Abstract
Study design:
Systematic literature review and meta-analysis.
Objective:
In symptomatic subjects to: (1) examine the effects of a single session of joint mobilization on pain at rest and with most painful movement, and (2) compare the effects when joint mobilization is provided to a specific or non-specific spinal level.
Background:
Joint mobilization is routinely used for treating spinal pain in conjunction with other interventions, but its unique effect is not well understood. Further, there is controversy about the role of ‘specific level’ techniques in producing benefit.
Methods:
Searches were performed for randomized controlled trials (RCTs) using electronic databases (MEDLINE, CINAHL, and PEDro) from 1966 through November 2010. Methodological quality was assessed using previously detailed criteria. Meta-analysis and meta-regression were conducted on eligible studies.
Results:
Eight RCTs with a mean methodological score of 10/12 were included. Significant heterogeneity (P = 0.075) was found in the overall meta-analysis estimate. When stratified by body location, no significant individual effect was found for pain at rest. However, there was a statistical mean difference [0.71 (95% confidence interval: 0.13–1.28)] between pain at rest for the cervical and lumbar individual means.
Conclusions:
We found multiple studies which provided evidence that a single session of joint mobilization can lead to a reduction of pain at rest and with most painful movement. When using joint mobilization, the need for specific versus non-specific level mobilization may be influenced by anatomical region; the direction of effect in the cervical spine was toward specific mobilization and in the lumbar spine towards non-specific mobilization.
Keywords: Spinal mobilization, Specific level, Pain
Introduction
Passive joint mobilization techniques are frequently used by clinicians to assess for and treat spinal disorders.1,2 During assessment, spinal mobilizations appear useful in identifying the symptomatic spinal level,3,4 and deviations from normal accessory motion may be associated with pain.5–8 When used for treatment, there is good evidence to support the combination of joint mobilization and exercise.9 However, treatment combinations obscure the effect of the individual interventions that make up that treatment. Understanding the relative contribution of elements within a combined treatment approach allows clinicians to adjust a treatment element to address the variations in needs of individual patients. Therefore, examining the effect of spinal mobilization alone could help clinical decision-making and complement the current understanding of joint mobilization in animal and lab-based research.10,11
In a 2008 systematic review by Schmid et al.,12 the authors assessed 15 studies investigating the effects of spinal mobilization alone on pain measures and range of motion. Data were pooled in this review, and the resultant suggestion was that joint mobilization improved outcomes by 20% relative to controls who did not receive mobilizations. Another review found similar modest improvements with spinal mobilization.13 These reviews focused on the immediate effects of treatment applied to the cervical spine. Further, similar effects, decreased pain and increased motion, have been observed when mobilization was performed at the asymptomatic level (non-specific level) or at the symptomatic level (the specific level).14 In addition, a third systematic review that included both randomized and non-randomized controlled trials concluded that a single session of spinal mobilization may have little or no clinically meaningful or lasting effect.15 The study by Vernon et al.14 and that by Hegedus et al.15 only included studies which examined the effects of joint mobilization and not those studies which combined joint mobilization with other interventions.
Consequently, the primary purpose of this systematic review and meta-analysis was to examine the effects of a single session of joint mobilization in symptomatic subjects, performed at any spinal region, on changes in self-reported pain at rest and self-reported pain with the most painful movement. Examining the effect of joint mobilization on pain with most painful movement is not common in meta-analyses but is warranted, as this is a common assessment of effectiveness in clinical practice. The second purpose of this study was to compare the changes in pain that occur when a single session of joint mobilization is provided to a specific or a non-specific level of symptoms within the same spinal region.
Methods
Search strategy
A systematic literature search was performed for relevant articles in MEDLINE (1966 to October 2010), CINAHL (1983 to November 2010), and PEDro for randomized controlled trials (RCTs) on the immediate effects of joint mobilization to the spine in symptomatic subjects. The search was limited using the terms ‘Human’ and ‘English’. Search terms included ‘manual therapy’, ‘joint mobilization’, ‘joint mobilisation’, ‘spinal manual therapy’, ‘manipulation therapy’, ‘low back pain’, ‘thoracic pain’, ‘cervical pain’, ‘randomised controlled trial’, and ‘randomized controlled trial’. MESH terms were used when available. The search strategy used for the MEDLINE database is provided in APPENDIX A. In addition, the reference lists from previously performed systematic reviews of single-session spinal mobilization were reviewed and studies were included, if they met the selection criteria. In addition, all applicable studies irrespective of original search source were cross-referenced to identify articles that met inclusion criteria but had not been located during the electronic database search.
Selection criteria
RCTs investigating the effects of a single session of passive joint mobilization in subjects with current cervical, thoracic, or lumbar pain were deemed potentially relevant. For the purpose of this review, joint mobilization was defined as a non-thrust (e.g. Grade i–iv), oscillatory mobilization procedure directed at the spinal joints. To address our second purpose, the RCT could explore the importance of mobilization at the specific level identified by therapist as contributing to the problem in comparison to mobilization provided at a non-specific level. Also, those studies that reported extremity symptoms deemed to be referred from the spine were included. Studies with subjects of any age were included. Details of the joint mobilization technique used were required so as to discern that passive mobilization was being performed and not joint manipulation, which we defined as high-velocity, low-amplitude thrust manipulation, or other forms of manual therapy, such as muscle energy, massage, myofascial, or trigger point techniques. No limit was placed on the number of bouts of mobilization occurring during a single session. Only immediate, within-session, effect studies were included (a single session of mobilization). The outcomes of interest were changes in self-reported pain at rest and self-reported pain with the most painful movement as a result of the mobilization. Studies were excluded if they involved animals, if high-velocity, low-amplitude thrust manipulation was performed, if only long-term effects of joint mobilization were examined, or if joint mobilization was combined with another intervention where the effects of the joint mobilization alone could not be established.
Study selection and data extraction
Two authors (ES and EH) independently evaluated the potentially relevant studies for inclusion. Disagreements regarding inclusion were resolved by consensus. If consensus could not be reached, a third reviewer (RC) independently reviewed the article and provided input. The vote of the third reviewer resolved any disagreement.
Relevant data from each included article were extracted by one author (RC) and once completed, checked by the primary author (ES) (Table 1). These data included: (1) participant characteristics and clinical condition; (2) characteristics of the treatment intervention (mobilization) and comparison group(s); (3) list of co-interventions and duration of follow-up; and (4) primary outcomes for a self-reported pain at rest and self-reported pain with the most painful movement.
