the dependence of needy parents on government benefits by promoting job preparation [and] work …” (United States 104th Congress, 1996, p.9). The legislation disproportionately affects single mothers, as they comprise approximately 96% of adults receiving TANF in the U.S. (Jones-DeWeever et al., 2003). Legislative mandates within TANF require immediate participation in job-search and/or employment-preparation activities for TANF recipients. Although employment preparation activities vary widely, expectations for women receiving TANF are clear: they need to find a job to support themselves and their children and maintain work as long as possible. When TANF program expectations are not met, sanctions are applied, which result in reductions in income support, and/or other benefits (Moffitt, 2003; Polit et al., 2001).
The implementation of TANF resulted in a precipitous drop in the number of people receiving assistance, increased employment, and higher earnings for those who left welfare for work. From 1996 to 2000, there was a 50% decline in TANF receipt – from 4.4 million families in 1996 to 2.2 million in 2000 (Fagnoni, 2001a); however, work participation rates increased 9% following welfare reform, with 59% moving into employment before, and 68% moving into employment after TANF job-search requirements were enacted (Jones-DeWeever et al., 2003). Among those who become employed, job tenure increased from 18 to 24 months, and household income increased 40% to 70% pre- and post-reform (Cancian et al., 2000; Jones-DeWeever et al., 2003; Moffitt, 2003; Polit, Widom, et al., 2001).
These apparent gains, however, have been tempered by other findings. Immediately post-reform, when the “most able” TANF recipients transitioned into work (Fagnoni, 2001a), 65% remained below the Federal Poverty Level (FPL) (Jones-DeWeever et al., 2003), 57% worried they would run out of food, and 33% skipped meals to stretch their food supply (Loprest, 1999a). Of those employed, 60% work more than 35 hours per week (Acs & Loprest, 2007), only 25–33% remain at the same job for more than one year (Jones-DeWeever et al., 2003; Polit et al., 2001), and 22–26% of TANF leavers reapply for TANF within one year, calling into question whether long-term self-sufficiency for many in this population is possible (Acs & Loprest, 2007; Cancian et al., 2000; Cao, 1996). Moreover, welfare analysts have repeatedly cautioned policymakers that the early employment gains attributed to welfare reform were observed during a time of economic stability, and that an economic downturn would likely result in vastly different TANF policy outcomes (Ziliak, 2002).
Embedded within these overall trends is significant variability in employment outcomes across the TANF population. Between 30–85% of TANF recipients confront one or more obstacles that hamper employment – including barriers related to education, work experience, and poor health (Acs & Loprest, 2007; Loprest & Zedlewski, 2006). Among them, health-related barriers are perhaps the most problematic for TANF programs to address (Fagnoni, 2002), although they are highly prevalent in the TANF population. An estimated 27–48% of TANF recipients report a health condition that limits their ability to work (Loprest & Maag, 2009; Zedlewski, 1999); up to 60% meet diagnostic criteria for Major Depressive Disorder, Post-Traumatic Stress Disorder, Generalized Anxiety Disorder, and/or a social phobia; and 70% report some limitation in physical functioning (Corcoran & Chen, 2004). In the presence of unaddressed barriers, the likelihood of moving from `welfare-to-work' and becoming self-sufficient is slim, and worsens as the number and severity of barriers increases (Zedlewski, 1999). Among the U.S. adult population with a health-related disability, 55% maintain employment, compared to only 18.2% of the TANF population with a health-related disability (Loprest & Maag, 2009).
To date, little is known about the longitudinal employment patterns of TANF recipients with chronic health conditions over time, what role macroeconomic factors play in shaping these patterns, or how to improve health and long-term employment outcomes in this group. Most studies of employment patterns among TANF recipients, for example, are based on annual cross-sectional employment data, and do not capture shorter-term employment dynamics or the cumulative rate of work over time (Corcoran & Chen, 2004; Polit et al., 2001). Of the few studies that do, findings indicate those with a health condition are employed, on average, 5.4 fewer months per year than those without (Corcoran & Chen, 2004). Despite these findings, only two intervention studies to address the health needs of women in TANF programs have been completed. Morgenstern and colleagues (2009) found intensive case management improved abstinence rates and the odds of employment among women in TANF with substance abuse disorders (n=302). Similarly, we have demonstrated that public health nursing (PHN) health screening, referral, and case management for women with chronic health conditions in TANF programs improved both depression and functional status (n=432) (Kneipp et al., 2011).
Fluctuations in the labor market have been shown to influence both welfare use and health. In late 2009, the unemployment rate in the low-wage labor force was estimated at 30%, compared to a rate of 3–4% among higher-income workers (Sum & Khatiwada, 2010). As low-wage workers are disproportionately affected during economic downturns, welfare exits due to employment decrease and applications for welfare benefits increase (Hoynes, 2000; Kwon & Meyer, 2011). Comparing data for calendar years 2007 and 2010, TANF caseloads rose an average of 11.5% in the U.S. since the onset of the recession in December 2007; however, there was wide variability in TANF participation changes across states, with caseloads in 18 states decreasing an average of 10%, while increasing an average of 25.3% in all others (U.S. Department of Health and Human Services, 2011).
In terms of health, studies have consistently shown that stress, mental health, and health-related quality of life worsen as unemployment rates rise (Davalos & French, 2011; Zivin et al., 2011). Albeit counterintuitive, total mortality and mortality from 8 of 10 preventable causes has been shown to decrease, while at the same time a number of physical health and health behavior indicators improve as state-level unemployment rates increase (Ruhm, 2000, 2001, 2005). These associations, however, vary in magnitude and direction by race and socioeconomic status (SES) (Suhrcke & Stuckler, 2012). For example, as the unemployment rate increases, the positive health effects observed in the general population are not found in African Americans and lower educated groups; rather, there is an opposite trend, with obesity and smoking rates increasing during times of economic recession in these populations (Charles & Decicca, 2008; Dooley & Catalano, 1984; Dooley et al., 1981). Taken together, these findings suggest economic recessions impact welfare program participation and the ability to leave TANF for employment, and differentially impact health by race and SES. Despite this, remarkably little is known about the effect of the recent economic recession on employment outcomes for TANF recipients with chronic health conditions, or whether interventions intended to improve health and employment in this group would be more or less effective with fluctuations in the labor market.
In this article, we report on employment findings using data from a randomized controlled trial (RCT) that tested the efficacy of a public health nursing (PHN) case management and Medicaid knowledge and skills training intervention for women in Welfare Transition Programs (WTPs) with one or more chronic health conditions. We use a generic reference to `Welfare Transition Programs (WTPs)' throughout this article to represent welfare-to-work programs across the U.S. that women receiving TANF are required to participate in. While there is some variability in the services provided in WTPs, they all operate under the same set of federal guidelines and serve a common purpose: to move TANF recipients into employment (Danziger & Seefeldt, 2003; Fagnoni, 2001a). Further description of the intervention, the main effect of the intervention on employment outcomes from the RCT, and post-hoc exploratory findings related to the role of the recession on employment outcomes are reported here. Although this article focuses on employment outcomes from the trial, the health outcomes from the intervention are presented in detail elsewhere (Kneipp et al., 2011). Taken together, these findings add to a more nuanced understanding of the relationships between health, employment, and the larger economy in the TANF population. Specifically, the aims of our analyses were to examine:
the main effect of the PHN intervention on employment outcomes by comparing women randomized to either the intervention or control group;
the main effect of the recession on employment outcomes by comparing women unexposed to the recession while in the RCT to those fully exposed to the recession while in the RCT;
the extent to which (a) recession exposure or (b) select sociodemographic and health characteristics modify the main intervention effect on employment outcomes.
