Abstract
BACKGROUND
Hepatitis B (HBV) induced hepatocellular carcinoma (HCC) is the greatest cancer health disparity affecting Asian Americans, but the prevalence of screening to detect HBV is suboptimal.
AIMS
Our aims were to determine the effectiveness of electronic health record (EHR) prompts to increase ordering of HBV tests among primary care providers (PCPs) within an academic health system.
METHODS
We conducted a randomized, controlled trial between April and June 2011 among 76 PCPs caring for 175 outpatient adults with Chinese or Vietnamese surnames, with appointments with providers and no history of HBV testing. Providers were randomized to either receive an EHR prompt for HBV testing prior to patients’ appointments or usual care. Primary outcomes were the proportion of patients 1) whose physician ordered a HBsAg test and 2) who completed testing. Secondary outcomes were A) test results and B) whether the physicians followed-upon the results.
RESULTS
HBsAg tests were ordered for 36/88 (40.9%) of the intervention patients and 1/87 (1.1%) of the control patients [χ2 (df=1) =41.48, p<0.001]. Thirty intervention patients (34.1%) and no control patients completed the HBsAg test [χ2 (df=1) =35.80, p<0.001]. Four (13.3%) of the completed tests were HBsAb positive, 14 (46.7%) were immune and 12 (40%) were unprotected from HBV. Two HBsAg positive patients were referred to specialists, and 3 unprotected patients were vaccinated for HBV.
CONCLUSIONS
EHR-based provider prompts significantly increased HBV testing in Chinese and Vietnamese patients when compared to “usual care.” EHR prompts are a promising intervention that could significantly increase screening for HBV.
Keywords: hepatitis B, Asian American, hepatocellular carcinoma, electronic health record
INTRODUCTION
Hepatocellular carcinoma (HCC) ranks the highest in cumulative rise in cancer mortality among men (50%) and women (29%) in the United States [1, 2]. The incidence and death rates for liver cancer are disproportionately higher in Chinese and Vietnamese Americans and far exceed the rates observed in non-Hispanic white men and women [3]; therefore, HCC is considered to be the greatest cancer health disparity affecting Asian Americans [4, 5]. In California, Vietnamese Americans have the highest age-adjusted incidence rates of HCC (54.3/100,000) and Chinese Americans have the third highest (23.3/100,000) [6]. Screening for the hepatitis B virus (HBV), which accounts for over 80% of all HCC cases in this population, is potentially lifesaving [7, 8].
The Centers for Disease Control and Prevention (CDC) recommend that all foreign-born individuals from Asia and other regions of intermediate to high HBV endemicity along with their household contacts be tested for HBV infection, but many Asian Americans have never been tested [9–14]. Approximately two million individuals are chronically infected with HBV in the United States and are increasing due to immigration from HBV-endemic countries [15, 16]. A majority are of Asian ancestry who are likely to acquire HBV through vertical transmission or horizontal transmission in childhood [17]. Diagnosis of HBV remains low (400,000–600,000) with only 20%–30% aware of their infection [15, 19]. Less than a third of HCC patients were tested for HBV prior to their diagnosis [20].
Multiple barriers to HBV testing such as language, lack of insurance, low socioeconomic status, negative perception of Western medicine, and lack of HBV knowledge have been documented [10–14, 21, 22]. Facilitators for testing include having a regular source of medical care, knowledge that HBV can spread during childbirth, HCC risk in chronic HBV carriers, a provider’s recommendation for testing and asking the provider for testing. The strongest predictor for completing HBV testing was if the patient asked for the test together with the provider’s recommendation [23–29].
Electronic physician prompts have been noted as effective tools to promote the health care [30, 31]. These methods have been utilized to substantially improve breast, colorectal, and cervical cancer screening [32–35]. However, to the best of our knowledge, electronic prompts have never been tested for HBV screening. The purpose of this study was to determine the effectiveness of an EHR prompt for HBV testing by primary care providers (PCP) in at-risk Asian American patients.
METHODS
This was a randomized, controlled study conducted between April 1, 2011 and June 30, 2011 at fifteen urban primary care clinics within an academic healthcare system in Sacramento, California. We determined the baseline rate of HBsAg testing and the prevalence of HBV infection among Chinese and Vietnamese patients based on their surnames, being ages 18–64 years, and not pregnant, who had a medical encounter in 2010. Patients with a HBsAg test at any time were considered tested, and those with a positive HBsAg test were considered infected.