Table 1. Details of patient characteristics, interventions, and outcomes in the included randomized trials.
| Study | Participants | Interventions | Outcomes |
| Aquino et al. (2009)37 | 48 individuals with chronic non-specific neck pain | Group A treatment: central/unilateral PA or transverse mobilization applied to symptomatic vertebral level | Pain (NRS: 0–10): |
| Group B comparison: central/unilateral PA or transverse mobilization applied to randomly selected vertebral level | Pre-post difference: | ||
| Co-interventions: none | RP: A, 0; B, 0.54 | ||
| Duration of therapy: 1 session | MP: A, 2.67; B, 2.62 | ||
| Palpation: A, 2.42; B, 2.37 | |||
| SMD (RP): −0.52 (95% CI: −1.87–0.83) | |||
| SMD (MP): −0.13 (95% CI: −1.63–1.38) | |||
| SMD (palpation): −0.16 (95% CI: −1.31–0.99) | |||
| Chiradejnant et al. (2002)40 | 120 individuals with non-specific low back pain | Group A treatment: central/unilateral PA mobilization applied to symptomatic vertebral level | Pain (NRS: 0–10): |
| Group B comparison: central/unilateral PA mobilization applied to randomly-selected vertebral level | Pre-post difference: | ||
| Co-interventions: none | RP: A, 1.34; B, 0.88 | ||
| Duration of therapy: 1 session | MP: A, 1.51; B, 1.13 | ||
| Chiradejnant et al. (2003)36 | 140 individuals with non-specific low back pain | Group A treatment: therapist-selected PA or transverse mobilization applied to symptomatic level | Pain (NRS: 0–10): |
| Group B comparison: randomly-selected PA or transverse mobilization applied to symptomatic level | Pre-post difference: | ||
| Co-interventions: none | RP: A, 1.3; B, 1.2 | ||
| Duration of therapy: 1 session | MP: A, 1.7; B, 1.4 | ||
| Perceived effect (11-point Likert scale): | |||
| Pre-post difference: A, 1.4; B, 1.2 | |||
| Coppieters et al. (2003)35 | 20 subjects with neurogenic cervicobrachial pain | Group A treatment: cervical lateral glide mobilization applied to 1 or more vertebral levels including symptomatic level | Pain (NRS: 0–10): |
| Group B comparison: therapeutic ultrasound applied to symptomatic region, 5 minutes, 0.5 W/cm2, 1 mHz, 5 cm2 head, 20% sonation time | Pre-post difference: A, 1.5; B, 0.4 | ||
| Co-interventions: none | Symptom distribution area: | ||
| Duration of therapy: 1 session | Pre-post difference: A, 9.7; B, 3.8 | ||
| Kanlayanaphotporn et al. (2009)34 | 60 individuals with neck pain | Group A treatment: unilateral PA mobilization applied to symptomatic side | Pain (VAS: 0–100): |
| Group B comparison: unilateral or central PA mobilization applied to a randomly-selected side | Pre-post difference: | ||
| Co-interventions: none | RP: A, 10.8; B, 12.3 | ||
| Duration of therapy: 1 session | MP: A, 16.7; B, 16.9 | ||
| Kanlayanaphotporn et al. (2010)12 | 60 individuals with neck pain | Group A treatment: central PA mobilization applied to cervical vertebrae | Pain (VAS: 0–100): |
| Group B comparison: randomly-selected central or unilateral PA mobilization applied to cervical vertebrae | Pre-post difference: | ||
| Co-interventions: none | RP: A, 18.3; B, 13.0 | ||
| Duration of therapy: 1 session | MP: A, 21.9; B, 12.7 | ||
| Schomacher (2009)38 | 126 individuals with neck pain | Group A treatment: translatoric traction mobilization applied to symptomatic vertebral level | Pain (NRS: 0–10): |
| Group B comparison: translatoric traction mobilization applied to vertebral level located 3 levels above or below symptomatic vertebral level | Pre-post difference: A, 1.3; B, 1.7 | ||
| Co-interventions: none | |||
| Duration of therapy: 1 session | |||
| Sterling et al. (2010)39 | 39 individuals with whiplash-associated disorder | Group A treatment: cervical lateral glide mobilization applied to cervical vertebrae | Pain (VAS: 0–10): |
| Group B comparison: manual contact with no movement of cervical vertabae | Pre-post difference: | ||
| Co-interventions: none | During NFR stimulation: A, −0.4; B, −0.9 | ||
| Duration of therapy: 1 session | SMD: 0.47 (95% CI: −1.23 to −2.07) |
Note: MP, most painful movement; NFR, nociceptive flexion reflex; NRS, numeric rating scale; PA, posterioranterior; RP, resting pain; SMD, standard mean difference between groups; VAS, visual analogue scale.
Methodological quality
Two reviewers (ES and EH) independently assessed the risk of bias in the included studies using criteria previously reported in the literature.16 The following bias characteristics were examined in each study: randomization; concealment of treatment allocation; blinding of patient, provider, and the outcome assessor; incomplete data; withdrawal/drop-out rate and intention-to-treat analysis; selective outcomes reporting; similarity of groups at baseline; similarity of co-interventions provided; similarity in timing of assessment. Studies were dichotomized into high or low risk of bias based on these characteristics, with those studies possessing six or more of the design features being labeled as ‘low risk’ according to Furlan et al.17
Data analysis
All analyses were performed in Stata 11 (Stata Corp,. College Station, TX, USA) using ‘metan’ and ‘metereg’ commands to analyze the effects of specific level spine mobilization versus non-specific level spine mobilization with two outcomes; self-reported pain at rest and self-reported pain with the most painful movement. The use of standardized weighted mean differences (WMDs) for the purposes of meta-analysis has been questioned due to lack of validity and reliability.18–20 Furthermore, the 0–10 numeric rating scale (NRS) and the 0–100 mm visual analog scale (VAS) have been reported to lack linearity and interchangeability,21,22 a requirement for the use of standardized mean differences.18 Therefore, in order to improve clinical interpretability, studies with differing outcomes measures were analyzed in separate analysis with unstandardized WMDs. The 95% confidence limit difference (CLD), calculated as the upper confidence limit subtracted from the lower confidence limit, was used to determine the precision of mean difference and WMD estimates with smaller values indicating more precise estimates.23 Because the power to detect publication bias may be limited with fewer than 10 studies, publication bias was not formally tested.24 Homogeneity test statistics and their P values were used to assess consistency of estimated WMDs across studies. Homogeneity for combining studies with an overall estimate was set a priori at an alpha level of P>0.15. A higher P value was chosen to test for heterogeneity since these tests have low power particularly when there are few studies analyzed.25 To explore overall heterogeneity and determine if the effects differ by study characteristics, random effects meta-regression (stratified analysis) was used to estimate associations between WMDs. A restricted maximum likelihood method of precision weighted meta-regression models incorporating random effects was used to estimate the among study variance.26 Data from eligible studies were extracted independently by one of the authors (AG) and checked for inconsistencies by the primary author (ES).
