Abstract
The evidence base for cognitive behavioral therapy (CBT) to treat child emotional and behavioral symptoms following exposure to trauma in youth is compelling, but relatively few studies are available on preschool children and on moderators of treatment outcomes. This paper examines maternal and child characteristics as moderators of posttraumatic stress (PTS) treatment outcomes in preschool children. Outcome data from a previously published randomized trial in three to six year old preschool children with diagnostic interview data from participating mothers were used. Hypotheses were tested via hierarchical linear modeling. Maternal depression was associated with higher initial child posttraumatic stress disorder (PTSD) symptoms, and was associated with increasing PTSD symptom trends at follow up suggesting potential child PTSD symptom relapse. Maternal PTSD symptoms similarly predicted differential child separation anxiety symptom change but not child PTSD symptom change. Targeting dyads with child PTSD symptoms and maternal depression or PTSD symptoms with enhanced interventions may be a useful strategy to improve treatment maintenance.
Keywords: moderators of outcome, posttraumatic stress, cognitive behavioral therapy, children
1. Introduction
Research suggests that exposure to traumatic experiences can trigger a number of negative outcomes in youth and children (Carrión, Weems, Ray & Reiss, 2002; Carrión, Weems, & Reiss, 2007; Scheeringa, Zeanah, Myers, & Putnam, 2003). Research also indicates that these are evident even in very young children such that three to six year olds may experience posttraumatic stress (PTS) including the emotional and behavioral problems associated with the diagnosis of posttraumatic stress disorder (PTSD; Scheeringa et al., 2003). These symptoms include negative re-experiencing, avoidance, emotional numbing and hyper-arousal (APA, 1994). Fortunately, cognitive-behavioral therapy (CBT) for PTS in youth has been shown to be efficacious (Silverman et al., 2008). However, only three randomized trials have examined CBT for PTS young children (Cohen & Mannarino, 1996a; Deblinger, Stauffer, & Steer, 2001; Scheeringa, Weems, Cohen, Amaya-Jackson, & Guthrie, 2011) and results suggest feasibility and efficacy in preschool (e.g., 3 to 6 years) children (i.e., results suggest reduction in rates of the diagnosis of PTSD, reduction of PTSD symptoms, and comorbid symptoms).
In a review and meta-analysis of the child and adolescent PTS treatment literature, Silverman et al. (2008) noted that while CBT treatments appeared generally efficacious many youth are still symptomatic and very little work has been done examining potential moderators and predictors of treatment outcome. Indeed individual level CBT treatment data suggests wide variability in youth PTSD symptom change (Taylor & Weems, 2011). Kazdin (2003) defines an intervention moderator as a “characteristic that influences the direction or magnitude of the relation between the intervention and outcome” (p. 3) implying differential symptom change as a function of putative moderators. The Silverman et al. (2008) review highlights the importance of examining the role of parent characteristics in differential outcomes. Indeed, the results of their meta-analysis showed that including parents in the children’s treatment did appear to enhance child anxiety and depressive symptom outcomes but did not appear to enhance child PTSD symptom outcomes.
Cohen and Mannarino (1996b; 2000) have examined predictors of child PTS outcomes and indicated that the Parent Emotional Reaction Questionnaire was a strong familial predictor of treatment outcome at post treatment (Cohen & Mannarino, 1996b). Given the limited data on moderators of outcomes in youth with PTS, drawing more broadly from the child anxiety treatment literature provides additional support for the importance of maternal characteristics. Berman et al. (2000) examined predictors of treatment outcomes of exposure based CBT with data from two outcome studies for childhood anxiety disorders (specific phobias, generalized, social and separation anxiety disorders, Silverman et al., 1999a, 1999b). Parents’ self-ratings of depression at pre-treatment were associated with treatment failure, defined as not having ‘recovered’ (i.e. no longer meeting criteria for the DSM diagnostic criteria for the primary and targeted phobic or anxiety disorder)”. Children’s comorbid diagnoses of depression, and depressive symptoms, as well as trait anxiety at pre-treatment were also associated with treatment failure. Age, income, and primary anxiety diagnosis were not predictors of success or failure in therapy.
Southam-Gerow, Kendall, and Weersing (2001) also examined child and parent predictors of poor response in CBT treatment outcomes (i.e., not meeting criteria for any anxiety disorder versus still meets criteria for one anxiety disorder immediately after treatment or at 1 year follow up). Older age was associated with poor treatment response immediately following treatment and maternal depression was associated with poor response at 1 year follow up. Ethnicity, gender, family income, and a measure of therapeutic relationship were not associated with treatment outcome. It is important to note that none of these studies formally examined differential symptom change as a function of putative moderators (i.e., the studies either simply tested predictors of post assessment or follow up scores (i.e., Cohen & Mannarino, 1996b; 2000) or compared those who did well versus those who did relatively poorly (i.e., Berman et al., 2000; Southam-Gerow et al., 2001).