Patient Eligibility and Identification
The patient eligibility criteria were: outpatients enrolled in the EHR (Epic Care, version Summer 2009; Epic Systems Corporation, Verona, Wisconsin), ages 18–64 years, with Chinese or Vietnamese surnames who had a scheduled appointment in a primary care clinic (General Internal Medicine or Family Practice) within the 3 month study period, who were not pregnant and without a history of an HBsAg test. The surnames were selected from a publication of the 50 most common Chinese and Vietnamese ethnically associated surnames, with surnames that are found in more than one ethnicity, e.g., “Lee,” excluded [36]. The database included the patient’s medical record number (MRN), name, gender, ethnic background, language, scheduled appointment date, scheduled PCP, and outpatient clinic name. Our planned sample size of 50 patients in each arm was designed to detect the difference between a clinically significant testing rate of 50% in the intervention group and 20% in the control group (based on the baseline prevalence of testing) with 80% power at the 0.05 level, 2-sided. Our final sample size was larger due to faster accrual than anticipated. With an appointment cancellation rate of approximately 26%, we produced a database of 175 eligible candidates from our search criteria to achieve the sample size for our study (Figure 1).
Figure 1.
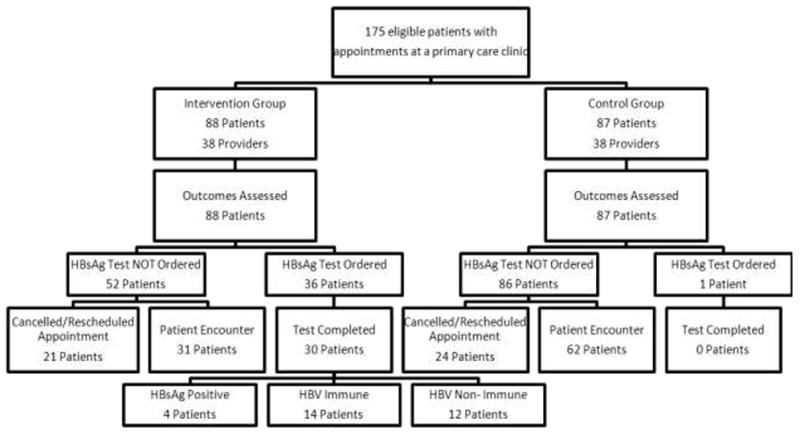
Follow-Chart Depicting Sequence and Outcomes of Electronic Prompting for HBV testing. Diagram of patient and provider eligibility and randomization. Providers were randomized prior to the first patient’s appointment. HBsAg: hepatitis B surface antigen; HBV: hepatitis B virus.
Provider Randomization and Intervention
We randomly assigned providers 1:1 to the intervention or control prior to the first eligible patient’s appointment with a PCP. No trainees were involved. Patients were allocated according to their provider’s assignment. Providers in the intervention received an electronic prompt 24 hours before their patient’s scheduled appointment that identified the patient as a candidate for HBV testing and urged the provider to evaluate the patient for testing. The message, sent by a hepatologist to the provider’s EHR inbox, consisted of several components including a description of the CDC recommendations for HBV testing in at-risk Asian populations, the high prevalence of HBV in Asia, and a list of the appropriate laboratory tests for proper HBV screening. The recommended HBV laboratory panel included the hepatitis B surface antigen (HBsAg), the hepatitis B surface antibody (anti-HBs), and the hepatitis B core antibody (anti-HBc) tests. An explanation of how to evaluate the results of the viral markers was also included in the EHR text. This provider message was directly linked to the patient’s EHR chart to facilitate laboratory test ordering. Providers randomized into the control group did not receive an electronic message (“usual care”). This study was approved by the Institutional Review Board of the University of California, Davis, and an exemption of the informed consent was obtained because it would have compromised the purpose of the intervention.
Study Outcomes and Data Collection
The primary outcomes of this study were (1) rates of HBsAg ordering by providers and (2) HBsAg test completion by patients. Secondary outcomes were (A) the results of the laboratory tests, i.e., patient’s HBV status, and (B) whether the providers initiated actions based on the laboratory test results.
All data were collected through manual reviews of the EHR after a 3-month post-intervention window, considered to be a reasonable time to allow patients to complete their test orders and for providers to initiate any actions based on the test results. All patient data were collected from the EHR, and PCP demographics, race (Asian or non-Asian), gender, and medical specialty (family practice or internal medicine), were collected from the biographies on the medical center’s website. Patient status was dichotomized into: new patient (no past provider encounters) or returning patient (at least one previous provider encounter). The visit types were categorized into either preventive care (e.g., general check-up) or medical complaint. Patients who rescheduled or did not show up to their appointment did not have a consult note and were categorized as “No Data.” Information on whether providers acknowledged receipt of the EHR prompt was described.
