Abstract
Objectives:
Upper cervical movement impairment and muscle dysfunction have been identified as core components of cervicogenic headache (CGH) pathogenesis. The purpose of this single-group pre–post test pilot study was to investigate the short-term effects of a specific soft tissue massage (SSTM) intervention to the cervical spine on range of upper cervical motion.
Methods:
Eight subjects (mean age 28.1 years) with published criteria of CGH (mean history of headache for 7.1 years) were investigated. Range of rotation of the upper cervical spine to the left and right was determined by the flexion–rotation test. Movement was assessed in three phases: pre-intervention, intervention, and post-intervention. The SSTM intervention consisted of an 8-minute soft tissue massage to the cervical muscles bilaterally.
Results:
Pre-intervention measures of flexion–rotation test range of motion prior to the intervention over two assessment points were consistent. In contrast, a repeated measures analysis of variance revealed a significant improvement in range of rotation to the left and right after the first (P<0.01), second (P<0.01), but not third intervention (P = 0.19), from an average range of 27.5° at baseline to 45.9° at the third treatment session. After the 2-week post-intervention phase, range of motion remained stable without decline, and was considered full range.
Discussion:
This pilot study provides preliminary evidence of the potential for SSTM to improve, at least in the short-term, upper cervical range of motion in people with CGH.
Keywords: Cervicogenic headache, Flexion–rotation test, Massage, Cervical movement impairment
Introduction
Cervicogenic headache (CGH) is a relatively common disorder with an estimated prevalence of 20% among the chronic headache population, and a 4∶1 female disposition.1 The diagnosis of CGH is based on the evaluation of subjective features and physical examination findings.2,3 In terms of the physical examination, there is evidence of impairment of cervical range of motion (CROM) and muscle extensibility,4,5 as well as impairment of upper cervical segmental motion in people with CGH.6 Specific movement impairment includes the flexion–rotation test (FRT), which has recently been identified as a valid and reliable measure of upper cervical motion.7–10 This test has been found to be useful in the diagnosis of CGH,9 and has potential as an outcome measure.11,12
Physical interventions commonly applied in the management of CGH include manipulative therapy and massage. While there is growing evidence to support the use of manipulative therapy,13,14 evidence is lacking for the use of massage.15 Despite this lack of evidence, massage therapy is commonly sought and utilized by people who suffer from all forms of headache. For example, approximately 50% of one sample of 432 patients attending tertiary outpatient clinics in Germany were reported to have tried massage therapy to alleviate their symptoms.16 The explanation for why patients sought complimentary therapy was to explore all avenues of treatment, not just drug intervention. Another explanation for why massage therapy is frequently used by clinicians is because of the high prevalence of cervical muscle tightness4 and trigger points17,18 in people who suffer from different headache forms.
Neurophysiological effects of massage have been demonstrated in preliminarily animal studies, where massage induces acute antinociceptive effects involving opioid and oxytocin interaction.19 Another mechanism supporting the use of massage therapy in patients with headache may be related to alteration in the sensitization state of the trigeminocervical nucleus.20 Since massage may influence the trigeminocervical nucleus, massage also has the potential to change neck muscle tone through alteration of the trigeminoreticular pathway.21 However, there is a lack of evidence demonstrating the efficacy of massage therapy in the management of CGH, particularly with respect to its effects on upper cervical movement impairment and muscle length. Major limitations in the studies published to date include a lack of stringent quality trials and the use of multimodal adjuncts along with the massage technique.22
No study to date has addressed specific massage techniques targeting cervical muscle tightness related to CGH. Therefore, the purpose of our study was to investigate the short-term effect of specific soft tissue massage on upper CROM evaluated by the FRT.
Methods
Study design
A within-subject repeated measures pilot study design was used, with subjects acting as their own controls using baseline data collected on two assessment points prior to the first treatment session. Time was the independent variable. CROM was the dependent variable and was measured via the FRT at baseline, before and after each of three treatment sessions and 2 weeks following the final treatment.
