Abstract
Objectives
Examine utilization of chaplain services among Veterans Affairs (VA) patients with colorectal cancer (CRC).
Methods
In 2009, the Cancer Care Assessment & Responsive Evaluation Studies questionnaire was mailed to VA CRC patients diagnosed in 2008 (67% response rate). Multivariable logistic regression examined factors associated with chaplain utilization.
Results
Of 918 male respondents, 36% reported utilizing chaplains. Chaplain services were more likely to be utilized by patients with higher pain levels (OR=1.017; 95% CI=0.999–1.035), younger age (age OR=0.979; 95% CI=0.964–0.996) and later cancer stage (early stage OR=0.743; 95% CI=0.559–0.985).
Conclusions
Chaplain services are most utilized by younger, sicker patients.
Keywords: cancer, oncology, colorectal neoplasms, hospital chaplaincy service, Veterans health
INTRODUCTION
Receiving a diagnosis of colorectal cancer can have far reaching effects. About a third of patients who receive a diagnosis of cancer report experiencing significant, potentially debilitating, distress as a result (Vachon, 2006). This distress can take many forms, including physiological, social, financial, and spiritual (Arndt, Merx, Stegmaier, Ziegler, & Brenner, 2004; Fitchett et al., 2004; Mickley, Soeken, & Belcher, 1992; Spiegel, 1994). The pervasive impact that a cancer diagnosis can exert on every dimension of life may even persist in the face of a favorable disease prognosis (Flannelly, Weaver, & Handzo, 2003). Following a cancer diagnosis, patients often are confused and reflective about their lives, and many turn to faith and spiritual counseling (Dunn et al., 2006; Hamilton, Jackson, Abbott, Zullig, & Provenzale, 2011). For those who regularly attend religious services, there is evidence that they experience less spiritual struggle and emotional distress when diagnosed (Fitchett, et al., 2004). This translates into a demand for services that extends beyond the traditional medical field and may include pastoral care. In the community setting, clergy members are often on the frontline of mental health care, serving as counselors and addressing mental health care needs due to their accessibility (Milstein, Manierre, Susman, & Bruce, 2008; Weaver, Flannelly, Flannelly, & Oppenheimer, 2003). In the healthcare setting, a multidisciplinary team of allied health care professionals – often including chaplains, social workers, psychologists, and psychiatrists, among others – has been recommended to ensure that all aspects of cancer patients’ well being are addressed (Millstein, Manierre, & Yali, 2010; Weaver, et al., 2003).
In recent years, there has been increased emphasis on utilizing a wide range of providers, including chaplains, for comprehensive cancer care and spiritual health (Weaver, et al., 2003). However, the majority of research focuses on the inclusion of clinically trained staff rather than on the provision of spiritually oriented, hospital-based chaplain services. Many studies on utilization of chaplain services have been conducted in the palliative care setting, but people with cancer may feel an increased spiritual need regardless of disease prognosis (Flannelly, et al., 2003). While scientific evidence supporting a linkage between chaplain care and long-term improvement on cancer disease progression or mortality is lacking, there is evidence that physical health, quality of life, and spiritual well-being are closely connected (Cavendish et al., 2007; Holland et al., 1999; Stefanek, McDonald, & Hess, 2005). Patients receiving spiritual care at the end of life report higher quality of life and make different treatment decisions, like starting hospice earlier in the course of care (Balboni et al., 2010). Previous studies in this domain tend to examine patients near the end of life rather than across the broader trajectory of disease. Our study brings a unique perspective because it surveys newly diagnosed patients across the disease trajectory, not just those near the end of life.
Patients with colorectal cancer may have a variety of reasons for pursuing chaplain services. Chaplains are trained to assist patients who are dealing with physical pain or end of life issues (Galek et al., 2009; Sinclair, Mysak, & Hagen, 2009). They may also be preferred to mental health care providers among patients concerned about the stigma attached to their diagnosis. Even for patients with a positive prognosis, social stigma can be an issue due to fear of others knowing about a colostomy or their disease status (MacDonald & Anderson, 1984; Phelan et al., 2011). There is evidence that patients have different expectations regarding chaplains’ services depending on their age. For example, a study at the Mayo Clinic found that patients older than 35 years were more likely to expect a hospital chaplain to visit without being requested (Piderman et al., 2008). Younger individuals are less likely to have established membership in a traditional religious organization (Life, 2008) and, as a result, may not have a built-in spiritual support network when they become seriously ill. It has also been shown that younger patients are more likely to experience spiritual distress in the face of a diagnosis with advanced cancer (Hui et al., 2011). Middle-aged people are more likely to be fearful of death compared to older people, likely because of a perceived disconnect between the desired and expected time left to live (Cicirelli, 2006). Moreover, as awareness of death increases, middle-aged adults are more likely to report a fear of physical loss than their older aged counterparts (Cicirelli, 2006). In contrast, older individuals may be visited by members and clergy from their religious center, making them less reliant on hospital chaplains than someone without this builtin spiritual support (Life, 2008). Chaplains are trained to help both patients and their loved ones cope with these issues. A three-year study at Memorial Sloan Kettering Cancer Center examining use of chaplain services found that chaplains also served patients’ family and friends rather than working directly with patients themselves. The study also found that chaplain interventions differed according to patients’ religious views, disease progression, and whether the patient or just family members were present (Flannelly, et al., 2003).
