Abstract
Background
A superior cavopulmonary connection is commonly performed before the Fontan procedure in patients with a functionally univentricular heart. Data are limited regarding associations between a prior superior cavopulmonary connection and functional and ventricular performance late after the Fontan procedure.
Methods
We compared characteristics of those with and without prior superior cavopulmonary connection among 546 subjects enrolled in the Pediatric Heart Network Fontan Cross-Sectional Study. We further compared different superior cavopulmonary connection techniques: bidirectional cavopulmonary anastomosis (n equals 229), bilateral bidirectional cavopulmonary anastomosis (n equals 39), and hemi-Fontan (n equals 114).
Results
A prior superior cavopulmonary connection was performed in 408 subjects (75%); the proportion differed by year of Fontan surgery and centre (p-value less than 0.0001 for each). The average age at Fontan was similar, 3.5 years in those with superior cavopulmonary connection versus 3.2 years in those without (p-value equals 0.4). The type of superior cavopulmonary connection varied by site (p-value less than 0.001) and was related to the type of Fontan procedure. Exercise performance, echocardiographic variables, and predominant rhythm did not differ by superior cavopulmonary connection status or among superior cavopulmonary connection types. Using a test of interaction, findings did not vary according to an underlying diagnosis of hypoplastic left heart syndrome.
Conclusions
After controlling for subject and era factors, most long-term outcomes in subjects with a prior superior cavopulmonary connection did not differ substantially from those without this procedure. The type of superior cavopulmonary connection varied significantly by centre, but late outcomes were similar.
Keywords: Congenital heart disease, Fontan, functionally univentricular heart, quality of life
The Fontan procedure provides excellent surgical palliation for many patients with functionally univentricular physiology and has evolved over time.1 Performing a superior cavopulmonary connection before completion of the Fontan procedure has become more frequent. Volume unloading the univentricular heart at an earlier age is postulated to decrease morbidity at Fontan completion. Retrospective, single-centre reports suggest that early outcomes are improved in high-risk patients who had an intermediate superior cavopulmonary connection.2,3 Data are limited to determine whether a prior superior cavopulmonary connection results in improved late-term outcomes in patients who have undergone the Fontan procedure.
The Pediatric Heart Network Fontan Cross-Sectional database4 provides a very well-characterised cohort of surviving subjects from seven North American centres. We sought to determine whether long-term health status, medical complications, or laboratory measures of cardiac function differed between subjects who did and did not have an intermediate superior cavopulmonary connection. In addition, we compared subjects with different types of cavopulmonary connections to determine whether a particular technique is associated with superior outcomes. We hypothesised that subjects with an intermediate superior cavopulmonary connection would have more favourable long-term outcomes but that these outcomes would not vary by type of superior cavopulmonary connection technique.
Subjects and methods
Subjects were survivors of surgical palliation for functionally univentricular heart culminating in a Fontan procedure, who were age group of 6–18 years at the time of sampling. Medical records were screened for 1078 patients, of whom 831 (77%) were determined to be potentially eligible for participation. After being contacted, 637 patients (60%) were fully eligible, and consent was obtained from 546 (86%). Complete details of the study design have been previously published.5
Measurements
Standardised data forms were used to extract pertinent data from the medical record regarding details of cardiac anatomy, type of surgical repair, and both early and late complications since Fontan surgery, including onset of supraventricular or ventricular arrhythmias requiring treatment. Standardised assessment of functional health status was obtained using the Parent Report Child Health Questionnaire and the self-reported Child Report Child Health Questionnaire in subjects aged 10 years or older. Exercise performance was assessed using bicycle ergometry.6 Predominant rhythm was determined with 12-lead electrocardiograms. Ventricular size, function, atrioventricular valve, and semilunar valve regurgitation were obtained using centrally interpreted echocardiographic measurements. Echocardiographic quantitative variables were converted to z-scores based on body surface area with the use of published normal values and methods.7 Resting brain natriuretic peptide concentration was analysed at a core laboratory. Anthropometric z-scores were calculated using Centers for Disease Control algorithms.8
Statistical analysis
Exploratory analyses incorporating graphical and tabular displays assessed evidence in favour of trends and associations. Characteristics of subjects with and without superior cavopulmonary connection were compared with Student’s t- and chi-square test statistics. Generalised additive modelling was used to produce smooth estimates of the proportion of subjects with a superior cavopulmonary connection by calendar year. Subject characteristics among the three different superior cavopulmonary connection procedures were similarly compared. Covariable-adjusted comparisons were obtained using mixed-effects linear and logistic regression analyses, with the study site treated as a random intercept. Not all subjects completed all laboratory tests. Similar to other reports from this cohort, subjects were excluded from exercise analyses if maximal effort was not obtained (peak respiratory exchange ratio greater than or equal to 1.1) and subjects were excluded from echocardiographic analyses if no mass or volume data were available.9,10 Analyses were performed using SAS software version 9.2 (SAS Institute, Cary, North Carolina, United States of America) and the R system version 2.8.1 (R Foundation for Statistical Computing, Vienna, Austria).