Subjects
Twenty-four volunteers, recruited as a sample of convenience from university students and staff, were screened for potential inclusion in the study. Recruitment was achieved by on campus advertising seeking people suffering from headache and neck pain. Inclusion criteria were CGH at least twice per week, together with headache defined according to the criteria proposed by Sjaastad3 and further evaluated by Antonaci,23 with the exception of diagnostic anaesthetic blocks. These criteria were intermittent, side dominant headache of moderate intensity, without side shift. The headache was required to be preceded by ipsilateral neck pain and precipitated or aggravated by neck movement or posture. Subjects were excluded if they also met the International Headache Society criteria for migraine or tension-type headache,2 or had adverse response to vertebro-basilar insufficiency tests, previous neck trauma, rheumatoid arthritis or neurological signs. In addition, subjects were excluded if they were unable to tolerate the FRT (none were excluded in this way). Consequently, nine subjects met the eligibility criteria. One subject withdrew during the pre-intervention phase due to family commitments leaving eight female subjects aged between 18 and 53 years. Demographic details are shown in Table 1.
Table 1. Subject demographic details (n = 8).
| Variable | Mean (standard deviation) |
| Age (years) | 28.1 (11.6) |
| Gender | 8 female |
| Headache duration (years) | 7.1 (5.8) |
| Headache frequency (per day) | 0.69 (0.19) |
| Headache intensity (0–10) | 3.57 (1.7) |
| Bilateral headache | 6 |
| Unilateral headache | 2 |
Curtin University Human Research Ethics Committee approved this study and all subjects provided written informed consent.
Measurements
FRT
As this was a group post-graduate student project spread over the course of one academic year, three physiotherapists (authors YB, CC, and OJ), trained in using the FRT, were used to assess the FRT over the course of the study period. Previously we have established high levels of intra-rater reliability for range of motion measured by trained examiners during the FRT. Intra-class correlation coefficients were reported as 0.95 (95% confidence interval: 0.90–0.98).8 Furthermore, range of motion recorded during the test and examiner interpretation of the test have been shown to be consistent over time with kappa of 0.92 and a minimal detectable change of at most 7°.8
The FRT was carried out according to previously reported guidelines.8 With the subject relaxed in supine, the cervical spine was pre-positioned in maximal end-range flexion and the head passively rotated to the left and the right.8 End-range rotation was determined either by firm resistance encountered by the therapist or the subject reporting the onset of pain, whichever came first. The purpose was to measure range of motion irrespective of the cause of limitation, in the least provocative manner, to minimize the potential for symptom exacerbation. The examiner determined mobility by using a modified CROM device as shown in Fig. 1. The CROM device is a floating compass (Plastimo Airguide Inc. (Compasses), Buffalo Groove, IL, USA) attached to the apex of the head by Velcro straps.24,25 Preliminary investigation of inter-rater reliability for these examiners was found to be excellent (intra-class correlation coefficient⩾0.89).
Figure 1.
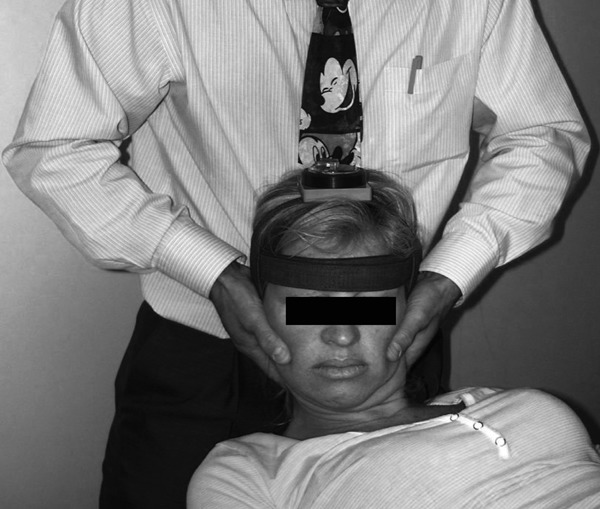
Flexion–rotation test measurement position and modified cervical range of motion measurement device.
