Abstract
Background
Research on reactivity to alcohol and drug cues has either ignored affective state altogether or has focused rather narrowly on the role of negative affect in craving. Moreover, until recently, the relevant analyses of affect and craving have rarely addressed the ambivalence often associated with craving itself. The current study investigated how both negative and positive affect moderate approach and avoidance inclinations associated with cue-elicited craving in a clinical sample diagnosed with substance use disorders.
Methods
One hundred forty-four patients (age range 18–65, mean 42.0; n = 92 male) were recruited from an inpatient detoxification unit for substance abuse. Participants completed a baseline assessment of both positive and negative affect prior to completing a cue-reactivity paradigm for which they provided self-report ratings of inclinations to approach (use) and avoid (not use) alcohol, cigarettes, and non-psychoactive control substances (food and beverages).
Results
Participants with elevated negative affect reported significantly higher approach ratings for cigarette and alcohol cues, whereas those high in positive affect showed significantly higher levels of avoidance inclinations for both alcohol and cigarette cues and also significantly lower approach ratings for alcohol cues, all relative to control cues.
Conclusions
Results for negative affect are consistent with previous cue reactivity research, whereas results for positive affect are unique and call attention to its clinical potential for attenuating approach inclinations to substance use cues. Further, positive affect was related to both approach and avoidance inclinations, underscoring the utility of a multidimensional conceptualization of craving in the analysis.
Keywords: craving, approach, avoidance, cue-reactivity, positive affect, negative affect
1. Introduction
With nearly 9% of the U.S. population age 12 or older diagnosable with Substance Use Disorders (SUDs) -- most notably alcohol and tobacco use problems (SAMHSA, 2010) -- SUDs are undeniably a major public health concern. The high rates of comorbidity of SUDs with anxiety and mood disorders (e.g., Grant et al., 2004) serves to complicate this problem, but also directs attention to the need for a better understanding of links between affect and compulsive use of popular psychoactive substances (cf. Leshner, 1997). Despite strong links between affect and addictive behaviors, research on reactivity to alcohol and drug cues has typically presented substance use cues only, without regard to the person’s affective state or has focused rather narrowly on the role of negative affect in craving. Moreover, until recently, the relevant analyses of affect and craving have rarely addressed the ambivalence often associated with craving itself (see Stritzke, McEvoy, Wheat, Dyer, & French, 2007, for a review). An ambivalence model of craving acknowledges both the desire to consume a substance (approach inclination) and the desire to not consume it (avoidance inclination). By examining the interplay of positive and negative affect with the desire to approach and the desire to avoid substance use, the present study sought to further elucidate the links between affect and subjective craving experiences for alcohol and tobacco.
1.1. Approach and Avoidance as Separate Dimensions of Subjective Craving Experiences
Theories accounting for substance user’s reactivity to drug related stimuli often focus on craving, which has been defined as cue-elicited motivation to consume the substance (e.g., Sayette et al., 2000; Tiffany & Coklin, 2000; Tiffany, 1990). Cue-elicited craving is thought to develop through a process of conditioning, in which drug-related cues are repeatedly paired with positively and/or negatively reinforcing drug effects (e.g., Baker, Piper, McCarthy, Majeskie, & Fiore, 2004; Carter & Tiffany, 1999); however, such conceptualizations fail to account for the ambivalence that substance abusers commonly display toward the drugs they abuse (e.g., Stritzke et al., 2007; Breiner, et al. 1999; Tiffany, 1990). For example, ambivalence about use, defined as the simultaneous desire to use and to not use psychoactive substances, has been identified as a hallmark feature of addiction, and is central to many clinical formulations of substance use disorders (e.g., Orford, 2001; Heather, 1998). Further, Tiffany’s (1990) cognitive processing model of craving posits that the subjective experience of craving may occur when the immediate gratification of urges to use are impeded by internal motivations to abstain (i.e., abstinence promotion). Despite acknowledgements of the importance of competing desires (Kavanagh et al., 2012; Anton, 1999; Tiffany, 1990), ambivalence is often overlooked in the study of craving.
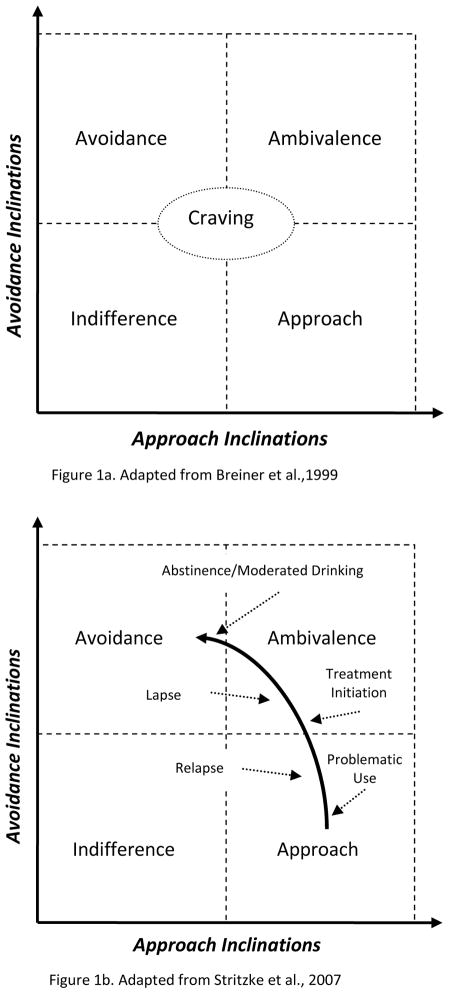
To address this concern, Breiner, Stritzke, and Lang (1999) introduced an ambivalence conceptualization of craving (AMC). Consistent with qualitative (e.g., Smith-Hoerter, Stasiewicz & Bradizza, 2004), quantitative (e.g., Stritzke et al., 2004; Curtin et al., 2005; Schlauch, Breiner, et al., 2012), and neurobiological findings (e.g., Cacioppo et al., 1999, Barkby et al.,2012), the AMC views craving as a complex experience highlighting the importance of not only craving or desires to use (approach inclinations), but also competing desires to not use (avoidance inclinations). These two dimensions of reactivity are thought to develop through different psychobiological systems following repeated, systematic exposure to reinforcing and punishing events associated with such substance use (Ledoux, 2000; Lang, 1995; Stasiewicz & Maisto, 1993), and are proposed to be orthogonal to one another resulting in four hypothetical quadrants (see Figure 1 top panel; Breiner et al., 1999; Stritzke et al., 2007; McEvoy, Stritzke, French, Lang, & Ketterman, 2004). Further, while these dimensions may be activated reciprocally (e.g., high on one dimension, low on the other), approach and avoidance inclinations are independent and can be activated simultaneously to elicit different motivational states that vary as a function of drinking and/or recovery status (see Figure 1 bottom panel).
Figure 1.
Ambivalence Model of Craving.