The purpose of this study was to expand the childhood PTS treatment literature by examining maternal and child characteristics as moderators of PTS outcomes using data from a previously published randomized trial (Scheeringa et al., 2011). Scheeringa et al. (2011) randomly assigned 64 youth to either 12-session manualized CBT or 12-weeks wait list. In the randomized design the intervention group improved significantly more on symptoms of PTSD. After the waiting period, all participants were offered treatment. Effect sizes were large for PTSD symptoms and were maintained at a six-month follow up. Overall, findings suggested that CBT was feasible with preschool children and effective for treating PTS. Drawing from the extant literature, we predicted that maternal depression may negatively affect PTS outcomes.
The extant research suggests maternal depression may impede treatment and/or treatment maintenance in child internalizing interventions (Berman et al., 2000; Southam-Gerow et al., 2001). Similar findings exist in the disruptive behavior disorders treatment literature as well (Chronis, Gamble, Roberts, & Pelham, 2006; Owens et al., 2003). Theoretically, offspring of depressed parents are at increased risk for developing anxiety disorders (see Colletti et al., 2009) and depressed mothers may have difficulty fostering the therapeutic process of maintaining treatment gains. Scheeringa and Zeanah (2001) have proposed theoretical models of the parent-child relationship to guide future research. In their moderating effect model, the caregivers’ relationships with their children affect the strength of the relations between the traumatic events and the children’s symptomatic responses. Maternal depression may therefore affect this relationship (Colletti et al., 2009) and create a context of prolonged treatment-resistant PTSD in offspring (see also Pat-Horenczyk, Rabinowitz, Rice, & Tucker-Levin, 2009).
We also test whether maternal PTSD symptoms moderate outcomes similar to those of maternal depression as there is evidence to suggest maternal PTSD symptoms are predictive of child outcomes in longitudinal research (Laor, Wolmer, Mayes, & Gershon, 1997). Child comorbid depression and separation anxiety symptoms were also tested as moderators given the findings of Berman et al (2000). Finally, we explored age, gender, and minority status, but did not expect effects based on past research. Hypotheses were tested via hierarchical linear modeling (HLM; Byrk & Raudenbush, 1987; 1992). HLM analyses are ideally suited for formally testing moderators of treatment outcomes (differential symptom change) across pretreatment to follow up where sharp declines are expected from pre-to post treatment followed by smaller decreases or leveling off from post treatment to follow up (i.e., a curvilinear trajectory). HLM provides an efficient approach to modeling complex trends in individual outcome over time (as well as the effects of between subjects variables), including the curvilinear relations expected (Tate & Hokason, 1993) and so would provide a methodological advance to the extant literature by modeling the expected growth curves and formally testing maternal and child characteristics as moderators of these curves. HLM has the additional advantage for use with missing data common in treatment studies that are problematic for conventional repeated measures techniques (ANOVA’s) for the participants across all three measurement points (pre, post, six-month follow-up).
2. Method
2.1 Participants and Procedures
Data are from a randomized trial reported in Scheeringa et al. (2011) where additional details can be found. Briefly, inclusion criteria were (1) experienced a life-threatening traumatic event. (2) Age between 36 and 83 months at the time of the most recent trauma and at the time of enrollment. (3) Four or more PTSD symptoms with at least one of them being a re-experiencing symptom from criterion B or an avoidance symptom from criterion C. A re-experiencing or avoidance symptom was required for the exposure exercises to be salient in CBT for trauma (i.e., all participants either met DSM-IV or the alternative preschool criteria algorithm; see Scheeringa et al., 2003; Scheeringa, Zeanah, & Cohen, 2011). Exclusion criteria: (1) Head trauma with Glascow Coma Scale score of 7 or less in the emergency room. (2) Mental retardation, autistic disorder, blindness, deafness, and foreign language speaking families. Participants were recruited for three main types of trauma exposure (acute, chronic, disaster). For example, children who suffered acute single blow trauma victims were mainly recruited from a Level I Trauma Center. Children who suffered chronic repeated events were recruited through the three main battered women’s programs in the New Orleans metropolitan area. The staff at these programs gave the mothers our phone number. Children who were victims of the Hurricane Katrina disaster were recruited primarily through newspaper ads. After it was known that children met the inclusion and exclusion criteria from being evaluated in the assessment study, then caregivers were approached about participation in this treatment study.
