Abstract
Knee pain is common amongst the sporting and general population. Numerous examination procedures are used to apply diagnostic labels to knee symptoms, such as McMurray’s test, which is used to diagnose a meniscal injury. However, previously in the literature the validity compared with a ‘gold standard’ and the reliability between examiners of such tests has been questioned. In this case study, we report on a sports woman, diagnosed by her general practitioner with a meniscal injury and demonstrating a positive McMurry’s test, who was examined using repeated movements as in the McKenzie system of mechanical diagnosis and therapy. Following self-application of extension exercises and extension exercises with over-pressure the McMurry’s test became negative, and she returned to full sporting activities. The case study indicates a further caution about the use of single orthopaedic test procedures. Not only is their validity and reliability questionable, but also following treatment using repeated movements if positive tests can be made negative, this provides an additional query to their validity.
Keywords: Knee, McMurry’s test, Mechanical diagnosis and therapy, Validity
Introduction
Knee pain is common amongst the general population and the population who participate in sporting activities, and a common cause of knee pain are meniscal problems, with a reported incidence of 8.27 per 1000 person-years amongst an active-duty military population.1 Knee pain may originate from various structures located in or close to the knee joint, such as the lateral meniscus or lateral collateral ligament,2 but also be pain referred from proximal structures such as the hip joint3 or the lumbar spine. A range of pathoanatomical diagnoses are routinely applied to these symptoms, such as meniscal, cruciate, or collateral ligament tears, patellofemoral pain syndrome or osteoarthritis.4
A large range of diagnostic physical examination procedures for the knee exist, which purport to allow the application of these diagnostic labels. For instance, it is suggested that McMurray’s or Apley’s test can be used to detect meniscal lesions. However, recent systematic reviews have identified poor levels of sensitivity and specificity when these tests were compared to a reference standard of findings at surgery or arthroscopy.5–8 The conclusions from one review was that the McMurray’s test is very specific, but has a very low sensitivity, whereas joint line tenderness has fairly good sensitivity, but poor specificity.8 Another review looked only at the McMurray’s test, and concluded from 11 studies that it had relatively high specificity, but low sensitivity; and that furthermore the modified tests had enhanced diagnostic accuracy.5 One review included 18 studies and conducted a meta-analysis, with pooled sensitivity and specificity being 70 and 71% for McMurray’s and 63 and 77% for joint line tenderness.7 The final review considered three tests in a meta-analysis and reported diagnostic odds ratios; with joint line tenderness being the best test, followed by McMurray’s and Apley’s test (diagnostic odds ratios 11, 4, 2 respectively).6 Furthermore, the reliability of meniscal tests has not been demonstrated in the literature.5,9 This might not be considered a problem for patients with significant pain and functional problems that are undergoing surgery for clear pathoanatomical lesions. However, issues about the validity and reliability of special tests at the knee must be considered in the work-up between failed conservative therapy and the transition to possible surgical management.