The present study examined the extent to which male patients with colorectal cancer utilized chaplain services in the Veterans Health Administration. The VA chaplain service, initiated in 1945, is tasked with meeting spiritual healthcare needs of Veterans (Affairs, 2011). Hospital-based chaplains are available at VA medical centers nationwide, 24-hours a day, in both inpatient and outpatient settings. Chaplains are trained to accommodate multiple faiths and religious views so that they are equipped to better meet the spiritual needs and beliefs of diverse patients. Chaplains provide a wide range of services, including identifying “at risk” patients, grief counseling, family counseling, and values clarification. Many of these supportive services help patients learn to cope with a recent colorectal cancer diagnosis (Affairs, 2011). The current study examined chaplain utilization, predictors of chaplain utilization, and satisfaction with chaplaincy services among newly diagnosed colorectal cancer patients in the VA.
METHODS
This analysis examined utilization of and experience with hospital-based chaplain services through a nationwide Veterans Affairs (VA) survey of patients newly diagnosed colorectal cancer in 2008. The protocol for survey administration and use of data for analysis were approved by the Institutional Review Board (IRB) of the Minneapolis VA Medical Center and University of Minnesota School of Medicine. The Durham VA Medical Center IRB also approved using survey data for analysis.
The C-CARES Survey
A team of researchers from VA Health Services Research & Development, Department of Defense, National Cancer Institute, and the University of Minnesota collaborated to develop the Cancer Care Assessment and Responsive Evaluation (C-CARES) survey. The primary purpose of C-CARES was to assess patient-reported experience with the VA healthcare system, including both clinical and non-clinical care, among newly diagnosed colorectal cancer patients. C-CARES included several domains of questions assessing diagnosis and access to care, cancer treatments, symptoms, hospice care, primary care, barriers to care, and care coordination among others, and was written at an 8th grade reading level. C-CARES also queried patients about their utilization of and experience with VA’s hospital-based chaplain program.
Patient Identification and Survey Mailing
Patients were identified through the VA Central Cancer Registry (VACCR). The VACCR uses custom software (OncoTraX) that integrates with the VA electronic health record system to identify all cancer cases diagnosed and treated within VA, making it a comprehensive resource for patient identification. It has been estimated that VACCR captures approximately 90% of cancer cases treated in VA (Jackson et al., 2010; Zullig et al., 2012).
C-CARES aimed to survey all eligible VA patients nationwide who were newly diagnosed with colorectal cancer in 2008. To be included in the survey cohort, patients had to meet the following eligibility criteria: 1) newly diagnosed with colorectal cancer during calendar year 2008, 2) received over half of their cancer care at any medical center in the VA healthcare system, and 3) living at the time of the mailing. After attaining the initial list from the VACCR (n=2,555), a research assistant at the Minneapolis VA manually reviewed patients’ electronic medical record to confirm eligibility criteria, including vital status, and to identify the patient’s mailing address to which the survey would be sent. Surveys were mailed to 2,090 patients between August and November 2009.
The self-administered C-CARES survey was mailed directly to the patients’ homes. A ten-dollar incentive was included in the survey packet to encourage participation.