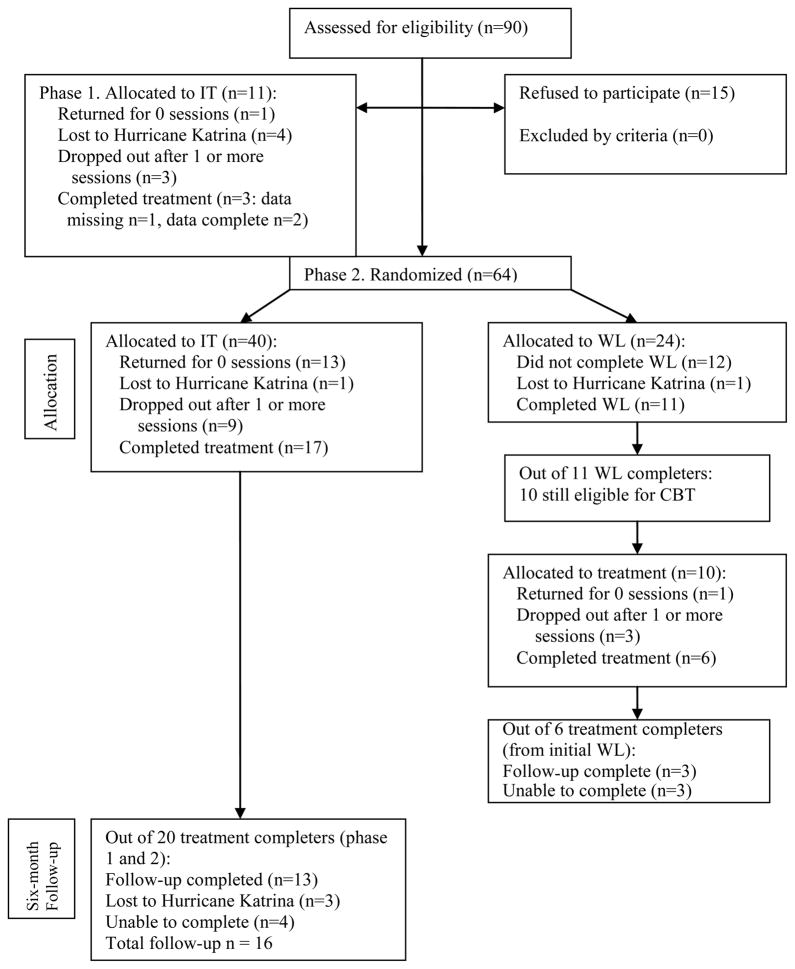
Eight-five participants were approached through this process. An additional five participants were enrolled by word of mouth outside of this process, giving a total of 90 participants assessed for eligibility and approached. Fifteen caregivers refused. CONSORT Flow Diagram (Altman et al., 2001) is in Appendix 1. Children’s mean age was 5.3 years (SD 1.1), 66.2% male, 59.5% Black/African-American, 35.1% White and 5.4% Other race. Maternal caregivers mean age was 34.8 years (SD 9.7) on average with 13.5 years (SD 2.7) of education.
Appendix 1.
Flow chart of group assignment, attrition, treatment completers, and six-month follow-up assessment.
Note: IT = immediate treatment, WL = wait list
2.2 Measures
The Preschool Age Psychiatric Assessment (PAPA) (Egger et al., 2006) is a semi-structured psychiatric interview with the caregiver about the child. Modules administered for this study were PTSD, major depressive disorder (MDD), separation anxiety disorder (SAD), oppositional defiant disorder (ODD), and attention-deficit/hyperactivity disorder (ADHD). The PAPA instrument has been the focus of a number of preschool PTSD validity studies (e.g., Scheeringa et al., 1995, 2003; 2011) and published test-retest reliability kappas are .73 for PTSD, .72 MDD, .60 for SAD, .57 for ODD, and .74 for ADHD. The PTSD module included developmental modifications to wording of A2 acute reaction, B1 intrusive recollections, B2 nightmares, B3 dissociative experiences, C5 detachment or estrangement, and D2 irritability based on prior empirical work (Scheeringa et al., 2003). Interviewers received extensive training prior to their first live interviews and then throughout the study the principal investigator met individually with interviewers weekly to watch their most symptomatic interviews on videotape in order to prevent drift, critique technique, and correct coding errors. Of the treatment completers, the children at pre-treatment had means of 8.0 (SD = 2.8) PTSD symptoms, 3.0 (SD = 2.2) depressive symptoms, 2.5 (SD = 1.8) SAD symptoms, 4.3 (SD = 2.5) ODD symptoms, and 7.8 (SD = 5.2) ADHD symptoms; all indicative of markedly symptomatic individuals except perhaps in respect to depression.