Results
Study selection
The initial electronic database searches resulted in the identification of 1237 articles. Figure 1 displays the flow of the articles through the review process. Seventeen articles were selected for detailed review with only eight eligible for inclusion in the final analyses. Reasons for exclusion of nine articles at this time were related to non-randomization of subjects, lack of immediate assessment following joint mobilization, and manual techniques apart from joint mobilization being performed.25–33
Figure 1.
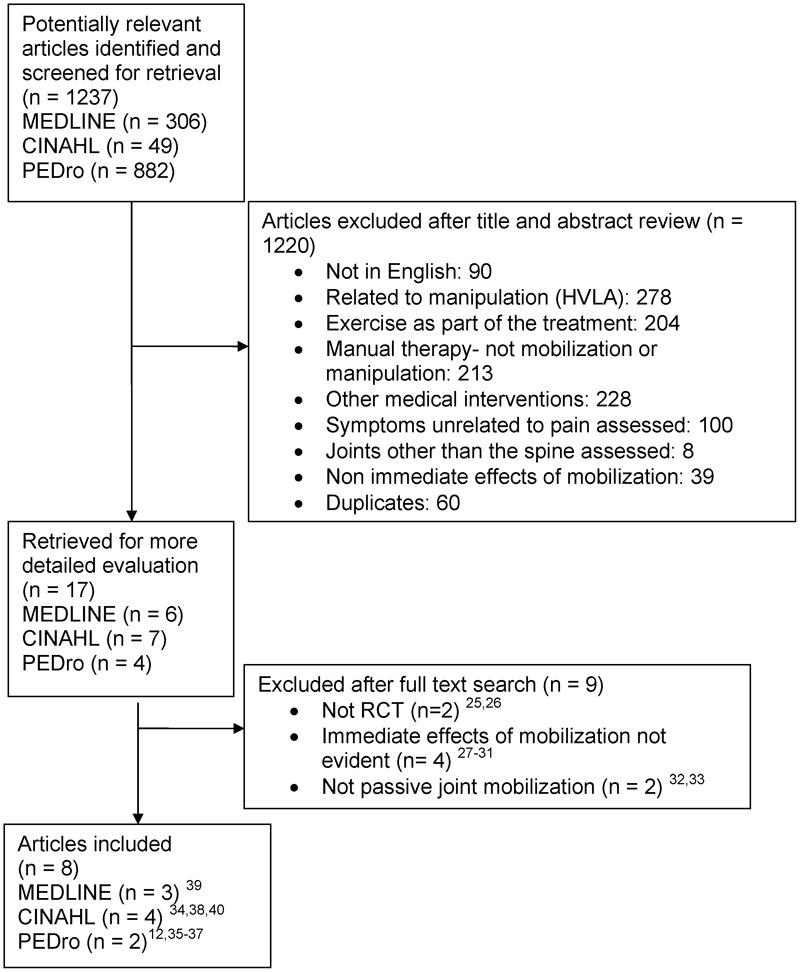
Selection process for studies included in the analysis.
Methodological quality
The eight articles14,36–42 underwent methodological review which indicated a mean score of 10 out of 12 (range 7–12) using the guidelines provided by Furlan et al. (Fig. 2).17
Figure 2.
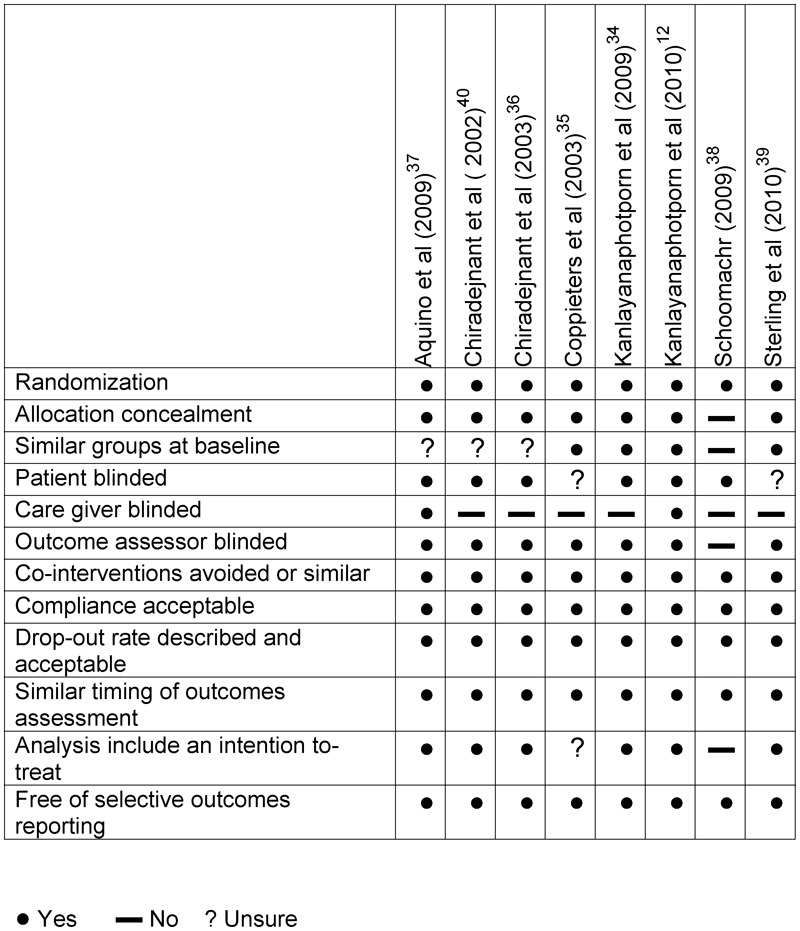
Summary of methodological qualities of studies based on criteria by Furlan et al.15
Meta-analysis
Due to the heterogeneity of the results from the eight studies included in the systematic review, it was not possible to combine these results so that a meta-analysis could be performed. However, it was possible to combine a smaller subset of these studies that pertained to the outcome of joint mobilization at specific and non-specific levels in the same spinal region.