One common knee diagnosis, especially in the sporting population, is the meniscal lesion, often diagnosed by a combination of a comprehensive history and the results of physical examination procedures.7–9 McMurray’s meniscal test is commonly used to detect tears in the posterior segment of the meniscus, this was first described by McMurray in 1942.10 In the literature, there have been various interpretations of the McMurray’s test, with the original description reporting a painful snap or click that is familiar to the patient as being considered a positive test.10 The original description suggested that according to the rotation of the leg different segments of the meniscus were being tested with internal rotation testing the posterior section of the lateral meniscus and external rotation testing the medial cartilage.10 These suppositions have not been verified. There have been modifications of the original test with the addition of varus/valgus or weight-bearing components, which have reported better levels of diagnostic accuracy in the literature.5 Others report pain produced on testing, in the presence or absence of a click, as a positive test.11 Differing interpretations of this test may be a reason for the variability in accuracy reported in various studies.11
Utilizing the McMurray’s test as part of an assessment process is aimed at establishing a pathoanatomical diagnosis, which might be treated conservatively, but may need referral for surgical consideration. An alternative method of diagnosis is a ‘classification system’, such as the McKenzie method of mechanical diagnosis and therapy (MDT).12 This method involves a structured mechanical evaluation of repeated or sustained movements to assess for symptomatic and mechanical responses to classify patients into one of three mechanical syndromes – Derangement, Dysfunction, Postural, or into an ‘other’ grouping. Each syndrome requires a different management approach and is individualized to the patient.12–14
The conceptual model for the ‘derangement syndrome’ is that it occurs due to internal dislocation of articular tissue that causes a disturbance in the normal resting position of the affected joint surfaces.12 The clinical definition of derangement syndrome however is dependent on the symptomatic and mechanical responses to repeated movements.12 This examination style has been shown to be reliable amongst trained therapists with a kappa value of 0.83 when 97 therapists rated 25 patient vignettes.15 The classification system has also been effective at classifying patients with extremity problems; with 388 patients being classified by 30 therapists and 64% classified in one of the MDT syndromes. The largest group were those with derangement; 37% of the total, and 43% derangement in 103 patients with knee problems.16
This case study documents an individual referred with a ‘lateral meniscal tear – positive McMurray’s test’ that, following a McKenzie evaluation, was classified as a ‘derangement’ of the knee and successfully treated accordingly. The case study illustrates the use of directional preference decision-making in patients with extremity problems, but also challenges the link between a positive orthopaedic test, such as McMurray’s meniscal test, and a pathoanatomical diagnosis. The patient consented for the case study to be written up and submitted to a medical journal with anonymous patient details.
Patient History
Ms G. was an 18-year-old female elite nationally ranked swimmer, due to start a USA College Scholarship shortly. Pre-injury, she trained every day of the week for about two hours in the pool, one day twice a day, and with additional dry land sessions focusing on core stability on another two days. She attended university, where she sat for long periods without difficulty, and also worked in a shop three days a week where she stood for long hours. Five weeks previously the lateral knee pain had started during a heavy kick swimming session, but she could not recall any specific event. The following day she visited her general practitioner (GP) who diagnosed ‘lateral meniscus tear with a positive McMurray’s test’, prescribed ibuprofen three times daily for two weeks, and referred her for physiotherapy. After the two weeks as she did not feel that the non-steroidal anti-inflammatory drugs were helping she did not re-new the prescription. She received eight sessions of physiotherapy involving ultrasound, hamstring stretches and quadriceps strengthening with no effect so the physiotherapist referred her back to the GP.
The GP still found a positive McMurray’s test and referred her on to an orthopaedic surgeon. Her coach suggested she attend our clinic for a second opinion.
At initial assessment she reported her symptoms to be intermittent and produced with walking downstairs or hills, squatting, lunging forward on her right knee, kicking at swimming, prolonged standing at work and ‘as the day progressed’. She reported no clicking and no swelling. Symptoms were eased by rest, massage and by avoiding aggravating factors. She reported no previous history of knee pain, and had had no imaging. She had stopped kicking at swimming training, and had reduced her work in the shop to two days as both these activities worsened her symptoms (Figure 1).
Figure 1.