Adjustment for covariates
We have learnt from previous study analyses that many of the results of tests performed at the time of cross-sectional evaluation differed among age groups. Exercise performance decreased with age.6 Echocardiographically measured mass-to-volume ratio, dP/dt, and Tei index also varied by age.4 Therefore, for outcomes measured at the time of cross-sectional testing – for example, functional health status, echocardiography, and exercise testing – age-adjusted comparisons are reported. Owing to the fact that the cohort of subjects having a superior cavopulmonary connection was younger and followed up for less time since Fontan completion, medical history variables collected since Fontan hospitalisation are also reported using age-adjusted comparisons. Medication use among subjects and frequency of certain catheter interventions varied considerably across the seven centres.11 Therefore, where centre or era differences might exist, we adjusted for subject age at Fontan cross-sectional enrolment, year that Fontan surgery was performed, and study centre. Owing to the fact that decisions regarding type of superior cavopulmonary connection may be influenced by the underlying functionally univentricular heart anatomy, specifically the presence of hypoplastic left heart syndrome, we examined whether any statistically significant differences in the analyses of superior cavopulmonary connection technique comparisons were modified by the presence or absence of hypoplastic left heart syndrome via a test of interaction.
The Fontan Cross-Sectional Study protocol was approved by the Pediatric Heart Network Protocol Review Committee and an independent Data and Safety Monitoring Board, as well as the Institutional/Ethics Review Boards at each of the seven clinical centres and the Data Coordinating Center. All centres followed the same protocol and study procedures.
Results
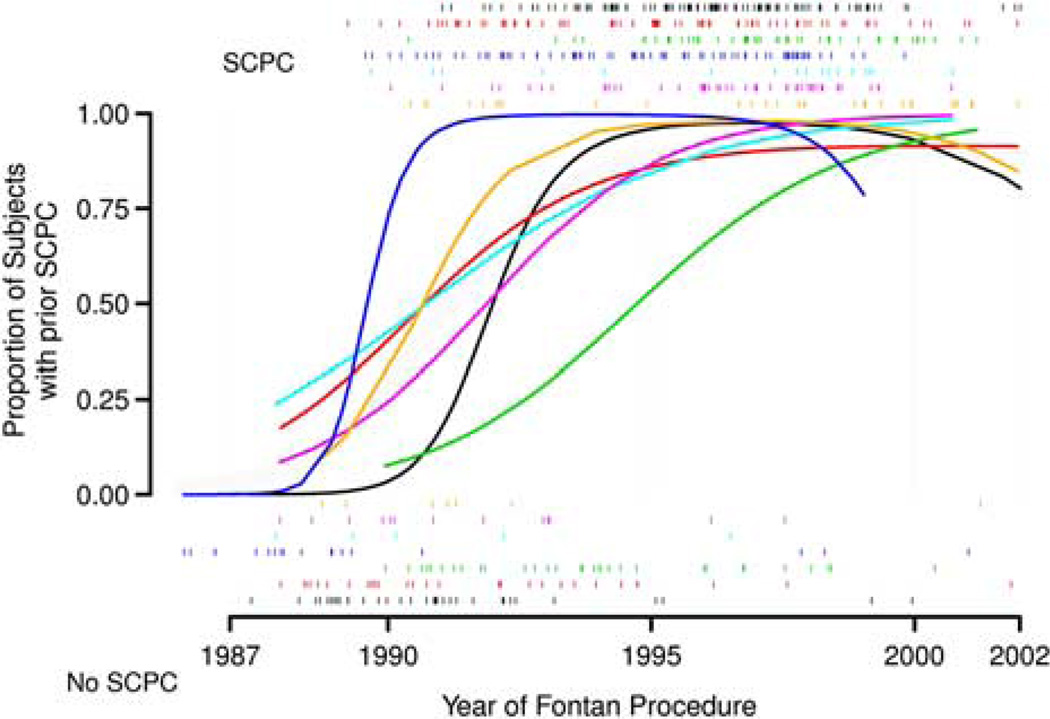
Medical record review recorded the performance of a superior cavopulmonary connection in 408 of the 546 subjects (75%). There was a rapid increase in the frequency of subjects with a superior cavopulmonary connection around 1990 (Fig 1). The use of a superior cavopulmonary connection increased over this time period at all centres (p-value less than 0.0001). After adjusting for year of Fontan and age at enrolment, the percentage of subjects having a superior cavopulmonary connection varied significantly among centres (61–82%, p-value less than 0.0001).
Figure 1.
Smoothed proportion of subjects with superior cavopulmonary connection (SCPC) by year and by clinical centre. Rug plots at the top and bottom record the dates of SCPC and no SCPC procedures, respectively. Estimates were obtained using generalised additive mixed models.