The addition of a distinct avoidance dimension has numerous advantages clinically and methodologically (see Stritzke et al., 2007 for a review). Further, it has been argued that measuring “craving” or “urge to use” exclusively in terms of approach inclinations without consideration of a separate, yet concurrent, avoidance inclination may misrepresent a motivational disposition that is actually a combination of both, thus significantly diminishing the utility of the information obtained (Breiner et al., 1999). Indeed, studies examining avoidance inclinations using both cue reactivity paradigms and self-report measures have provided support for its incremental validity in predicting substance-related variables in both non-clinical and clinical samples. For example, approach and avoidance can be independently measured as separate dimensions of cue reactivity (e.g. Schlauch, Breiner et al., 2012; Curtin et al., 2005; Stritzke et al., 2004). Further, avoidance has been shown to moderate the effect of approach inclinations on drinking (Schlauch, Levitt et al., 2012), is incrementally related to taking steps to make a change (Klein et al., 2007; Schlauch, Breiner et al., 2012, Schlauch, Stasiewicz, et al., 2012), and distinguishes between clinically significant subgroups of smokers trying to quit (high approach, high avoidance) and not quit (high approach, low avoidance; Stritzke et al., 2004). Finally, avoidance inclinations may be more predictive of relapse among alcoholics, rather than increases in approach inclinations (Stritzke et al., 2007). This is important as it suggests that once internal or external cues trigger urges to use, people can resist them but it takes effort (Tiffany, 1990). The AMC provides a framework for which alcohol/drug use is not inevitable when approach is activated, but rather dependent on competing desires and effortful control such that the stronger one’s avoidance inclinations are, the less likely the decisional balance tips in favor of use. However, despite these promising findings, to date no studies have examined the factors influencing both approach and avoidance inclinations.
1.2. Affect and Craving
The idea that substance use is intimately related to affect and the desire to regulate it is far from novel and enjoys considerable empirical support (cf., Kassel & Veilleux, 2010; Sher & Grekin, 2007). Thus, it is not surprising that there are numerous theoretical accounts of the relationship between approach inclinations and affect in the substance abuse literature (e.g., Baker, Morse, & Sherman, 1987; Baker, Piper, Fiore, McCarthy, & Majeske, 2004; Kavanagh, Andrade, & May, 2005; Tiffany, 1990; Robinson & Berridge, 1993; Stasiewicz & Maisto, 1993). Collectively, these accounts provide varied predictions on the relationship between affect and craving, and point to both positive and negative affect as a precipitant of craving, as a consequence of craving, and as a defining feature of craving (i.e., craving as an affective state).
As a precipitant of craving, negative affect has received considerable empirical support. For example, laboratory procedures inducing negative affect consistently trigger cue-elicited craving (i.e., approach inclinations) in alcoholics (e.g., Cooney, Litt, Morse, Bauer, & Gaupp, 1997; Fox, Berquist, Hong, & Sihna, 2007) and cigarette smokers (e.g., Conklin & Perkins, 2005; Maude-Griffin & Tiffany, 1996; Perkins & Grobe, 1992; Tiffany & Drobes, 1990). As a consequence of craving, negative affect is predicted (e.g.,) when access to the target substance is delayed or blocked (i.e., frustrative non-reward; Kavanagh et al., 2005; Stasiewicz & Maisto, 2003; Tiffany, 1990). In addition, negative affect may also arise in the form of guilt and/or anxiety when craving (i.e., approach inclination) is elicited in a person who is actively attempting to control his or her use (Kavanagh et al., 2005). Finally, negative affect has been described as the predominant emotional reaction in most or all craving experiences (Baker et al., 2004; Kavanagh et al., 2005; Nosen et al., 2012). In all cases, negative affect is predicted to be positively associated with approach inclinations (desire to use) and to varying degrees negatively associated with avoidance inclinations (desire to not use). For example, the predicted negative relationship between negative affect and avoidance inclinations might be stronger in those who have lower abstinence self-efficacy and weaker among those attempting to regulate or control their use of an addictive substance.
With regard to positive affect, it is also viewed as an antecedent (e.g., Baker, Morse, & Sherman, 1987) and consequence of craving (Kavanagh et al., 2005), and also as an appetitive-motivational response akin to the experience of craving itself (Robinson & Berridge, 1993; Stewart, de Witt, & Eikelboom, 1984). Further, it has been argued that the potential for positive affect to elicit craving may be more active in the early stages of addiction (e.g., Tiffany, 2010). In contrast to negative affect, positive affect as a predictor of approach inclinations has received much less empirical support (c.f., Tiffany, 2010) and the conditions in which it is predicted to be a consequence of craving are limited to situations in which consumption is imminent and negative consequences for use are low (Kavanagh et al., 2005). Of the few reports finding significant relationships, positive affect may augment the impact of substance-related imagery on craving in non-clinical populations, with the combined effect as strong as negative affect (Maude-Griffin & Tiffany, 1996; Tiffany & Drobes, 1990). In an alcohol dependent sample, Mason and colleagues (2008) found a significant relationship between positive affect (experimentally induced) and higher ratings to beverage cues on a measure of craving strength (i.e., “How strong is your craving to drink alcohol”). Interestingly, no significant relationships were found between positive affect and craving measures of intentions to use, expectations of positive effects, or lack of control; however, several limitations were noted. Despite increased craving strength following the positive affect induction, manipulation checks revealed that participants’ affective valence remained unchanged. Further, the images used to induce positive affect may have very well triggered craving responses themselves due to their associations with drinking behaviors (e.g., sporting events), a point acknowledged by the authors. Finally, although negative affect was successfully induced using images, no effect on cue-elicited craving was noted, a finding inconsistent with previous literature.
As an appetitive-motivational stimulus, positive affect is thought to share common features of the pleasurable or rewarding elements of substance use. Whether by activation or sensitization of neural systems of reward (e.g., Baker et al., 1987; Robinson & Berridge, 1993; Stewart et al., 1984), or enhancement of an appetitive-motivational process (Kavanagh et al., 2005), positive affect is predicted to maintain substance use approach behaviors. However, positive mood may also inhibit craving, or the accentuation of craving, by exerting influence on self-regulatory processes (e.g., Tice, Baumesiter, Shmueli, & Muraven, 2007) such as self-efficacy and negative expectancies for use, with the latter posited to influence avoidance inclinations. Thus, in contrast to negative affect, the role of positive affect on craving is less straightforward and the nature of its influence appears to depend on such factors as substance availability, perceived negative consequences of use, and abstinence self-efficacy. Further, it is possible that those with greater positive affect in a clinical setting may have an increased inclination to avoid indulging because their positive affective state could very well reflect a sense of purpose and optimism in overcoming their addiction problems. Indeed, positive affect has been associated with greater restraint on smoking following a self-control depletion task (Shmueli & Prochaska, 2012). Therefore, studies examining both approach and avoidance inclinations and their relationships with positive and negative affective states may yield clinically useful information that would otherwise be obscured by traditional craving assessments (i.e. approach inclinations only).
1.3. Present Study
Using data from a larger cue-reactivity study designed to examine the relationship between personality variables and cue-elicited craving towards various psychoactive substances, we examined how positive and negative affect might differentially influence inclinations to both approach (use) and avoid (not use) substances to which they were exposed during a visual cue-reactivity task. Participants sampled from an inpatient SUD detoxification unit reported on their affect states, making separate ratings for positive and negative affect prior to completing a standardized cue-reactivity paradigm (Schlauch, Breiner et al., 2012; Curtin et al., 2005; Stritzke et al., 2004). Specifically, participants provided both approach and avoidance ratings in response to pictorial cues that included alcohol and cigarettes. The following predictions were derived from the existing literature and the ideas outlined above:
Baseline negative affect would be positively associated with approach inclinations for alcohol and cigarettes because negative affect has been shown to predict increased inclinations to indulge in addictive behavior, perhaps as a maladaptive effort to cope.
Baseline negative affect to would be negatively associated with avoidance inclinations for alcohol and cigarettes, as negative affect appears to decrease access to more adaptive coping responses in those with addiction.
Baseline positive affect would be negatively associated with approach inclinations because positive affect might diminish the magnitude of desire or perceived need for a psychoactive substance. This may be most evident in a clinical sample of substance abusers who may have stronger negative reinforcement motives for use.