Parent Depression and PTSD symptoms were measured with the NIMH-Diagnostic Interview Schedule (DIS) (Robins, Cottler, Bucholz, & Compton, 1995) modules for major depression and PTSD. There exists a large body of psychometric validation data for the DIS. The mean interrater reliability kappa for over 20 diagnoses was .69, ranging from .40 for panic disorder to 1.0 for anorexia nervosa. Using the clinician’s rating as the standard, the mean sensitivity of lay interviews for making diagnoses was 75% and mean specificity was 94% (Robins, Helzer, Croughan, & Radcliff, 1981). Caregivers had a mean of 4.2 depression symptoms (SD = 3.4), and 50% of caregivers had five or more symptoms (out of a possible nine symptoms), which is consistent with a diagnosis of major depressive disorder (APA, 2000). High maternal depression in this sample therefore reflects a clinically severe level of symptoms. Caregivers had a mean of 9.3 PTSD symptoms (SD = 4.8) (out of a possible 17 symptoms), also reflective of highly symptomatic individuals.
2.3 Procedures and Data Analysis
This study was approved by the Tulane University Institutional Review Board. After being screened for inclusion and exclusion criteria over the phone, caregivers arrived alone at the lab and informed consents obtained. Participants were monetarily compensated for their participation in the assessments but not for the treatment. As noted, youth were initially randomly assigned to either immediate12-session manualized CBT or a 12-weeks wait list. After the waiting period, all participants in the wait list were offered treatment. In total, data were available on 25 participants who completed treatment and 16 assessed for six-month follow up. There were no differences between those located and not located on the post-treatment number of PTSD, MDD, SAD, ODD, or ADHD symptoms, child age, child sex, mothers’ levels of depression symptoms, PTSD symptoms, age, or level of schooling. However, minority families were more likely to drop out than non-minorities [X2 (1) = 8.73, p < .01]. Minority status was examined as a potential moderator of outcomes.
As noted, hypotheses were tested via trend analyses using HLM (Byrk & Raudenbush, 1987, 1992). In the first stage of the analysis, HLM was used to estimate the within subject change (random effects, level 1) to test the appropriateness of quadratic (curvilinear) trends expected for pre- to post-treatment with follow up (i.e., the expected sharp declines from pre-to post treatment followed by smaller decreases from post treatment to follow up) versus simple linear trends. The second stage HLM analyses were used to test the potential moderators of these trends (fixed effects, level 2) on the within-subject slopes for PTSD symptom levels across the three measurement points (pre-treatment, post-treatment, and follow up). The linear values [i.e., Times 1 (pre), 2 (post) and 3 (six-month follow-up)] were squared to create the quadratic curvilinear trend similar to previous research and as suggested by Byrk and Raudenbush (1992). Given the sample size and high degree of association among potential moderators (e.g., maternal depression and PTSD symptoms) analyses initially tested potential moderators in separate analyses. Incremental prediction was then tested for significant effects. We tested potential moderators on the PTSD, MDD, SAD, ODD, and ADHD symptom trends.
3. Results
Level 1 HLM analyses tested linear and curvilinear trends in the individual growth curves using restricted maximum likelihood estimation with robust standard errors. The results of the HLM analysis of the overall within subject change curves indicated significant linear [t(34) = −4.01, p<.05] and quadratic [t(34) = 2.73, p<.05] components [overall X2 (55) = 104.57, p < .001] for PTSD symptoms (and SAD symptoms see below). The significant curvilinear pattern is consistent with the anticipated large declines from pre-to post treatment followed by smaller decreases from post-treatment to follow up.