Methods
The data used in our analyses are from a RCT conducted between February 2007 and April 2010. This research was approved by the University of Florida and the University of North Carolina at Chapel Hill IRBs.
Intervention Description
Using a Community-Based Participatory Research (CBPR) approach (Minkler & Wallerstein, 2003), the intervention was designed in partnership with women enrolled in a Welfare Transition Program (WTP) in north central Florida. Given the high prevalence of health-related barriers to employment in the TANF population, the absence of evidence-based practices for managing health needs within the context of WTPs, and the likelihood of chronic health conditions interfering with employment if they are not well-managed, the intervention emphasized health screening, referral, and case management conducted by a public health nurse (PHN). We adopted the chronic health condition definition used by the National Health Interview Survey, which includes “conditions that are generally not cured, once acquired” (National Center for Health Statistics, 2003, p. 29). In this definition, we include mental health conditions characterized by episodes that can result in full recovery with treatment, but have a high rate of relapse among lower socioeconomic status groups; can result in recurring functional impairment that interferes with job performance; and which have been shown to be highly prevalent in the TANF population (i.e., major depression, post-traumatic stress disorder, and generalized anxiety) (Shear et al., 2000).
To ensure the intervention was culturally sensitive, respectful, and relevant to women in the WTP, we engaged the target population in co-developing the intervention (see Lutz et al., 2009, for a detailed description). Based on recommendations from women in WTPs, the intervention also included a one-time, brief (2-hour) training session on using Medicaid effectively. Participants in the intervention group met with a PHN at baseline and underwent a comprehensive health assessment. Referral and case management activities began at this initial visit, and focused on ensuring access to and coordination of care, disease management through regular primary care and/or specialist follow-up, health education, and disease prevention. Intervention participants were scheduled for a one-hour follow-up appointment with the PHN at 3, 6, and 9 months where their health-related status was reassessed and case management activities continued. Although the intensity of case management was individualized based on participant needs, PHN contact for case management purposes averaged 4 hours and 35 minutes per participant (mean = 261 minutes, SD = 112) over the 9-month study period.
Control group participants received what would be considered usual care in the local WTP. The WTP where the study was conducted routinely provided participants with information about agencies in the community that could provide health-related services; however, there was no standardized process used to screen for, or address, chronic health conditions that could act as barriers to employment. To reduce attrition, control group participants were offered an attenuated version of the intervention at the end of the 9-month observation period, which approximately 50% opted to receive. Additional details of the study design and the main intervention effects on health outcomes are reported elsewhere (Kneipp et al., 2011; Lutz et al., 2009).
Sample & Setting
The RCT included a convenience sample of 432 women enrolled in a WTP in one urban and one rural county in North Central Florida. Study recruitment, enrollment, and follow-up on all participants were completed between February 2007 and April 2010. While the two study counties reflect differences commonly observed between rural and urban settings, unemployment rates differed in the two counties by only 0.8% prior to the recession onset, and by 1.3% after the recession onset (U. S. Department of Labor, 2011).
Enrollment criteria required women be receiving TANF, not employed, be between the ages of 18 and 60 years, have at least one chronic health condition, and speak English. The chronic health condition criterion was met by either self-report of a physical or mental health condition diagnosed by a health provider, and/or findings from the PHN health screening, which could include a `positive' screen for depression (≥17 on the Beck Depression Inventory-II [BDI-II] confirmed by the Structured Clinical Interview for DSM Disorders Axis I, Non-patient [SCID-I/NP] – Major Depressive Episode/Disorder), anxiety (≥16 on the Beck Anxiety Inventory [BAI] confirmed by the SCID-I/NP – Generalized Anxiety Disorder), or post-traumatic stress disorder (PTSD) (based on the SCID-I/NP – PTSD) as a chronic health condition. To control for expected longer-term or permanent employment interruptions in the study sample, we excluded women who were pregnant or receiving disability income. Once enrolled, participants were randomized to either the intervention or control group following the Consolidated Standards of Reporting Trials (CONSORT) guidelines for randomization (Schulz et al., 2010).
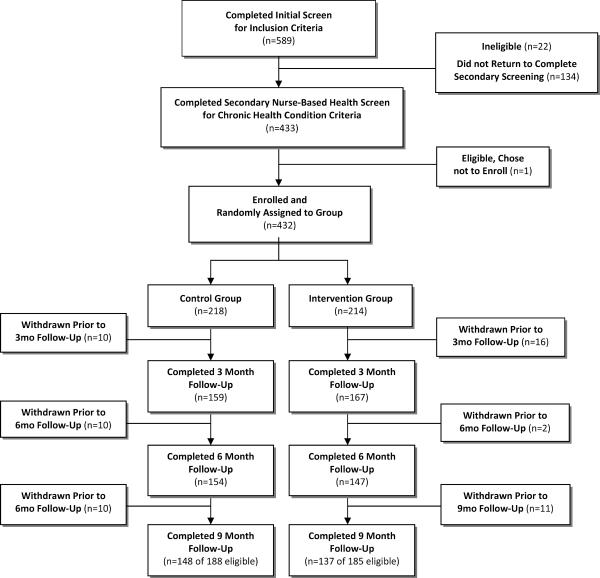
A detailed flow of participants through the study is depicted in Figure 1. During recruitment, 589 women were screened to determine if they met the initial inclusion criteria. Of those, 432 enrolled in the study (73% of those who completed initial screening). Fifty-nine participants (13.7%) had to be withdrawn at some point during the study course. Of the 373 eligible to complete the study, 76% (n=285) completed the 9-month follow-up.
Figure 1. Participant Screening, Enrollment, and Follow-Up Completion*.
*Participants withdrawn between the 3, 6, and 9 month follow-up were withdrawn by the PI due to no longer meeting inclusion criteria. Across groups, the primary reasons for withdrawal included becoming pregnant (14.6% of withdrawn participants), moved from area (52%), and other (33.3%). Reasons for withdrawal were distributed evenly across groups. Participants withdrawn for the study were not allowed to re-enter the study at a later time point; however, it was not uncommon for participants to miss an early follow-up visit and return for a subsequent follow-up. Of the 373 women eligible to complete the 9 month follow-up (i.e., those who were not withdrawn from the study - 188 in the CG, and 185 in the IG), 76% completed the final follow-up visit (n=285).
Measures
All measures were obtained at baseline and at 3, 6, and 9 months after enrollment.