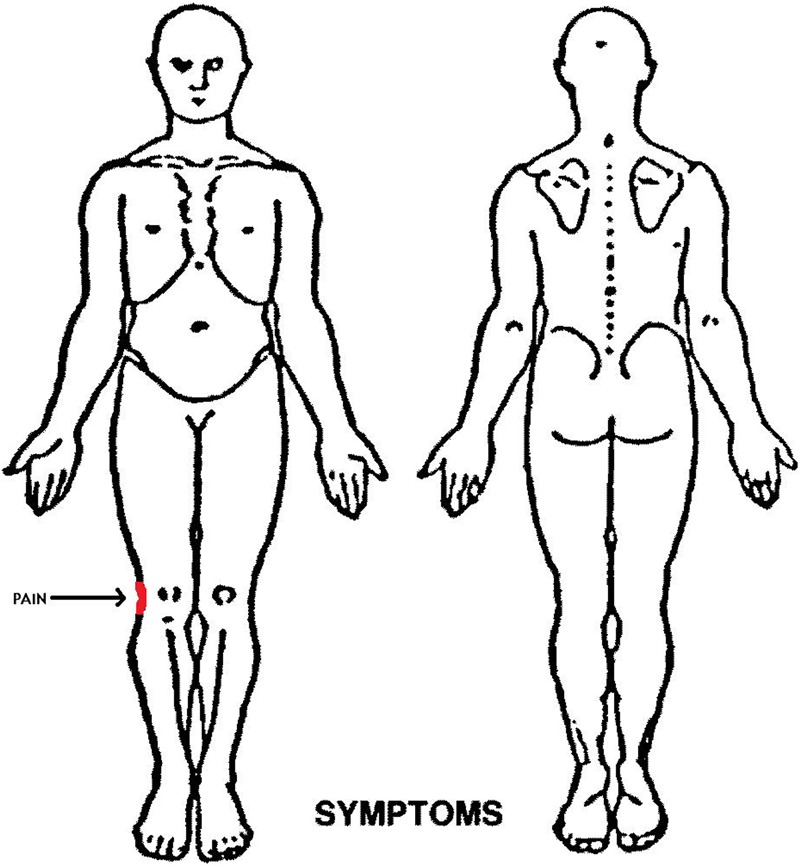
Body Chart.
Outcome Measures
On a numeric pain scale, she rated her pain as 6/10 on average but reported this could increase to 8/10 with descending stairs, freestyle kicking or squatting. She scored 14/40 on the Lower Limb Task Questionnaire (40/40 – means no perceived functional disability) and 3.3/10 on the Patient Specific Functional Scale (10/10 = means full function). The Lower Limb Task Questionnaire has been shown to have a Cronbach score of 0.91, and moderate construct validity with other outcome measures (r 0.51–0.86), and intra-class correlation of 0.95.17 The Patient-Specific Functional Scale has been evaluated with patients with knee problems and shown test–retest reliability of 0.84, and sensitivity to change was also high (Pearson’s 0.78).18
Physical Examination
Observation of the patient revealed normal appearance with no obvious swelling of the knee. She reported no pain in standing or at rest. Functional tests were performed to gain a baseline understanding of her symptomatic and mechanical presentation. Right lateral knee pain was produced with active squat and single knee bend at three quarter range. Active knee extension produced pain and there was restriction of about 10 degrees extension compared to her left side. Passive knee extension in supine produced pain at end range and revealed a similar loss of range of movement of about 10 degrees as estimated by visual observation. Passive knee flexion also produced pain and revealed a 20 degree loss of movement again estimated by visual observation. On performance of McMurray’s lateral meniscal test, she reported marked lateral knee pain and apprehension, no ‘click’ was palpated or heard. Resisted tests of both knee flexion and extension also produced pain, but of a lesser degree. No further special tests were conducted at this point as the response to repeated movements needed to be evaluated first. In the MDT examination baseline tests, such as those conducted above, are followed by repeated movements.
Repeated movement tests, which are a key component of the MDT physical examination, were utilized to assess for symptomatic and mechanical responses. Therapist applied passive repeated knee flexion was initially assessed as this was the most restricted movement. Ten repetitions of passive knee flexion produced lateral knee pain and resulted in a decrease in her squat range of movement. Active knee extension in sitting produced lateral knee pain but was no worse following and did not alter the range of active or passive movement. Passive knee extension in supine was then assessed which resulted in an initial increase in her pain but following the application of 3×10 repetitions she reported a decreasing level of pain at the end of range. On standing, she reported a return to no symptoms, but there was an increase in range of movement with the squat test. McMurray’s test was still ‘positive’.
Provisional Classification
A provisional classification, which was based on the findings of the examination, was made of derangement, with a potential directional preference for extension. The patient was instructed to perform passive knee extension exercises, 10×4–5 times daily by applying an extension movement to the knee with her hands above the patellar while in a seated position with her foot on the floor (Figure 2). She was advised to avoid sitting with her knee flexed at University and she was allowed to continue swimming.
Figure 2.