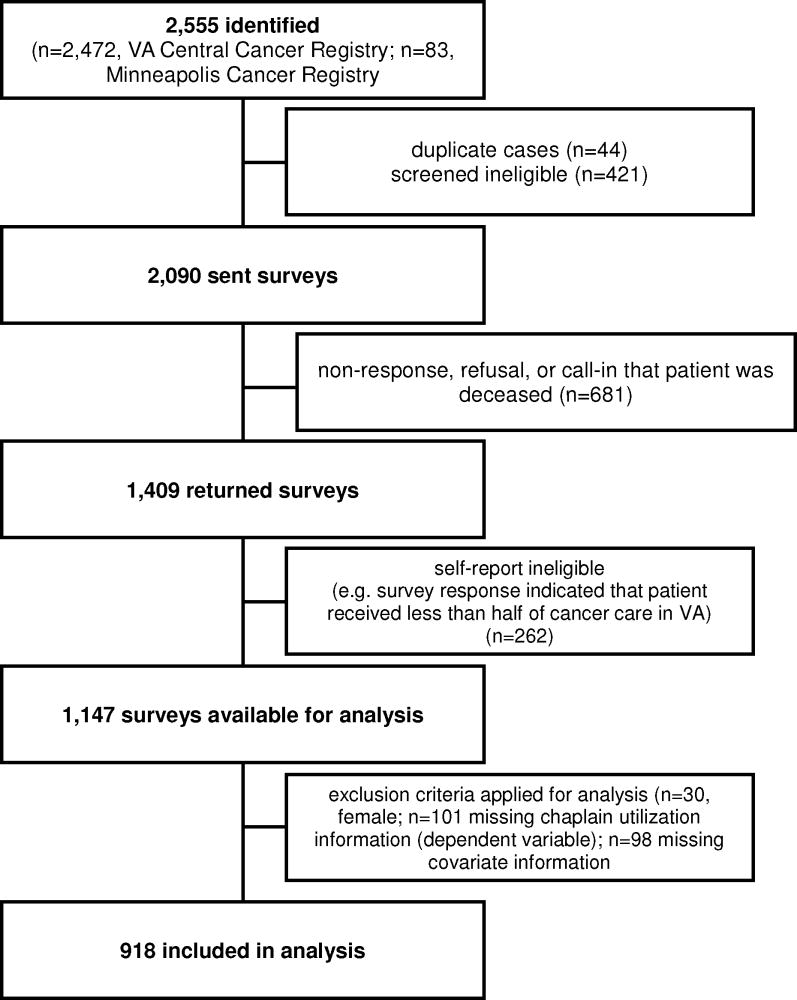
A total of 1,409 surveys were returned, resulting in an overall response rate of approximately 67%. Individuals who indicated that they received most of their cancer care outside of the VA were excluded from analysis. After this secondary eligibility screening process, a total of 1,147 surveys were used for analysis. Additionally, surveys without a response regarding utilization of chaplain services (n=101) or with missing information on any of the covariates (n=98) were omitted from analysis (Figure 1). The small number of women made gender comparisons statistically infeasible so female respondents (n=30) were also excluded. As a result, 918 male patients were included in these analyses.
Figure 1.
Survey Flow
Patient Reported Utilization of Chaplain Services
Respondents were asked whether they received help for their emotions or mood from VA nurses, physicians, mental health specialists, and chaplains. Patients were asked, “During the last 6 months, did a doctor or nurse give you the help that you wanted with your emotions or mood?” Response options included: ‘Yes’, ‘No’, ‘I am not sure’, and ‘Help not wanted’. Next, patients were asked, “During the last 6 months, did you talk with a therapist, counselor or clergy about your emotions or mood?” Response options included: ‘Yes’, ‘No’, and ‘I am not sure’. A subsequent question asked, “Did you ever talk with a chaplain (priest, minister, rabbi, etc.) while at the VA since you were diagnosed with colorectal cancer?” Responses options included: ‘Yes’ and ‘No’. Patients who responded ‘yes’, that they had spoken with a chaplain, were asked about their experience with chaplain services. Questions included: “How helpful was the chaplain?” and “Overall, how satisfied were you with the chaplain services at the VA?” Patients responded to each of these questions on a five-point Likert scale ranging from ‘not at all’ to ‘extremely.’
Patients who did not utilize chaplain services were asked their reason for non-use. Response options included: ‘not interested or did not need chaplain services at the VA’, ‘not aware that chaplain services were available’, ‘the chaplain was not available’, and ‘some other reason.’
Outcome
The outcome variable, utilization of chaplain services, was derived from the following question in the C-CARES survey: “Did you ever talk to a chaplain (priest, minister, rabbi, etc.) while at the VA since you were diagnosed with colorectal cancer?” As previously described, response options were ‘yes’ or ‘no’.
Explanatory Variables
Measures of patient characteristics, disease characteristics, and symptoms were included as explanatory and control variables. Patient characteristics included age (continuous), race (binary), employment status (binary), educational level (binary), income (categorical), and social support (categorical). Age was measured as a continuous variable describing the age at CRC diagnosis. Race information was aggregated into four mutually exclusive categories: white, black, Hispanic, or other race. Race was determined base on two hierarchical sources. First, the race category indicated by the respondent on the returned survey was used. Race from the VA Central Cancer Registry was utilized if the patient failed to report race on the C-CARES survey. The C-CARES survey served as the data source for employment status, educational level, and annual income. Respondents were considered employed if they reported any part-or full-time employment. Educational level was binary – respondents who reported completing high school or higher-level education versus respondents who reported partial completion of high school or less education. Annual income was in four distinct categories: less than $10,000, between $10,000 and $20,000, between $20,001 and $40,000, or greater than $40,000.