Baseline positive affect would be positively associated with avoidance inclinations for alcohol and cigarettes, because of the recent negative consequences of their use and because positive affect appears to increase access to more adaptive coping options and/or alternative sources of reinforcement (e.g., greater self-regulation).
2. Method
2.1. Participants
Participants (n=144) were recruited from an inpatient detoxification unit for substance abuse (12-bed inpatient substance abuse treatment program). Participants had a mean age of 42.0 (SD = 11.0; range 18–65 years) and were predominantly male (64%) and Caucasian (62.7%; 25.4% African American, 3.5% Multi-racial, 3.5% American Indian/Native Alaskan, 4.9% Other). Sixty-six percent reported that they were admitted voluntarily and approximately 96% reported that they were actively trying to reduce or cease use of psychoactive substances (see Table 1 for summary of demographic information).
Table 1.
Demographic Information
| Overall Sample (n=144) | Alcohol Analysis (n=129) | Cigarette Analysis (n=116) | |
|---|---|---|---|
|
|
|||
| Mean Age | 42.0 (11.0) | 42.6 (10.7) | 42.5 (11.0) |
| Female | 36.0% | 33.3% | 37.7% |
| Race | |||
| Caucasian | 62.7% | 61.9% | 58.8% |
| African American | 25.4% | 24.6% | 26.3% |
| Multi-racial | 3.5% | 4.0% | 4.4% |
| Native American/Alaskan | 3.5% | 4.0% | 4.4% |
| Other | 3.5% | 4.0% | 4.4% |
| Unknown | 1.4% | 1.6% | 1.8% |
| Employment Status | |||
| Full-time | 20.0% | 21.0% | 19.6% |
| Part Time | 12.8% | 12.9% | 9.0% |
| Unemployed/Job Seeking | 35.7% | 34.7% | 40.2% |
| Retired | 11.4% | 11.3% | 11.6% |
| Unemployed/Not Seeking | 16.4% | 17.7% | 16.1% |
| Student | 3.6% | 2.4% | 3.6% |
| Marital Status | |||
| Single | 33.6% | 34.4% | 35.7% |
| Married | 21.0% | 21.1% | 18.3% |
| Relationship/Not Married | 14.7% | 12.5% | 13.9% |
| Divorced | 28.0% | 28.9% | 28.7% |
| Widowed | 2.8% | 3.1% | 3.5% |
| Annual Income | |||
| $0 to $20,000 | 61.1% | 59.5% | 61.3% |
| $20,001 to $40,000 | 19.1% | 21.6% | 18.9% |
| $40,001 to $60,000 | 6.1% | 6.9% | 5.7% |
| $60,001 to $80, 000 | 3.8% | 2.6% | 3.8% |
| $80,001 to $100,000 | 3.8% | 3.4% | 3.8% |
| Over $100,000 | 6.1% | 6.0% | 6.6% |
| Education (mean years) | 12.5 (2.5) | 12.5 (2.7) | 12.3 (2.5) |
| Voluntary Admission | 66.0% | 65.6% | 66.4% |
| Number of Days on Unit (mean) | 2.2 (1.1) | 2.2 (1.1) | 2.2 (1.1) |
The inpatient substance abuse treatment program provides detoxification to individuals experiencing episodes of excessive substance use or withdrawal complications. Admission criteria to the program include a) being diagnosed with a SUD, b) assessed as cooperative and non-violent, c) current alcohol or substance use at a quantity and frequency sufficient to have developed tolerance and be at risk of withdrawal symptoms when substances are terminated, d) require a minimum of 24 hour medical and nursing services, and d) absence of signs and symptoms requiring acute inpatient hospitalization (e.g., schizophrenia, actively suicidal). Both voluntary and involuntary (e.g., court mandated, physician referred, law-enforcement) admissions are accepted, with an average stay of 3.7 days over the past year. At the time of participation, the average stay in the unit was 2.2 days (SD = 1.1). The most common medications prescribed to control withdrawal symptoms are Librium and Vistaril. In addition, nicotine patches are also provided to cigarette smokers, as smoking is not permitted on the unit. Participants reported a wide range of substance use, including alcohol, cocaine (and its derivatives), and prescription medication (including benzodiazepines and opiates). Of particular interest for the current study, 80.6% reporting daily smoking and 89.6% indicating multiple problems related to alcohol use (see Tables 2 for summary of substance use histories).
Table 2.
Summary of Substance Use
| Overall Sample (n=144) | Alcohol Analysis (n=129) | Cigarette Analysis (n=116) | |
|---|---|---|---|
|
|
|||
| SMAST (13-item) | 7.9 (4.2) | 8.8 (3.5) | 7.6 (4.2) |
| DAST (28-item) | 12.4 (8.4) | 11.9 (8.5) | 12.6 (8.3) |
| Average Drinks/Week | 67.2 (83.8) | 73.5 (85.3) | 64.1 (80.6) |
| Cigarettes per Day | 18.1 (13.3) | 18.1 (13.4) | 22.5 (11.1) |
| Substance Use (Past 30 Days) | |||
| Marijuana | 37.1% | 35.5% | 42.8% |
| Amphetamines | 9.6% | 9.1% | 10.8% |
| Crack Cocaine | 25.7% | 21.8% | 26.8% |
| Cocaine | 22.9% | 20.2% | 25.9% |
| Barbiturates | 15.2% | 15.3% | 16.2% |
| Benzodiazepines | 26.2% | 22.4% | 26.5% |
| Narcotics (pain pills) | 25.7% | 22.4% | 28.6% |
| Heroin | 2.8% | 3.2% | 3.5% |
2.2. Materials
2.2.1. Equipment
A HP Pavilion dv9000 computer (laptop) and a projection unit were used to project the substance cues and instruction slides onto a white projection screen. Microsoft Powerpoint © software was used to control the timing and presentation of the preparatory slides, substance and control cues, and rating periods.
2.2.2. Slides
Sixty-nine slides, representing alcoholic beverages (n = 15; 6 beer, 6 hard liquor, 3 wine), cigarettes (n = 6), food (n = 6), non-alcoholic beverages (n = 6), marijuana (n = 6), stimulant drugs (n = 12; 6 cocaine, 6 crack-cocaine), prescription medication (n = 12; 6 benzodiazepines, 6 opiates), and heroin (n=6), were presented to participants. Within all categories, individual cues varied by setting (e.g., bar, restaurant, home, neutral background) and activity state (e.g., substance sitting untouched on table, held in hand, or actively consumed). Brand names and identifying symbols were excluded to the extent possible. Further, to avoid contamination of reactivity to substance cues with reactions to affective information conveyed by people depicted with the substance, cues were displayed without human involvement whenever possible. When people were depicted along with a substance, facial expressions and body posture were kept neutral. The alcoholic beverage, cigarette, food, and non-alcoholic beverage images were obtained from the Normative Appetitive Picture System (NAPS; Stritzke et al., 2004), which have been previously validated for measuring both approach and avoidance inclinations in three independent samples (Schlauch, Breiner et al., 2012; Stritzke et al., 2004; Curtin et al., 2005). Further, the total number of slides per category vary for the purpose of depicting a full range of possible substances or beverages (e.g., 15 total alcoholic beverages depicting beer, hard liquor and wine). In the current study, three sets of 23 images were created and presented in each of six possible presentation orders, counterbalanced across participants. Within each set, images were distributed quasi-randomly so that no cue type was repeated twice in a row and each category was not systematically followed by another particular category.