Medical history before the Fontan procedure
Subject characteristics and medical history before and at the Fontan procedure are shown in Table 1. Subjects with a previous superior cavopulmonary connection were more likely to have been born with hypoplastic left heart syndrome. The number of non-superior cavopulmonary connection cardiac surgeries performed before the Fontan procedure was higher in subjects with a prior superior cavopulmonary connection. Greater severity of atrioventricular valve regurgitation and a history of decreased ventricular function and arrhythmia before Fontan were more likely in those with a superior cavopulmonary connection. At the pre-Fontan catheterisation, subjects with a superior cavopulmonary connection had higher systemic arterial oxygen saturations (85 plus or minus 4% versus 82 plus or minus 6%), lower ventricular enddiastolic pressures (8 plus or minus 3 versus 9 plus or minus 3 millimetres of mercury), and lower mean pulmonary artery pressure (11 plus or minus 3 versus 13 plus or minus 4 millimetres of mercury, p-value less than 0.001 for all) compared with those without a superior cavopulmonary connection.
Table 1.
Subject characteristics through Fontan completion by superior cavopulmonary connection status.
| Superior cavopulmonary connection, mean ± standard deviation or % |
No superior cavopulmonary connection, mean ± standard deviation or % |
Adjusted p-value* |
|
|---|---|---|---|
| Medical history: before Fontan procedure | |||
| Total number of subjects | 408 | 138 | |
| Anatomy | 0.2 | ||
| Double inlet left ventricle (%) | 13 | 20 | 0.2 |
| Mitral atresia (%) | 6 | 5 | 0.7 |
| Tricuspid atresia (%) | 19 | 30 | 0.1 |
| Unbalanced atrioventricular septal defect (%) | 4 | 3 | 0.6 |
| Heterotaxy (%) | 7 | 9 | 0.4 |
| Hypoplastic left heart syndrome (%) | 26 | 5 | <0.001 |
| Other (%) | 25 | 28 | 0.1 |
| Prior non-superior cavopulmonary connection surgeries | 3.5 ± 1.8 | 1.5 ± 1.3 | <0.001 |
| Catheter interventions | 0.9 ± 1.2 | 0.4 ± 0.8 | 0.09 |
| Severity of atrioventricular valve regurgitation | 0.01 | ||
| None/trivial (%) | 61 | 79 | |
| Mild (%) | 33 | 20 | |
| Moderate/severe (%) | 7 | 1 | |
| End-diastolic pressure (mmHg) | 7.5 ± 3.4 | 8.9 ± 3.0 | <0.001 |
| Mean pulmonary artery pressure (mmHg) | 10.9 ± 2.8 | 13.2 ± 4.3 | <0.001 |
| Oxygen saturation (%) | 84.7 ± 4.4 | 81.8 ± 6.2 | <0.001 |
| Decreased ventricular function (%) | 20 | 10 | 0.008 |
| Arrhythmia (%) | 24 | 13 | 0.03 |
| Thrombosis (%) | 5 | 2 | 0.3 |
| Stroke (%) | 4 | 1 | 0.2 |
| Medical history: Fontan hospitalisation | |||
| Median length of hospital days (IQR) | 11 (8,17) | 14 (10,23) | 0.4 |
| Pericardial effusion (%) | 8 | 20 | 0.03 |
| Pleural effusion (%) | 26 | 27 | 0.4 |
| Number of discharge medications | 3.8 ± 1.7 | 3.6 ± 1.5 | 0.01 |
| Antithrombotic (%) | 71 | 55 | 0.009 |
| Angiotensin-converting enzyme inhibitor (%) | 58 | 33 | 0.7 |
| Diuretics (%) | 94 | 92 | 0.06 |
p-Value adjusted for centre, age at enrolment, year of Fontan, age at Fontan
Medical history at Fontan hospitalisation (Table 1)
The age at which the Fontan procedure was performed did not differ by superior cavopulmonary connection status, 3.5 plus or minus 2.0 years in those with a superior cavopulmonary connection versus 3.2 plus or minus 2.3 years in those without (p-value equals 0.4). After adjustments for era and centre differences, a substantially lower proportion of subjects with a superior cavopulmonary connection developed post-operative pericardial effusions. After adjustments, subjects with a prior superior cavopulmonary connection were discharged following the Fontan with more medications and were more likely to be prescribed antithrombotics.
Subject characteristics late after Fontan (Table 2)
Table 2.