A lack of social support is a factor known to impact the use of psychosocial services (McDowell, Occhipinti, Ferguson, & Chambers, 2010; Steginga et al., 2008). In order to assess patients’ social support system, patients were asked, “If you had to choose, which person is most likely to help or take care of you, if you needed it?” Possible responses included: ‘my spouse’, ‘my daughter’, ‘my son’, ‘my boyfriend/girlfriend or partner’, ‘another family member’, ‘a friend or neighbor’, ‘other’, and ‘no one would help or take care of me’. Responses were combined into three mutually exclusive variables indicating support from spouse, family and friends (apart from the spouse), or no one.
In addition to patient characteristics, we also controlled for disease characteristics and symptoms. Stage at diagnosis, aggregated into early stage (i.e., Stage I or II) versus late stage (i.e, Stage III or IV), was included in the model. To assess symptom severity within the last six months, C-CARES contained validated PROMIS scales for fatigue, pain, and depression (DeWalt, Rothrock, Yount, Stone, & Group, 2007; Reeve et al., 2007). A t-score for each scale was calculated for every respondent. PROMIS scale t-score distributions are standardized such that the mean for the general U.S. population is 50 and the standard deviation around this mean is ten (DeWalt, et al., 2007; Reeve, et al., 2007). Higher scores indicated greater severity of symptoms. In order for PROMIS scales to be meaningful, patients must respond to all survey items. PROMIS scale calculation would not be possible with incomplete data; surveys with missing information on any PROMIS symptom survey item were excluded from analysis.
To assess symptoms, we asked questions on fatigue, pain and depression. Fatigue was measured using the validated PROMIS fatigue scale (Cella et al., 2010; DeWalt, et al., 2007). Examples of questions included, “How often did you experience extreme exhaustion?” and “How often did you run out of energy?” Patients responded to questions using the following categories: ‘never’, ‘rarely’, ‘sometimes’, ‘often’, or ‘always’.
Pain was measured using the six validated PROMIS pain scale items(Cella, et al., 2010; DeWalt, et al., 2007). Examples of pain questions include, “How much did pain interfere with your enjoyment of life?” and, “How much did pain interfere with your ability to concentrate?” Patients indicated either: ‘not at all’, ‘a little bit’, ‘somewhat’, ‘quite a bit’, or ‘very much’.
Depression was assessed using questions from the validated PROMIS depression scale to assess problems with mood (Cella, et al., 2010; DeWalt, et al., 2007). Expressions of mood or depression problems included, “I felt worthless” and, “I felt that I had nothing to look forward to.” Response options included: ‘never’, ‘rarely’, ‘sometimes’, ‘often’, or ‘always’. The PROMIS scale t-scores were then calculated separately for pain, fatigue, and depression (Reeve, et al., 2007).
Analysis
Statistical analyses were performed using Stata (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP). We conducted multivariable logistic regression analysis to determine the likelihood that respondents with specific patient, disease, and symptom characteristics would report utilization of chaplain services.
RESULTS
Survey Respondents
Survey respondents were predominately white (76%) males with a mean age of 67.5 years. The majority of survey respondents were not employed (81%). Most had attained a high school degree or higher level of education (84%). Annual incomes were less than $10,000 for approximately 84% of survey respondents. Slightly fewer than half of respondents reported their spouse as their primary social support. Approximately 5% reported no source of social support. Slightly more than half (61%) of patients were diagnosed with early stage disease (i.e., Stage I or II) compared to late stage disease (i.e., Stage III or IV; 39%). We compared the reported frequency of symptoms among the survey respondents and U.S. population. Survey respondents were similar to the general U.S. population in terms of reporting symptoms of fatigue, pain, and mood (Table 1).
Table 1.
Characteristics of survey respondents (n=918)
| Percent/Mean | SD (Min, Max) | |
|---|---|---|
| Patient Characteristics | ||
| Age | 67.5 | 9.8 (26, 90) |
| Male | 100.0 | -- |
| White race | 76.0 | -- |
| Black race | 13.6 | -- |
| Hispanic | 5.6 | -- |
| Other race | 4.8 | -- |
| Employment and Educational Status | ||
| Employed | 19.2 | -- |
| Not employed | 80.8 | -- |
| High school or higher education | 84.3 | -- |
| Less than high school education | 15.7 | -- |
| Annual Income | ||
| < $10,000 | 84.37 | -- |
| $10,000 – $20,000 | 49.2 | -- |
| $20,001 – $40,000 | 24.5 | -- |
| >$40,000 | 10.6 | -- |
| Social Support | ||
| Spouse | 48.2 | -- |
| Family and Friends | 40.9 | -- |
| No one | 4.7 | -- |
| Stage at Diagnosis | ||
| Early stage (i.e, Stage I or II) | 61.3 | -- |
| Late stage (i.e., Stage III or IV) | 38.7 | -- |
| Symptoms | ||
| Fatigue | 53.0 | 9.8 (32.5, 82.7) |
| Pain | 51.3 | 10.7 (41.0, 78.1) |
| Mood problems | 50.5 | 10.9 (37.1, 81.1) |
Utilization of Chaplain Services
Approximately 39% of survey respondents reported that a doctor or nurse did not provide help needed with their emotions or mood. This indicates that there may be a need for psychosocial and spiritual support services that chaplains may be able to provide. Approximately 19% of patients reported talking with a therapist, counselor, or clergy about their emotions or mood, and 36% of respondents indicated that they had spoken with a VA chaplain since receiving their diagnosis.