Procedures
Two baseline (TC) measurements of the FRT to the left and the right were recorded 14 days apart prior to the first intervention session. This was followed by a 1-week intervention period where three separate treatment sessions (T1, T2, and T3) were conducted with the FRT assessed before (Tpre) and after each session (Tpost). A final assessment of the FRT (Tfinal) was carried out 2 weeks after T3.
The physiotherapist (DH) who applied the intervention is an experienced massage therapist, and was blind to the subjects’ dominant symptomatic side, the degree of restriction demonstrated at baseline, and the changes in range that resulted from each intervention.
The sequence of the data collection process is outlined in Fig. 2.
Figure 2.
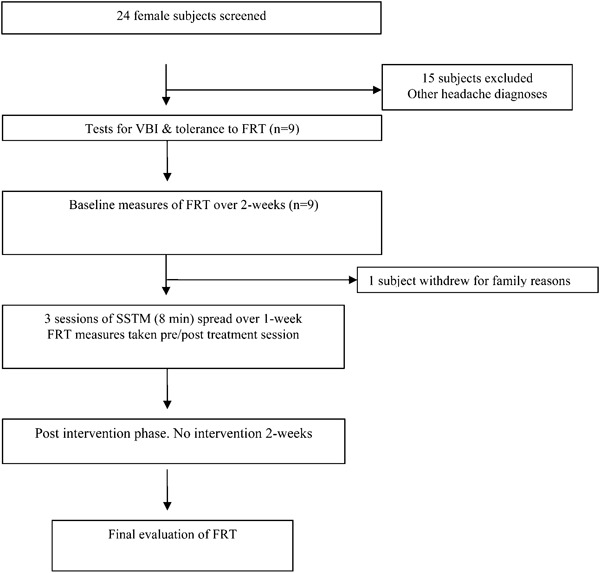
Flow chart of subjects through the study. VBI: vertebrobasilar artery insufficiency; FRT: flexion–rotation test; SSTM: specific soft tissue massage.
For the intervention, the subject was positioned in supine and towels were wrapped around the body to ensure even temperature. The external occipital protuberance and superior nuchal line of the occiput rested on a pillow so that the neck and shoulders were exposed. Each subject received an 8-minute standard SSTM using Sorbolene massage cream (Livingstone International Pty Ltd, Rosebery, Australia). Circular kneading was first performed using the distal pad of the third digit, repeated three times on the target tissue. Specific segmental kneading was performed bilaterally on the cervical articular pillars from the C7 vertebra to the occiput. Each kneading stroke was repeated three times over each vertebral level. Following this, the head was turned to the contralateral side to expose the unilateral levator scapular muscle and circular kneading was continued focussing on the distal attachment on the superior border and superior angle of the scapular to the proximal attachments of the transverse processes of C1 and C2, and posterior tubercles of C3 and C4. This process was repeated on the opposite side. Following this, the same circular kneading technique was used bilaterally, commencing from the mastoid process along the superior nuchal line targeting the sternocleidomastoid and upper trapezius muscles. This sequence was repeated three times. The same technique was applied more inferolaterally to longissmus capitis, splenius capitus and moving medially and deeper to semispinalis capitis muscles. Following this, massage was commenced on the suboccipital muscles, distal to the inferior nuchal line, from lateral to medial. The hand positions for these techniques are illustrated in Figs. 3–5.
Figure 3.

Circular kneading technique, applied bilaterally using the pads of the index and middle fingers, directed to the sternocleidomastoid, upper trapezius, longissimus capitis, splenius capitus, and semispinalis capitis muscles.
Figure 5.

Circular kneading, using the pads of the index and middle fingers, directed to the right articular pillar from the occiput to the C7 vertebral levels.
Figure 4.

Circular kneading, using the pads of the index and middle fingers, directed to the levator scapula muscle, with the head and neck in left rotation.
Data analysis
All analyses were conducted using SPSS version 14.0 (SPSS Inc., Chicago, IL, USA), and statistical significance was accepted at the 0.05% level of confidence. Normality of distribution was confirmed prior to data analysis.