Current subject characteristics by superior cavopulmonary connection status.
| Superior cavopulmonary connection, mean ± standard deviation or % (n) |
No superior cavopulmonary connection, mean ± standard deviation or % (n) |
Adjusted p-value* |
|
|---|---|---|---|
| Post-Fontan medical history | |||
| Total number of subjects | 408 | 138 | |
| Weight for age at study (percentile) | 38 ± 32 | 48 ± 31 | 0.05 |
| Height for age at study (percentile) | 33 ± 31 | 36 ± 28 | 0.1 |
| Number of surgeries | 0.4 ± 0.9 | 0.5 ± 1.1 | 0.05 |
| Stroke (%) | 2 | 1 | 0.02 |
| Thrombosis (%) | 6 | 11 | 0.01 |
| Protein-losing enteropathy (%) | 4 | 4 | 0.4 |
| Arrhythmia (%) | 18 | 28 | 0.5 |
| Child Health Questionnaire Physical Summary Score | 45 ± 12 (n = 380) | 45 ± 11 (n = 131) | 0.3 |
| Child Health Questionnaire Psychosocial Summary Score | 47 ± 11 (n = 380) | 49 ± 10 (n = 131) | 0.01 |
| Echocardiography | |||
| Ejection fraction (%) | 59 ± 11 (n = 318) | 58 ± 10 (n = 96) | 0.3 |
| Mass to volume ratio z-score | 1.2 ± 0.4 (n = 314) | 1.2 ± 0.4 (n = 92) | 0.3 |
| Exercise testing | |||
| Resting oxygen saturation (%) | 94 ± 4 (n = 291) | 94 ± 4 (n = 114) | 0.07 |
| Peak oxygen consumption (ml/kg/min) | 27 ± 6 (n = 109) | 27 ± 6 (n = 57) | 0.2 |
| Per cent predicted peak oxygen consumption | 67 ± 15 (n = 109) | 66 ± 14 (n = 57) | 0.2 |
| Peak oxygen consumption at ventilatory anaerobic threshold (ml/kg/min) | 18 ± 6 (n = 105) | 18 ± 5 (n = 57) | 0.6 |
| Per cent predicted peak oxygen consumption at ventilatory anaerobic threshold | 78 ± 23 (n = 105) | 75 ± 19 (n = 57) | 0.9 |
| Brain natriuretic peptide (pg/ml), mean | 23 ± 46 (n = 377) | 34 ± 53 (n = 133) | 0.7 |
| Brain natriuretic peptide (pg/ml), median (IQR) | 12 (7–23) | 18 (8–36) |
IQR5interquartile range
p-value adjusted for centre, age at enrolment, year of Fontan, age at Fontan
The mean age at study enrolment was 4 years younger among the subjects with a prior superior cavopulmonary connection as compared with those without (11 plus or minus 3 versus 15 plus or minus 3 years, p-value less than 0.001) and the mean time between Fontan completion and cross-sectional testing was 4 years shorter compared with those with superior cavopulmonary connection procedures (8 plus or minus 3 versus 12 plus or minus 3 years, p-value less than 0.001). Although height-for-age percentile was not different among groups, weight-for-age percentile was significantly lower in the superior cavopulmonary connection cohort (38 plus or minus 32 versus 48 plus or minus 31 percentile). Stroke occurring after the Fontan was rare, but more likely in those with a superior cavopulmonary connection (2% versus 1%, unadjusted). Conversely, thrombosis (6% versus 11%) and additional cardiac surgeries following Fontan completion were less likely in those with a superior cavopulmonary connection. The Psychosocial Summary Score derived from the Child Health Questionnaire was statistically significantly lower in those who underwent a superior cavopulmonary connection. We found an average of a 2-point difference between groups; however, a clinically meaningful difference is considered to be 5 points. This difference remained even within subgroups defined by a diagnosis of hypoplastic left heart syndrome and the presence versus absence of medical conditions captured on the Parent Report Child Health Questionnaire. In subjects 10 years and older who completed the Child Report Child Health Questionnaire, the mean score in the domain of general health perceptions was lower in subjects with a superior cavopulmonary connection (data not shown). We found no differences between groups in assessment of ventricular performance by echocardiography, exercise testing, or measurement of brain natriuretic peptide level.
Centre variability
Of the 408 subjects with a superior cavopulmonary connection, 13 subjects had more than one type of procedure performed – for example, hemi-Fontan with a left-sided bidirectional cavopulmonary anastomosis – and were excluded from analyses comparing superior cavopulmonary connection techniques. An additional 13 subjects were excluded because of low frequency of their superior cavopulmonary connection type: eight subjects with a classic Glenn and five subjects with a Kawashima procedure. The remaining 382 subjects had a bidirectional cavopulmonary anastomosis (n equals 229), a hemi-Fontan (n equals 114), or a bilateral bidirectional cavopulmonary anastomosis (n equals 39). There was substantial variation in the type of superior cavopulmonary connection procedures by clinical site and underlying anatomic diagnosis (Table 3). Of the seven participating centres, five centres primarily performed bidirectional cavopulmonary anastomosis procedures (69–88%) and two centres primarily performed hemi-Fontan procedures (66% and 90%).
Table 3.