Respondents were also asked about reasons for not utilizing chaplain services. Of those who responded, 73% cited that they were not interested or did not need chaplain services. The next most common response was that the respondent was not aware that chaplain services were available (approximately 15%), indicating a possible gap.
Satisfaction with Chaplain Services
A minority of respondents reported their level of satisfaction with and helpfulness of chaplain services. Of those patients who responded, when asked about their level of satisfaction with chaplain services, 64% of survey respondents reported being very or extremely satisfied. Similarly, 48% of survey respondents indicated that the chaplain was very or extremely helpful. In contrast, only 13% indicated that they were not at all or only a little satisfied and 23% indicated that the chaplain was not at all or a little helpful.
Multivariate Logistic Regression
Age, stage of disease, and level of pain had statistically significant affects on the odds of utilizing chaplain services (Table 2). A one-year increase in age was associated with decreased odds of utilizing chaplain services (OR 0.979; 95% CI 0.964, 0.996; p=0.014). Similarly, early stage at diagnosis was associated with reduced odds of utilizing chaplain services (OR 0.743; 95% CI 0.559, 0.985; p=0.039). Neither race, employment status, level of education, nor annual income had a significant impact on the odds of utilizing chaplain services. Social support also had no significant impact on utilization of chaplain services. Fatigue and depression had no effect of utilization of chaplain services. Being in pain, however, was associated with increased odds of utilizing the services of chaplains (OR 1.017, 95% CI 0.999, 1.035, p=0.054).
Table 2.
Multivariate logistic regression results describing factors associated with utilization of chaplain services. (n=918)
| OR | 95% CI | p | |
|---|---|---|---|
| Patient Characteristics | |||
| Age | 0.979 | (0.964, 0.996) | 0.014* |
| Race | 1.058 | (0.891, 1.260) | 0.518 |
| Not employed† | 1.100 | (0.756, 1.60) | 0.6317 |
| Less than high school education†† | 0.791 | (0.523, 1.198) | 0.268 |
| Annual Income††† | |||
| < $10,000 | 0.757 | (0.431, 1.329) | 0.332 |
| $10,000 – $20,000 | 1.007 | (0.624, 1.625) | 0.978 |
| $20,001 – $40,000 | 1.101 | (0.665, 1.821) | 0.709 |
| Social Support†††† | |||
| Family and friends | 1.029 | (0.772, 1.373) | 0.841 |
| No one | 0.853 | (0.432, 1.684) | 0.647 |
| Disease Characteristics & Symptomsδ | |||
| Early stage | 0.743 | (0.559, 0.985) | 0.039* |
| Fatigue | 1.006 | (0.985, 1.027) | 0.580 |
| Pain | 1.017 | (0.999, 1.035) | 0.054* |
| Depression | 1.000 | (0.984, 1.017) | 0.971 |
Indicates statistical significance.
The referent employment status category is part- or full-time employment.
The referent educational category is completion of high school or greater.
The referent annual income category is >$40,000.
The referent social support category is spouse.
Symptoms are based on PROMIS scores.
Early stage of disease is a dichotomous variable where earlystage=1 if Stage I or II and earlystage=0 if Stage III or IV disease.
DISCUSSION
This analysis finds that patients’ age, stage of disease at diagnosis, and level of pain affect the odds of reporting use of chaplain services. Patients who have more advanced cancer and feel more discomfort may perceive themselves to be closer to the end of life compared to asymptomatic patients who share a common diagnosis of colorectal cancer. Younger patients diagnosed with late stage disease may experience a high level of spiritual distress and fear of death (Cicirelli, 2006; Hui, et al., 2011), particularly since a cancer diagnosis may be unanticipated. Young patients are less likely to expect a chaplain visit to occur automatically in a hospital setting (Piderman, et al., 2008). Therefore, younger patients may actively seek chaplain services and be more likely to report them in a survey.