Demographic & Health Measures
A brief description is included here, with these measures also presented in Table 1 for descriptive, comparative purposes by intervention group assignment and recession exposure group. Demographic variables include self-reported race, age, education level, and the number of times TANF was received previously. Health variables include the Beck Depression Inventory-II (Beck et al., 1996), the General Health subscale from the Short Form 12 version 2 (SF12v2) (Ware et al., 2005), a composite measure of functional status derived from four dimensions of the SF 12v2, the number of chronic health conditions reported at baseline, and the number of self-reported symptoms based on a review of systems checklist commonly used during primary care visits.
Table 1.
Baseline Sociodemographic & Select Health Sample Characteristics, by Select Groups (Full Sample, n=432)
| Intervention & Control Group Comparisons | Total Sample | Recession Exposure Group Comparisons | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Characteristic | Intervention | Control | Group Diff p* | No Exposure | Mixed-Exposure | Full Exposure | Group Diff p** | |
|
|
|
|||||||
| n=214 | n=218 | n=432 | n=120 | n=149 | n=163 | |||
|
|
|
|||||||
| Mean (SD) % | Mean (SD) % | Mean (SD) % | ||||||
| Age‡ | 28.8 (7.3) | 30.8 (8.9) | .03 | 29.8 (8.2) | 29.8 (8.0) | 30.1 (8.9) | 29.5 (7.4) | .99 |
| Race | ||||||||
| Black/African American | 61.2% | 51.4% | 56.3% | 51.7% | 55.0% | 60.7% | ||
| Caucasian | 35.5% | 43.1% | .09 | 39.4% | 44.2% | 39.6% | 35.6% | .57 |
| Other | 3.3% | 5.5% | 4.4% | 4.2% | 5.4% | 3.7% | ||
| Ethnicity | ||||||||
| Hispanic | 4.2% | 5.1% | .82 | 4.6% | 1.7% | 6% | 5.5% | .17 |
| Education Level | ||||||||
| <12th Grade | 32.4% | 32.6% | .84 | 32.4% | 35% | 36.2% | 27.0% | .47 |
| High School Diploma/GED | 27.8% | 26.6% | 27.8% | 26.7% | 26.2% | 30.1% | ||
| Some College/College Degree | 39.8% | 40.8% | 39.8% | 27.8% | 37.6% | 43% | ||
| County | ||||||||
| Urban | 78.5% | 82.1% | .35 | 80.3% | 80% | 79.2% | 81.6% | .86 |
| Rural | 21.5% | 17.9% | 19.7% | 20% | 20.8% | 18.4% | ||
| Prior TANF Receipt | ||||||||
| Never | 21.5% | 25.2% | .32 | 23.4% | 20% | 21.5% | 27.6% | .32 |
| 1–2 | 50.5% | 45.9% | 48.2% | 53.3% | 47.0% | 45.4% | ||
| 3–4 | 16.4% | 12.8% | 14.6% | 10.8% | 15.4% | 16.6% | ||
| 4+ | 11.7% | 16.1% | 13.9% | 15.8% | 16.1% | 10.4% | ||
| No. Jobs Held in Past Year | ||||||||
| None | 17.3% | 21.6% | .55 | 19.4% | 15.0% | 20.8% | 21.5% | .64 |
| 1–2 | 64.5% | 59.2% | 61.8% | 61.7% | 60.4% | 63.2% | ||
| 3–4 | 12.2% | 15.1% | 13.7% | 17.5% | 13.4% | 11.0% | ||
| 5 or More | 6.1% | 4.1% | 5.1% | 5.8% | 5.4% | 4.3% | ||
| No. of Jobs Left in Past Year Due to Health Problems | ||||||||
| None | 66.8% | 74.8% | .7 | 70.8% | 65.8% | 71.1% | 74.2% | .31 |
| 1 or More | 33.2% | 25.2% | 29.2% | 34.2% | 28.9% | 25.8% | ||
| Number of Children‡ | 2.5 (1.3) | 2.5 (1.2) | .85 | 2.5 (1.3) | 2.6 (1.3) | 2.4 (1.3) | 2.4 (1.2) | .31 |
| Mean Age of Children‡ | 6.6 (5.0) | 7.5 (6.0) | .20 | 7.1 (5.6) | 6.9 (5.4) | 7.0 (4.8) | 7.2 (6.3) | .11 |
| Single/unmarried | 89.3% | 87.6% | .60 | 88.4% | 88.3% | 92.6% | 84.7% | .09 |
| Total Household Income¥ | $687.5 (427.8) | $626.2 (440.3) | .11 | $656.6 (434.4) | $731.3 (462.5) | $582.3 (324.5) | $665.0 (518.8) | .11 |
| Number of Chronic Health Conditions‡ | 3.7 (2.1) | 3.8 (2.5) | .93 | 3.8 (2.3) | 3.8 (2.4) | 3.7 (2.2) | 3.8 (2.4) | .97 |
| Number of Generalized Symptoms‡ | 8.3 (6.4) | 7.9 (6.9) | .50 | 8.1 (6.6) | 7.8 (6.8) | 8.6 (7.0) | 7.8 (6.2) | .56 |
| BDI-II Depression Screen | ||||||||
| Positive (BDI-II ≥ 17) | 52.5% | 47.2% | .96 | 52.7% | 51% | 52.6% | 53.9% | .90 |
| Negative (BDI-II ≤ 17) | 47.5% | 52.8% | 47.3% | 49% | 47.4% | 46.1% | ||
| Functional Status (SF-12v2)ǂ | 61.9 (23.3) | 60.9 (23.7) | .66 | 61.4 (23.5) | 59.2 (22.5) | 62.8 (23.2) | 61.7 (24.5) | .34 |
| General Health (SF-12v2)ǂ | 41.1 (23.4) | 41.4 (23.4) | .87 | 41.3 (22.8) | 43.1 (24.6) | 39.2 (20.7) | 41.8 (23.3) | .42 |
Includes income from food stamps, TANF, work-related income, and income received from others; non-normal distribution; differences based on Wilcoxon rank sum.
Non-normal distribution; Wilcoxon rank sum test used to evaluate intervention and control group differences, and Kruskal-Wallis rank test used to assess group differences by recession exposure.
Differences in select characteristics between intervention and control group, at baseline.
Differences between groups that entered and completed study before onset of recession (No Exposure), entered the study before the onset of the recession but completed after the onset (Mixed-Exposure), and both entered and completed the study after the onset of the recession (Full Exposure); χ%2 or other non-parametric tests of significance.