Specific versus non-specific mobilization
Six RCTs compared specific level versus non-specific level mobilization. Of these six studies, four measured the outcome of pain with the NRS and two with the VAS. Therefore, the four studies using the NRS were eligible for meta-analysis and meta-regression techniques. Conversely, the two studies that measured pain with the VAS were analyzed separately.
Pain at rest
For the analysis of pain at rest measured with the NRS scale, the overall heterogeneity was significant (P = 0.075). WMDs varied on both sides of the null between −0.54 and 0.46 (Fig. 3). Due to between study heterogeneity no overall summary estimate could validly describe these studies findings. When conducting stratified analysis using body location (cervical or lumbar) as the stratifying variable this heterogeneity greatly reduced (Table 3). In addition, stratification by body location produced results for the cervical and lumbar spine that were on opposite sides of the null value. The individual pooled mean difference for the cervical spine was −0.41 [95% confidence interval (CI): −0.86–0.03] (Fig. 4). The individual pooled mean difference [0.29 (95% CI: −0.06–0.64)] for the lumbar spine was in the direction opposite to that of the cervical spine (Fig. 5). A large significant (P = 0.02) difference of 0.71 (95% CI: 0.13–1.28) was found between these two means. This indicates that the effect from mobilization in the cervical spine differs from that in the lumbar spine with cervical mobilization favoring specific level mobilization and non-specific level mobilization in the lumbar spine.
Figure 3.
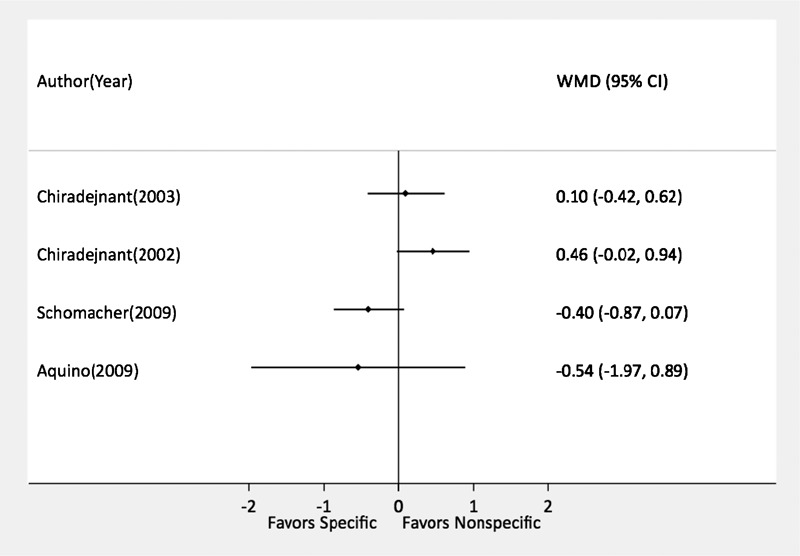
Comparison of the effect of specific versus non-specific mobilization measured with numeric pain rating scale for pain at rest. The Chiradejnant (2003) and (2002) papers reference the lumbar spine, and the Schomacher (2009) and Aquino (2009) papers reference the cervical spine.
Table 3. Stratified analysis and random effects meta-regression analysis of cervical and lumbar studies for pain at rest and most painful movement outcomes measured with numeric pain rating.
| Outcome | Study characteristic | No. studies | Weighted mean difference (95% CI) [95% CLD*] | Homogeneity P value | Difference of weighted estimates (95% CI) P value |
| Pain at rest | |||||
| Cervical | 2 | −0.41 (−0.86–0.03) [0.89] | 0.85 | 0 | |
| Lumbar | 2 | 0.29 (−0.06–0.64) [0.70] | 0.31 | 0.71 (0.13–1.28) 0.02 | |
| Most painful movement | |||||
| Cervical | 2 | −0.27 (−0.77–0.22) [0.99] | 0.76 | 0 | |
| Lumbar | 2 | 0.33 (−0.04–0.72) [0.75] | 0.83 | 0.61 (−0.01–1.24) 0.05 |
Note: CI, confidence interval; CLD, confidence limit difference.
Figure 4.
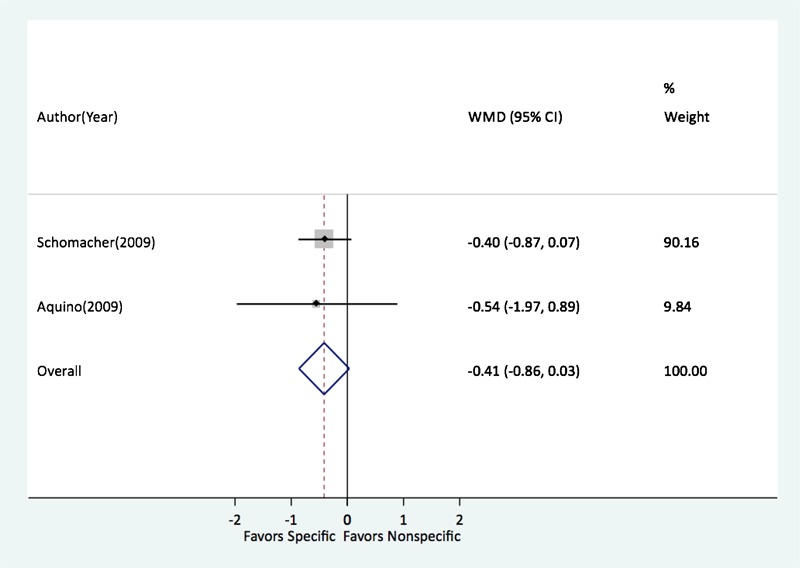
Comparison of the effect of specific versus non-specific mobilization in the cervical spine measured with numeric pain rating scale for pain at rest.