2.3. Measures
2.3.1. Cue reactivity ratings
For each cue, ratings of “Approach” and “Avoidance” were taken via self- report. The rating question for each was as follows: “How much do you want to consume the item right now?” and “How much do you want to avoid consuming the item right now?” Both scales were rated on 9-point scales, ranging from 0 (“not at all”) to 8 (“very much”). Participants were instructed to treat the approach and avoidance scales as independent and to rate the images quickly and completely in terms of their “initial reactions.” A separate page for each cue was used, on which the order of the rating scales was randomly presented. Similar procedures have been successfully used to collect approach and avoidance inclinations in both non-clinical and clinical populations (Stritzke et al., 2004; Curtin et al., 2005; Schlauch, Breiner et al., 2012).
2.3.2. Demographics
Demographic and other personal information including gender, age, race, marital and employment status, and education were collected using a self-report survey.
2.3.3. Drinking History Questionnaire
Alcohol use was assessed using the Drinking History Questionnaire (DHQ). The DHQ is a 10-item instrument based on the work of Cahalan, Cisin, and Crossley (1969) which assesses the quantity and frequency of current and past alcohol consumption, as well as subjective experiences and beliefs regarding the individual’s own use of alcohol.
2.3.4. Drug Abuse Screening Test
The Drug Abuse Screening Test (DAST; Skinner, 1982) is a 28-item True/False self-report instrument designed to tap various consequences related to drug abuse. Prior research has demonstrated the DAST to have strong reliability and validity as an index of substance use disorders (Skinner, 1982; Gavin et al., 1989).
2.3.5. Positive and Negative Affect Ratings
Affect ratings were assessed at baseline (i.e., prior to the cue-reactivity task) using the Positive and Negative Affect Schedule (PANAS; Watson, Clark & Tellegen, 1988). The PANAS, a 20-item self-report measure assessesing positive (PA) and negative (NA) affect, was used as the primary measure of affect. On a 5-point scale (1 = very slightly or not at all to 5 = extremely) participants indicate the extent to which they are currently experiencing each of the 20 different emotions included in the instrument. Both the positive affect (PA) and negative affect (NA) scales have been shown to be reliable (e.g., Watson, Clark & Tellegen, 1988).
2.3.6. Short-Michigan Alcohol Screening Test
The Short-Michigan Alcohol Screening test (SMAST; Selzer et al., 1975) is a 13-item True/False measure consisting of items related to alcohol abuse and drinking related problems. The SMAST has been deemed reliable and valid for measuring alcohol related problems (e.g., Selzer et al., 1975; Hays, Merz, & Nicholas, 1995), with scores of 2 indicating possible problematic use and 3 or higher problematic use (Selzer et al., 1975).
2.3.7. Survey of Alcohol and Drug Use
The Survey of Alcohol and Drug Use (SADU; Johnston et al., 2010) was used to assess frequency of drug use. The SADU is a self-report measure taken from the Monitoring the Future Survey that contains questions regarding history and frequency of use across a broad range of drugs. Specifically, participants report on the number of occasions for which they used a variety of substances in their lifetime, during the past 12 months, and during the past 30 days.
2.4. Procedure
Participants were recruited from an inpatient detoxification unit. Potential participants were told that the study would be conducted in two phases to be completed over a three-hour period: an image rating phase (~ 60 minutes) in which participants would rate images of commonly consumed items and a subsequent self-report phase (~ 60–120 minutes, varied by participant) in which they would complete questionnaires about their attitudes and behaviors. Data collection sessions were conducted in a group format on weekdays between 1 to 4 p.m. Each session could have up to 12 participants, though most sessions involved fewer than four participants due to a low census, prior participation, or patient decisions not to participate. Those who chose not to participate were typically given an alternate activity by the staff on the unit.
Participants agreeing to participate first completed baseline measures, including positive and negative affect ratings (i.e., PANAS). Next, participants were given a pencil and binder that included three sections for image rating (i.e., cue reactivity task), one for each set of 23 images. Instructions for rating the images on the two dimensions of approach and avoidance were provided followed by two practice trials. Each rating began with a 4-sec preparatory slide to focus attention and make sure participants’ binders were opened to the correct rating page. This was followed by presentation of a substance cue for 6-sec and then a 30-sec rating period. Based on findings from pilot studies of the present protocol and previous studies using similar procedures, it was expected that participants would generally finish their ratings within 15–20 seconds, leaving a rest period of about 10–15 seconds before the next preparatory slide signaled the conclusion of the current rating period. Between each set of pictures participants were given a 5-min break. Following the cue-reactivity task, participants were given a 15-minute break and then asked to complete additional questionnaires (i.e., drinking and substance use histories, SMAST, DAST, and demographics).
2.5. Data Analytic Strategy
Prior to all analyses, all variables were examined for outliers and normality and found to be within acceptable ranges. To examine our hypotheses, two separate multivariate regression analyses were conducted using a path analysis framework (MPLUS 6.11; Muthen & Muthen, 2011). For each analysis, approach and avoidance ratings for substance (alcohol or cigarettes) and control cues were regressed onto positive affect, negative affect and whether participants were admitted to the unit voluntarily or not (0=involuntary, 1=voluntary). We controlled for voluntary admission to the treatment unit due to expected differences on motivation to change behavior and their potential effects on both approach and avoidance inclinations. To provide generalizability across psychoactive substances, we chose to analyze alcohol and cigarette cues for two reasons: a) alcohol and cigarettes were the most frequently used substances among participants, and b) the alcohol and cigarette cues have been well validated for use in the current cue-reactivity paradigm. Previous research on cue-elicited craving suggests that reactivity to alcohol and cigarette cues vary as a function of history of use (Stritzke et al., 2004; Curtin et al., 2005; Schlauch, Breiner et al., 2012). Therefore, to ensure variability on both approach and avoidance inclinations in response to the cues, only participants who indicated multiple problems associated with their alcohol use (SMAST ≥ 2; n=129) or daily smoking (n=116) were used in the relevant analyses. Means, standard deviations, and correlations among the variables of interest are presented in Table 1.
3. Results
3.1. Alcohol Approach and Avoidance Reactivity Ratings
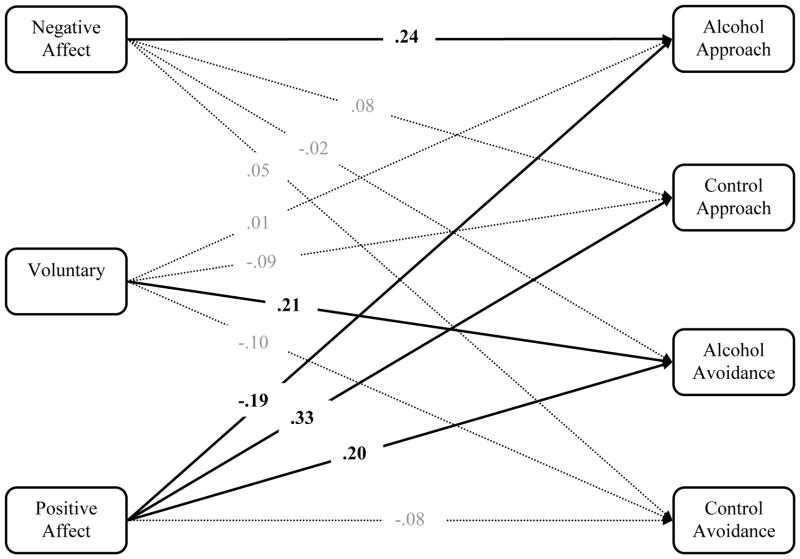
Results indicated a significant relationship between negative affect and alcohol approach ratings, but not for control cues, such that higher scores on negative affect were associated with higher approach ratings for alcohol (see Figure 2 and Table 4 for summary of results). Further, after constraining the paths to be equal, a chi-square difference test was non-significant (χ2(1) = 3.2, p= .072); however, consistent with our hypothesis, the pattern of results suggested that negative affect may differentially predict approach inclinations for alcohol cues when compared to control cues. There were no significant relationships between negative affect and avoidance ratings for alcohol or control cues. Results also indicated a significant relationship between positive affect and approach ratings for both alcohol and control cues, such that higher scores on positive affect were associated with lower approach ratings for alcohol and higher approach ratings for control cues. Further, a chi-square difference test indicated that the two paths were significantly different from one another (χ2(1) = 15.5, p= .000), suggesting that positive affect differentially predicted approach inclinations for alcohol cues when compared to control cues. In addition, positive affect was significantly associated with avoidance ratings for alcohol cues, but not control cues, such that higher scores on positive affect were associated with higher avoidance ratings for alcohol. Finally, results indicated that the two paths were significantly different from one another (χ2(1) = 5.4, p= .020), suggesting that positive affect differentially predicted avoidance inclinations for alcohol cues when compared to control cues.