Employment Measures
Four employment measures were constructed based on self-reported job beginning and ending dates gathered over the 9-month study period. Two of these relate to employment-entry (any employment and time-to-employment), while the other two reflect the amount and duration of employment (employment rate and maximum continuous employment). Constructed using employment date data, any employment refers to whether a participant was employed at any time during the 9-month study observation period. Time-to-employment measures the number of days from study enrollment to the beginning of employment. Given the majority of participants enrolled in the study within approximately one week of TANF benefits beginning, this is also a reasonable measure of the number of days from the onset of TANF receipt to beginning a job. Employment rate represents the proportion of time a participant spent working relative to the number of days observed in the study, calculated as: Number of days worked/Number of days possibly worked × 100. Maximum continuous employment measures the maximum number of days worked consecutively throughout the study, regardless of whether this continuous work period was at the same job, or different jobs. We allowed for up to a 7 day “gap” in employment as women may have moved from one job to another, in which case days within this gap (up to 7 days) would have been counted as continuous days working. In deriving this measure, we wanted to capture work effort that women could reasonably be expected to maintain some level of economic self-sufficiency, without having to re-apply for TANF benefits once in the workforce. An assumption of a 7 day gap, if it had occurred, was that income lost over this period of time “between jobs” could potentially be substituted with support from family, friends, or other non-TANF financial supports.
Recession Exposure
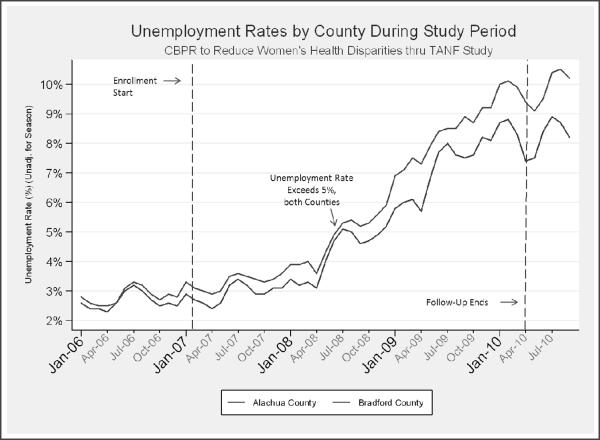
Although the National Bureau of Economic Research dates the onset of the most recent recession officially beginning in December 2007 (Rampell, 2008), the unemployment rate typically rises after a recession has been officially pronounced (Lee & Shields, 2011). As expected, unemployment rates in our study counties were relatively stable at or around 3% for several months after the recession onset (December 2007), but spiked quickly to nearly double this baseline rate in July 2008, where it exceeded 5% (U. S. Department of Labor, 2011). This marked increase occurred roughly mid-way through the 29 month study enrollment period (see Figure 2).
Figure 2.
Unemployment Rates by Study Counties, January 2006 – July 2010
In delineating recession exposed groups, our goal was to maximize the recession's impact on the ability to leave TANF for work. Given the lagged effect of recessions on unemployment, this meant for the purpose of constructing a recession exposure group variable it would be more appropriate to align the designated onset date more closely with the rise in unemployment rather than the “official” recession onset date. There were few findings in the literature, however, to empirically support selecting one unemployment rate threshold over another for delineating recession exposed groups. Ultimately, we used data from a recent study by Kwon & Meyer (2011), where the percentage of the TANF population exiting due to employment decreased roughly 10% as the unemployment rate rose 2% (from 4% to 6%) during the 2001 recession. This 2% rise during the 2001 recession approximated the 2% rise in unemployment observed in our study counties in July 2008. Therefore, for the recession exposure variable, participants were categorized into three groups based on their “exposure” to the recession and high (≥ 5%) unemployment rates, with 120 women in the full sample categorized as having “no exposure” (completing the 9-month study prior to July 2008), 149 having “mixed” exposure (enrolling prior to July 2008 but completing after this date), and 163 with “full” exposure (enrolling after July 2008, thus spending the entire study period in the labor market when the recession was most likely to impact employment opportunities).
Analyses
Analyses were conducted using Stata/SE 11.0 and SAS V. 9.2. Employment variables were calculated for participants who completed one or more follow-up measurements at 3, 6, or 9 months; thus our final analytic sample for the employment-related outcomes includes 353 women. Among those who completed each follow-up, less than 11% of data were missing on outcomes of interest; these subjects were deleted case-wise from analyses.
Given the goal of maximizing the differential impact of the recession on employment and the post-hoc, exploratory nature of the recession-related analyses, we included the two recession exposure groups that were clearly either unexposed or fully exposed to the recession while excluding the group that had mixed, or partial exposure to the recession from our main recession exposure effect and modification effect analyses. Thus, analyses that include tests of significance for differences in recession exposed groups are limited to participants in our final analytic sample (n=353) who had no exposure to the economic downturn while in the study (n=100) and participants who had enrolled and completed the study following the onset of the recession (i.e., the exposed group; n=130). Descriptive statistics of employment outcomes for each of the three recession groups were calculated to observe general trends, and are presented in Table 2.
Table 2.
Employment Outcomes by Group Assignment and Recession Exposure (n=353)*
|
|
|
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Full Sample |
Intervention Group |
Control Group |
||||||||||
| Recession Exposure§ |
Recession Exposure§ |
Recession Exposure§ |
||||||||||
| All | No Exposure | Mixed Exposure | Full Exposure | All | No Exposure | Mixed Exposure | Full Exposure | All | No Exposure | Mixed Exposure | Full Exposure | |
| Any Employment | ||||||||||||
| + Employment | 69% | 79.8% | 69.1% | 60.8% | 73.4% | 87.8% | 71.4% | 64.7% | 64.4% | 72% | 67.2% | 56.5% |
| No Employment | 31% | 20.2% | 30.9% | 39.2% | 26.6% | 12.2% | 28.6% | 35.3% | 35.2% | 28% | 32.8% | 43.5% |
| (n) | (353) | (99) | (123) | (130) | (173) | (49) | (56) | (68) | (179) | (50) | (67) | (62) |
| Time to Employment (in days)¥ | 90 | 70 | 93 | 122 | 72 | 47 | 56 | 115 | 107 | 93 | 108 | 155 |
| (n) | (243) | (79) | (85) | (79) | (127) | (43) | (40) | (44) | (116) | (36) | (45) | (35) |
| Employment Rate | 39.7 [28.6] | 47.2 [33.6] | 35.0 [36.1] | 35.0 [36.2] | 43.4 [36.0] | 53.7 [33.9] | 43.4 [37.3] | 36.0 [35.1] | 36.2 [35.1] | 40.7 [32.3] | 34.8 [34.8] | 34.0 [37.7] |
| (n) | (243) | (79) | (85) | (79) | (127) | (43) | (40) | (44) | (116) | (36) | (45) | (35) |
| Maximum Continuous Employment (in days) | 143.5 [84.4] | 142.7 [76.5] | 137.8 [88.9] | 150.3 [87.4] | 146.0 [86.1] | 144.7 [80.1] | 148.6 [93.9] | 144.7 [86.5] | 140.8 [82.8] | 140.3 [73.4] | 128.2 [84.2) | 157.4 [89.3] |
| (n) | (243) | (79) | (85) | (79) | (127) | (43) | (40) | (44) | (116) | (36) | (45) | (35) |
Analytic sample of participants in RCT with follow-up data at 3, 6, or 9 months, and for whom employment outcome of interest could be calculated; [SD].
No exposure = those who enrolled in the 9 month study period prior to onset of the recession, n= 100; full exposure = those who began study following onset of the recession, n= 130; and n=123 participants with differential, or inconsistent exposure to recession effects not included in the analyses.