Centres and underlying diagnosis by types of superior cavopulmonary connection procedures.
| Subjects (n = 382) |
Bidirectional cavopulmonary anastomosis (n = 229; %) |
Hemi-Fontan (n = 114; %) |
Bilateral bidirectional cavopulmonary anastomosis (n = 39; %) |
Adjusted p-value |
|
|---|---|---|---|---|---|
| Site | <0.0001* | ||||
| A | 95 | 88 | 3 | 8 | |
| B | 70 | 87 | 1 | 11 | |
| C | 47 | 81 | 4 | 15 | |
| D | 80 | 5 | 90 | 5 | |
| E | 17 | 59 | 29 | 12 | |
| F | 44 | 27 | 66 | 7 | |
| G | 29 | 69 | 7 | 24 | |
| Pre-Fontan anatomic diagnosis | <0.0001** | ||||
| Double inlet left ventricle | 50 | 72 | 24 | 4 | |
| Double inlet right ventricle | 6 | 33 | 50 | 6 | |
| Mitral atresia | 24 | 58 | 33 | 24 | |
| Tricuspid atresia | 69 | 72 | 25 | 3 | |
| Unbalanced atrioventricular septal defect | 18 | 67 | 11 | 22 | |
| Heterotaxy syndrome | 25 | 36 | 12 | 52 | |
| Hypoplastic left heart syndrome | 98 | 52 | 42 | 6 | |
| Other single ventricle | 92 | 60 | 30 | 10 |
Adjusted for age at enrolment, year of Fontan
Adjusted for site, age at enrolment, and year of Fontan
Comparisons of subjects according to the type of superior cavopulmonary connection (Table 4)
Table 4.
Subject characteristics by the type of superior cavopulmonary connection.
| Bidirectional cavopulmonary anastomosis (n = 229) |
Hemi-Fontan (n = 114) |
Bilateral bidirectional cavopulmonary anastomosis (n = 39) |
Adjusted p-value* |
|
|---|---|---|---|---|
| Pre-Fontan hospitalisation medical history | ||||
| History of arrhythmia before Fontan (%) | 27 | 10 | 41 | <0.001 |
| Fontan medical history | ||||
| Type of Fontan procedure | <0.0001 | |||
| Atriopulmonary connection (%) | 9 | 4 | 3 | |
| Intracardiac lateral tunnel (%) | 51 | 93 | 36 | |
| Extracardiac conduit (%) | 40 | 3 | 59 | |
| Other (%) | 0 | 1 | 3 | |
| Log of Fontan hospital stay | 2.5 ± 0.5 | 2.6 ± 0.9 | 2.6 ± 0.7 | 0.3 |
| Post-Fontan medical history | ||||
| Stroke (%) | 2 | 2 | 0 | 0.7 |
| Thrombosis (%) | 7 | 4 | 3 | 0.4 |
| Protein-losing enteropathy (%) | 4 | 2 | 8 | 0.2 |
| Post-Fontan arrhythmia (%) | 18 | 21 | 5 | 0.2 |
Adjusted for site, year of Fontan, age at Fontan, age at enrolment
A history of arrhythmia before the Fontan procedure, defined as the onset of supraventricular or ventricular arrhythmias requiring treatment, differed by superior cavopulmonary connection type, occurring in 10% with a hemi-Fontan, 27% in those with a bidirectional cavopulmonary anastomosis, and 41% in those with a bilateral bidirectional cavopulmonary anastomosis (adjusted p-value less than 0.001). The median age at Fontan completion was 2.2 years in those with a hemi-Fontan, 3.0 years in those with a bidirectional cavopulmonary anastomosis, and 3.7 years in those with a bilateral bidirectional cavopulmonary anastomosis (p-value less than 0.001). The type of superior cavopulmonary connection was associated with the type of Fontan performed (p-value less than 0.0001): the hemi-Fontan group was more likely to have Fontan completion via an intracardiac tunnel, 93% compared with 51% in those with a bidirectional cavopulmonary anastomosis and 36% in those with a previous bilateral bidirectional cavopulmonary anastomosis. The duration of cardiopulmonary bypass at Fontan completion differed across the superior cavopulmonary connection types (p-value less than 0.001): 76 plus or minus 36 minutes for hemi-Fontan, 117 plus or minus 45 minutes for bilateral cavopulmonary anastomosis, and 131 plus or minus 44 minutes for bilateral bidirectional cavopulmonary anastomosis. Concurrent surgical procedures done at the time of Fontan completion also differed by superior cavopulmonary connection type (p-value less than 0.001), occurring in 13% with a hemi-Fontan, 51% with a bilateral bidirectional cavopulmonary anastomosis, and 57% with a bidirectional cavopulmonary anastomosis. Although the proportion of subjects with post-operative complications was generally similar among the three groups, the incidence of chylothorax differed (p-value equals 0.03), affecting 4% with a hemi-Fontan, 11% with a bidirectional cavopulmonary anastomosis, and 13% with a bilateral bidirectional cavopulmonary anastomosis. The predominant rhythm for each type of superior cavopulmonary connection and Fontan procedure was normal sinus (62–69%) and did not differ substantially by either the type of superior cavopulmonary connection performed (Table 5) or by the type of Fontan performed (data not shown).
Table 5.