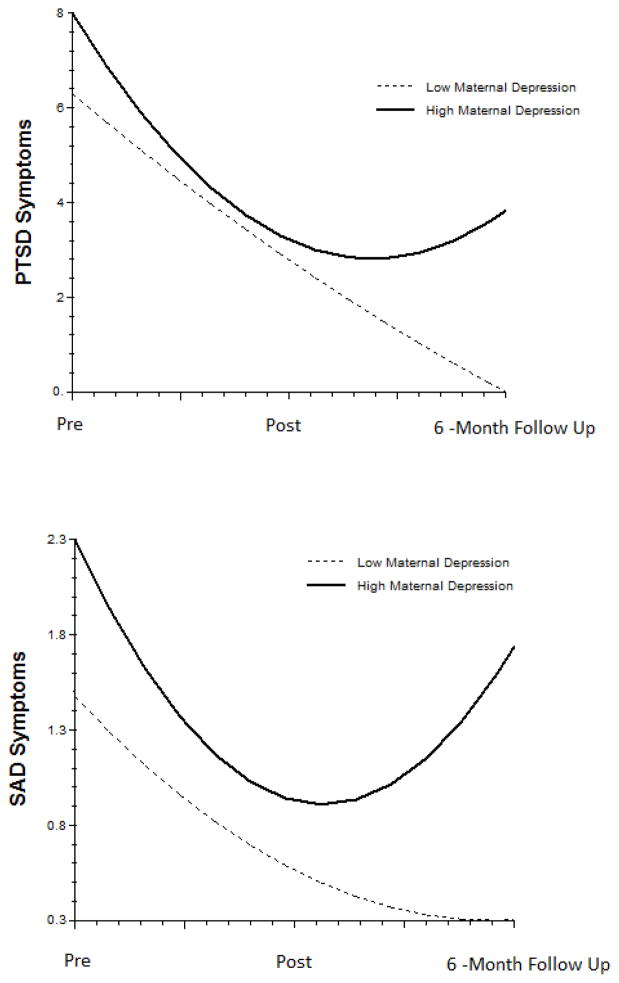
Level 2 analyses indicated that there were no significant effects of age, minority status, or gender on the linear or curvilinear effects. The results of the HLM analyses on the effect of maternal depression are presented in Table 1 and depicted visually in Figure 1. As shown in Table 1, high maternal depression was associated with greater initial PTSD symptoms (p < .05). Also, results indicated a significant effect of maternal depression (p < .05) for the quadratic trend, indicating that there was a significant difference in the individual change curves in PTSD symptoms depending on level of maternal depression. As can be seen from Figure 1 the trend shows a steeper initial decrease followed by a return to increased PTSD symptoms for children with high (highest quartile in the sample) maternal depression. The effects of maternal depression on change in ADHD, ODD or child depression outcomes were not significant; however, separation anxiety was significant applying a one tailed test [intercept t (54) = 1.90, p < .05 one tailed; and quadratic t (33) = 1.88, p <.05 one tailed; model X2 (54) = 135.72, p < .001]. As can be seen from Figure 1 the trend shows higher initial SAD symptoms, then an initial decrease followed by a return to increased SAD symptoms for children with high maternal depression.
Table 1.
HLM Estimation of the Influence of Maternal depression on Treatment Maintenance of PTSD Symptoms
| Fixed Effect | Coefficient | Standard Error | t | df | p |
|---|---|---|---|---|---|
| Intercept | 14.50 | 1.60 | 9.08 | 53 | <0.001 |
| Maternal depression | 1.25 | 0.49 | 2.57 | 53 | 0.013 |
| For Linear slope | |||||
| Intercept | −8.81 | 1.93 | −4.56 | 32 | <0.001 |
| Maternal depression | −1.36 | 0.59 | −2.32 | 32 | 0.027 |
| For Curvilinear slope | |||||
| Intercept | 1.59 | 0.47 | 3.41 | 32 | 0.002 |
| Maternal depression | 0.38 | 0.14 | 2.72 | 32 | 0.011 |
Note: model random effects X2(53) = 101.03, p < 0.001
Figure 1.
Growth Curves Depicting the Influence of Maternal Depression on Treatment Maintenance of Child PTSD and SAD Symptoms
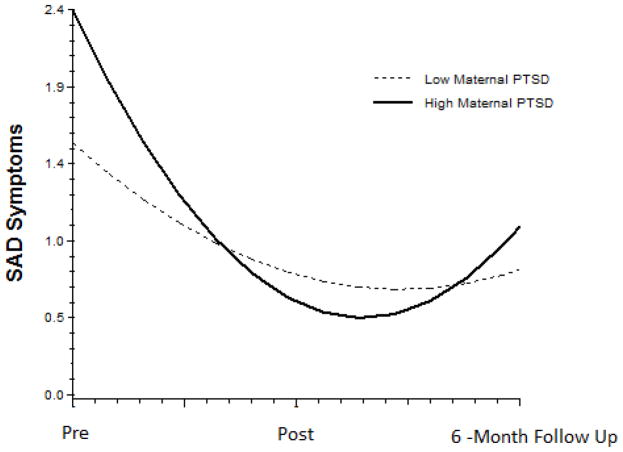
The effect of maternal PTSD symptoms on change in child PTSD symptoms were not significant [linear and quadratic p’s > .1; the relation of maternal PTSD symptoms on Child PTSD symptoms intercept was significant applying a one tailed test; intercept t (54) = 1.74, p < .05 one tailed]. The effect maternal PTSD on change in child separation anxiety was significant [intercept t (54) = 3.67, p < .01; and quadratic t (32) = 3.04, p <.01; model X2 (54) = 177.93, p < .001]. As can be seen from Figure 2 the trend shows higher initial SAD symptoms, then an initial decrease followed by a return to increased SAD symptoms for children with high maternal PTSD. When maternal depression was also included in the model the effect of maternal PTSD on child SAD symptom trajectories remained significant [quadratic t (30) = 2.51, p < .05] while the effect of maternal depression was not evident [quadratic t (30) = 0.43, p >.1; overall model X2 (53) = 182.10, p < .001]. Maternal PTSD symptoms did not have a statistically significant effect on any other child outcomes (all p’s greater than .1).