Medians, based on Kaplan-Meier curve estimates.
Logistic regression was used to assess the main effects of the intervention and recession exposure on any employment. For time-to-employment, the Kaplan-Meier method with log-rank tests was used. For the employment rate analysis of main effects, a zero-inflated negative binomial (ZINB) model was used to account for over-dispersion and excess zero values (i.e., participants who did not work at all during the study period, or 31%), which could not be appropriately accounted for using a standard Poisson regression approach (Long, 1997). To analyze the main effects of the intervention and recession exposure on maximum continuous employment among participants that began employment during the study period (n=243), we applied a general linear model. All recession analyses also controlled for the main effects of the intervention group.
To examine whether recession exposure modified the main intervention effects on employment in the intervention and control groups, we included an interaction term of recession exposure x group for each of the four employment measures. To better understand how any of the wide range of sociodemographic and health characteristics at baseline might have modified the intervention effect on employment, we took a two-step approach based on emerging recommendations for guiding modification effect (i.e., subgroup) analyses of RCT data across characteristics observed at baseline. These include limiting analyses to variables that are theoretically and empirically related to the outcome of interest; using interaction terms to evaluate modifying effects; recognizing the power limitations associated with statistical testing of interaction terms in post-hoc, sub-group analyses; and emphasizing the exploratory, hypothesis-generating nature of the findings (Assmann et al., 2000; Knol & VanderWeele, 2012; Peduzzi et al., 2002; Piantadosi, 2005; Wang et al., 2007). From a theoretical perspective, the sociodemographic and health characteristics observed at baseline were potentially relevant modifiers of the intervention given previous findings in the literature (Burtless, 1997; Danziger et al., 2002; Fagnoni, 2002; Polit et al., 2001). To assess the direct relevance of these characteristics as potential modifiers within our specific study sample, we first examined bivariate associations between each of the sociodemographic and health characteristics measured at baseline with each of the four employment outcome variables. In our second step, those variables associated with employment at the p<.05 significance level in the bivariate analyses were then evaluated as potential modifiers of employment by testing for significant interactions with interventiongroup assignment.
Finally, to account for potential confounding, the number of possible days worked (i.e., the number of days participants were in the study) was controlled for in all analyses of any employment and maximum continuous employment.
Results
Sample Demographics
Sample demographics and health-related characteristics are detailed in Table 1. The RCT sample included women who were primarily Black or African American (56.3%), unmarried (88.4%), and had a mean age of 29.8 years. More than 80% had worked in the prior year, and over 76% had received TANF previously. Study participants reported a mean of 3.8 chronic health conditions, with the most common including headaches (53%), back pain (50%), depression (40%) and seasonal allergies (38%). Nearly 53% screened positive for possible depression using the Beck Depression Inventory-II at baseline. With the exception of participant age (mean = 28.8 vs. 30.8 years), there were no statistically significant differences in sociodemographic or health characteristics between the intervention and control groups at baseline, in relation to study retention, or across groups based on recession exposure (Table 1). There were, however, statistically insignificant trends by treatment group, such as the intervention group having a higher proportion of African Americans and women who had recently left jobs due to health problems. There were also some shifts in study participant characteristics based on recession exposure over the study period, with a higher proportion of African Americans, women with more education, and those that had not previously received TANF enrolling in the study after the recession began, although these differences were not statistically significant. Based on available state-level data, these shifts in study enrollment sociodemographic characteristics reflect what occurred in the TANF population as a whole from 2007 through 2009 (U.S. Department of Health and Human Services, 2011).
Main Intervention and Recession Exposure Effects
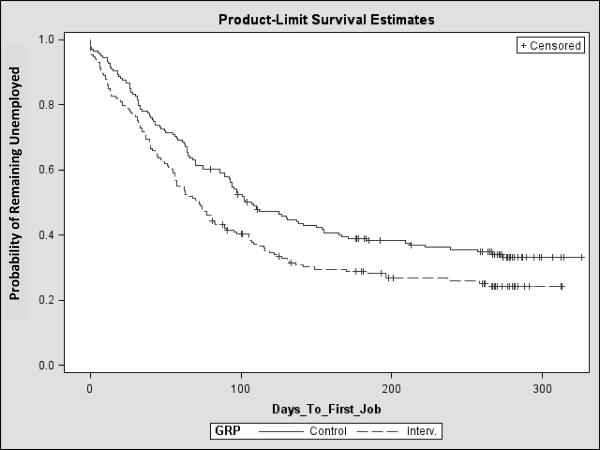
While controlling for possible days worked, among women who had follow-up employment data at either 3, 6, or 9 months (n=353), there was a marginally significant main intervention effect in any employment (i.e., whether a woman worked at all over the 9-month study period) by group assignment (p=0.05), with 73.4% of the intervention group moving into employment compared to 64.4% of the control group. There was a more robust group difference, however, in time-to-employment. The Kaplan-Meier curve (Figure 3) and log-rank test (p=0.01) show a significant decrease in the amount of time that elapsed between study enrollment and when women in the intervention group began working: median time-to-employment was 72 days for the intervention group and 107 days for the control group – over a one month difference. There was no group difference in employment rate or in maximum continuous employment.
Figure 3.
Survival Estimates for Remaining Unemployed, by Group Assignment
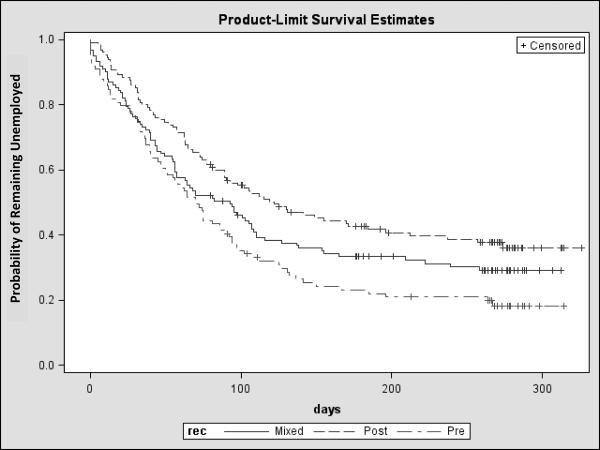
Findings were similar for the main effect of recession exposure. Controlling for group and possible days worked, the effect of the recession on any employment was significant (p=0.002), with 79.0% of study participants who had no exposure to the recession becoming employed, compared to only 60.8% of those fully exposed to the recession. There was also a significant difference in time-to-employment by recession exposure, with a median of 70 days for those with no recession exposure and 122 days for those fully exposed (p<0.001) – representing a difference of nearly two months (52 days). Employment outcomes by recession exposure group are presented in Table 2, while Figure 4 depicts the probability of remaining unemployed across the three recession exposure groups. There were no significant main recession effects on employment rate or maximum continuous employment.
Figure 4.