Studies have identified characteristics of spiritual care programs that are more likely to be viewed as valuable by members of a multidisciplinary care team: a) being physically located close to cancer care; b) reporting to senior hospital leaders; c) taking a multi-faith approach; and d) maintaining an academic affiliation (Sinclair, et al., 2009). These types of programs, however, are not very widespread, and although in general, medical and religious communities embrace the idea of spiritual well being as a component of comprehensive cancer care, in some healthcare organizations, healthcare professionals not trained in spiritual issues provide spiritual care. In one study, a substantial proportion of medical oncologists and nurses reported that they were primarily responsible for addressing spiritual needs with their patients (Kristeller, Zumbrun, & Schilling, 1999), but nearly 90% indicated that a chaplain would be better suited to meet this patient care need (Kristeller, et al., 1999).
In the VA, chaplain services are well integrated into patient care services. Chaplains are available throughout the VA healthcare system and are prepared to counsel patients of diverse faiths or religious views. A study among Veterans Affairs (VA) hepatocellular cancer patients found that chaplains, when part of a multidisciplinary care team, improved patient and family satisfaction with care (Van Cleave, Devine, & Odom-Ball, 1999).
It is important that healthcare providers be aware that newly diagnosed cancer patients may desire to see a chaplain and that patients may derive benefits from these interactions, such as decreased emotional distress and religious struggle (Fitchett, et al., 2004; Weaver, et al., 2003). Another recent VA study found that nearly 80% of colorectal cancer patients had documentation in their medical record of receiving some type of psychosocial support early in their diagnosis. Just over half of patients had documentation of at least some type of interaction with chaplain services (Hamilton, et al., 2011). This is higher than the 36% chaplain utilization rate found in our current study. This difference may be an artifact of data collection procedures. Our study uses patient-reported data, whereas the aforementioned study employed medical record abstraction to obtain data. Despite the incongruity in absolute percentage of use, both Hamilton and colleagues and our current study found that rates of chaplain use were higher than other forms of psychosocial support (i.e., psychologist, psychiatrist, or similar) among VA colorectal cancer patients.
Furthermore, this rate of psychosocial service utilization ranks higher than rates reported in some studies occurring in the private sector. For example, an Australian study found that less than half of cancer patients take advantage of chaplain and other psychosocial support services (Steginga, et al., 2008).
The current study found a minority (i.e., 15%) of survey respondents who were unaware of chaplain services. While the severity of this lack of awareness cannot be fully assessed by the current survey, there is gap in communication should be addressed. The scope of the current survey is limited to colorectal cancer patients during finite period of treatment, but patients with different types of cancer may utilize chaplain services differently. In addition, utilization of and satisfaction with chaplain services may be dependent on when a patient accesses chaplain services. The C-CARES surveyed patients following their initial diagnosis; however, it is possible that patients for whom more time has elapsed since their diagnosis or with recurrent cancer may report different chaplain utilization.
Limitations
The C-CARES survey was a self-administered survey. Response bias is a limitation with this data collection approach. Patients who responded to the survey had to have a mailing address. As such, homeless patients would not have been surveyed. Additionally, patients must have been physically well enough to respond to the survey. It is unlikely that patients who were hospitalized for an extended period of time or who were at the end of life would have responded to the C-CARES survey. These survey respondents were likely healthier than those patients that did not respond. It seems reasonable that sicker patients will have a greater proclivity to utilize chaplain services – both hospital-based and with their established clergy at home. As a result, this analysis may under report utilization of chaplain services. Recall bias is an issue with any health services survey. Patients may under- or over-report chaplain use due to perceived “correct” answers, social stigma, not remembering the encounter, or similar issues. We also do not know what specific services chaplains provided. Perhaps most importantly, the C-CARES survey did not inquire about religious affiliation or religiosity. Patients who are more religious may be more likely to seek assistance from chaplains. Future studies should examine this issue.
Conclusions
Over one-third of newly diagnosed colorectal cancer patients sought counsel from a VA hospital-based chaplain. This is a substantial proportion of patients, particularly since the cohort of survey respondents were relatively well distributed by stage of disease and slightly favored early stage disease. However, higher level of pain and greater stage of disease were positively associated with chaplain care-seeking behavior. Increased age was negatively associated with chaplain utilization. This suggests that, while chaplain services were utilized by a wider net of patients, the majority of use was likely among younger, sicker patients.
Acknowledgments
The authors acknowledge the statistical support and calculations provided by Deborah Finstad in Department of Family Medicine & Community Health and the University of Minnesota. This work was supported by the Inter-agency Quality of Cancer Care Committee, Applied Research Branch, National Cancer Institute through an Interagency Agreement with the Veterans Health Administration (IAG V246S-00054). Ms. Zullig was supported by funding from the National Cancer Institute (5R25CA116339). During part of this work, Dr. Jackson held a Merit Review Entry Program award from the Veterans Affairs Health Services Research & Development Service (MRP-05-312). Dr. Provenzale was supported by an NIH K24 (DK002926-07).