Predominant rhythm at study enrolment by the type of superior cavopulmonary connection.
| Bidirectional cavopulmonary anastomosis (n = 229) |
Hemi-Fontan (n = 114) |
Bilateral bidirectional cavopulmonary anastomosis (n = 39) |
Adjusted p-value* |
|
|---|---|---|---|---|
| Predominant rhythm | 0.3 | |||
| Normal sinus (%) | 69 | 62 | 63 | |
| Atrial escape (%) | 6 | 15 | 13 | |
| Junctional escape (%) | 5 | 8 | 0 | |
| Paced (%) | 8 | 10 | 11 | |
| Other (%) | 12 | 5 | 13 |
Adjusted for site, age at enrolment and type of Fontan procedures
Comparison of subjects according to the diagnosis of hypoplastic left heart syndrome
Among our cohort of Fontan subjects, 94% with an underlying diagnosis of hypoplastic left heart syndrome had a superior cavopulmonary connection performed. Therefore, we performed additional analyses to explore potential associations between pre-Fontan medical history and hypoplastic left heart syndrome versus other underlying diagnoses among all subjects having a superior cavopulmonary connection. Those with hypoplastic left heart syndrome had a greater number of cardiac surgical procedures between superior cavopulmonary connection and Fontan, p-value less than 0.001, but there were no differences in the history of arrhythmia, thrombosis, stroke, ventricular dysfunction, echo, or catheterisation variables between those with and without hypoplastic left heart syndrome (data not shown). Similarly, because decisions regarding the type of superior cavopulmonary connection may be influenced by the underlying functionally univentricular heart anatomy, specifically hypoplastic left heart syndrome, we examined whether any statistically significant differences in the analyses of superior cavopulmonary connection technique comparisons were modified by the presence or absence of hypoplastic left heart syndrome. Using a test of interaction, these results did not vary for those with and without an underlying diagnosis of hypoplastic left heart syndrome.
Comment
In 1990, the superior cavopulmonary connection was first described as an interim palliative procedure for candidates considered at high risk for a subsequent Fontan procedure.12 It has subsequently become widely used and single-centre studies have shown a survival advantage when employing a two-stage Fontan strategy.13,14 In our large multicentre cohort, 75% of subjects had an intermediate superior cavopulmonary connection before Fontan completion. The current study controlled for era effect by adjusting for subject age and year of Fontan and controlled for practice variation by adjusting for study centre. Although limited to a selected cohort of survivors of the Fontan procedure, this analysis identified few associations between an intermediate superior cavopulmonary connection procedure and improved later outcomes.
Associations with staged superior cavopulmonary connection in late follow-up
Decreasing chronic volume overload at a younger age will improve ventricular performance in subjects with a functionally univentricular heart.15,16 In a single-centre retrospective study, preadolescents with a functionally univentricular heart who underwent volume unloading surgery at an earlier age showed improved aerobic capacity compared with those with later unloading procedures.17 In the present study, the superior cavopulmonary connection was performed at a median age of 0.8 years; in the group without superior cavopulmonary connection, the Fontan was performed at a median of 3.5 years of age. Despite a significant difference in the timing of unloading surgery between groups, we could not demonstrate late differences in ventricular or exercise performance.
The superior cavopulmonary connection group had lower mean Psychosocial Summary Scores on the Parent Report Child Health Questionnaire despite adjustment for subject factors, which might confound the scores.We found an average of a 2-point difference between groups; however, a clinically meaningful difference is considered to be 5 points.18 This study cannot determine whether this finding is related to intrinsic subject factors or specifically to the superior cavopulmonary connection procedure. Future studies using an incident cohort established at birth may be able to more definitively evaluate this finding.
Comparison of superior cavopulmonary connection types
Comparisons between types of superior cavopulmonary connection procedures have been reported, but are largely limited to small, single-centre reports without adjustments for age and era effects. We found significant centre variation in the type of superior cavopulmonary connection performed. At the time of the Fontan procedure, the duration of cardiopulmonary bypass and incidence of chylothorax were lower in the hemi-Fontan group. This may reflect the need to do more extensive surgical dissection at the time of Fontan completion with a total cavopulmonary connection as compared with an intracardiac lateral tunnel completion. Despite these differences, we found that the length of Fontan hospital stay did not differ according to the type of superior cavopulmonary connection performed.