Survival Estimates for Remaining Unemployed, by Recession Exposure Group
Intervention Effect Modification Results
We also explored whether recession exposure modified the intervention effect on employment outcomes. Accounting for the number of days in the study, both group and recession were jointly significant predictors of any employment (p=.02 and p=.002); however, there was no significant interaction effect for a group × recession exposure interaction on any employment or time-to-employment. Within the control group, a Kaplan-Meier curve estimate of the median number of days to employment was 93 days in the `no exposure' group, and 155 days in the `full exposure' recession group. Within the intervention group the median days to employment was 47 and 115 days in the `no exposure' and `full exposure' recession groups. There was no group × recession exposure interaction effects on employment rate or on the maximum period of employment. The absence of a group × recession interaction is an important finding, indicating that even while in the midst of an economic recession; the improvements in any employment and time-to-employment that occurred in the PHN intervention group were maintained.
Bivariate analyses of the associations between baseline sociodemographic and health characteristics and each of the employment outcomes are presented in Table 3. While age, education, prior TANF receipt, and functional status were significantly associated with any employment and time-to-employment (p<.05), none of the sociodemographic or health characteristics at baseline were associated with employment rate or maximum continuous employment. Among these potential modifiers, age was fairly weakly correlated with education (r = .25), prior TANF receipt (r = .25), and functional status (r = −.11) based on Spearman rank coefficients (p<.05). None of the tests for interactions between age, education, prior TANF receipt, or functional status and any employment or time-to-employment were statistically significant at the p<.05 level.
Table 3.
Bivariate Relationships between Baseline Sociodemographic and Health Characteristics and Employment Outcomes
| Characteristic | Any Employmenta | Time-to-Employmentb | Employment Ratec | Max. Continuous Employmentd |
|---|---|---|---|---|
|
| ||||
| OR(SE) | X2,Coef (SE) | Coef (SE) | Coef. (SE) | |
| Age | .95* (.013) | −.031* (.009) | .002 (006) | .913 (.706) |
| Education | ||||
| < High School/GED | Reference | Reference | Reference | Reference |
| High School/GED | 2.06* (.617) | .341* (.164) | −.005 (.105) | 13.45 (13.9 |
| Some College/ College Degree | 1.60* (.428) | .216 (.156) | .026 (.100) | 13.27 (13.3) |
| Race | ||||
| Caucasian | Reference | Reference | Reference | Reference |
| African American | .75 (.181) | −.163 (.133) | −.012 (.084) | −2.77 (11.2) |
| Other | 4.4 (4.68) | .578 (.333) | .166 (.210) | 43.5 (28.1) |
| Prior TANF Receipt | ||||
| Never | Reference | Reference | Reference | Reference |
| 1–2 Times | .54 (.174) | −.351* (.159) | −.098 (.010) | −13.6 (13.3) |
| 3–4 Times | .45* (.182) | −.523* (.220) | −.179 (.139) | −34.5 (18.4) |
| < 4 Times | .61 (.253) | .437* (.215) | −.144 (.138) | −17.7 (18.2) |
| Depression (BDI-II) | .99 (.010) | −.007 (.005) | −.003 (.004) | −.513 (.468) |
| General Health (SF-12v2) | 1.00 (.005) | .002 (.003) | .002 (.002) | .112 (.258) |
| Functional Status (SF-12v2 Composite) | 1.01* (.005) | .006* (.003) | .001 (0.002) | .014 (.243) |
| Number of Chronic Health Conditions | .96 (.051) | −.005 (.031) | .004 (.019) | 3.93 (2.60) |
| Total Number of Symptoms | .99 (.017) | .003 (.009) | .001 (.007) | .483 (0.919) |
Discussion
Our primary finding from the RCT is that employment-entry outcomes (any employment and time-to-employment), but not outcomes related to the amount or duration of employment (employment rate and maximum continuous employment), are improved for women in Welfare Transition Programs (WTPs) with chronic health conditions who receive a public health nursing (PHN) case management intervention to address their health needs when compared to women receiving standard WTP services. Theoretically, employment entry gains in the intervention group were facilitated by PHNs working to better manage chronic health conditions and decrease health-related functional limitations. As reported elsewhere (Kneipp et al., 2011), the intervention group did have a significantly greater reduction in depressive symptoms and improvement in functional status than the control group over the 9-month intervention period, suggesting that addressing health barriers in this population can facilitate employment.
Given the post-hoc nature of the effect modification analyses conducted across baseline characteristics, our findings also cautiously suggest the intervention was equally effective in improving any employment and time-to-employment in our sample regardless of age, education, prior TANF receipt, and functional status. The fact that there was no difference in intervention effectiveness among women who differed on these characteristics is somewhat surprising – particularly for functional status, given the heterogeneity of our sample on these variables of interest and our exclusion of women from the study who were either applying for disability status or who were receiving Social Security Disability Income. While it seems reasonable to think that individuals with worse health-related functional status at baseline might reap greater benefit from a PHN case management intervention than those with better functioning, there is little evidence in the health-related literature that this is generally the case. This is primarily due to a lack of RCTs that are designed to examine differential impact across functional states and the absence of subgroup analysis findings in published reports (Smith et al., 2012).
Somewhat surprisingly, the main intervention effects on employment entry-related measures (any employment and time-to-employment) appear to have been maintained in the midst of a remarkably high unemployment rate, and while there was a 19% drop in the overall sample that went to work during the study following the onset of the recession. Among study participants who did go to work after the onset of the recession, it took nearly two additional months (a median of 52 additional days) to secure employment. Although there is some evidence of a downward employment trend for TANF recipients during weaker economic times (following 2001, when unemployment peaked at approximately 5.5%) (Kwon & Meyer, 2011), findings in this area are quite limited, with no comparable findings that have been reported in the TANF population during the current recession that we are aware of. Nonetheless, the lack of a significant group × recession exposure interaction should, as a post-hoc subgroup finding, be interpreted cautiously (Assmann et al., 2000).
To the extent that employment rate and maximum continuous employment capture dimensions of employment that are more consistent with the amount and duration of employment, the absence of intervention or recession effects on these measures suggests more research is needed to understand what factors promote long-term employment, advancement, and ultimately sustained self-sufficiency for this population. As the bulk of findings demonstrate, the jobs women receiving TANF are able to acquire are often short-lived. Regardless of health or other barriers to work, 19–22% return to TANF within one year, and 25–30% return within two years (Fagnoni, 2002; Loprest, 1999b; Loprest & Acs, 1996). Why these employment outcomes did not differ by recession exposure may have been explained by factors that were unaccounted for in the current study, such as the types of jobs; the social/interpersonal, administrative, or quality-related characteristics of jobs; or other competing personal/family demands that explain the relatively short-lived job tenure observed in this group, regardless of labor market strength and stability (Acs & Loprest, 2007).
There are study limitations that must be noted. First, the intervention-related results may not be generalizable to WTPs that already address chronic health conditions in their population, although comprehensive reports of WTPs nationwide suggest these are markedly few (U.S. Government Accountability Office, 2004). Our findings are also limited to TANF populations that are comprised predominantly of Caucasian and African American women. In addition, we could not account for all possible confounders related to the onset of the recession – some of which may be relevant to our findings – such as variability in the type of jobs impacted in local areas, and how this might intersect with the types of jobs women leaving TANF are likely to obtain.