Figure 2.
Growth Curves Depicting the Influence of Maternal PTSD on Treatment Maintenance of Child SAD Symptoms
Child SAD symptoms did show a significant effect on child PTSD symptom outcomes [intercept t (58) = 2.72, p < .01 two tailed; and quadratic t (36) = 2.22, p <.05 two tailed; model X2(58) = 100.00, p < .001]. However, when maternal depression was also included in the model the effect of child SAD on child PTSD symptoms trajectories was not evident [quadratic t (30) = 1.08, p >.1] while the effect of maternal depression remained significant [quadratic t (30) = 2.34, p <.05 two tailed; overall model X2(54) = 92.68, p < .001].
4. Discussion
The findings in this add to the existing understanding of interventions for PTS in young children. While maternal depression did not appear to have a negative effect on initial treatment gains, maternal depression did appear to be associated with greater initial PTSD symptoms and potential child PTSD symptom relapse with similar but less statistically robust findings on child SAD symptom outcomes. These findings are consistent with the extant literature indicating maternal factors generally (Cohen & Mannarino, 1996; 2000) and more specifically maternal depression as a consistent predictor of poorer child outcomes in treatment for anxiety disorders (Berman et al. 2000; Southam-Gerow et al., 2001). Given the relative consistency of maternal depression as a predictor, targeting maternal depression in a family-based CBT when treating PTS in youth (or otherwise making strong referrals for maternal treatment) may enhance treatment maintenance (see Pat-Horenczyk et al., 2009; see Chronis et al., 2006 for similar work with ADHD). The pattern of findings may stem in part from a shared genetic susceptibility to depression and anxiety problems in parent child dyads. That is, poorer child long-term PTS outcomes may be due to shared heritable risk factors rather than to an indirect effect of maternal depression through the parent-child relationship. Child SAD symptoms did show a significant effect on predicting child PTSD symptom outcomes but, when maternal depression was also included in the model the effect of child SAD symptoms on child PTSD symptom trajectories was not evident. It appears that the relatively strong association between maternal depression and child SAD in the sample may account for this finding (see Figure 1).
Interestingly, maternal PTSD symptoms did not moderate child PTSD outcomes but did moderate SAD outcomes. This finding may be considered in light of the longitudinal research on maternal and child PTS. For example, elevated parental PTSD symptoms have been found to correlate with elevated children’s PTSD symptoms 9 months after, but not 3 months after the event (Koplewicz et al., 2002). Similarly, following missile attacks in Israel, maternal intrusive PTSD symptoms positively correlated with child PTSD symptoms in 3- and 4-year-old displaced children 30 months after the attacks, but not 6 months after the attacks (Laor et al., 1997). The pattern of findings from these prospective studies inconsistently supported the notion that parents PTSD influences children’s PTSD symptoms, although it is notable that these were naturalistic follow-up studies and not treatment studies. In this study, SAD symptoms were consistently linked to maternal symptoms (i.e., change was predicted by both maternal PTSD and Depression symptoms) and so it may be that SAD symptoms are more sensitive to the maternal emotional context than child PTSD symptoms in this age group. While such a conclusion should be considered tentative as there are a number of possibilities (e.g., evolution in the expression of PTS see Weems, Saltzman, Reiss & Carrión, 2003), this interpretation is a developmentally attractive one in that separation fears tend to be pronounced earlier in childhood (Weems, 2008).
As noted, the results of the Silverman et al. (2008) meta-analysis showed that including parents in the children’s treatment did appear to enhance child anxiety and depressive symptom outcomes but did not appear to enhance child PTSD symptom outcomes. Taken together with the results in this study suggests the need to examine more subtle variation in outcome measures (De Los Reyes & Kazdin, 2006; 2008). As Kazdin (2003) has noted, identifying moderators can sometimes lead to the identification of potential treatment mechanisms. While speculative, the complex relation between child symptom outcomes and maternal symptoms in this study may be pointing out that an important mechanism of effective CBT for PTS in young children is fostering the parent child relationship and/or creating a context of positive family support.