Considerable attention had been paid to sinus node function following superior cavopulmonary connection and Fontan procedures. Theoretically, certain procedures such as the hemi-Fontan and or lateral tunnel Fontan are associated with greater risk of sinus node dysfunction when compared with similar procedures that can be undertaken without surgery close to the sinus node, for example, bidirectional cavopulmonary anastomosis or extra-cardiac conduit. We found the opposite – a significantly lower proportion of subjects with arrhythmias before Fontan completion in those who had a hemi-Fontan compared with those with a bidirectional cavopulmonary anastomosis or bilateral bidirectional cavopulmonary anastomosis. Our finding was in contrast to a single-centre comparison among 51 patients with a bidirectional cavopulmonary anastomosis and 79 with a hemi-Fontan, which showed higher sinus node dysfunction on post-operative day 1 in the hemi-Fontan group. However, at the time of cross-sectional follow-up – on average 8 years after Fontan completion – this difference in arrhythmia frequency did not persist. Our long-term findings support previous studies showing no significant difference in the longterm underlying rhythm either by type of superior cavopulmonary connection or type of Fontan.19,20
Limitations
The study cohort was limited to subjects 6 years and older, who had survived the Fontan procedure and agreed to participate in this study. Furthermore, the associations of a superior cavopulmonary connection procedure on early or late mortality, if any, and short-term outcomes cannot be assessed in this cross-sectional study. Medical history before the cross-sectional evaluation was ascertained by retrospective review and must be viewed in the light of the limitations of this data source. The large majority of subjects with hypoplastic left heart syndrome had a superior cavopulmonary connection performed and those with hypoplastic left heart syndrome made up one-quarter of the superior cavopulmonary connection group. We found few differences after accounting for the underlying diagnosis of hypoplastic left heart syndrome, but the differences – or lack thereof – we did find could be related to the diagnostic imbalance between groups in this cross-sectional study. The types of superior cavopulmonary connection procedures performed were not randomly assigned and numbers particularly of bilateral bidirectional cavopulmonary anastomosis may be too small to detect significant differences. In addition, some outcomes were rare, which may limit the ability to detect associations.
Conclusions
This is the largest multicentre cohort to specifically explore the associations between a staged superior cavopulmonary connection and long-term outcomes in patients who have undergone the Fontan procedure. Among a selected group of patients who have survived a Fontan procedure, after controlling for subject and era factors, long-term outcomes in subjects with a superior cavopulmonary connection did not differ substantially from those without this procedure. The type of superior cavopulmonary connection procedure varied significantly by centre, but late outcomes were similar.
Acknowledgements
National Heart, Lung, and Blood Institute: Gail Pearson, Mario Stylianou, Judith Massicot-Fisher*, Marsha Mathis*, Victoria Pemberton. Data Coordinating Center: New England Research Institutes, Lynn Sleeper, Steven Colan, Paul Mitchell*, Dianne Gallagher, Patti Nash*, Gloria Klein, Minmin Lu, Thomas Travison*, Yanli Wang*, Shan Chen. Network Chair: Lynn Mahony, University of Texas Southwestern Medical Center. Clinical Site Investigators: Children’s Hospital Boston, Jane Newburger (PI), Stephen Roth*, Roger Breitbart, Jonathan Rhodes, Jodi Elder*, Ellen McGrath*; Children’s Hospital of New York, Welton M. Gersony (PI), Daphne T. Hsu*, Seema Mital*, Beth Printz*, Ashwin Prakash*, Darlene Servedio*; Children’s Hospital of Philadelphia, Victoria Vetter (PI), Bernard J. Clark*, Mark Fogel, Steven Paridon, Jack Rychik, Margaret Harkins*, Jamie Koh*; Duke University, Page A. W. Anderson (PI) – deceased, Rene Herlong*, Lynne Hurwitz, Jennifer S. Li, Ann Marie Nawrocki*; Medical University of South Carolina, J. Philip Saul (PI), Andrew M. Atz, Andrew D. Blaufox*, Girish Shirali, Jon Lucas*, Amy Blevins*; Primary Children’s Medical Center, Salt Lake City, Utah, LuAnn Minich (PI), Richard Williams, Linda Lambert, Michael Puchalski; Hospital for Sick Children, Toronto, Brian McCrindle (PI), Timothy Bradley, Kevin Roman*, Jennifer Russell, Shi-Joon Yoo, Elizabeth Radojewski, Nancy Slater. Echocardiography Core Laboratory: Children’s Hospital Boston: Steven Colan (Director), Marcy Schwartz*, Renee Margossian. Protocol Review Committee: Michael Artman, Chair; Dana Connolly, Timothy Feltes, Julie Johnson, Jeffrey Krischer, G. Paul Matherne. Data and Safety Monitoring Board: John Kugler (Chair); Kathryn Davis, David J. Driscoll, Mark Galantowicz, Sally A. Hunsberger, Thomas J. Knight, Catherine L. Webb, Lawrence Wissow. *No longer at the institution listed. Funding: Supported by U01 grants from the National Heart, Lung, and Blood Institute (HL068269, HL068270, HL068279, HL068281, HL068285, HL068292, HL068290, HL068288) This work is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health/ National Heart, Lung, and Blood Institute.