Figure 5.
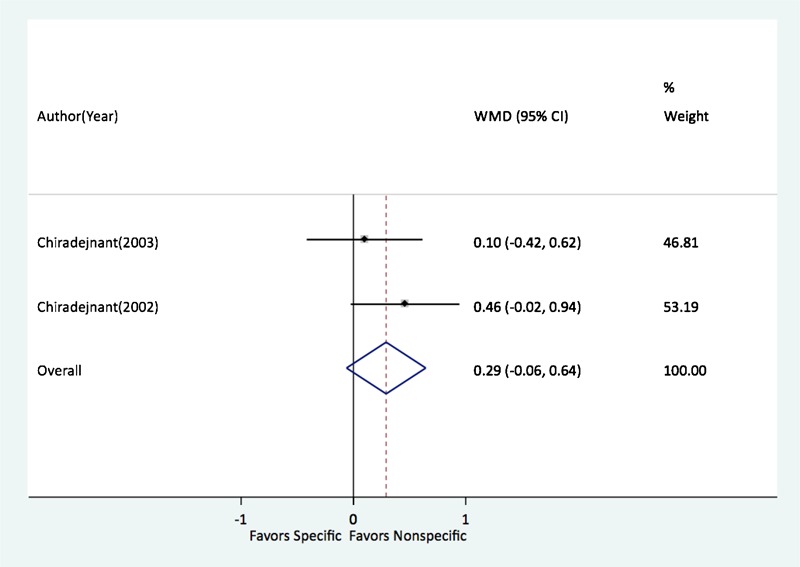
Comparison of the effects of specific versus non-specific mobilization in the lumbar spine measured with numeric pain rating scale for pain at rest.
Two studies measured pain at rest using the VAS with their mean differences being on both sides of the null value (Table 2). These two studies were found to be statistically homogenous (P = 0.189) with an overall mean difference of 0.92 (95% CI: −3.94–5.78).
Table 2. Study characteristics and effect estimates for six studies examining the effect of specific-level versus non-specific mobilization on pain at rest and pain with most painful movement.
| Study | N specific level group | N non-specific level group | Body location | Pain measure | Pain at rest mean difference (95% CI) [95% CLD*] | Most painful movement mean difference (95% CI) [95% CLD] |
| Chiradejnant et al. (2002)40 | 60 | 60 | Lumbar | NRS | 0.46 (−0.02–0.94) [0.97] | 0.38 (−0.16–0.92) [1.08] |
| Chiradejnant et al. (2003)36 | 70 | 70 | Lumbar | NRS | 0.10 (−0.42–0.62) [1.03] | 0.30 (−0.23–0.83) [1.06] |
| Aquino et al. (2009)37 | 24 | 24 | Cervical | NRS | −0.54 (−1.97–0.89) [2.86] | −0.05 (−1.62–1.52) [3.13] |
| Schomacher (2009)38 | 59 | 67 | Cervical | NRS | −0.40 (−0.87–0.07) [0.94] | −0.30 (−0.82–0.22) [1.05] |
| Kanlayanaphotoporn (2009)34 | 30 | 30 | Cervical | VAS | −1.5 (−7.55–4.55) [12.11] | −0.20 (−8.7–8.31) [17.02] |
| Kanlayanaphotoporn (2010)12 | 30 | 30 | Cervical | VAS | 5.3 (−2.85–13.45) [16.30] | 9.2 (0.46–17.94) [17.47] |
Note: CI, confidence interval; CLD, confidence limit difference; NRS, numeric rating scale; VAS, visual analogue scale.
Pain with most painful movement
In the analysis of the four studies measuring the most painful movement with the NRS, the overall homogeneity was P = 0.279. The WMDs varied and were on both sides of the null value. The pooled weighted mean estimate was 0.11 (95% CI: −0.19–0.41) for these four studies, A single study characteristic of location of mobilization (i.e., cervical versus lumbar) once again explained a large amount of the heterogeneity in the cervical spine estimate (P = 0.767) with a pooled mean difference favoring specific level mobilization [−0.27 (95% CI: −0.77–0.22). Similarly, a large amount of heterogeneity (P = 0.836) was explained in the lumbar spine estimate [0.34 (95% CI: −0.04–0.72)], which favored non-specific level mobilization. The difference between the cervical and lumbar estimate was large [0.61 (95% CI: −0.01–1.24)] although not significantly (P = 0.05) different from one another.
For the two studies measuring most painful movement with the VAS, estimates were on both sides of the null. In addition, these estimates demonstrated significant heterogeneity (P = 0.131) and were substantially imprecise (Table 2). As such, no overall estimate was produced and with the small number of studies no stratified analysis was conducted.
Discussion
We found that multiple studies provided evidence that a single session of joint mobilization can lead to a reduction of self-reported pain at rest and self-reported pain with the most painful movement.14,36–41 The studies supporting this statement were methodologically strong when assessed using the criteria set forth by Furlan et al.17 Due to the heterogeneity of the results from these studies, it was not possible to complete a meta-analysis using the eight studies; however, a meta-analysis of a subsection of these studies that examined the significance of mobilizations applied at the specific level of joint dysfunction or a non-specific level did provide noteworthy results.
Spinal joint mobilization is now widely recognized as a technique that reduces pain and increases limited segmental motion.12,27,43 The efficacy of joint mobilization is best quantified when the patient only receives mobilization and not mobilization combined with other interventions such as thermal modalities,44 muscular mobilization,31 or exercise.30 It has also been of benefit when studies have assessed the initial effect of mobilization directly after the mobilization and not several hours or days later.29 With the passage of time, it becomes more difficult to attribute the immediate changes in self-reported pain at rest and self-reported pain with the most painful movement solely to the mobilization provided. Therefore, the studies included in this systematic review were selected based on the inclusion criteria of examining the immediate effect of a single session of joint mobilization. The studies that were included in this systematic review showed low bias, and the results of the studies could be interpreted as being of value to the clinician because the risk of spurious results was minimized.
This systematic review differs from other recent systematic reviews on passive joint mobilization on several aspects. A systematic review by Schmid et al.12 focused on the evidence supporting the involvement of the supraspinal systems in mediating the effects of passive cervical joint mobilization. Of the 15 studies in their review, 10 examined the effects of joint mobilization on an asymptomatic population, and four examined the effect of joint mobilization on lateral epicondylagia. Studies in this current review only included those where symptomatic subjects were examined. The studies by Sterling et al.41 and Coppetiers37 were the only studies common to both systematic reviews.