Data Analysis
Baseline characteristics of the patients and providers in each arm were compared using the χ2 test for dichotomous variables and t-test for continuous variables, as were the characteristics of patients. The same methods were used to compare the study arms with respect to whether or not an HBsAg test was ordered, whether or not the order was completed, and within the intervention group, to determine the association of patient and provider characteristics with the order of a test. Statistical significance was assessed at the 0.05 level (2-sided). We accounted for clustering of patients within providers using generalized estimating equations to model any associations with statistically significant χ2 test or t-test p-values. Statistical analyses were completed with the SPSS version 17.0 [IBM SPSS, Armonk, New York 2008].
RESULTS
Over the 3-month study period, 175 Chinese or Vietnamese patients were scheduled to see a provider and included in the analysis. Thirty-three patients did not keep their appointment and 12 rescheduled an appointment date outside of our study period. A total of 88 patients scheduled to be seen by 38 providers were in the intervention group, and 87 patients scheduled to be seen by 38 providers were in the control group (Figure 1). Baseline demographics of the providers were similar for race, gender, and medical specialty (Table 1). Twenty of 38 intervention providers and 19 of 38 control providers had only 1 patient while the maximum number of patients seen by a provider was 9 and 7 in the intervention and control groups, respectively. Patients in the intervention and control groups were similar in age, race, gender, patient status, and visit type (Table 1). Of the 175 patients, 139 (79.4%) identified English as their language of preference while 7 (4.0%) specified Vietnamese, 1 (0.6%) Mandarin, 5 (2.9%) Cantonese, 3 (1.7%) Hmong, 1 (0.6%) Mien, and 19 (10.9%) declined to state/no data. Among those who identified their race, 136/175 (77.1%) identified Asian, 5 (2.9%) identified as other, and 3 (1.7%) identified as white, and 31 (17.7%) declined to state/no data. The eight other/white were included on the principle of intention to treat because they had a Chinese or Vietnamese surname (presumably married or mixed race). Of the 8 patients, 6 were in the control group and did not receive a test order, and one (“other race”) in the intervention group received a test order and ultimately was diagnosed as positive for HBV. No other demographic data could be utilized to elucidate more information on the ethnic backgrounds of those classified in nondescript groups. A majority of the intervention and control patients were returning patients who had past medical consultations. There were no significant differences between the intervention and control groups on all measured demographic characteristics.
Table 1.
Comparison of baseline intervention and control primary care provider and patient characteristics
| Characteristics | Intervention | Control | P-value | |
|---|---|---|---|---|
| Primary Care Provider | ||||
| Patient to Provider Ratio ± SD | 2.32±1.95 | 2.29±1.81 | 0.95 | |
| Race | 0.20 | |||
| Asian | 8 (21.1%) | 13 (34.2%) | ||
| Gender | 0.49 | |||
| Female | 20 (52.6%) | 23 (60.5%) | ||
| Medical Specialty | 0.49 | |||
| Family Medicine | 23 (60.5%) | 20 (52.6%) | ||
|
| ||||
| Patient | ||||
| Mean Age ± SD (years) | 40.4±11.5 | 41.3±13.1 | 0.64 | |
| Ethnicity (surname) | 0.43 | |||
| Chinese | 60 (68.2%) | 64 (73.6%) | ||
| Gender | 0.68 | |||
| Females | 54 (61.4%) | 56 (64.4%) | ||
| Language: | 0.95 | |||
| English | 70 (79.5%) | 69 (79.3%) | ||
| Asian Language | 8 (9.1%) | 9 (10.3%) | ||
| Unknown | 10 (11.4%) | 9 (10.3%) | ||
| Racial Background | 0.31 | |||
| Asian | 69 (78.4%) | 67 (77.0%) | ||
| White/Other | 2 (2.3%) | 6 (6.9%) | ||
| Unknown | 17 (19.3%) | 14 (16.1%) | ||
| Patient Status* | 0.54 | |||
| Return | 74 (84.1%) | 76 (87.4%) | ||
| Visit Type† | 0.48 | |||
| Preventive Care | 35 (39.8%) | 27 (31.0%) | ||
| Medical Issues | 32 (36.4%) | 36 (41.4%) | ||
| No Consult Note | 21 (23.9%) | 24 (27.6%) | ||
Note: Primary care provider: n = 38 for both intervention and control groups
Patient: n = 88 intervention, n = 87 control
SD = Standard Deviation
Patient status was defined as return if the patient had at least one documented visit with a physician within the UC Davis Health System.