Figure 2.
Summary of Standardized Estimates for the Alcohol Cue Analysis (n=129). Note: Covariances and residual variance estimates are not presented for ease of presentation.
Table 4.
Summary of results from multivariate regression analyses: Unstandardized estimates, standard errors, and standardized estimates.
| Alcohol (n=129) | Cigarettes (n=116) | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Estimate | SE | p-value | Estimate | SE | p-value | |
| NA -> Substance AP | .07 | .03 | .005 | .08 | .02 | .001 |
| NA -> Control AP | .02 | .02 | .339 | .01 | .02 | .482 |
| Voluntary -> Substance AP | .07 | .44 | .868 | −.48 | .41 | .246 |
| Voluntary -> Control AP | −.32 | .30 | .276 | −.34 | .33 | .295 |
| PA -> Substance AP | −.06 | .03 | .028 | −.04 | .02 | .114 |
| PA -> Control AP | .07 | .02 | .000 | .06 | .02 | .001 |
| NA -> Substance AV | −.01 | .02 | .781 | −.01 | .02 | .789 |
| NA -> Control AV | .01 | .02 | .584 | .03 | .02 | .148 |
| Voluntary -> Substance AV | 1.04 | .42 | .012 | .61 | .44 | .167 |
| Voluntary -> Control AV | −.35 | .30 | .235 | −.36 | .33 | .268 |
| PA -> Substance AV | .06 | .02 | .018 | .06 | .02 | .013 |
| PA -> Control AV | −.02 | .02 | .364 | −.01 | .02 | .616 |
Note. PA = PANAS Positive Affect, NA = PANAS Negative Affect, AP = Approach Reactivity, AV = Avoidance reactivity, Voluntary = Voluntarily admitted to unit (0=no, 1=yes), Substance = Alcohol or Cigarettes depending on sample used in analysis.
p <.05,
p<.01
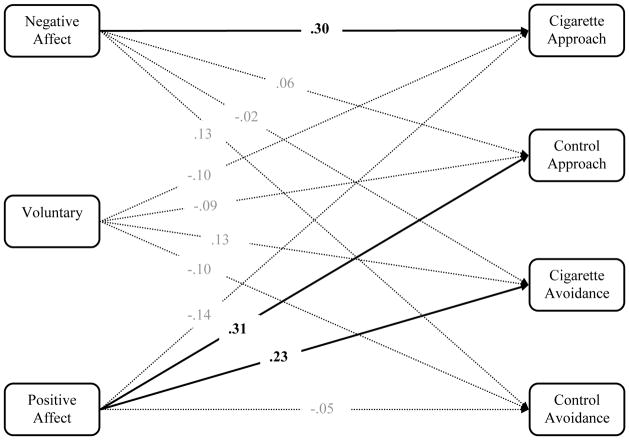
3.2. Cigarette Approach and Avoidance Reactivity Ratings
Results indicated a significant relationship between negative affect and approach ratings for cigarettes, but not control cues, such that higher scores on negative affect were associated with higher approach ratings for cigarettes (see Figure 3 and Table 4 for summary of results). Further, a chi-square difference indicated a significant difference between the two approach rating paths (χ2(1) = 4.5, p = .034), suggesting that negative affect was differentially associated with approach inclinations toward cigarette cues when compared to control cues. There were no significant relationships between negative affect and avoidance ratings for cigarette or control cues. Results also indicated a significant relationship between positive affect and approach ratings for control cues. Although the relationship between positive affect and approach ratings for cigarette cues were non-significant, a chi-square difference test indicated that the two paths were significantly different from one another (χ2(1) = 9.9, p = .002), suggesting that positive affect was differentially associated with approach inclinations for cigarette cues when compared to control cues (i.e., decreased approach inclinations for cigarette cues). In addition, positive affect was also significantly associated with avoidance ratings for cigarette cues, but not control cues, such that higher scores on positive affect were associated with higher avoidance ratings for cigarettes. Finally, results indicated that the two paths were significantly different from one another (χ2(1) = 5.6, p =.018), suggesting that positive affect was differentially associated with avoidance inclinations toward cigarette cues when compared to control cues.
Figure 3.
Summary of Standardized Estimates for the Cigarette Cue Analysis (n=116). Note: Covariances and residual variance estimates are not presented for ease of presentation.
4. Discussion
We examined the relationship between affect and craving within the context of a novel theoretical model of craving that conceptualizes approach (desire to consume a substance) and avoidance (desire not to consume a substance) as two orthogonal dimensions within subjective craving experiences (Breiner et al., 1999; Stritzke et al., 2007). Although the role of negative affect in precipitating or potentiating inclinations to use psychoactive substances -- particularly alcohol and tobacco use -- is well established, relatively little attention has been given to how positive affect might moderate inclinations to use (i.e., approach inclinations) or not use substances of abuse (i.e., avoidance inclinations). The current study sought to address these issues by completely crossing the two dimensions embodied in the Ambivalence Model of Craving with the two dimensions of affect within a clinical sample of patients from a detoxification center for those with substance use disorders.
Perhaps the most novel finding from the study emerged in the association between positive affect and approach and avoidance inclinations. As predicted, participants with higher levels of positive affect at baseline reported significantly lower approach inclinations for alcohol and showed a similar trend toward lower desire to smoke cigarettes relative to control cues. Also as predicted, those high in positive affect at baseline reported significantly higher inclinations to avoid both alcohol and cigarettes relative to control cues. The relationship between positive affect and cue-elicited reactivity is a novel finding as it suggests that positive affect may moderate both the desire to use and the desire to avoid using problem substances. Interestingly, research suggests that positive affect may be associated with a greater capacity for self-regulation (e.g., Tice et al., 2007), including greater restraint on smoking behavior following a self-control depletion task (Shmueli & Prochaska, 2012). Such findings may be due to increased avoidance inclinations, which may protect against relapse (Stritzke et al., 2007). In this connection, one might speculate that participants with higher positive affect were not only entertaining more non-drug options while in the detoxification facility, but if they could sustain this positive state upon release, might also be in a better position to apply more functional alternatives or engage in better self-regulation where avoidance of further substance use is concerned. Such a notion is consistent with Fredrickson’s (2001) broaden-and-build theory of positive affect, which asserts that positive affect can broaden individuals’ cognitive capacity in such a way to broaden one’s repertoire of coping options. Indeed, research suggests that positive affect is associated with enhanced cognitive flexibility (Garland, 2010) such that individuals experiencing positive affect are more open to information (Estrada, Isen, & Young, 1997), and are more creative and integrative in their thinking (Isen, Rosenzweig, & Young, 1991).