Changes over time (eight assessment points: TC, T1pre, T1post, T2pre, T2post, T3pre, T3post, and Tfinal) in the range recorded during the FRT were analysed with a repeated measures analysis of variance. Where changes were significant over time, paired t-tests were used for pair-wise comparisons. Separate models were constructed for range of movement to the left and right sides.
Power analysis and sample size
To estimate an appropriate sample size for this study, data from a previous study were used, in which a mean range of 27.6° rotation recorded during the FRT was found in people suffering from CGH.24 A change in range of motion greater than the minimal detectable change of 7° over the length of the study was considered clinically significant. Hence, with a level of significance set at 0.05, the sample size was calculated at 8.
Results
Table 2 shows range of rotation recorded during the FRT at each of eight test occasions. Initially, prior to the first intervention for each side at baseline TC, the mean range recorded during the FRT was similar at the two assessment points 2 weeks apart, thus demonstrating a consistent pattern of movement impairment. Immediately after each intervention, there were variable increases in mean range of motion recorded during the FRT: gaining 10.9 and 11.5° for right and left rotation following T1; 6.4 and 5.9° for right and left rotation following T2; and 5.1 and 3.8° for right and left rotation following T3. Following a non-intervention period of 2 weeks, the final ranges (Tfinal) recorded for the FRT were 43.9 and 40.6° to the left and right, respectively.
Table 2. Mean (standard deviation) range recorded during the flexion–rotation test (FRT) over time (n = 8).
| FRT | Baseline | Treatment 1 | Treatment 2 | Treatment 3 | Final | |||
| Pre | Post | Pre | Post | Pre | Post | |||
| Right | 26 (10.6) | 28 (8.8) | 38.9 (3.8) | 35.1 (6.7) | 41.5 (6.2) | 40.8 (3.8) | 45.9 (5.5) | 40.6 (8) |
| Left | 27.1 (11.5) | 28.8 (13.1) | 40.3 (6.2) | 36.5 (10.7) | 42.4 (10.1) | 42 (4.8) | 45.8 (7.1) | 43.9 (5.6) |
Figure 6 provides a visual illustration of some of the changes in range recorded during the FRT at different phases of the study, specifically for mean range recorded during the FRT to the left.
Figure 6.
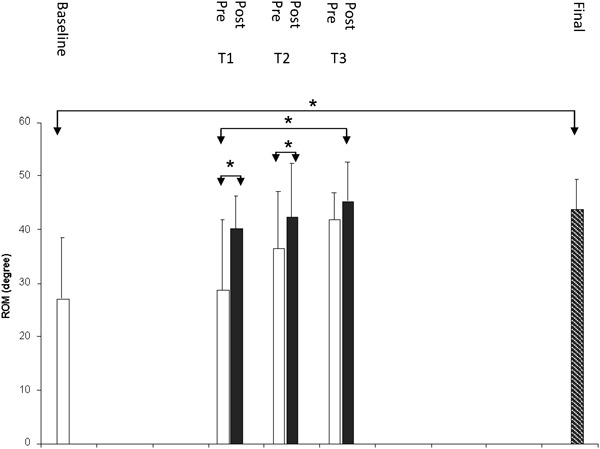
Range recorded during the flexion–rotation test (to the left) before, during, and after the interventions (*significant increase P<0.01). n = 8. ROM = range of motion; T1 = treatment 1; T2 = treatment 2; T3 = treatment 3.
Prior to the first treatment session, there was no significant difference between range recorded at TC and T1pre for either left or right rotation (P = 0.52). In contrast, there was a significant increase in range following the first treatment session between T1pre and T1post (P<0.01); there was a similarly significant increase in range during the FRT between T2pre and T2post (P<0.01). There was no significant change in range following the third treatment session (P = 0.19), nor following the final treatment session and the final follow-up (P = 0.12). In contrast, there were significant differences between ranges recorded at TC and T3post (P = 0.01); T1pre and T3post (P<0.01); T1pre and T1post (P<0.01); and T2pre and T2post (P<0.01).