Visit types were determined by whether the EHR note listed a medical issue as a chief complaint or one of the following preventive care services: a general checkup, annual physical exam, or a well-woman exam. Only collected from patients who attended their scheduled appointment.
Baseline rates of HBsAg testing in this medical center were 17.3% and 18.5%, and the prevalence of HBV was 17.2% and 21.3% in Chinese and Vietnamese patients, respectively. Of 175 patients, 45 (25.7%) patients either missed their appointment or rescheduled their appointment outside of the study period. Patients who kept versus patients who missed or rescheduled their appointments were similar in terms of gender and ethnicity. The only variable that appeared to differentiate these two groups was age: patients that missed their scheduled appointments were somewhat younger than the patients that kept their appointments (37.5±12.4 versus 42.0±12.1; t (df=173) = 2.17, p = 0.032). We do not believe potential participation in this study affected the rate or reasons for missing or rescheduling appointments as patients would not have known of being recommended for HBV testing until they met with their provider.
In the 67 intervention patients the providers of 48 (71.6%) intervention patients documented assessing HBV testing for the patients in the electronic consult notes, and providers for 19 (28.4%) patients made no documentation. The 21 patients that rescheduled or missed their scheduled appointment did not have a consult note to verify whether the physician acknowledged receiving the electronic message.
For primary outcome (1), 36 (40.9%) of the 88 intervention patients and 1 (1.1%) of the 87 control patients received an order for HBsAg testing (Figure 1, Table 3;χ2 (df=1) =41.48, p< 0.001). Thirty (34.1%) patients in the intervention arm and no patients in the control arm completed the HBV laboratory tests for primary outcome (2) [χ2 (df=1) =35.80, p< 0.001]. Among the intervention patients that made their appointments, the mean patient age, gender, ethnicity, and patient status did not differ between those that received an HBsAg test order and those without a test order (Table 2). However, patients who visited their provider for preventive care were much more likely to receive the HBsAg test order than those with medical complaints [χ2 (df=1) =4.23, p = 0.040]. No significant differences were detected in provider demographics between those that did and did not order the HBsAg test. All significant variables remained statistically significant after accounting for within-provider clustering.
Table 2.
Characteristics of the intervention group comparing appointment-keeping patients for whom a hepatitis B test was ordered versus not ordered
| Test Ordered (n=36) | Test Not Ordered (n=31) | P-Value | |
|---|---|---|---|
| Mean Age ± SD (years) | 43.1±10.9 | 38.4±11.6 | 0.091 |
| Gender | 0.31 | ||
| Female | 20 (55.6%) | 21 (67.7%) | |
| Ethnicity | 0.57 | ||
| Chinese | 22 (61.1%) | 21 (67.7%) | |
| Visit Type | 0.040 | ||
| Preventive Care | 23 (63.9%) | 12 (38.7%) | |
| Patient Status | 0.95 | ||
| Return | 30 (83.3%) | 26 (83.9%) | |
| Provider Race | 0.43 | ||
| Asian | 15 (41.7%) | 10 (32.3%) | |
| Provider Gender | 0.21 | ||
| Female | 24 (66.7%) | 16 (51.6%) | |
| Provider Specialty | 0.47 | ||
| Family Practice | 24 (66.7%) | 18 (58.1%) |
Patients completed their laboratory test orders in a median 2.5 days with 83.3% of the patients completing the test within 15 days (mean 9.7±14.8 days; range 0–57 days). For secondary outcome (A), 13.3% of the tested patients were HBsAg positive, 46.7% were HBV immune (HBsAb positive), and 40.0% were HBV non-immune.
For secondary outcome (B), we tracked patients’ laboratory results. The patients who tested HBsAg positive or HBV non-immune were tracked for 3 months after the intervention. Two patients with HBV infection were referred to a specialist, and the other 2 did not receive any actions by their PCP. Of the 12 HBV non-immune patients, 25% were administered their first dose of the HBV vaccine within our study period, and 75% of the patients did not receive any further care with regard to their hepatitis B status.
DISCUSSION
HBV-induced HCC is the greatest cancer health disparity that affects Asian Americans [4, 5]. Testing of all at-risk individuals for HBV is recommended but baseline HBV testing prevalence was low (< 20%) in Chinese and Vietnamese patients. Documented barriers include language, lack of insurance, low socioeconomic status, lower education level, negative perception of Western medicine, lack of HBV knowledge, younger age, and lack of access to care and therefore, increased the risk of HBV transmission [10–14, 21–29, 37]. Recruiting insured patients from an academic clinical practice allowed us to minimize many of these confounding variables. A majority (79.4%) of patients identified English as their primary language, decreasing the likelihood of language being an influential factor in ordering the HBV test or patients’ abilities to communicate with their providers. Patients seen at these clinics had readily accessible interpreters via video conferencing if needed.