Also as predicted, participants experiencing higher levels of negative affect showed significantly increased approach inclinations for both alcohol and cigarettes, compared to approach of control cues. In contrast, higher levels of negative affect were not associated with lower avoidance inclinations for either alcohol or cigarettes. It is possible that the sample and the setting in which the study was conducted may have restricted the variability on avoidance ratings, such that the relatively unpleasant experience of a detoxification unit may have resulted in uniformly high levels of avoidance inclinations. Nevertheless, the divergence of approach and avoidance inclinations does lend further support to the validity of assessing both dimensions within subjective craving experiences. Without such a distinction between craving (approach inclinations) and concurrently activated competing desires to not use (avoidance inclinations), some key differences observed in this study would have been obscured. Further, despite non-significant effects of negative affective state on avoidance ratings, results of the approach ratings were consistent with previous research examining the relationship between negative affect and both alcohol and cigarette cue-elicited craving (e.g., Cooney et al., 1997; Fox et al., 2007; Conklin & Perkins, 2005; Maude-Griffin & Tiffany, 1996).
In sum, results of this study indicated that affective state moderates responses to psychoactive substance cues, such that individuals with higher positive affect are better able to manage craving experiences than those low in positive affect, both in terms of approach and avoidance inclinations, and necessitate that clinicians attend to the role of both positive and negative affect in relapse prevention. The current findings suggest that at least equal attention be given to enhancing positive affect, because of positive affect’s potential benefits on decreased approach inclinations and increased avoidance inclinations. Hence, it is encouraging to see that most contemporary cognitive-behavior therapies incorporate a “behavioral activation” component aimed specifically at enhancing positive affect. In many ways, such strategies are consonant with the “lifestyle balance” prescription for relapse prevention outlined by Marlatt and Gordon (1985; also see Marlatt & Witkiewitz, 2005) more than a quarter century ago. In both the original model and its adaptation, “positive addictions” such as exercise and meditation, and a host of other interventions that arguably lead to higher levels of positive affect, are encouraged. Given that higher positive affect was most strongly associated with elevated avoidance ratings in the present study, more effort directed at improving positive affect in SUD clients could have benefits. At the very least, it appears appropriate to deliberately attune patients in SUD treatment to how fluctuations in positive and negative affect might influence their craving and ability to manage it successfully.
4.1. Limitations and Future Directions
Although this study offered some insights that could advance understanding of the relationship between affective states and craving, it is not without limitations. Our use of an inpatient sample provided an opportunity for greater generalization to clinical SUD populations, but this particular inpatient sample had some features that might limit the generalizability to other substance dependent samples. First, participants were recruited from an acute detoxification facility where stays were short and many may not be fully detoxified at the time of participation, so the effects of their withdrawal status on responses to the research protocol are unknown and may differ from those in later stages of treatment or recovery. For example, acute withdrawal likely elicits negative affect and the use of medications to control such withdrawal symptoms may impact general arousal ratings and subsequent craving responses. However, such concerns appear to be mitigated by several factors. Negative affect experienced in the context of withdrawal may simply serve to perpetuate subsequent craving experiences (e.g., Kavanagh et al., 2005) rather than confound the current findings. In addition, there is literature suggesting that those in withdrawal and receiving detoxification medication (i.e., Librium) do not differ on cue-elicited approach craving compared to those not requiring detoxification (Monti, Rohsenow, Rubonis, Niaura, Sirota, Colby, & Abrams 1993). In fact, findings from Monti and colleagues (1993) suggest that the greatest reactivity to cues occur early in treatment and such effects were not moderated by withdrawal status. Thus, one could argue that early on in the detoxification process (i.e., 2.2 days on average) reactivity ratings would be enhanced rather than attenuated. In addition, the novel findings in the current study, namely the effect of positive affect on both approach and avoidance reactivity, are less likely to be the result of withdrawal states. In some respects, results demonstrating significant relationships between positive affective and increased avoidance inclinations are remarkable considering the population under investigation. Nevertheless, as this is the first study to examine both positive and negative affect’s impact on approach and avoidance dimensions of cue-elicited craving, future research is needed to fully understand these relationships.
Second, many patients in our sample were poly-substance users and we were not in a position to evaluate all of their other dependencies or how they might interact with alcohol and/or tobacco abuse and dependence. Further, it is likely that participants were representative of other substance abusing populations with comorbid psychiatric disorders, including mood, anxiety, and personality disorders. However, it is important to note that individuals in acute distress (e.g., suicidal) or actively psychotic are not admitted to the treatment unit. Unfortunately we were not in a position to collect information on clinical diagnoses and thus the effect of comorbidity could not be evaluated. Future research would benefit from understanding the factors that may moderate the relationship between affect and craving, particularly individual difference factors, such as personality and comorbid psychopathology.
Third, approximately 34% of patients in our sample were admitted involuntarily and might have been without a clear intention to change their substance use or enter formal treatment after discharge from detoxification, despite the vast majority self-reporting desires to reduce or cease use of psychoactive substances. Obviously, participants who were not actively trying to curtail their psychoactive substance use might respond differently than those seeking to change and we had no way of directly controlling for this. It is interesting to note that those who “voluntarily” entered treatment demonstrated greater avoidance inclinations toward alcohol compared to those who were mandated, a finding consistent with previous research demonstrating significant associations between avoidance inclinations and taking steps to make a change (Schlauch et al., 2012; Klein et al., 2007). Nevertheless, considering the fact that some form of coercion is not an uncommon aspect of many allegedly “voluntary” forays into treatment, perhaps our sample was not so different from the norm. In any case, additional research will be needed to address these sampling issues.
Another limitation is that the relationships of interest were examined by means of a correlational design. Although baseline positive affect was associated with decreased approach and increased avoidance ratings, and baseline negative affect with increased approach ratings, it cannot be said for certain that variations in these ratings were directly attributable to or caused by participants’ affective states. In addition, the current study relied on self-report assessments of approach and avoidance in response to pictorial cues and affective states due to the setting in which the research was conducted. Further experimental investigations will be needed to determine how direct manipulation of affect might cause changes in the two dimensions within the craving experience, including multi-method assessments of both cue-elicited reactivity and affective states. It is also important to note that the current study was concerned with the impact of affect on future craving experiences, rather than affective states in response to cue-elicited craving. This is an important distinction as cues associated with substance use not only elicit craving responses, but also affective states associated with such experiences (e.g., Nosen, Nillni, Berenz, Schumacher, Stasiewicz, & Coffey, 2012). Future research should explore the reciprocal relationships between affect and craving, as well as conduct longer-term follow-up evaluation of the predictive utility of both affective states and approach and avoidance inclinations in substance abuse relapse. These limitations notwithstanding, the results of the present study call for further investigation of the association between affect, and particularly positive affect, and the approach and avoidance inclinations. Additional research in this area holds promise for improving clinical interventions for SUDs.
Table 3.