Finally, there are clear policy implications that stem from our results. Our findings parallel those of Morgenstern and colleagues (2009), who demonstrated providing intensive case management services for TANF participants with substance use barriers improves abstinence rates and employment outcomes. However, most state welfare programs are not prepared to implement health-related interventions, as they do not typically have staff with the expertise needed to appropriately screen applicants for mental or physical health problems, or address them if identified. While it is common practice for welfare programs to indicate they `screen' for mental or physical barriers to employment simply by asking recipients about whether they have a history of either (Fagnoni, 2001b), studies of welfare implementation reveal that case managers, faced with limited time and resources, avoid asking recipients about mental health or other problems that would complicate case planning (Lurie & Riccucci, 2003; Robles et al., 2003). Thus, most recipients are simply assigned to work activities, regardless of whether they are capable of fulfilling them for any extended period of time. This model of providing services to women with barriers to employment is potentially harmful at a time when TANF recipients lose a portion of their income benefits for failing to comply with WTP work requirements. To help women in WTPs meet self-sufficiency goals, evidence-based interventions such as this can begin to alleviate some of the barriers to employment that exist. To improve long-term outcomes for this group and reduce future, or `repeat', entry into the TANF system due to health barriers, however, additional research that builds on the findings from this and other studies continues to be needed.
Reports employment findings from the first RCT designed to reduce chronic health condition-related barriers to employment for women receiving welfare in the U.S.
Over 73% of women who received public health nursing case management entered employment compared to only 64.4% of other women receiving TANF.
Public health nursing case management resulted in women entering employment 35 days earlier than other women receiving TANF.
Intervention efficacy on employment-entry outcomes was similar regardless of age, education level, prior TANF receipt, or functional status at study entry.
Public health nursing case management improves employment-entry outcomes for women leaving TANF – regardless of recession exposure.
Acknowledgements
The authors disclosed receipt of the following financial support for the research and/or authorship of this article: The first author received a grant from the National Institutes of Health and the National Institute of Nursing Research (NIH/NINR Grant # 5R01NR009406), which funded the research. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or the NINR.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acs G, Loprest P. TANF Caseload Composition and Leavers Synthesis Report Report submitted to the U.S. Department of Health and Human Services, Administration for Children and Families, Office of Planning, Research, and Evaluation. The Urban Institute; Washington, D.C.: 2007. [Google Scholar]
- Assmann SF, Pocock SJ, Enos LE, Kasten LE. Subgroup analysis and other (mis)uses of baseline data in clinical trials. The Lancet. 2000;355:1064–1049. doi: 10.1016/S0140-6736(00)02039-0. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II Manual. The Psychological Corporation, Harcourt Brace & Company; San Antonio: 1996. p. 38. [Google Scholar]
- Burtless GT. Welfare recipients' job skills and employment prospects. The Future of Children. 1997;7:39–51. [PubMed] [Google Scholar]
- Cancian M, Haveman R, Meyer DR, Wolfe B. Before and After TANF: The Economic Well-Being of Women Leaving Welfare. Institute for Research on Poverty; Madison, Wisconsin: 2000. [Google Scholar]
- Cao J. Welfare Recipiency and Welfare Recidivism: An Analysis of the NLSY Data. Institute for Research on Poverty; Madison, WI: 1996. [Google Scholar]
- Charles KK, Decicca P. Local labor market fluctuations and health: is there a connection and for whom? Journal of Health Economics. 2008;27(6):1532–1550. doi: 10.1016/j.jhealeco.2008.06.004. doi: 10.1016/j.jhealeco.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Corcoran M, Chen J. Temporary employment and welfare-to-work Program on Poverty and Social Welfare Policy, University of Michigan. Ann Arbor, MI: 2004. [Google Scholar]
- Danziger S, Corcoran M, Heflin C, Kalil A, Levine J, Rosen D, Seefeldt K, Siefert K, Tolman R. Barriers to the Employment of Welfare Recipients. Vol. 02–508. Population Studies Center at the Institute for Social Research, University of Michigan; Ann Arbor, MI: 2002. [Google Scholar]
- Danziger SK, Seefeldt KS. Barriers to employment and the 'hard to serve': Implications for services, sanctions and time limits. Social Policy & Society. 2003;2(2):151–160. [Google Scholar]
- Davalos ME, French MT. This recession is wearing me out! Health-related quality of life and economic downturns. Journal of Mental Health Policy & Economics. 2011;14(2):61–72. [PubMed] [Google Scholar]
- Dooley D, Catalano R. Why the economy predicts help-seeking: a test of competing explanations. Journal of Health & Social Behavior. 1984;25(2):160–176. [PubMed] [Google Scholar]
- Dooley D, Catalano R, Jackson R, Brownell A. Economic, life, and symptom changes in a nonmetropolitan community. Journal of Health & Social Behavior. 1981;22(2):144–154. [PubMed] [Google Scholar]
- Fagnoni C. Data Available to Assess TANF's Progress. United States General Accounting Office; Washington, D.C.: 2001a. [Google Scholar]
- Fagnoni C. Welfare Reform: More Coordinated Federal Effort Could Help States and Localities Move TANF Recipients with Impairments Toward Employment. United States General Accounting Office; Washington, DC: 2001b. [Google Scholar]
- Fagnoni C. Welfare Reform Outcomes for TANF Recipients with Impairments. United States General Accounting Office; Washington, DC: 2002. p. 32. [Google Scholar]
- Hoynes HW. Local labor markets and welfare spells: Do demand conditions matter? The Review of Economics and Statistics. 2000;82(3):351–368. [Google Scholar]
- Jones-DeWeever A, Peterson J, Song X. Before and After Welfare Reform: The Work and Well-Being of Low-Income Single Parent Families. Institute for Women's Policy Research; Washington, D.C.: 2003. [Google Scholar]
- Kneipp SM, Kairalla J, Lutz BJ, Pereira DB, Hall A, Flocks J, Beeber L, Schwartz T. Effectiveness of Public Health Nursing Case-Management on the Health of Women Receiving Temporary Assistance for Needy Families: Findings from a Randomized Controlled Trial using Community Based Participatory Research. American Journal of Public Health. 2011;101(9):1759–1768. doi: 10.2105/AJPH.2011.300210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. International Journal of Epidemiology. 2012;41(2):514–520. doi: 10.1093/ije/dyr218. doi: 10.1093/ije/dyr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon HC, Meyer DR. How do economic downturns affect welfare leavers? A comparison of two cohorts. Children and Youth Services Review. 2011;33(5):588–597. [Google Scholar]