Biography
Ms. Zullig is a Project Coordinator with the Center for Health Services Research in Primary Care at the Durham Veterans Affairs Medical Center. In that role she has worked with national cancer care collaboratives, many of which place emphasis on the role of clergy in providing supportive cancer care. In addition, Ms. Zullig is a doctoral candidate in Health Policy and Management at the University of North Carolina at Chapel Hill. She currently holds a Masters in Public Health.
Footnotes
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- Arndt V, Merx H, Stegmaier C, Ziegler H, Brenner H. Quality of life in patients with colorectal cancer 1 year after diagnosis compared with the general population: a population-based study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2004;22(23):4829–4836. doi: 10.1200/JCO.2004.02.018. [DOI] [PubMed] [Google Scholar]
- Balboni TA, Paulk ME, Balboni MJ, Phelps AC, Loggers ET, Wright AA, Prigerson HG. Provision of spiritual care to patients with advanced cancer: associations with medical care and quality of life near death. J Clin Oncol. 2010;28(3):445–452. doi: 10.1200/jco.2009.24.8005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavendish R, Edelman M, Naradovy L, Bajo MM, Perosi I, Lanza M. Do pastoral care providers recognize nurses as spiritual care providers? Holistic nursing practice. 2007;21(2):89–98. doi: 10.1097/01.HNP.0000262024.35196.11. [DOI] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Group PC. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of clinical epidemiology. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicirelli VG. Fear of death in mid-old age. J Gerontol B Psychol Sci Soc Sci. 2006;61(2):75–81. doi: 10.1093/geronb/61.2.p75. [DOI] [PubMed] [Google Scholar]
- DeWalt DA, Rothrock N, Yount S, Stone AA, Group PC. Evaluation of item candidates: the PROMIS qualitative item review. Medical care. 2007;45(5 Suppl 1):S12–21. doi: 10.1097/01.mlr.0000254567.79743.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn J, Lynch B, Rinaldis M, Pakenham K, McPherson L, Owen N, Aitken J. Dimensions of quality of life and psychosocial variables most salient to colorectal cancer patients. Psychooncology. 2006;15(1):20–30. doi: 10.1002/pon.919. [DOI] [PubMed] [Google Scholar]
- Fitchett G, Murphy PE, Kim J, Gibbons JL, Cameron JR, Davis JA. Religious struggle: prevalence, correlates and mental health risks in diabetic, congestive heart failure, and oncology patients. Int J Psychiatry Med. 2004;34(2):179–196. doi: 10.2190/UCJ9-DP4M-9C0X-835M. [DOI] [PubMed] [Google Scholar]
- Flannelly KJ, Weaver AJ, Handzo GF. A three-year study of chaplains’ professional activities at Memorial Sloan-Kettering Cancer Center in New York city. Psycho-oncology. 2003;12(8):760–768. doi: 10.1002/pon.700. [DOI] [PubMed] [Google Scholar]
- Galek K, Vanderwerker LC, Flannelly KJ, Handzo GF, Kytle J, Ross AM, Fogg SL. Topography of referrals to chaplains in the Metropolitan Chaplaincy Study. J Pastoral Care Counsel. 2009;63(1–2):6-1-13. [PubMed] [Google Scholar]
- Hamilton NS, Jackson GL, Abbott DH, Zullig LL, Provenzale D. Use of psychosocial support services among male veterans affairs colorectal cancer patients. Journal of Psychosocial Oncology. 2011;29(3):242–253. doi: 10.1080/07347332.2011.563346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland JC, Passik S, Kash KM, Russak SM, Gronert MK, Sison A, Baider L. The role of religious and spiritual beliefs in coping with malignant melanoma. Psycho-oncology. 1999;8(1):14–26. doi: 10.1002/(SICI)1099-1611(199901/02)8:1<14::AID-PON321>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Hui D, de la Cruz M, Thorney S, Parsons HA, Delgado-Guay M, Bruera E. The frequency and correlates of spiritual distress among patients with advanced cancer admitted to an acute palliative care unit. Am J Hosp Palliat Care. 2011;28(4):264–270. doi: 10.1177/1049909110385917. [DOI] [PubMed] [Google Scholar]