Discussion
In our pilot study, all subjects presented with restriction of range recorded during the FRT when compared with reported normal values,24,26 which is consistent with previous reports for subjects with CGH. Baseline measurements for range recorded during the FRT to the right (26°) and left (27.1°) were comparable to those reported by Ogince et al.25 and Hall and Robinson,24 who found that CGH subjects demonstrated a mean range of 27.6 and 20.4° to the right and left, respectively. Furthermore, at the initial two evaluation points prior to any intervention, there was less than a 2° difference in mean range recorded during the FRT, indicating a degree of consistency and stability of measurements. While two measurements 2 weeks apart are not conclusive evidence of stability, a previous report has demonstrated stability of FRT range of motion measures recorded over a 2-week period in people with chronic symptoms of CGH.8
Following the first two massage sessions, there was a significant increase in range of motion, with an overall significant increase in range from baseline to the final assessment point. Mean range achieved following the final massage session was 45.9° to the right side and 45.8° to the left side. These ranges are consistent with those reported for asymptomatic people.24,25,27 The greatest increase in range was achieved after the first treatment session. However, there was an apparent cumulative effect of the SSTM on range of motion. Interestingly, and in line with general clinical practice experience, range gained at each assessment point was not completely maintained until the following session. However, range after the 2-week non-intervention period was significantly better than at baseline and greater than the minimal detectable change reported for the FRT.8 These results indicate that SSTM may have potential value (in the short-term) for improving upper CROM in people with CGH.
Range of upper cervical movement, as determined by the FRT, is related to the severity of headache symptoms (headache frequency, intensity, and duration).12 Hence the gain in range found in this study may possibly equate to a reduction in headache symptoms. It was not the intention of this study to investigate the effect of massage therapy on pain and disability, as a larger sample size would have been required for that. Further studies are required to investigate whether or not improvement in range of motion delivers improvement in headache symptoms.
This pilot study provides preliminary evidence that SSTM techniques influence upper CROM in people suffering from CGH. During the SSTM intervention, specific tissues were targeted including upper cervical muscles that attached to the superior and inferior nuchal lines on the occiput and to upper cervical segments between the occiput and C2 vertebra. These massage techniques included the classic techniques of effleurage and specific circular kneading over the specific cervical muscle structures. Evidence has shown a higher prevalence of tightness in the cervico-brachial muscles in CGH subjects.4,28 The present study findings suggest that SSTM may influence muscle tightness related to CGH by increasing range of upper CROM.
Soft tissue massage to cervical muscles has frequently been used in the management of headaches29 in order to cause relaxation of muscles. Indeed in the clinical setting, it has shown that almost 40% of physiotherapists use soft tissue techniques such as massage to manage clinical cases.29 However, previous reports have not specified the particular muscle treated, the type of soft tissue techniques used, and the duration of the treatment for CGH. In contrast, the present study found that three 8-minute treatment sessions targeting upper cervical musculature increased and maintained upper CROM over a 2-week post-treatment interval.
Another reported method of improving impairment identified by the FRT to manage CGH symptoms includes a Mulligan sustained natural apophyseal glide.30 One study found an immediate improvement in range during the FRT after a single application of this sustained natural apophyseal glide technique.11 Repeated application of this gave sustained headache relief. However, not all people who suffer from CGH may be suitable for this technique, for example due to potential impact on the vertebral artery due to the rotational stress. So SSTM may be a viable alternative, or addition to the treatment plan for managing patients presenting with CGH.
Limitations
It is important to recognize that there are a number of limitations to this pilot study. Firstly, the sample size was small, with only eight subjects; hence the potential for error is much greater than that in a larger sample. We recommend that subsequent studies should investigate a larger sample to verify these results. Secondly, the mean age of subjects was 28.1 years, which is much younger than previous reports for subjects with CGH.31 However, it is uncertain whether this age difference has any implications. Thirdly, due to the lack of control group in our study, a randomized, placebo controlled trial is required to verify that the increase in range recorded during the FRT was due to the effect of the SSTM. Further studies are also required to investigate the influence of change in upper CROM and its effect on symptoms.