Means, standard deviations, and bivariate correlations for variables in each path analysis
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Alcohol (n=129) | |||||||||
| 1. PA | 30.0 | 8.5 | -- | −.18* | −.23** | .31** | .21* | −.10 | .07 |
| 2. NA | 27.2 | 8.4 | -- | .27** | .02 | −.06 | .06 | −.01 | |
| 3. Alcohol AP | 3.3 | 2.5 | -- | −.02 | −.23** | .15 | .01 | ||
| 4. Control AP | 4.7 | 1.7 | -- | .18* | −.26** | −.07 | |||
| 5. Alcohol AV | 5.5 | 2.3 | -- | −.14 | .23** | ||||
| 6. Control AV | 2.5 | 1.6 | -- | −.11 | |||||
| 7. Voluntary | .66 | .46 | -- | ||||||
| Cigarettes (n=116) | |||||||||
| 1. PA | 29.5 | 8.9 | -- | −.10 | −.19* | .28** | .25** | −.08 | .20* |
| 2. NA | 24.2 | 8.7 | -- | .31** | .03 | −.05 | .14 | −.01 | |
| 3. Cigarette AP | 5.9 | 2.2 | -- | −.10 | −.53** | .08 | −.13 | ||
| 4. Control AP | 4.6 | 1.7 | -- | .21* | −.23* | −.04 | |||
| 5. Cigarette AV | 3.0 | 2.3 | -- | .05 | .17 | ||||
| 6. Control AV | 2.6 | 1.7 | -- | −.11 | |||||
| 7. Voluntary | .66 | .47 | -- | ||||||
Note. PA = PANAS Positive Affect, NA = PANAS Negative Affect, AP = Approach Reactivity, AV = Avoidance reactivity, Voluntary = Voluntarily admitted to unit (0=no, 1=yes)
p <.05,
p<.01
Highlights.
We examined the effect of negative and positive affect on cue-elicited craving.
Negative affect predicted increased approach inclinations for alcohol and cigarettes.
Positive affect predicted decreased approach inclinations for alcohol.
Positive affect predicted increased avoidance inclinations for alcohol and cigarettes.
Findings underscore the utility of a multidimensional conceptualization of craving.
Acknowledgments
Role of Funding Source
Funding for this study and write-up of this manuscript was provided by NIAAA Grant T32-AA007583. NIAAA had no further role in study design; in the collection, analysis, and interpretation of data; in writing this manuscript, or in the decision to submit the paper for publication.
We thank Dr. Jay A. Reeve for his support during data collection, and Stefanie Caggiano and Megan Hickox for their assistance in data collection and entry.
Footnotes
Contributors
Robert C. Schlauch and Alan R. Lang designed the study. Daniel Gwynn-Shapiro served as project coordinator and conducted literature searches. Robert C. Schlauch, Daniel Gwynn-Shapiro, and Alan R. Lang conceptualized the manuscript, and Robert C. Schlauch conducted all statistical analyses. Paul R. Stasiewicz and Danielle S. Molnar contributed to the discussion sections and provided feedback on manuscript drafts. All authors contributed to and have approved the final manuscript.
Conflict of Interest
No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anton RF. Alcohol craving – a renaissance. Alcoholism: Clinical and Experimental Research. 1999;23:1287–1288. doi: 10.1111/j.1530-0277.1999.tb04348.x. [DOI] [PubMed] [Google Scholar]
- Baker TB, Morse E, Sherman JE. The motivation to use drugs: A Psychobiological analysis of urges. In: Rivers C, editor. The Nebraska Symposium on Motivation: Vol. 34, Alcohol and addictive behavior. Lincoln: University of Nebraska Press; 1987. pp. 257–323. [PubMed] [Google Scholar]
- Baker TB, Piper M, McCarthy D, Majeskie M, Fiore M. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Barkby H, Dickson JM, Roper L, Field M. To approach or avoid alcohol? Automatic and self-reported motivational tendencies in alcohol dependence. Alcoholism: Clinical and Experimental Research. 2012;36:361–368. doi: 10.1111/j.1530-0277.2011.01620.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breiner MJ, Stritzke WGK, Lang AR. Approaching avoidance: a step essential to the understanding of craving. Alcohol Research & Health. 1999;23:197–206. [PMC free article] [PubMed] [Google Scholar]
- Cahalan D, Cisin IH, Crossley HM. American drinking practices: A national study of drinking behavior and attitudes. Monographs of the Rutgers Center of Alcohol Studies. 1969;6:260. [Google Scholar]
- Cacioppo JT, Gardner WL, Berntson GG. The affect system has parallel and integrative processing components: form follows function. Journal of Personality and Social Psychology. 1999;76:839–855. [Google Scholar]
- Carter BL, Tiffany ST. Meta-analysis of cue-reactivity in addiction research. Addiction. 1999;94:327–340. [PubMed] [Google Scholar]
- Conklin CA, Perkins KA. Subjective and reinforcing effects of smoking during negative mood induction. Journal of abnormal psychology. 2005;114:153–164. doi: 10.1037/0021-843X.114.1.153. [DOI] [PubMed] [Google Scholar]
- Cooney NL, Litt MD, Morse PA, Bauer LO, Gaupp L. Alcohol cue reactivity, negative-mood reactivity, and relapse in treated alcoholic men. Journal of Abnormal Psychology. 1997;106:243–250. doi: 10.1037//0021-843x.106.2.243. [DOI] [PubMed] [Google Scholar]
- Curtin JJ, Barnett NP, Colby SM, Rohsenow DJ, Monti PM. Cue reactivity in adolescents: measurement of separate approach and avoidance reactions. Journal of Studies on Alcohol. 2005;66:332–343. doi: 10.15288/jsa.2005.66.332. [DOI] [PubMed] [Google Scholar]
- de Wit H, Phan L. Positive reinforcement theories of drug use. In: Kassel JD, editor. Substance abuse and emotion. Washington, DC: American Psychological Association; 2010. pp. 83–108. [Google Scholar]
- Estrada CA, Isen AM, Young MJ. Positive affect facilitates integration of information and decreases anchoring in reasoning among physicians. Organizational Behaviour and Human Decision Processes. 1997;72:117–135. [Google Scholar]
- Fox HC, Berquist kL, Hong KI, Sinha R. Stress-induced and alcohol cue-induced craving in recently abstinent alcohol-dependent individuals. Alcoholism: Clinical and experimental research. 2007;31:395–403. doi: 10.1111/j.1530-0277.2006.00320.x. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist. 2001;56:218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Fredrickson B, Kring AM, Johnson DP, Meyer PS, Penn DL. Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review. 2010;30:849–864. doi: 10.1016/j.cpr.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin DR, Ross HE, Skinner HA. Diagnostic validity of the DAST in the assessment of DSM-III drug disorders. British Journal of Addiction. 1989;84:301–307. doi: 10.1111/j.1360-0443.1989.tb03463.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hays RD, Merz JF, Nicholas R. Response burden, reliability and validity of the CAFÉ, Short MAST, and AUDIT alcohol screening measures. Behavior research methods, instruments, & computers. 1995;27:277–280. [Google Scholar]
- Heather N. A conceptual framework for explaining drug addiction. Journal of Psychopharmacology. 1998;12:3–7. doi: 10.1177/026988119801200101. [DOI] [PubMed] [Google Scholar]
- Isen AM, Rosenzweig AS, Young MJ. The influence of positive affect on clinical problem solving. Medical Decision Making. 1991;11:221–227. doi: 10.1177/0272989X9101100313. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2009 (NIH Publication No. 10–7583) Bethesda, MD: National Institute on Drug Abuse; 2010. [Google Scholar]
- Kassel JD, Veilleux JC. Introduction: The complex interplay between substance abuse and emotion. In: Kassel JD, editor. Substance abuse and emotion. Washington, DC: American Psychological Association; 2010. pp. 83–108. [Google Scholar]
- Kavanagh DJ, Andrade J, May J. Imaginary relish and eexquisite torture: The elaborated intrusion theory of desire. Psychological Review. 2005;112:446–467. doi: 10.1037/0033-295X.112.2.446. [DOI] [PubMed] [Google Scholar]