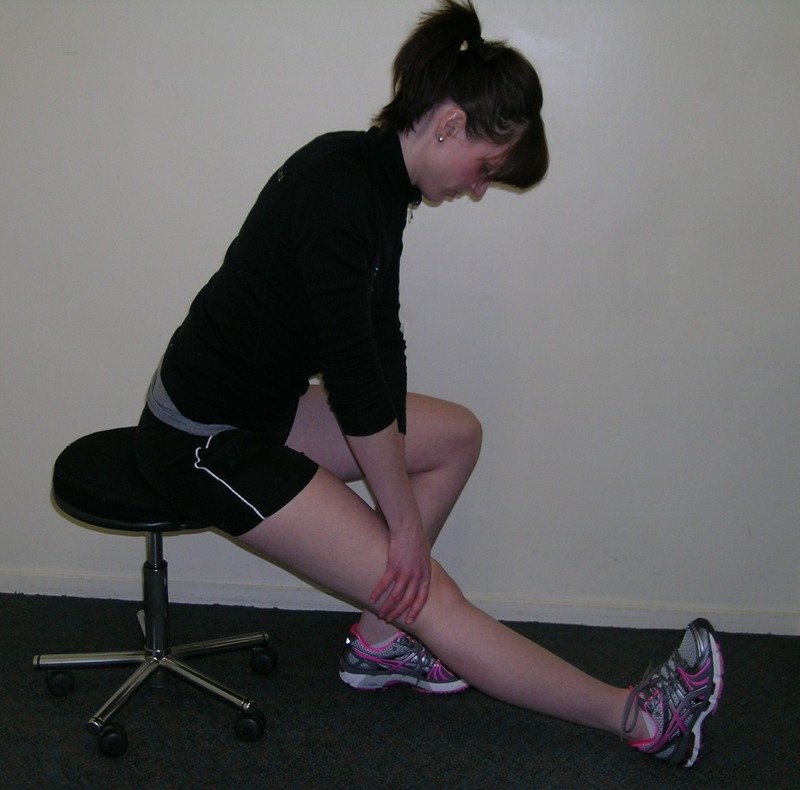
Knee Extention in sitting.
Session 2
Four days later she reported she had been compliant with her exercises and had noted a 30% improvement both in pain and function. She reported decreased pain with walking downstairs but had not attempted to kick at swimming yet. Examination revealed improved knee extension and flexion, less pain with McMurray’s test and less pain with squatting. She was advised to continue with the same exercise at the same frequency and intensity.
Session 3
Three days later she reported her symptoms were at the same level as day four; however, she had managed to swim 4 lengths of freestyle with no aggravation. Examination revealed end-range pain with knee extension, and end-range loss of knee flexion but still reproduction of pain with McMurray’s test. She had pain at the same range when testing her squat similar to day four. She was advised to progress her exercise to performing passive knee extension exercises in standing, resting her back against the wall, with her foot on the floor (Figure 3). The intent of this exercise was to increase the weight-bearing property of the exercise and therefore utilized as a progression of force.12
Figure 3.

Knee Extention in standing.
Session 4
Ms G. returned six days later and reported a 75% improvement. She was able to freestyle swim 1 km with minimal pain. On assessment, she had end-range pain with both knee extension and flexion, but full ROM and a negative McMurray’s test. She was able to squat fully with a ‘feeling’ of tightness to the lateral aspect of her knee at end range. She was advised to continue her exercise and gradually increase her swimming. She was also advised to perform her home exercise pre- and post-swimming sessions.
Session 5
A week later Ms G. now reported >95% improvement in her knee pain and function. She reported 1/10 pain with swimming but she was now participating in full squad sessions. She scored 34/40 on the Lower Limb Task Questionnaire and 9.3/10 on the Patient Specific Functional Scale. Assessment revealed a full pain-free range of knee flexion and extension, full pain free squat and single knee bend. McMurray’s test was negative. She was advised to continue with her current exercise regime until complete resolution and was discharged from the clinic with the prophylactic advice of continuing her passive knee extension exercises pre- and post-swimming sessions for the following 6 weeks or if she developed any lateral knee symptoms.
Ms G. was followed up 14 months after attending physiotherapy. She was still attending college in the USA, undertaking a full academic programme, and swimming training five to six times weekly, as well as two dry-land sessions. She had maintained her scholarship at the college in the USA.