Conclusion
In this pilot study, three 8-minute treatment sessions of upper cervical SSTM over a 1-week period significantly improved range recorded during the FRT to the left and the right after each massage session. Furthermore, range of motion was maintained for 2 weeks after the end of the intervention period. These results suggest that SSTM may have benefits in the management of patients with CGH, but further research is required to confirm this.
References
- 1.Haldeman S, Dagenais S. Cervicogenic headaches: a critical review. Spine J. 2001; 1: 31–46 [DOI] [PubMed] [Google Scholar]
- 2.Classification Committee of the International Headache Society The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004; 24 Suppl 1: 9–160 [DOI] [PubMed] [Google Scholar]
- 3.Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. The Cervicogenic Headache International Study Group. Headache. 1998; 38: 442–5 [DOI] [PubMed] [Google Scholar]
- 4.Zito G, Jull G, Story I. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Man Ther. 2006; 11: 118–29 [DOI] [PubMed] [Google Scholar]
- 5.Zwart JA. Neck mobility in different headache disorders. Headache. 1997; 37: 6–11 [DOI] [PubMed] [Google Scholar]
- 6.Hall T, Briffa K, Hopper D, Robinson K. Reliability of manual examination and frequency of symptomatic cervical motion segment dysfunction in cervicogenic headache. Man Ther. 2010; 15: 542–6 [DOI] [PubMed] [Google Scholar]
- 7.Hall T, Briffa K, Hopper D. The influence of lower cervical joint pain on range of motion and interpretation of the flexion–rotation test. J Man Manip Ther. 2010; 18: 126–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall T, Briffa K, Hopper D, Robinson K. Long-term stability and minimal detectable change of the cervical flexion-rotation test. J Orthop Sports Phys Ther. 2010; 40: 225–9 [DOI] [PubMed] [Google Scholar]
- 9.Hall TM, Briffa K, Hopper D, Robinson K. Comparative analysis and diagnostic accuracy of the cervical flexion-rotation test. J Headache Pain. 2010; 11: 391–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takasaki H, Hall T, Oshiro S, Kaneko S, Ikemoto Y, Jull G. Normal kinematics of the upper cervical spine during the Flexion-Rotation Test - In vivo measurements using magnetic resonance imaging. Man Ther. 2011; 16: 167–171 [DOI] [PubMed] [Google Scholar]
- 11.Hall T, Chan HT, Christensen L, Odenthal B, Wells C, Robinson K. Efficacy of a C1-C2 self-sustained natural apophyseal glide (SNAG) in the management of cervicogenic headache. J Orthop Sports Phys Ther. 2007; 37: 100–7 [DOI] [PubMed] [Google Scholar]
- 12.Hall TM, Briffa K, Hopper D, Robinson KW. The Relationship between Cervicogenic Headache and Impairment Determined by the Flexion-Rotation Test. J Manipulative Physiol Ther. 2010; 33: 666–71 [DOI] [PubMed] [Google Scholar]
- 13.Bronfort G, Haas M, Evans R, Leiniger B, Triano J. Effectiveness of manual therapies: the UK evidence report. Chiropr Osteopat. 2010; 18: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gross A, Miller J, D'Sylva J, Burnie SJ, Goldsmith CH, Graham N, Haines T, Bronfort G, Hoving JL. Manipulation or mobilisation for neck pain: a Cochrane Review. Man Ther. 2010; 15: 315–33 [DOI] [PubMed] [Google Scholar]
- 15.Biondi DM. Physical treatments for headache: a structured review. Headache. 2005; 45: 738–46 [DOI] [PubMed] [Google Scholar]