- Lee K, Shields KK. Decision-making in hard times: What is a recession, why do we are and how do we know when we are in one? North American Journal of Economics and Finance. 2011;22:43–60. [Google Scholar]
- Long JS. Regression Models for Categorical and Limited Dependent Variables. Sage Publications; Thousand Oaks, CA: 1997. [Google Scholar]
- Loprest P. Families Who Left Welfare: Who are They and How Are They Doing? The Urban Institute; Washington, DC: 1999a. [Google Scholar]
- Loprest P. How Families That Left Welfare Are Doing: A National Picture. The Urban Institute; Washington, D.C.: 1999b. [Google Scholar]
- Loprest P, Acs G. Profile of Disability Among Families on AFDC. The Urban Institute; Washington, D.C.: 1996. [Google Scholar]
- Loprest P, Maag E. Disabilities Among TANF Recipients: Evidence from the NHIS Report Prepared for the U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. The Urban Institute; Washington, D. C.: 2009. [Google Scholar]
- Loprest P, Zedlewski S. The Changing Role of Welfare in the Lives of Low-Income Families with Children. The Urban Institute; Washington, D.C.: 2006. [Google Scholar]
- Lurie I, Riccucci N. Changing the `culture' of welfare offices: From vision to the front lines. Administration & Society. 2003;34:653–677. [Google Scholar]
- Lutz BJ, Kneipp S, Means D. Developing a health screening questionnaire for women in welfare transition programs in the United States. Qualitative Health Research. 2009;19:105–115. doi: 10.1177/1049732308327347. doi: 10.1177/1049732308327347. [DOI] [PubMed] [Google Scholar]
- Minkler M, Wallerstein N. Community Based Participatory Research for Health. Jossey-Bass; San Francisco: 2003. [Google Scholar]
- Moffitt R. The role of non-financial factors in exit and entry in the TANF program Welfare, Children, and Families: A Three-City Study. Johns Hopkins University; 2003. [Google Scholar]
- Morgenstern J, Neighbors CJ, Kuerbis A, Riordan A, Blanchard KA, McVeigh KH, Morgan TJ, McCrady B. Improving 24-month abstinence and employment outcomes for substance-dependent women receiving temporary assistance for needy families with intensive case management. American Journal of Public Health. 2009;99:328–333. doi: 10.2105/AJPH.2007.133553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics . 2002 National Health Interview Survey (NHIS) Public Use Data Release Survey Description. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Hyattsville, MD: 2003. [Google Scholar]
- Peduzzi P, Henderson W, Hartigan P, Lavori P. Analysis of randomized controlled trials. Epidemiology Reviews. 2002;24(1):26–38. doi: 10.1093/epirev/24.1.26. [DOI] [PubMed] [Google Scholar]
- Piantadosi S. Clinical Trials: A Methodologic Perspective. 2nd ed. John Wiley &Sons, Inc.; Hoboken, New Jersey: 2005. [Google Scholar]
- Polit DF, London AS, Martinez JM. The Health of Poor Urban Women: Findings from the Project on Devolution and Urban Change. Manpower Demonstration Research Corporation; New York: 2001. [Google Scholar]
- Polit DF, Widom R, Edin K, Bowie S, London AS, Scott EK. Is Work Enough? The Experiences of Current and Former Welfare Mothers. Manpower Demonstration Research Corporation; New York: 2001. [Google Scholar]
- Rampell C. December 2007: The Date the Recession (Officially) Began, The New York Times. 2008 Retrieved from http://economix.blogs.nytimes.com/2008/12/01/december-2007-the-date-the-recession-officially-began/
- Robles A, Doolittle F, Gooden S. Community Service Jobs in Wisconsin Works: The Milwaukee County Experience. Manpower Research Demonstration Corporation; New York: 2003. [Google Scholar]
- Ruhm CJ. Are recessions good for your health? Quarterly Journal of Economics. 2000;115:617–650. [Google Scholar]
- Ruhm CJ. Economic Expansions are Unhealthy: Evidence from Microdata. National Bureau of Economic Research; Cambridge, MA: 2001. [Google Scholar]
- Ruhm CJ. Healthy living in hard times. Journal of Health Economics. 2005;24:341–363. doi: 10.1016/j.jhealeco.2004.09.007. [DOI] [PubMed] [Google Scholar]
- Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. Trials. 2010;11(32):1–8. doi: 10.4103/0976-500X.72352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear MK, Greeno C, Kang J, Ludewig D, Frank E, Swartz HA, Hanekamp M. Diagnosis of nonpsychotic patients in community clinics. Am J Psychiatry. 2000;157(Journal Article):581–587. doi: 10.1176/appi.ajp.157.4.581. [DOI] [PubMed] [Google Scholar]
- Smith SM, Soubhi H, Fortin M, Hudon C, O'Dowd T. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Systematic Reviews. 2012;4:CD006560. doi: 10.1002/14651858.CD006560.pub2. doi: 10.1002/14651858.CD006560.pub2. [DOI] [PubMed] [Google Scholar]
- Suhrcke M, Stuckler D. Will the recession be bad for our health? It depends. Soc Sci Med. 2012;74(5):647–653. doi: 10.1016/j.socscimed.2011.12.011. doi: 10.1016/j.socscimed.2011.12.011. [DOI] [PubMed] [Google Scholar]
- Sum A, Khatiwada I. Labor Underutilization Problems of U.S. Workers Across Household Income Groups at the End of the Great Recession: A Truly Great Depression Among the Nation's Low Income Workers Amidst Full Employment Among the Most Affluent. Northeastern University, Center for Labor Market Studies; Boston, MA: 2010. [Google Scholar]
- U. S. Department of Labor . Local Area Unemployment Statistics: Bureau of Labor Statistics. 2011. [Google Scholar]
- U.S. Department of Health and Human Services . TANF Caseload Data - Number of Families and Recipients - 2007, 2008, 2009, 2010. Administration for Children & Families; Washington, D.C.: 2011. [Google Scholar]
- U.S. Government Accountability Office . TANF and SSI: Opportunities Exist to Help People with Impairments Become Self-Sufficient. Washington, DC: 2004. [Google Scholar]
- Personal Responsibility and Work Opportunity Reconciliation Act 1996.
- Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM. Statistics in medicine--reporting of subgroup analyses in clinical trials. New England Journal of Medicine. 2007;357(21):2189–2194. doi: 10.1056/NEJMsr077003. doi: 10.1056/NEJMsr077003. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. How to Score Version 2 of the SF-12 Health Survey. Quality Metric Incorporated; Lincoln, Rhode Island: 2005. [Google Scholar]
- Zedlewski S. Work-Related Activities and Limitations of Current Welfare Recipients. The Urban Institute; Washington, DC: 1999. [Google Scholar]
- Zedlewski SR. Work Activity and Obstacles to Work Among TANF Recipients. The Urban Institute; Washington, DC: 1999. [Google Scholar]
- Ziliak JP. Social policy and the macro-economy: What drives welfare caseloads in the US? Social Policy & Society. 2002;2(2):133–142. [Google Scholar]
- Zivin K, Paczkowski M, Galea S. Economic downturns and population mental health: research findings, gaps, challenges and priorities. Psychological Medicine. 2011;41(7):1343–1348. doi: 10.1017/S003329171000173X. doi: 10.1017/S003329171000173X. [DOI] [PMC free article] [PubMed] [Google Scholar]