This study was initiated to determine whether electronic prompting might increase HBV testing among patients who all had equal access to care and who were not pregnant and not receiving prenatal care (which includes HBsAg testing as a standard of care). In our novel approach to promote HBV testing in Asian Americans, we achieved more than a 2-fold increase in HBsAg testing from 18.5% to 50.0% in Vietnamese patients and from 17.3% to 36.7% in Chinese patients when compared to the baseline testing rates.
In the intervention group, 83.3% of patients completed laboratory tests ordered by their physician, confirming that provider recommendation is a most influential determinant for getting tested [24, 29]. Even with a relatively small sample of 175 patients, our randomized, controlled trial demonstrated that the intervention significantly improved HBsAg testing rates in patients versus “usual care,” where only 1 of 87 patients (1.1%) received the HBsAg test order. Patients were more likely to receive the test order during preventive care visits than when they had a medical complaint. HBV testing should be considered in all at-risk individuals according to the CDC recommendations; however, there are clinical barriers to test ordering [9]. Providers documented assessing HBV testing in 71.6% of the intervention patients that kept their appointments. Various reasons for not ordering the HBV tests would have included patients already been tested or vaccinated previously. Additionally, time constraints, lack of HBV knowledge, unfamiliarity with CDC guidelines, lack of Asian language abilities, the patient’s medical priorities, and patients canceling or rescheduling their appointments are possible factors that may contribute to providers not ordering the tests even when electronically prompted [38, 39]. Barriers to implementing this practice exist, and these findings elucidate some potential issues that need to be considered within the context of other medical care priorities. Our study findings reinforce the IOM’s recommendations to educate both providers and patients on hepatitis B and provide empirical evidence on the utility of the clinical setting for encouraging testing [15, 19, 39–41].
The prevalence rate of HBsAg positivity of those tested for secondary outcome (A) is 13.3%, which is consistent with the rates between 10% and 15% for Chinese and Vietnamese Americans. Through early detection of chronic HBV infection by this intervention, providers may be able to initiate antiviral treatment earlier to suppress viral replication, which has been shown to reduce liver inflammation and fibrosis, and slow disease progression into cirrhosis, the primary risk factor for HCC [46–48]. Half of the patients identified as HBV carriers were referred to specialists to properly manage their disease. Management of chronic HBV patients also involves HCC surveillance allowing for more treatment options [8, 49].
We also found that 40% of the tested patients were susceptible to HBV infection. Through this EHR intervention, the PCPs became aware of the patient’s HBV status by ordering the laboratory tests and were able to initiate vaccination protocols [9]. One-fourth of the HBV non-immune patients were administered the HBV vaccine, but others were not administered the vaccine because they had not returned for another appointment within the post-intervention period.
Our study had some limitations. Our EHR did not have country of birth information on patients or ethnic identifiers, as those items were optional. Hence as a surrogate, we used known Chinese and Vietnamese surnames. First, Chinese and Vietnamese patients were identified through surnames commonly associated with these groups, but surnames that are associated with other ethnic groups, e.g., “Lee,” were excluded. However, the typically Chinese surname, “Li”, (also pronounced “Lee”) was included. Therefore, the Chinese and Vietnamese in this study may not be inclusive of all Chinese and Vietnamese patients. Secondly, we decided on a 3 month time period for patients to complete test orders and for providers to act on the test results, but the optimal time for these objectives to be completed has not yet been determined. As such, our findings may be an underestimate of effectiveness. Finally, many providers had more than one patient, lending to the possibility of a learning effect for HBsAg test ordering by providers with multiple patients in the intervention group; however, our results remained statistically significant after accounting for within-provider clustering and there was no significant trend in ordering by physicians over time.
On the other hand, this study has numerous strengths. First, this study is a prospective randomized, controlled trial with objective outcomes. Second, outcomes were tracked through EHRs assuring standardization and efficiency. Identifying Chinese and Vietnamese surnames has been automated in our EHR, and other Asian surnames can be programmed to link with ICD codes and lab results. As a result, the process for increasing serological testing could be adopted by other health systems with EHRs. This was not our first such study focused on increasing serological testing for HBV among Asian Americans [20, 29, 50]. Most importantly, the size of the effect is large and clinically significant.