A systematic review by Vernon and Humphreys13 examined the change scores in pain with a single session of manual therapy in subjects with chronic cervical pain. The authors examined RCTs that used joint manipulation, joint mobilization, and ischemic compression. Four studies on joint mobilization were included in the review along with seven more related to manipulation or ischemic compression. The authors did not feel the studies on joint mobilization could be simply summarized or interpreted, and they reported that the evidence for mobilization was less substantial than for manipulation with fewer studies on joint mobilization reporting smaller immediate changes. This review by Vernon and Humphreys13 is limited to interpretation of the effectiveness of joint mobilization in the management of chronic cervical pain. There is no attempt in either the Schmid et al.12 or Vernon and Humphreys13 papers to statistically combine the outcomes in the form of a meta-analysis.
The assessment of consistency of effects, by testing heterogeneity, is an important part of meta-analysis.45 Inconsistencies, as seen with heterogeneous results, may reduce the confidence on treatment recommendations from meta-analysis.45 This is the first meta-analyses to explain the heterogeneity in pooled estimates of specific level versus non-specific level mobilization in the spine. The heterogeneity in pooled estimates with both outcome of pain at rest and pain with the most painful movement was largely explained by one study characteristic; where in the body (cervical versus lumbar) the intervention was applied. Specific level mobilization versus non-specific level mobilization is dependent on the body location in which it is applied; specific level mobilization favored the cervical spine whereas non-specific level mobilization favored the lumbar spine which has implications for specificity of clinical interventions.
Our individual pooled estimates lacked statistical significance and most demonstrated decreased precision which may be due to the small number of studies, which met eligibility requirements for this meta-analysis.
Various manual therapy techniques exist to address pain in the spine.42 Similar to HVLA, the choice of mobilization technique has traditionally been dependent on biomechanical limitations identified at a specific spinal level or the spinal level associated with a patient’s chief complaint. For example, the presence of a barrier to spinal surfaces approximating in the spine would direct the use of a technique which would bring the surfaces together. This concept of a biomechanical limitation has been recently challenged by the neurophysiological model of symptom modulation.46 What is not well understood is the combined interaction of the biomechanical and neurophysiological models. Our findings question the importance of specificity of technique when treating patients with spinal conditions, especially those with low back pain. It may be the case that cervical mobilization techniques rely on more precise patient set up and execution with respect to the anatomy of the cervical spine, while in the case of the lumbar spine, less specific techniques are performed with less emphasis on the exact level that is being affected. It is possible that outcomes relate to an altered biomechanical limitation in the lumbar spine in relation to the biomechanical limitation in the cervical spine.
Although a difference in response to the biomechanical model could be expected between the cervical and lumbar spines, the neurophysiological response to joint mobilization is expected to be similar in both regions of the spine. While a mechanical stimulus to the body is thought to initiate the neurophysiological mechanisms, it is unclear how specific the mechanical stimulus needs to be. Animal and human studies have both shown neurophysiological manual therapy effects that seem to involve centrally-mediated processes. Sluka et al.10 observed bilateral changes in mechanical withdrawal thresholds in rats following unilateral joint mobilization. These effects are thought to be mediated through supra-spinal mechanisms that influence pain responses at both local and remote regions. Bialosky et al.47 showed similar improvements in pain and disability following an actual and sham neurodynamic technique in patients with carpal tunnel syndrome. Interestingly, while similar clinical improvements were noted, only the group receiving the actual neurodynamic technique showed reductions in temporal summation, a behavioral measure of excitability within the dorsal horn of the spinal cord. These findings may highlight that other factors unrelated to the specificity of the technique may influence the clinical benefits of manual therapy including reductions in clinical pain intensity. Bishop et al.48 investigated the effects of upper thoracic manual therapy on neurophysiological effects using pain sensitivity testing. Bishop et al.48 found a unique effect of upper thoracic thrust manipulation on temporal summation measured at both upper extremity and lower extremity regions compared to control interventions. Interestingly, in similar previous studies by George et al.49 and Bialosky et al.50 lumbar thrust manipulation influenced temporal summation at the lower extremity region only. These findings may provide early evidence of differences in neurophysiological effects based on spinal region of application. This evidence is preliminary, however, and has not been extensively studied for techniques other than thrust manipulation.
There are several limitations with this study. From 1237 articles, only eight were found to be acceptable when methodological rigor was assessed, and of the eight there was not one study completed on the thoracic spine. The thoracic spine is frequently assessed and treated using mobilization techniques. Subsequently, the findings of this review cannot be generalized to the thoracic spine. When studies were combined on the lumbar and cervical spine in the meta-analysis that examined the role of level of mobilization, there were a limited number of studies in each group. Also, there was a lack of clinical homogeneity between the studies included in each group. Only one of the cervical studies identified a sub population of patients to include in their study: patients with over three months of cervical pain.39 The other cervical study,40 and the two lumbar studies38,42 enrolled patients with cervical pain and lumbar pain without defining the duration of symptoms. The duration of a patient’s symptoms can be a factor that alters the response to joint mobilization. Another area of difference between the studies lies in the duration that the mobilization techniques were applied. In the lumbar studies,38,42 subjects received two 1-minute repetitions of mobilization. In comparison to this, subjects in the study by Schomacher,40 received 4 minutes of joint mobilization. Aquino et al.39 did not indicate the duration of joint mobilization. The number of studies included in the meta-analysis limited our ability to statistically assess publication bias; therefore, publication bias cannot be ruled out. Moreover, with only four studies included in the meta-analysis and two studies for each cervical and lumbar stratified analysis, caution should be exercised with extrapolating from these estimates. Furthermore, four of our studies, two cervical and two lumbar were conducted by the same authors, which may also bias these meta-analysis estimates. This literature would benefit from comparative studies addressing the topic of specific level versus non-specific level mobilization in the cervical and lumbar spine from different authors to see if these associations continue to exist. An additional way to strengthen the argument for the role of specific level versus non-specific level mobilization would be to look at objective measures of changes in central sensitivity. Examples of these measures would be pain pressure threshold and nociceptive flexion reflex responses; this current study just examines self-reported pain at rest and self-reported pain with the most painful movement.