References
- 1.Khairy P, Poirier N, Mercier LA. Univentricular heart. Circulation. 2007;115:800–812. doi: 10.1161/CIRCULATIONAHA.105.592378. [DOI] [PubMed] [Google Scholar]
- 2.Bridges ND, Jonas RA, Mayer JE, Flanagan MF, Keane JF, Castaneda AR. Bidirectional cavopulmonary anastomosis as interim palliation for high-risk Fontan candidates. Early results. Circulation. 1990;82(5 Suppl):IV170–IV176. [PubMed] [Google Scholar]
- 3.Norwood WI, Jacobs ML. Fontan’s procedure in two stages. Am J Surg. 1993;166:548–551. doi: 10.1016/s0002-9610(05)81151-1. [DOI] [PubMed] [Google Scholar]
- 4.Anderson PA, Sleeper LA, Mahony L, et al. Contemporary outcomes after the Fontan procedure: a Pediatric Heart Network multicenter study. J Am Coll Cardiol. 2008;52:85–98. doi: 10.1016/j.jacc.2008.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sleeper LA, Anderson P, Hsu DT, et al. Design of a large cross-sectional study to facilitate future clinical trials in children with the Fontan palliation. Am Heart J. 2006;152:427–433. doi: 10.1016/j.ahj.2006.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paridon SM, Mitchell PD, Colan SD, et al. A cross-sectional study of exercise performance during the first 2 decades of life after the Fontan operation. J Am Coll Cardiol. 2008;52:99–107. doi: 10.1016/j.jacc.2008.02.081. [DOI] [PubMed] [Google Scholar]
- 7.Sluysmans T, Colan SD. Theoretical and empirical derivation of cardiovascular allometric relationships in children. J Appl Physiol. 2005;99:445–457. doi: 10.1152/japplphysiol.01144.2004. [DOI] [PubMed] [Google Scholar]
- 8.Kuczmarski RJ, Odgen CL, Grummer-Strawn LM. Hyattsville, Maryland: National Center for Health Statistics; 2000. CDC Growth Charts: United States. Advance Data from Vital and Health Statistics; No. 314. [Google Scholar]
- 9.McCrindle BW, Zak V, Sleeper LA, et al. Laboratory measures of exercise capacity and ventricular characteristics and function are weakly associated with functional health status after Fontan procedure. Circulation. 2010;121:34–42. doi: 10.1161/CIRCULATIONAHA.109.869396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atz AM, Zak V, Breitbart RE, et al. Factors associated with serum brain natriuretic peptide levels after the Fontan procedure. Congenit Heart Dis. 2011;6:313–321. doi: 10.1111/j.1747-0803.2011.00496.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson PA, Breitbart RE, McCrindle BW, et al. The Fontan patient: inconsistencies in medication therapy across seven pediatric heart network centers. Pediatr Cardiol. 2010;31:1219–1228. doi: 10.1007/s00246-010-9807-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lamberti JJ, Spicer RL, Waldman JD, et al. The bidirectional cavopulmonary shunt. J Thorac Cardiovasc Surg. 1990;100:22–29. [PubMed] [Google Scholar]
- 13.d’Udekem Y, Iyengar AJ, Cochrane AD, et al. The Fontan procedure: contemporary techniques have improved long-term outcomes. Circulation. 2007;116(11 Suppl):I157–I164. doi: 10.1161/CIRCULATIONAHA.106.676445. [DOI] [PubMed] [Google Scholar]
- 14.Attanavanich S, Limsuwan A, Vanichkul S, Lertsithichai P, Ngodngamthaweesuk M. Single-stage versus two-stage modified Fontan procedure. Asian Cardiovasc Thorac Ann. 2007;15:327–331. doi: 10.1177/021849230701500413. [DOI] [PubMed] [Google Scholar]
- 15.Uemura H, Yagihara T, Kawashima Y, et al. What factors affect ventricular performance after a Fontan-type operation? J Thorac Cardiovasc Surg. 1995;110:405–415. doi: 10.1016/S0022-5223(95)70237-7. [DOI] [PubMed] [Google Scholar]
- 16.Sluysmans T, Sanders SP, van d V, et al. Natural history and patterns of recovery of contractile function in single left ventricle after Fontan operation. Circulation. 1992;86:1753–1761. doi: 10.1161/01.cir.86.6.1753. [DOI] [PubMed] [Google Scholar]
- 17.Mahle WT, Wernovsky G, Bridges ND, Linton AB, Paridon SM. Impact of early ventricular unloading on exercise performance in preadolescents with single ventricle Fontan physiology. J Am Coll Cardiol. 1999;34:1637–1643. doi: 10.1016/s0735-1097(99)00392-7. [DOI] [PubMed] [Google Scholar]
- 18.Landgraf JM, Abetz L, Ware JE. The Child Health Questionnaire (CHQ): A User’s Manual. Boston, Massachusetts: The Health Institute, New England Medical Center; 1996. [Google Scholar]
- 19.Cohen MI, Bridges ND, Gaynor JW, et al. Modifications to the cavopulmonary anastomosis do not eliminate early sinus node dysfunction. J Thorac Cardiovasc Surg. 2000;120:891–900. doi: 10.1067/mtc.2000.109708. [DOI] [PubMed] [Google Scholar]
- 20.Cohen MI, Wernovsky G, Vetter VL, et al. Sinus node function after a systematically staged Fontan procedure. Circulation. 1998;98(19 Suppl):II352–II358. [PubMed] [Google Scholar]