Our intervention resulted could be valuable in the early detection of chronic HBV carriers which could potentially reduce the HBV-induced HCC disproportionately higher mortality rates in Asian Americans who are the USA’s fastest growing racial group [51]. According to the Pew Report [51], of those ages 18 and older, 76% of Chinese Americans and 84% of Vietnamese Americans are foreign-born. This study offers empirical evidence for the efficacy and effectiveness of employing electronic prompting of HBV testing for at-risk Chinese and Vietnamese Americans in a clinical setting and lends itself to the reduction of HBV-induced HCC disparities. Future research should include identifying other barriers of providers for ordering HBV tests, follow-up of the actions of providers for patients who tested HBV positive or who need to be vaccinated, expanding these interventions to include other groups, and to investigate the role of patient-activation tailored interventions to ask providers to order testing.
Acknowledgments
This study was supported in part by the UC Davis School of Medicine Office of the Dean and P01CA109091-A1 from the National Cancer Institute & the National Institute on Minority Health and Health Disparities. However, the views expressed are those of the authors and do not necessarily reflect the views of the National Institute of Health.
Footnotes
The data herein were presented as a poster at the Fourth American Association for Cancer Research (AACR) Conference on The Science of Cancer Health Disparities in Racial/Ethnic Minority Populations & the Medically Underserved, 9/20/2011, Washington, DC, pp. 136.
Disclosure of financial arrangements
Dr. Bowlus receives research support and consulting fees from Bristol Myers Squibb and Gilead.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v1.2, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 10 [Internet] Lyon, France: International Agency for Research on Cancer; 2010. [accessed Sep 24, 2011]. Available from URL: http://globocan.iarc.fr. [Google Scholar]
- 2.Siegel R, Ward E, Brawly O, Jemal A. Cancer statistics, 2011: The impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–36. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 3.Miller BA, Chu KG, Hanley BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008;19:227–56. doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen MS., Jr Cancer health disparities among Asian Americans: what we do and what we need to do. Cancer. 2005;104:2895–902. doi: 10.1002/cncr.21501. [DOI] [PubMed] [Google Scholar]
- 5.Chang ET, Keegan THM, Gomez SL, et al. The burden of liver cancer in Asians and Pacific Islanders in the Greater San Francisco Bay Area, 1990 through 2004. Cancer. 2007;109:2100–8. doi: 10.1002/cncr.22642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCracken M, Olsen M, Chen MS, Jr, Jemal A, Thun M, Cokkinides V, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin. 2007;57:190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- 7.Hwang JP, Hassan MM. Survival and hepatitis status among Asian Americans with hepatocellular carcinoma treated without liver transplantation. BMC Cancer. 2009;9:46. doi: 10.1186/1471-2407-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen JG, Parkin DM, Chen QG, et al. Screening for liver cancer: results of a randomized controlled trial in Qigong, China. J Med Screen. 2003;10:204–9. doi: 10.1258/096914103771773320. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC) Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR. 2008;57:1–21. [PubMed] [Google Scholar]
- 10.Taylor VM, Jackson JC, Pineda M, Pham P, Fischer M, Yasui Y. Hepatitis B knowledge among Vietnamese immigrants: implications for prevention of hepatocellular carcinoma. J Cancer Educ. 2000;15:51–5. doi: 10.1080/08858190009528654. [DOI] [PubMed] [Google Scholar]
- 11.Taylor VM, Tu SP, Woodall E, et al. Hepatitis B knowledge and practices among Chinese immigrants to the United States. Asian Pac J Cancer Prev. 2006;7:313–7. [PubMed] [Google Scholar]
- 12.Taylor VM, Choe JH, Yasui Y, Li L, Burke N, Jackson JC. Hepatitis B awareness, testing, and knowledge among Vietnamese American men and women. J Community Health. 2005;30:477–90. doi: 10.1007/s10900-005-7282-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson MJ, Taylor VM, Jackson JC, et al. Hepatitis B knowledge and practices among Chinese American women in Seattle, Washington. J Cancer Educ. 2002;17:222–6. doi: 10.1080/08858190209528842. [DOI] [PubMed] [Google Scholar]
- 14.Wu CA, Lin SY, So SK, Chang ET. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco Bay Area, California. Asian Pac J Cancer Prev. 2007;8:127–34. [PubMed] [Google Scholar]
- 15.Cohen C, Holmberg SD, McMahon BJ, et al. Is chronic hepatitis B being undertreated in the United States? J Viral Hepat. 2011;18:377–83. doi: 10.1111/j.1365-2893.2010.01401.x. [DOI] [PubMed] [Google Scholar]
- 16.Maddrey WC. Hepatitis B: an important public health issue. J Med Virol. 2000;61:362–6. doi: 10.1002/1096-9071(200007)61:3<362::aid-jmv14>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 17.Lee WM. Hepatitis B virus infection. N Engl J Med. 1997;11:1733–45. doi: 10.1056/NEJM199712113372406. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. [Accessed February 14, 2012.];Hepatitis B. Department of Communicable Diseases Surveillance and Response. < www.who.inst/csr/disease/hepatitis/HepatitisB/_whocdscsrlyo2002_2.pdf.