Discussion
This case report documents a patient who received a clinical diagnosis of meniscus lesion as she had a positive McMurray’s test. However, in response to repeated movements she restored function and range of movement at her knee, and returned to full sporting activity, and no longer had a positive McMurray’s test. The case demonstrates the benefit of a thorough mechanical evaluation and interpretation of the history and physical examination of the problem, and most importantly not relying on the responses of individual orthopaedic special tests in isolation.
The McMurray’s test in this case study was initially ‘positive’, however, other factors negated the diagnosis of a meniscus injury. Although the patient did have pain localized to the lateral joint margin, in conjunction with an apparent ‘obstruction’ to movement and pain on testing the McMurray’s test, the history and examination indicated that the menisci may not be the origin of the complaint. On performing a structured MDT assessment, it became apparent that there was a directional preference for extension. With repeating this particular movement over a period of 3 weeks, the pain and obstruction to movement improved and the McMurray’s test became negative. We cannot determine which anatomical structure may have been involved in the initial symptoms and mechanical disruption; however, intra-articular inclusions have the potential to become displaced within the knee joint and cause ‘derangement’ type pathologies, such as observed in this case report.19 However, the purpose of a MDT examination is not to make a specific structural diagnosis, but to see if repeated movements in a specific direction can alter baseline findings, as occurred in this case. The speed with which baseline findings changed, in terms of symptom response and range of movement, meant this patient should be classified as derangement, and the positive directional preference exercises pursued as the direction of management.
The use of MDT in patients with extremity problems was first described in 2000,12 and there has not been a documented study describing the application of directional preference forces at the knee previously. In fact until recently publications relating to use of MDT in the extremities was limited to case studies,13,20,21 but there has also been a reliability study,15 and a survey.16 In the survey 44 patients with knee problems were classified as derangement out of a total of 103 (43%, 95% confidence interval 33–52%) patients with knee problems, and of these 44, 40 (91%) had a directional preference of extension, as in this case study.
Diagnosis according to a non-specific mechanical syndrome classification system guides the clinician in the clinical decision-making process and administering the appropriate management strategy for that individual.12 The management strategy given to this patient was not determined by a structural or pathoanatomical diagnosis but based on a classification system. The diagnosis of ‘derangement’ determined the management strategy for this patient. The McMurray’s test was a good baseline measurement, utilized as part of subsequent reassessments, but it was not useful as a diagnostic tool. Management was determined by the response to repeated active and passive movements at the knee, which demonstrated clear symptomatic and mechanical responses. These allowed classification of the problem as derangement, and also offered a clear directional preference for management of the problem. The ‘positive’ McMurray’s test appeared to be irrelevant and clinically only useful as a ‘mechanical baseline’ measurement.
It has been suggested that the usefulness of following a pathoanatomical classification system for shoulder problems has not been proven, and instead a non-specific classification system based on clinical characteristics, responses to treatment, and prognosis should be used.22 Further research needs to explore the application of such non-specific classification systems to other extremity problems, such as at the knee.
Conclusion
This case study details the examination of a patient referred to physiotherapy with the diagnosis of lateral meniscal tear, based on the reproduction of pain during McMurray’s meniscal test. Following a structured assessment according to principles of MDT, the patient was diagnosed with a ‘derangement’. Self-management strategies were prescribed that reduced pain and improved mobility and function. The case study demonstrates the benefits of the MDT assessment in the extremities, and the problems with placing too much reliance on individual orthopaedic special tests.