The present study is limited by its sample size. Because the power to detect significant effects was low in this study, results of non-significant findings should be interpreted with caution. Attrition was also high in this study relative to other outcome trials (Cohen & Mannarino, 1996a; Deblinger et al., 2001; see Silverman et al., 2008). Minority families were more likely to drop out and we recruited from an urban area with a large minority population that had experienced a devastating disaster (hurricane Katrina) and so these factors may have contributed to the relatively large attrition. In addition, the study also relied on maternal caregivers’ reports. It might be the case that reports from other sources (such as fathers or observations) would result in additional information about the prediction of changes in PTS following treatment. While in very young children parents’ reports represent a main source of information making this an inherent limitation (Cohen & Mannarino, 1996a; Deblinger et al., 2001), future outcome studies might benefit from observational outcome measures. Finally, a limitation to generalizing results to other populations is that the sample included relatively more males than females and African-Americans were overrepresented in this study. While the ethnic composition might be considered a positive feature in that it extends the literature to a population that has been relatively understudied in clinical trials (Silverman et al., 2008) inference to the general population of preschool youth is less clear from this sample.
Highlights.
Tested maternal and child characteristics as moderators of posttraumatic stress treatment outcomes in preschool children.
Maternal depression was associated with increasing PTSD symptom trends at follow up suggesting child PTSD symptom relapse.
Maternal PTSD similarly predicts differential child separation anxiety symptom change.
Targeting dyads with child PTSD and maternal depression with enhanced interventions may improve treatment maintenance.
Acknowledgments
Supported by NIMH grant 5R34MH070827. The authors thank the Medical Center of Louisiana Charity Hospital Trauma Center and staff, the Metropolitan Battered Women’s Program, Crescent House, and the St. Bernard Battered Women’s Program.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen A, Saltzman WR, Brymer MJ, Oshri A, Silverman WK. An empirically informed intervention for children following exposure to severe hurricanes. The Behavior Therapist. 2006;29:118–124. [Google Scholar]
- Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, et al. The revised CONSORT statement for reporting randomized trials: Explanation and elaboration. Annals of Internal Medicine. 2001;134:663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Berman SL, Weems CF, Silverman WK, Kurtines WK. Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy. 2000;31:713–731. [Google Scholar]
- Bryk AS, Raudenbush SW. Application of hierarchical linear models to assessing change. Psychological Bulletin. 1987;101:147–158. [Google Scholar]
- Bryk A, Raudenbush SW. Hierarchical Linear Models for Social and Behavioral Research: Applications and Data Analysis Methods. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Carrión VG, Weems CF, Ray R, Reiss AL. Towards an empirical definition of pediatric PTSD: The phenomenology of PTSD symptoms in youth. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:166–173. doi: 10.1097/00004583-200202000-00010. [DOI] [PubMed] [Google Scholar]
- Carrión VG, Weems CF, Reiss AL. Stress predicts brain changes in children: A pilot longitudinal study on youth stress, PTSD, and the hippocampus. Pediatrics. 2007;119:509–516. doi: 10.1542/peds.2006-2028. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Gamble SA, Roberts JE, Pelham WE. Cognitive-behavioral depression treatment for mothers of children with Attention-Deficit/Hyperactivity Disorder. Behavior Therapy. 2006;37:143–158. doi: 10.1016/j.beth.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Cohen J, Mannarino A. A treatment outcome study for sexually abused preschool children: Initial findings. Journal of the American Academy of Child and Adolescent Psychiatry. 1996a;35:42–50. doi: 10.1097/00004583-199601000-00011. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Factors that mediate treatment outcome of sexually abused preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 1996b;35(10):1402–1410. doi: 10.1097/00004583-199610000-00028. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP. Predictors of treatment outcome in sexually abused children. Child Abuse & Neglect. 2000;24:983–994. doi: 10.1016/s0145-2134(00)00153-8. [DOI] [PubMed] [Google Scholar]