The quality of research being completed on a single session of joint mobilization on the spine is promising. A recent systematic review by Hegedus et al.15 on the duration of effectiveness of joint mobilization discovered that there is very little research in this area. For joint mobilization to continue to be a valued tool in the management of spinal dysfunction more must be known about the carry over effect of a session of mobilization. Another key component in the use of joint mobilization is the necessity for accuracy of technique application depending on the location of the spine being treated. The findings of this meta-analysis raises questions about the notion that joint mobilization always needs to be applied at the exact pathological level when treating the lumbar spine.
Conclusion
This systematic review supports the argument that joint mobilization to the spine does lead to an immediate effect on pain at rest and pain with the most painful movement. A meta-analysis of a subset of these studies did identify that the effect of mobilization relating to a specific level or non-specific level was different based on the region of the spine being treated; the direction of effect in the cervical spine was toward specific mobilization and in the lumbar spine towards non-specific mobilization, indicating body location modified the relationship between specific versus non-specific mobilization with pain at rest.
References
- 1.Allison G, Edmonston S, Kiviniemi K, Lanigan H, Simonsen AV, Walcher S. Influence of standardized mobilization on the posteroanterior stiffness of the lumbar spine in asymptomatic subjects. Physiother Res Int. 2001;6:145–56 [DOI] [PubMed] [Google Scholar]
- 2.Powers CM, Kulig K, Harrison J, Bergman G. Segmental mobility of the lumbar spine during a posterior to anterior mobilization: assessment using dynamic MRI. Clin Biomech. 2003;18:80–3 [DOI] [PubMed] [Google Scholar]
- 3.Abbott JH, McCane B, Herbison P, Moginie G, Chapple C, Hogarty T. Lumbar segmental instability: a criterion-related validity study of manual therapy assessment. BMC Musculoskelet Disord. 2005;6:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Humphreys BK, Delahaye M, Peterson CK. An investigation into the validity of cervical spine motion palpation using subjects with congenital block vertebrae as a ‘gold standard’. BMC Musculoskelet Disord. 2004;5:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kulig K, Powers CM, Landel RF, Chen H, Fredericson M, Guillet M, et al. Segmental lumbar mobility in individuals with low back pain: in vivo assessment during manual and self-imposed motion using dynamic MRI. BMC Musculoskelet Disord. 2007;8:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abbott JH, Fritz JM, McCane B, Shultz B, Herbison P, Lyons B, et al. Lumbar segmental mobility disorders: comparison of two methods of defining abnormal displacement kinematics in a cohort of patients with non-specific mechanical low back pain. BMC Musculoskelet Disord. 2006;7:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jull G, Treleavan J, Versace G. Manual examination of spinal joints: is pain provocation a major diagnostic cue for dysfunction? Aust J Physiother. 1994;40:159–63 [DOI] [PubMed] [Google Scholar]
- 8.Jull G, Zito G, Trott P, Potter H, Shirley D. Inter-examiner reliability to detect painful upper cervical joint dysfunction. Aust J Physiother. 1997;43:125–9 [DOI] [PubMed] [Google Scholar]
- 9.Gross AR, Goldsmith C, Hoving JL, Haines T, Peloso P, Aker P, et al. Conservative management of mechanical neck disorders: a systematic review. J Rheumatol. 2007;34:1083–102 [PubMed] [Google Scholar]
- 10.Sluka K, Skyba K, Radhakrishnan R, Lepper B, Wright A. Joint mobilization reduces hyperalgesia associated with chronic muscle and joint inflammation in rats. J Pain. 2006;7:602–7 [DOI] [PubMed] [Google Scholar]
- 11.Moss P, Sluka K, Wright A. The initial effects of knee joint mobilization on osteoarthric hyperalgesia. Man Ther. 2007;12:109–18 [DOI] [PubMed] [Google Scholar]
- 12.Schmid A, Brunner F, Wright A, Bachmann LM. Paradigm shift in manual therapy? Evidence for a central nervous system component in the response to passive cervical joint mobilisation. Man Ther. 2008;13:387–96 [DOI] [PubMed] [Google Scholar]
- 13.Vernon H, Humphreys BK. Chronic mechanical neck pain in adults treated by manual therapy: a systematic review of change scores in randomized controlled trials of a single session. J Man Manip Ther. 2008;16:E42–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanlayanaphotporn R, Chiradejnant A, Vachalathiti R. Immediate effects of the central posteroanterior mobilization technique on pain and range of motion in patients with mechanical neck pain. Disabil Rehabil. 2010;32:622–8 [DOI] [PubMed] [Google Scholar]
- 15.Hegedus E, Slaven E, Goode A, Butler R. The neurophysiological effects of a single session of spinal joint mobilization: does the effect last? J Man Manip Ther. 2011;19:143–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gross A, Miller J, D’Sylva J, Burnie SJ, Goldsmith CH, Graham N, et al. Manipulation or mobilisation for neck pain: a Cochrane Review. Man Ther. 2010;15:315–33 [DOI] [PubMed] [Google Scholar]
- 17.Furlan AD, Pennick V, Bombardier C, van Tulder M. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine. 2009;34:1929–41 [DOI] [PubMed] [Google Scholar]
- 18.Cummings P. Meta-analysis based on standardized effects is unreliable. Arch Pediatr Adolesc Med. 2004;158:595–7 [DOI] [PubMed] [Google Scholar]
- 19.Greenland S, Schlesselman JJ, Criqui MH. The fallacy of employing standardized regression coefficients and correlations as measures of effect. Am J Epidemiol. 1986;123:203–8 [DOI] [PubMed] [Google Scholar]
- 20.Greenland S, Maclure M, Schlesselman JJ, Poole C, Morgenstern H. Standardized regression coefficients: a further critique and review of some alternatives. Epidemiology. 1991;2:387–92 [PubMed] [Google Scholar]
- 21.Holdgate A, Asha S, Craig J, Thompson J. Comparison of a verbal numeric rating scale with the visual analogue scale for the measurement of acute pain. Emerg Med. 2003;15:441–6 [DOI] [PubMed] [Google Scholar]
- 22.Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003;3:310–6 [DOI] [PubMed] [Google Scholar]