References
- 1.Jones JC, Burks R, Owens BD, Sturdivant RX, Svoboda SJ, Cameron KL. Incidence and risk factors associated with meniscal injuries among active-duty US military service members. J Athletic Training. 2012;47:67–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khaund R, Flynn SH. Iliotibial band syndrome: a common source of knee pain. Am Fam Physician. 2005;71:1545–50 [PubMed] [Google Scholar]
- 3.Lesher JM, Dreyfuss P, Hager N, Kaplan M, Furman M. Hip joint pain referral patterns: a descriptive study. Pain Med. 2008;9:22–5 [DOI] [PubMed] [Google Scholar]
- 4.Van Middelkoop M, van Linschoten R, Berger MY, Koes BW, Bierma-Zeinstra SMA. Knee complaints seen in general practice: active sport participants versus non-sport participants. BMC Musculoskeletal Dis. 2008;9:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hing W, White S, Reid D, Marshall R. Validity of the McMurray’s test and modified versions of the test: a systematic literature review. J Man Manip Ther. 2009;17:22–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meserve BB, Cleland JA, Boucher TR. A meta-analysis examining clinical test utilities for assessing meniscal injury. Clin Rehab. 2008;22:143–61 [DOI] [PubMed] [Google Scholar]
- 7.Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. J Orth Sports Phys Ther. 2007;37:541–50 [DOI] [PubMed] [Google Scholar]
- 8.Malanga GA, Andrus S, Nadler SF, McLean J. Physical examination of the knee: a review of the original test description and scientific validity of common orthopaedic tests. Arch Phys Med Rehabil. 2003;84:592–603 [DOI] [PubMed] [Google Scholar]
- 9.Mohan BR, Gosal HS. Reliability of clinical diagnosis in meniscal tears. Int Orthop. 2007;31:57–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McMurray TP. The semilunar cartilages. Br J Surg. 1942;29:407–14 [Google Scholar]
- 11.Akseki D, Ozcan O, Boya H, Pinar H. A new weight-bearing meniscal test and a comparison with McMurray’s test and joint line tenderness. J Arthroscopic Rel Surg. 2004;20:951–8 [DOI] [PubMed] [Google Scholar]
- 12.McKenzie R, May S. The human extremities mechanical diagnosis & therapy. Waikanae: Spinal Publications; 2000 [Google Scholar]
- 13.Aina A, May S. Case report – A shoulder derangement. Man Ther. 2005;10:159–63 [DOI] [PubMed] [Google Scholar]
- 14.Clare H, Adams R, Maher C. Reliability of the McKenzie spinal pain classification using patient assessment forms. Physiotherapy. 2005;90:114–9 [Google Scholar]
- 15.May S, Ross J. The McKenzie classification system in the extremities: a reliability study using McKenzie assessment forms and experienced clinicians. J Manip Physiol Ther. 2009;32:556–63 [DOI] [PubMed] [Google Scholar]
- 16.May SJ, Rosedale R. A survey of the McKenzie classification system in the extremities: prevalence of mechanical syndromes and preferred loading strategies. Phys Ther. 2012;92:1175–86 [DOI] [PubMed] [Google Scholar]
- 17.McNair PJ, Prapavessis H, Collier J, Bassett S, Bryant A, Larner P. The Lower-Limb Tasks Questionnaire: an assessment of validity, reliability, responsiveness, and minimal important differences. Arch Phys Med Rehabil. 2007;88:993–1001 [DOI] [PubMed] [Google Scholar]
- 18.Chatman AB, Hymans SP, Neel JM, Binkley JM, Stratford PW, Scomberg A, et al. The Patient-Specific Functional Scale: Measurement properties in patients with knee dysfunction. Phys Ther. 1997;77:820–9 [DOI] [PubMed] [Google Scholar]
- 19.Mercer S. Derangements in the peripheral joints: anatomical possibilities in the knee and shoulder. 11th Conference on Mechanical Diagnosis and Therapy, Rio de Janeiro, Brazil, 2009 [Google Scholar]
- 20.Littlewood C, May S, A contractile dysfunction of the shoulder. Manual Therapy. 2007;12:80–83 [DOI] [PubMed] [Google Scholar]
- 21.Kaneko S, Takasaki H, May S, Application of mechanical diagnosis and therapy to a patient diagnosed with de Quervain's disease: a case study. J Hand Ther. 2009;22:278–284 [DOI] [PubMed] [Google Scholar]
- 22.Schellingerhout JM, Verhagen AP, Thomas S, Koes B. Lack of uniformity in diagnostic labelling of shoulder pain: Time for a different approach. Man Ther. 2008;13:478–83 [DOI] [PubMed] [Google Scholar]