- 16.Gaul C, Eismann R, Schmidt T, May A, Leinisch E, Wieser T, Evers S, Henkel K, Franz G, Zierz S. Use of complementary and alternative medicine in patients suffering from primary headache disorders. Cephalalgia. 2009; 29: 1069–78 [DOI] [PubMed] [Google Scholar]
- 17.Calandre EP, Hidalgo J, Garcia-Leiva JM, Rico-Villademoros F. Trigger point evaluation in migraine patients: an indication of peripheral sensitization linked to migraine predisposition? European Journal of Neurology. 2006; 13: 244–9 [DOI] [PubMed] [Google Scholar]
- 18.Calandre EP, Hidalgo J, Garcia-Leiva JM, Rico-Villademoros F, Delgado-Rodriguez A. Myofascial trigger points in cluster headache patients: a case series. Head Face Med. 2008; 4: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lund I, Ge Y, Yu LC, Uvnas-Moberg K, Wang J, Yu C, Kurosawa M, Agren G, Rosen A, Lekman M, Lundeberg T. Repeated massage-like stimulation induces long-term effects on nociception: contribution of oxytocinergic mechanisms. Eur J Neurosci. 2002; 16: 330–8 [DOI] [PubMed] [Google Scholar]
- 20.Piovesan EJ, Di Stani F, Kowacs PA, Mulinari RA, Radunz VH, Utiumi M, Muranka EB, Giublin ML, Werneck LC. Massaging over the greater occipital nerve reduces the intensity of migraine attacks: evidence for inhibitory trigemino-cervical convergence mechanisms. Arquivos de neuro-psiquiatria. 2007; 65: 599–604 [DOI] [PubMed] [Google Scholar]
- 21.Panneton WM, Gan Q, Livergood RS. A trigeminoreticular pathway: implications in pain. PloS one. 2011; 6: e24499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Van Tulder M, Santaguida L, Gagnier J, Ammendolia C, Dryden T, Doucette S, Skidmore B, Daniel R, Ostermann T, Tsouros S. A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain. Evid Based Complement Alternat Med. 2012; 953139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Antonaci F, Ghirmai S, Bono G, Sandrini G, Nappi G. Cervicogenic headache: evaluation of the original diagnostic criteria. Cephalalgia. 2001; 21: 573–83 [DOI] [PubMed] [Google Scholar]
- 24.Hall T, Robinson K. The flexion-rotation test and active cervical mobility–a comparative measurement study in cervicogenic headache. Man Ther. 2004; 9: 197–202 [DOI] [PubMed] [Google Scholar]
- 25.Ogince M, Hall T, Robinson K, Blackmore AM. The diagnostic validity of the cervical flexion-rotation test in C1/2-related cervicogenic headache. Man Ther. 2007; 12: 256–62 [DOI] [PubMed] [Google Scholar]
- 26.Smith K, Hall T, Robinson K. The influence of age, gender, lifestyle factors and sub-clinical neck pain on cervical range of motion. Man Ther. 2007; 13: 552–559 [DOI] [PubMed] [Google Scholar]
- 27.Hall TM, Robinson KW, Fujinawa O, Akasaka K, Pyne EA. Intertester reliability and diagnostic validity of the cervical flexion-rotation test. J Manipulative Physiol Ther. 2008; 31: 293–300 [DOI] [PubMed] [Google Scholar]
- 28.Jull G, Barrett C, Magee R, Ho P. Further clinical clarification of the muscle dysfunction in cervical headache. Cephalalgia. 1999; 19: 179–85 [DOI] [PubMed] [Google Scholar]
- 29.Grant T, Niere K. Techniques used by manipulative physiotherapists in the management of headaches. The Australian Journal of Physiotherapy. 2000; 46: 215–222 [DOI] [PubMed] [Google Scholar]
- 30.Mulligan B. Manual therapy — ‘AGS’, ‘NAGS’, MWMS’ etc. 6th ed. Wellington: Plane View Services; 2010 [Google Scholar]
- 31.Sjaastad O, Bakketeig LS. Prevalence of cervicogenic headache: vaga study of headache epidemiology. Acta Neurol Scand. 2007;117:173–80 [DOI] [PubMed] [Google Scholar]