- Colletti CJM, Forehand R, Garai E, Rakow A, McKee L, Fear JM, Compas BE. Parent depression and child anxiety: An overview of the literature with clinical implications. Child Youth Care Forum. 2009;38:151–160. doi: 10.1007/s10566-009-9074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Conceptualizing changes in behavior in intervention research: The range of possible changes model. Psychological Review. 2006;113:554–583. doi: 10.1037/0033-295X.113.3.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. When the evidence says, “Yes, no, and maybe so”: Attending to and interpreting inconsistent findings among evidence-based interventions. Current Directions in Psychological Science. 2008;17:47–51. doi: 10.1111/j.1467-8721.2008.00546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deblinger E, Stauffer L, Steer R. Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their nonoffending mothers. Child Maltreatment. 2001;6:332–343. doi: 10.1177/1077559501006004006. [DOI] [PubMed] [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A. Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. In: Nolen-Hoeksema S, Cannon TD, Widiger T, editors. Annual Review of Clinical Psychology. Vol. 3. 2007. pp. 1–27. [DOI] [PubMed] [Google Scholar]
- Koplewicz H, Vogel J, Solanto M, Morrissey R, Alonso C, Abikoff H, et al. Child and parent response to the 1993 World Trade Center bombing. Journal of Traumatic Stress. 2002;15:77–85. doi: 10.1023/A:1014339513128. [DOI] [PubMed] [Google Scholar]
- Laor N, Wolmer L, Mayes LC, Gershon A. Israeli preschool children under scuds: a 30-month follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:349–356. doi: 10.1097/00004583-199703000-00013. [DOI] [PubMed] [Google Scholar]
- Owens EB, Hinshaw SP, Kraemer HC, Arnold LE, Abikoff HB, Cantwell DP, et al. What treatment for whom for ADHD: Moderators of treatment in the MTA. Journal of Consulting and Clinical Psychology. 2003;71:540–552. doi: 10.1037/0022-006x.71.3.540. [DOI] [PubMed] [Google Scholar]
- Pat-Horenczyk R, Rabinowitz R, Rice A, Tucker-Levin A. The search for risk and protective factors in childhood PTSD: From variables to processes. In: Brom D, Pat-Horenczyk R, Ford J, editors. Treating Traumatized Children: Risk, Resilience and Recovery. Routledge; 2009. pp. 51–71. [Google Scholar]
- Robins LN, Cottler LB, Bucholz KK, Compton WM. Diagnostic Interview Schedule for DSM-IV. Washington University; St Louis, Missouri: 1995. [Google Scholar]
- Robins L, Helzer JE, Croughan J, Radcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics and validity. Archives of General Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Weems CF, Cohen J, Amaya-Jackson L, Guthrie D. Trauma-focused cognitive-behavioral therapy for posttraumatic stress disorder in three through six year-old children: A randomized clinical trial. Journal of Child Psychology and Psychiatry. 2011;52:853–860. doi: 10.1111/j.1469-7610.2010.02354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH. A relational perspective on PTSD in early childhood. Journal of Traumatic Stress. 2001;14:799–815. doi: 10.1023/A:1013002507972. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Drell MJ, Larrieu JA. Two approaches to the diagnosis of posttraumatic stress disorder in infancy and early childhood. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:191–200. doi: 10.1097/00004583-199502000-00014. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Myers L, Putnam FW. New findings on alternative criteria for PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(5):561–570. doi: 10.1097/01.CHI.0000046822.95464.14. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Cohen JA. PTSD in children and adolescents: Towards an empirically based algorithm. Depression and Anxiety. 2011;28:770–782. doi: 10.1002/da.20736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southam-Gerow MA, Kendall PC, Weersing VR. Examining outcome variability: Correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology. 2001;30:422– 436. doi: 10.1207/S15374424JCCP3003_13. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Lumpkin PW, Carmichael DH. Treating anxiety disorders in children with group cognitive-behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 1999a;67:995–1003. doi: 10.1037//0022-006x.67.6.995. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Rabian B, Serafini LT. Contingency management, self-control, and education support in the treatment of childhood phobic disorders: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 1999b;67:675–687. doi: 10.1037//0022-006x.67.5.675. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Ortiz CD, Viswesvaran C, Burns BJ, Kolko DJ, Putnam FW, et al. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):156–183. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Tate RL, Hokanson JE. Analyzing individual status and change with hierarchical linear models: Illustration with depression in college students. Journal of Personality. 1993;61:181–206. doi: 10.1111/j.1467-6494.1993.tb01031.x. [DOI] [PubMed] [Google Scholar]
- Taylor LK, Weems CF. Cognitive-behavior therapy for disaster exposed youth with posttraumatic stress: Results from a multiple-baseline examination. Behavior Therapy. 2011;42:349–363. doi: 10.1016/j.beth.2010.09.001. [DOI] [PubMed] [Google Scholar]
- Weems CF. Developmental trajectories of childhood anxiety: Identifying continuity and change in anxious emotion. Developmental Review. 2008;28:488–502. [Google Scholar]
- Weems CF, Saltzman K, Reiss AL, Carrión VG. A prospective test of the association between emotional numbing and hyperarousal in youth with a history of traumatic stress. Journal of Clinical Child & Adolescent Psychology. 2003;32:166–171. doi: 10.1207/S15374424JCCP3201_15. [DOI] [PubMed] [Google Scholar]