- 19.Institute of Medicine. Hepatitis and liver cancer: a national strategy for the prevention and control of hepatitis B and C. Washington, D.C: the National Academies Press; 2010. [PubMed] [Google Scholar]
- 20.Bastani R, Glenn BA, Taylor VM, et al. Integrating theory into community interventions to reduce liver cancer disparities: the Health Behavior Framework. Prev Med. 2010;50:63–7. doi: 10.1016/j.ypmed.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen H, Tu SP, Teh CZ, et al. Lay beliefs about hepatitis among North American Chinese: implications for hepatitis prevention. J Community Health. 2006;31:94–112. doi: 10.1007/s10900-005-9000-6. [DOI] [PubMed] [Google Scholar]
- 22.Tran TT. Understanding cultural barriers in hepatitis B virus infection. Cleve Clin J Med. 2009;76:S10–3. doi: 10.3949/ccjm.76.s3.03. [DOI] [PubMed] [Google Scholar]
- 23.Taylor VM, Yasui Y, Burke N, et al. Hepatitis B testing among Vietnamese American men. Cancer Detect Prev. 2004;28:170–7. doi: 10.1016/j.cdp.2004.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coronado GD, Taylor VM, Tu SP, et al. Correlates of hepatitis B testing among Chinese Americans. J Community Health. 2007;32:379–90. doi: 10.1007/s10900-007-9060-x. [DOI] [PubMed] [Google Scholar]
- 25.Bazargan M, Bazargan SH, Calderon JL, Husaini BA, Baker RS. Mammography screening and breast self-examination among minority women in public housing projects: the impact of physician recommendations. Cell Mol Biol. 2003;49:1213–8. [PubMed] [Google Scholar]
- 26.Chang ET, Nguyen BH, So SK. Attitudes toward hepatitis B and liver cancer prevention among Chinese Americans in the San Francisco Bay Area, California. Asian Pac J Cancer Prev. 2008;9:605–13. [PubMed] [Google Scholar]
- 27.Taylor VM, Jackson JC, Tu SP, et al. Cervical cancer screening among Chinese Americans. Cancer Detect Prev. 2002;26:139–45. doi: 10.1016/s0361-090x(02)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taylor VM, Schwartz SM, Yasui Y, et al. Pap testing among Vietnamese women: health care system and physician factors. J Community Health. 2004;29:437–50. doi: 10.1007/s11123-004-3393-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nguyen TT, McPhee SJ, Stewart S, et al. Factors associated with hepatitis B testing among Vietnamese Americans. J Gen Intern Med. 2010;25:694–700. doi: 10.1007/s11606-010-1285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Persell SD, Kaiser D, Dolan NC, et al. Changes in performance after implementation of a multifaceted electronic-health-record-based quality improvement. Med Care. 2011;49:117–25. doi: 10.1097/MLR.0b013e318202913d. [DOI] [PubMed] [Google Scholar]
- 31.Jimbo M, Nease DE, Jr, Ruffin MT, 4, Rana GK. Information technology and cancer prevention. CA Cancer J Clin. 2006;56:26–36. doi: 10.3322/canjclin.56.1.26. [DOI] [PubMed] [Google Scholar]
- 32.Mandelblatt JS, Yabroff KR. Effectiveness of interventions designed to increase mammography use: a meta-analysis of provider-targeted strategies. Cancer Epidemiol Biomarkers Prev. 1999;8:759–67. [PubMed] [Google Scholar]
- 33.McPhee SJ, Bird JA, Fordham D, Rodnick JE, Osborn EH. Promoting cancer prevention activities by primary care physicians: results of a randomized, controlled trial. JAMA. 1991;266:538–44. [PubMed] [Google Scholar]
- 34.Sarfaty M, Wender R. How to increase colorectal cancer screening rates in practice. CA Cancer J Clin. 2007;57:354–66. doi: 10.3322/CA.57.6.354. [DOI] [PubMed] [Google Scholar]
- 35.Vinker S, Nakar S, Rosenberg E, Kitai E. The role of family physicians in increasing annual fecal occult blood test screening coverage: a prospective intervention study. Isr Med Assoc J. 2002;4:424–5. [PubMed] [Google Scholar]