- Kavanagh DJ, Statham DJ, Feeney GFX, Young RMD, May J, Andrade J, Connor JP. Measurement of alcohol craving. Addictive Behaviors. 2012 doi: 10.1016/j. addbeh.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Klein AA, Stasiewicz PR, Koutsky JR, Bradizza CM, Coffey SF. A psychometric evaluation of the Approach and Avoidance of Alcohol Questionnaire (AAAQ) in alcohol dependent outpatients. Journal of Psychopathology and Behavior Assessment. 2007;4:231–240. [Google Scholar]
- Lang PJ. The emotion probe: Studies of motivation and attention. American Psychologist. 1995;50:372–385. doi: 10.1037//0003-066x.50.5.372. [DOI] [PubMed] [Google Scholar]
- LeDoux J. Emotion circuits in the brain. Annual Review of Neuroscience. 2000;23:155–184. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- Leshner AI. Drug abuse and addiction treatment research. Archives of General Psychiatry. 1997;54:691–694. doi: 10.1001/archpsyc.1997.01830200015002. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR, editors. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 1985. [Google Scholar]
- Marlatt GA, Witkiewitz K. Relapse Prevention for Alcohol and Drug Problems. In: Marlatt GA, Donovan DM, editors. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. 2. Guilford Press; New York, NY: 2005. [Google Scholar]
- Mason BJ, Light JM, Escher T, Drobes DJ. Effect of positive and negative affective stimuli and beverage cues on measures of craving in non treatment-seeking alcoholics. Psychopharmacology. 2008;200(1):141–150. doi: 10.1007/s00213-008-1192-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maude-Griffin PM, Tiffany ST. Production of smoking urges through imagery: The impact of affect and smoking abstinence. Experimental and clinical psychopharmacology. 1996;4:198–208. [Google Scholar]
- McEvoy P, Stritzke WGK, French DJ, Lang A, Ketterman RL. Comparison of three models of alcohol craving in young adults: A cross-validation. Addiction. 2004;99:482–497. doi: 10.1111/j.1360-0443.2004.00714.x. [DOI] [PubMed] [Google Scholar]
- Monti PM, Rohsenow DJ, Rubonis AV, Niaura RS, Sirota AD, Colby SM, Abrams DB. Alcohol cue reactivity: Effects of detoxification and extended exposure. Journal of studeies on alcohol. 1993;54:235–245. doi: 10.15288/jsa.1993.54.235. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 2011. [Google Scholar]
- Nosen E, Nillni YI, Berenz EC, Schumacher JA, Stasiewicz PR, Coffey SF. Cue-elicited affect and craving: Advancement of the conceptualization of craving in co-occuring posttraumatic stress disorder and alcohol dependence. Behavior modification. doi: 10.1177/0145445512446741. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orford J. Excessive appetites: A psychological view of addictions. 2. New York, NY: Wiley; 2001. [Google Scholar]
- Perkins KA, Grobe JE. Increased desire to smoke during acute stress. British journal of addiction. 1992;87:1037–1040. doi: 10.1111/j.1360-0443.1992.tb03121.x. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. The neural basis of craving: An incentive-sensitization theory of addiction. Brain research reviews. 1993;18:247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- Sayette M, Shiffman S, Tiffany S, Niaura R, Martin C, Shadel W. The measurement of drug craving. Addiction. 2000;95:S189–S210. doi: 10.1080/09652140050111762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlauch RC, Levitt A, Bradizza CM, Stasiewicz PR, Maisto SA, Zhuo Y, Connors GJ. Approach and avoidance dimensions of craving predict drinking following treatment initiation in patients diagnosed with a severe mental illness and alcohol use disorder. Alcoholism: Clinical and experimental research. 2012;35(6):227A. supplement to June 2012. [Google Scholar]
- Schlauch RC, Breiner MJ, Stasiewicz PR, Christensen RL, Lang AR. Women inmate substance abusers’ reactivity to visual alcohol, cigarette, marijuana, and crack- cocaine cues: Approach and avoidance as separate dimensions of reactivity. Journal of psychopathology and behavioral assessment. 2012 doi: 10.1007/s10862-012-9313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlauch RC, Stasiewicz PR, Bradizza CM, Gudleski GD, Coffey SF, Gulliver SB. Relationship between approach and avoidance inclinations to use alcohol and treatment outcomes. Addictive Behaviors. 2012;37:824–830. doi: 10.1016/j.addbeh.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selzer ML, Vinokur A, Rooijen L. A Self-Administered Short Michigan Alcoholism Screening Test (SMAST) Journal of Studies on Alcohol. 1975;36:117–126. doi: 10.15288/jsa.1975.36.117. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Grekin ER. Alcohol and affect regulation. In: Gross JJ, editor. Handbook of emotion regulation. New York: Guilford Press; 2007. pp. 560–580. [Google Scholar]
- Shmueli D, Prochaska JJ. A test of positive affect induction for countering self- control depletion in cigarette smokers. Psychology of addictive behaviors. 2011;26:157–161. doi: 10.1037/a0023706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA. The drug abuse screening test. Addictive Behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Smith-Hoerter KE, Stasiewicz PR, Bradizza CM. Subjective reactions to alcohol cue exposure: A qualitative analysis of patients’ self-reports. Psychology of Addictive Behaviors. 2004;18:402–406. doi: 10.1037/0893-164X.18.4.402. [DOI] [PubMed] [Google Scholar]
- Stasiewicz PR, Maisto SA. Two-factor avoidance theory: The role of negative affect in the maintenance of substance use and substance use disorder. Behavior Therapy. 1993;24:337–356. [Google Scholar]
- Stewart J, de Witt H, Eikelboom R. Role of unconditioned and conditioned drug effects in the self-administration of opiates and stimulants. Psychological Review. 1994;91:251–268. [PubMed] [Google Scholar]
- Stritzke WGK, Breiner MJ, Curtin JJ, Lang AR. Assessment of substance cue reactivity: Advances in reliability, specificity, and validity. Psychology of Addictive Behaviors. 2004;18:148–159. doi: 10.1037/0893-164X.18.2.148. [DOI] [PubMed] [Google Scholar]
- Stritzke WGK, McEvoy PM, Wheat LR, Dyer KR, French DJ. The yin and yang of indulgence and restraint: The ambivalence model of craving. In: O’Neal PW, editor. Motivation of health behavior. Hauppauge, NY: Nova Science Publishers, Inc; 2007. pp. 31–47. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings (Office of Applied Studies, NSDUH Series H-38A, HHS Publication No. SMA 10–4856Findings) Rockville, MD: 2010. [Google Scholar]
- Tice DM, Baumeister RF, Shmueli D, Muraven M. Restoring the self: Positive affect helps improve self-regulation following ego depletion. Journal of experimental social psychology. 2007;43:379–384. [Google Scholar]
- Tiffany ST. Drug craving and Affect. In: Kassel JD, editor. Substance abuse and emotion. Washington, DC: American Psychological Association; 2010. pp. 83–108. [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: Role of automatic and nonautomatic processes. Psychological Review. 1990;97:147–168. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Conklin CA. A cognitive processing model of alcohol craving and compulsive alcohol use. Addiction. 2000;95:S145–S153. doi: 10.1080/09652140050111717. [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Drobes DJ. Imagery and smoking urges: The manipulation of affective content. Addictive Behaviors. 1990;15:531–539. doi: 10.1016/0306-4603(90)90053-z. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]