- 23.Poole C. Low P-values or narrow confidence intervals: which are more durable? Epidemiology. 2001;12:291–4 [DOI] [PubMed] [Google Scholar]
- 24.Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53:1119–29 [DOI] [PubMed] [Google Scholar]
- 25.Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions The Cochrane Collaboration 2011; No. Version 5.1.0 [updated March 2011] [Google Scholar]
- 26.Thompson SG, Sharp SJ. Explaining heterogeneity in meta-analysis: a comparison of methods. Stat Med. 1999;18:2693–708 [DOI] [PubMed] [Google Scholar]
- 27.Hanrahan S, van Lunen BL, Tamburello M, Walker ML. The Short-term effects of joint mobilizations on acute mechanical low back dysfunction in collegiate athletes. J Athl Train. 2005;40:88–93 [PMC free article] [PubMed] [Google Scholar]
- 28.Goodsell M, Lee M, Latimer J. Short-term effects of lumbar posteroanterior mobilization in individuals with low-back pain. J Manipulative Physiol Ther. 2000;23:332–42 [PubMed] [Google Scholar]
- 29.Leaver AM, Maher CG, Herbert RD, Latimer J, McAuley JH, Jull G, et al. A randomized controlled trial comparing manipulation with mobilization for recent onset neck pain. Arch Phys Med Rehabil. 2010;91:1313–8 [DOI] [PubMed] [Google Scholar]
- 30.Bautmans I, van Arken J, van Mackelenberg M, Mets T. Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. J Rehabil Med. 2010;42:129–35 [DOI] [PubMed] [Google Scholar]
- 31.Hoving JL, Koes BW, de Vet HC, et al. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Ann Intern Med. 2002;136:713–22 [DOI] [PubMed] [Google Scholar]
- 32.Korthals-de Bos IB, Hoving JL, van Tulder MW, van der Windt DA, Assendelft WJ, van Mameren H, et al. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trial. BMJ. 2003;326:911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Costa LO, Maher CG, Latimer J. Re:Goldby LJ, Moore AP, Doust J, et al. A randomized control trial investigating the efficiency of musculoskeletal physiotherapy on chronic back pain disorder. Spine. 2006;31:1083–93 [DOI] [PubMed] [Google Scholar]
- 34.Martinez-Segura R, Fernandez-de-las-Penas C, Ruiz-Saez M, Lopez-Jimenez C, Rodriguez-Blanco C. Immediate effects on neck pain and active range of motion after a single cervical high-velocity low-amplitude manipulation in subjects presenting with mechanical neck pain: a randomized controlled trial. J Manipulative Physiol Ther. 2006;29:511–7 [DOI] [PubMed] [Google Scholar]
- 35.Groeneweg R, Kropman H, Leopold H, van Assen L, Mulder J, van Tulder MW, et al. The effectiveness and cost-evaluation of manual therapy and physical therapy in patients with sub-acute and chronic non specific neck pain. Rationale and design of a Randomized Controlled Trial (RCT). BMC Musculoskelet Disord. 2010;11:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kanlayanaphotporn R, Chiradejnant A, Vachalathiti R. The immediate effects of mobilization technique on pain and range of motion in patients presenting with unilateral neck pain: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90:187–92 [DOI] [PubMed] [Google Scholar]
- 37.Coppieters MW, Stappaerts KH, Wouters LL, Janssens K. The immediate effects of a cervical lateral glide treatment technique in patients with neurogenic cervicobrachial pain. J Orthop Sports Phys Ther. 2003;33:369–78 [DOI] [PubMed] [Google Scholar]
- 38.Chiradejnant A, Maher CG, Latimer J, Stepkovitch N. Efficacy of ‘therapist-selected’ versus ‘randomly selected’ mobilisation techniques for the treatment of low back pain: a randomised controlled trial. Aust J Physiother. 2003;49:233–41 [DOI] [PubMed] [Google Scholar]
- 39.Aquino RL, Caires PM, Furtado FC, Loureiro AV, Ferreira PH, Ferreira ML. Applying joint mobilization at different cervical vertebral levels does not influence immediate pain reduction in patients with chronic neck pain: a randomized clinical trial. J Man Manip Ther. 2009;17:95–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schomacher J. The effect of an analgesic mobilization technique when applied at symptomatic or asymptomatic levels of the cervical spine in subjects with neck pain: a randomized controlled trial. J Man Manip Ther. 2009;17:101–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sterling M, Pedler A, Chan C, Puglisi M, Vuvan V, Vicenzino B. Cervical lateral glide increases nociceptive flexion reflex threshold but not pressure or thermal pain thresholds in chronic whiplash associated disorders: a pilot randomised controlled trial. Man Ther. 2010;15:149–53 [DOI] [PubMed] [Google Scholar]
- 42.Chiradejnant A, Latimer J, Maher C, Stepkovitch N. Does the choice of spinal level treated during posteroanterior (PA) mobilisation affect treatment outcome? Physiother Theory Pract. 2002;18:165–74 [Google Scholar]
- 43.Powers CM, Beneck GJ, Kulig K, Landel RF, Fredericson M. Effects of a single session of posterior-to-anterior spinal mobilization and press-up exercise on pain response and lumbar spine extension in people with nonspecific low back pain. Phys Ther. 2008;88:485–93 [DOI] [PubMed] [Google Scholar]
- 44.Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Yu F, Adams AH. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: clinical outcomes from the UCLA neck-pain study. Am J Public Health. 2002;92:1634–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14:531–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bialosky JE, Bishop MD, Price DD, Robinson ME, Vincent KR, George SZ. A randomized sham-controlled trial of a neurodynamic technique in the treatment of carpal tunnel syndrome. J Orthop Sports Phys Ther. 2009;39:709–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bishop M, Beneciuk J, George S. Immediate reduction in temporal sensory summation after thoracic spinal manipulation. Spine J. 2011;11:440–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.George S, Bishop M, Bialosky J, Zeppieri G, Robinson M. Immediate effects of spinal manipulation on thermal pain sensitivity: an experimental study. BMC. 2006;7:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bialosky J, Bishop M, Robinson M, Zeppieri G, George S. Spinal manipulative therapy has an immediate effect on thermal pain sensitivity in people with low back pain: a randomized controlled trial. Phys Ther. 2006;89:1292–303 [DOI] [PMC free article] [PubMed] [Google Scholar]