- 36.Lauderdale DS, Kestenbaum B. Asian American ethnic identification by surname. Popul Res Policy Rev. 2000;19:283–300. [Google Scholar]
- 37.Choe JH, Taylor VM, Yasui Y, et al. Health care access and sociodemographic factors associated with hepatitis B testing in Vietnamese American men. J Immigr Minor Health. 2006 Jul;8:193–201. doi: 10.1007/s10903-006-9322-1. [DOI] [PubMed] [Google Scholar]
- 38.Khalili M, Guy J, Yu A, Li A, et al. Hepatitis B and hepatocellular carcinoma screening among Asian Americans: survey of safety net healthcare providers. Dig Dis Sci. 2011;56:1516–23. doi: 10.1007/s10620-010-1439-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lai CJ, Nguyen TT, Hwang J, Stewart SL, Kwan A, McPhee SJ. Provider knowledge and practice regarding hepatitis B screening in Chinese-speaking patients. J Cancer Educ. 2007;22:37–41. doi: 10.1007/BF03174373. [DOI] [PubMed] [Google Scholar]
- 40.Hu KQ. Hepatitis B virus (HBV) infection in Asian and Pacific Islander Americans (APIAs): how can we do better for this special population. Am J Gastroenterol. 2008;103:1824–33. doi: 10.1111/j.1572-0241.2008.01878.x. [DOI] [PubMed] [Google Scholar]
- 41.Wong PY, Xia V, Imagawa DK, Hoefs J, Hu KQ. Clinical presentation of hepatocellular carcinoma (HCC) in Asian-Americans versus non-Asian-Americans. J Immigr Minor Health. 2011;13:842–8. doi: 10.1007/s10903-010-9395-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chao SD, Chang ET, Le PV, Prapong W, Kiernan M, So SK. The Jade Ribbon Campaign: a model program for community outreach and education to prevent liver cancer in Asian Americans. J Immigr Minor Health. 2009;11:281–90. doi: 10.1007/s10903-007-9094-2. [DOI] [PubMed] [Google Scholar]
- 43.Do S. The natural history of hepatitis B in Asian Americans. Asian Am Pac Isl J Health. 2001;9:141–53. [PubMed] [Google Scholar]
- 44.Custer B, Sullivan SD, Hazlet TK, Iloeje U, Veenstra DL, Kowdley KV. Global epidemiology of hepatitis B virus. J ClinGastroenterol. 2004;38:s158–68. doi: 10.1097/00004836-200411003-00008. [DOI] [PubMed] [Google Scholar]
- 45.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46:1034–40. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- 46.Tong MJ, Hsien C, Hsu L, Sun HE, Blatt LM. Treatment recommendations for chronic hepatitis B: an evaluation of current guidelines based on a natural history study in the United States. Hepatology. 2008;48:1070–8. doi: 10.1002/hep.22476. [DOI] [PubMed] [Google Scholar]
- 47.Chang TT, Liaw YF, Wu SS, et al. Long-term entecavir therapy results in the reversal of fibrosis/cirrhosis and continued histological improvement in patients with chronic hepatitis B. Hepatology. 2010;52:886–93. doi: 10.1002/hep.23785. [DOI] [PubMed] [Google Scholar]
- 48.Papatheodoridis GV, Lampertico P, Manolakopoulos S, Lok A. Incidence of hepatocellular carcinoma in chronic hepatitis B patients receiving nucleos(t)ide therapy: a systematic review. J Hepatol. 2010;53:348–56. doi: 10.1016/j.jhep.2010.02.035. [DOI] [PubMed] [Google Scholar]
- 49.Tong MJ, Sun HE, Hsien C, Lu DS. Surveillance for hepatocellular carcinoma improves survival in Asian-American patients with hepatitis B: results from a community-based clinic. Dig Dis Sci. 2010;55:826–35. doi: 10.1007/s10620-009-1059-y. [DOI] [PubMed] [Google Scholar]
- 50.Maxwell AE, Bastani R, Chen MS, Jr, Nguyen TT, Stewart SL, Taylor VM. Constructing a theoretically based set of measures for liver cancer control research studies. Prev Med. 2010;50:68–73. doi: 10.1016/j.ypmed.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pew Research Center. The Rise of the Asian Americans. 2012 Jul 12; Accessible through www.pewsocialtrends.org.