- Jackson GL, Melton LD, Abbott DH, Zullig LL, Ordin DL, Grambow SC, Provenzale D. Quality of Nonmetastatic Colorectal Cancer Care in the Department of Veterans Affairs. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010 doi: 10.1200/JCO.2009.26.7948. (Journal Article) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristeller JL, Zumbrun CS, Schilling RF. ‘I would if I could’: how oncologists and oncology nurses address spiritual distress in cancer patients. Psycho-oncology. 1999;8(5):451–458. doi: 10.1002/(sici)1099-1611(199909/10)8:5<451::aid-pon422>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- MacDonald LD, Anderson HR. Stigma in patients with rectal cancer: a community study. J Epidemiol Community Health. 1984;38(4):284–290. doi: 10.1136/jech.38.4.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell ME, Occhipinti S, Ferguson M, Chambers SK. Prospective predictors of psychosocial support service use after cancer. Psycho-oncology. 2010 doi: 10.1002/pon.1774. (Journal Article) [DOI] [PubMed] [Google Scholar]
- Mickley JR, Soeken K, Belcher A. Spiritual well-being, religiousness and hope among women with breast cancer. Image--the journal of nursing scholarship. 1992;24(4):267–272. doi: 10.1111/j.1547-5069.1992.tb00732.x. [DOI] [PubMed] [Google Scholar]
- Millstein G, Manierre A, Yali AM. Psychological Care for Persons of Diverse Religions: A Collaborative Continuum. Professional Psychology: Research and Practice. 2010;41(5):371–381. [Google Scholar]
- Milstein G, Manierre A, Susman VL, Bruce ML. Implementation of a Program to Improve the Continuity of Mental Health Care Through Clergy Outreach and Professional Engagement (C.O.P.E.) Professional Psychology: Research and Practice. 2008;39(2):218–228. [Google Scholar]
- Pew Forum on Religion & Public Life. US Religious Landscape Survey. 2008 Retrieved November 13, 2011, 2011, from http://religions.pewforum.org/reports.
- Phelan SM, Griffin JM, Jackson GL, Zafar SY, Hellerstedt W, Stahre M, van Ryn M. Stigma, perceived blame, self-blame, and depressive symptoms in men with colorectal cancer. Psychooncology. 2011 doi: 10.1002/pon.2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piderman KM, Marek DV, Jenkins SM, Johnson ME, Buryska JF, Mueller PS. Patients’ expectations of hospital chaplains. Mayo Clin Proc. 2008;83(1):58–65. doi: 10.4065/83.1.58. [DOI] [PubMed] [Google Scholar]
- Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Teresi JA, Group PC. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS) Medical care. 2007;45(5 Suppl 1):S22–31. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- Sinclair S, Mysak M, Hagen NA. What are the core elements of oncology spiritual care programs? Palliat Support Care. 2009;7(4):415–422. doi: 10.1017/s1478951509990423. [DOI] [PubMed] [Google Scholar]
- Spiegel D. Health caring. Psychosocial support for patients with cancer. Cancer. 1994;74(4 Suppl):1453–1457. doi: 10.1002/1097-0142(19940815)74:4+<1453::aid-cncr2820741609>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Stefanek M, McDonald PG, Hess SA. Religion, spirituality and cancer: current status and methodological challenges. Psycho-oncology. 2005;14(6):450–463. doi: 10.1002/pon.861. [DOI] [PubMed] [Google Scholar]
- Steginga SK, Campbell A, Ferguson M, Beeden A, Walls M, Cairns W, Dunn J. Socio-demographic, psychosocial and attitudinal predictors of help seeking after cancer diagnosis. Psycho-oncology. 2008;17(10):997–1005. doi: 10.1002/pon.1317. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. National Chaplain Center Retrieved Web Page, 2011. 2011 from http://www.va.gov/chaplain/
- Vachon M. Psychosocial distress and coping after cancer treatment. Cancer Nurs. 2006;29(2 Suppl):26–31. doi: 10.1097/00002820-200603002-00011. [DOI] [PubMed] [Google Scholar]
- Van Cleave J, Devine P, Odom-Ball P. Multidisciplinary care of hepatocellular carcinoma. Cancer practice. 1999;7(6):302–308. doi: 10.1046/j.1523-5394.1999.76007.x. [DOI] [PubMed] [Google Scholar]
- Weaver AJ, Flannelly KJ, Flannelly LT, Oppenheimer JE. Collaboration between Clergy and Mental Health Professionals: A Review of Professional Health Care Journals from 1980 through 1999. Counseling and Values. 2003;47(3):162–171. [Google Scholar]
- Zullig LL, Jackson GL, Dorn RA, Provenzale DT, McNeil R, Thomas CM, Kelley MJ. Cancer incidence among patients of the U.S. Veterans Affairs Health Care System. Mil Med. 2012;177(6):693–701. doi: 10.7205/milmed-d-11-00434. [DOI] [PMC free article] [PubMed] [Google Scholar]