Abstract
Objective. To develop and implement a 1-credit-hour oncology pharmacy practice elective course for third-year pharmacy students and assess its impact on examination scores in a required pharmacotherapeutics course.
Design. Major topics were identified to focus on therapeutic management and supportive care of the oncology patient. Psychosocial topics were incorporated to help pharmacy students better relate to oncology patients.
Assessment. Learning was assessed by means of 2 computer-based examinations, weekly reflection posts, and a completed oncology service-learning project and reflection paper. Students enrolled in the course achieved higher pharmacotherapeutics oncology section examination scores than students who had not taken the course. Also, this course increased students’ interest in oncology pharmacy.
Conclusion. The oncology pharmacy elective course has received overwhelmingly positive feedback from students and student enrollment continues to grow. We will continue to offer this course to future practitioners.
Keywords: oncology, cancer, pharmacy, elective course, curriculum, pharmacotherapy
INTRODUCTION
Cancer impacts millions of Americans and their families. In 2010, there were an estimated 13.8 million Americans living with a cancer diagnosis.1 The American Cancer Society estimated that 1,638,910 people would be diagnosed with and 577,190 people would die of cancer in the United States in 2012.2 Further, cancer diagnoses are expected to increase, with an estimated 2.8 million people being diagnosed in the year 2050. This number accounts for the aging and growing population but does not address other increasing risk factors, such as obesity.3 The American Society of Clinical Oncologists released a statement in March 2007 predicting a significant oncologist shortage by as soon as 2020 because of increasing patient age and the increasing number of both new cancer diagnoses and cancer survivors.4
Pharmacists are trained healthcare practitioners who can assist with the increasing demands of oncology patients, but more are needed. Of an estimated 272,320 licensed pharmacists in the United States, there are currently 1,247 pharmacists who have received board certification as an Oncology Pharmacist (BCOP) through the Board of Pharmacy Specialties, an autonomous division of the American Pharmacists Association.5,6 Oncology pharmacists can assist with the pharmacotherapeutic management of medications, including dose adjustments for organ dysfunction and management of toxicities in the oncology patient. As the number of pharmaceutical drugs marketed for cancer continues to grow (in 2011 alone, 10 new cancer treatment drugs were approved), well-trained pharmacists are essential.
Along with the increase in cancer diagnoses, new oncology therapies, and the predicted oncologist shortage, the need for competent practicing pharmacists is critical in the care of patients with cancer. Good communication with patients increases patient satisfaction and improves patient adherence.7 Pharmacists can play a major role in communicating the potential side effects of therapy and providing the patient with a plan of action if they occur, particularly with respect to oral agents. This foundation can begin in pharmacy school, and Anderson and associates argue that it is more important than ever to offer this training to students.8 If future practitioners are to provide competent pharmaceutical care to oncology patients, they must have a solid understanding of drug therapy, patient safety, and the psychosocial aspects of cancer.
Cheung and associates examined oncology education in Canadian medical, pharmacy, and nursing schools as well as in medical residencies.9 Ten of 11 (90.9%) pharmacy colleges and schools responded, with 80% of pharmacy responders spending 1 week or less on cancer education. Only 30% of these institutions required cancer education, only 20% offered an elective course for cancer education, and 70% reported mentioning cancer treatment only a few times throughout their program.
Research suggests that students who receive more information about cancer treatment are more likely to have a positive attitude about treating cancer patients.10 In the United States, some interesting teaching opportunities have been developed. C-Change, a coalition of cancer organizations, developed a competency-based program to expand cancer education in the medical field.11 Four medical centers and universities took this approach and developed various education programs on topics such as cancer screening and survivorship.12 Two of the institutions required the program for their students in addition to providing it for their faculty; 2 others offered free registration to practicing nurses, advanced practice nurses, and physicians. These are innovative methods to increase cancer knowledge among healthcare professionals.
At Creighton University School of Pharmacy and Health Professions, all students receive 16 hours of oncology classroom instruction in the pharmacotherapeutics course during the spring semester of their third year (Table 1). There are numerous topics not covered in the pharmacotherapeutics course and students consistently struggle with concepts in the oncology section, which results in poor examination scores. To address this deficiency, a 1-credit-hour elective course was developed to enhance student knowledge in the area of oncology and expand what students are taught in Pharmacotherapeutics.
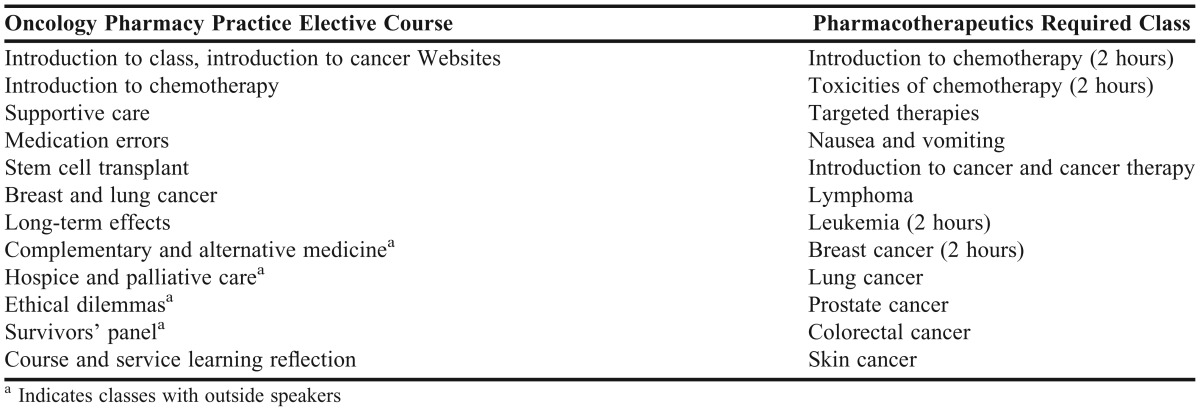
Table 1.
Topics Covered in the Oncology Pharmacy Practice Elective Course and Pharmacotherapeutics Required Course
DESIGN
A 1-credit-hour oncology pharmacy elective course was developed to provide instruction in pharmacotherapeutic management of oncologic diseases. Prerequisites included the fall and spring pharmacology series offered in the second year of the pharmacy program. Offered in the fall semester of the third year, the oncology pharmacy elective course provides an introduction to more complex information that students will receive in the Pharmacotherapeutics course in the spring semester of their third year. The theory behind creating the oncology elective course was that if students had an introduction to oncology topics before the oncology section in Pharmacotherapeutics in their spring semester, their examination scores in Pharmacotherapeutics would improve. The elective course also presented students with other psychosocial topics specific to oncology patients that were not covered in required courses, such as hospice/palliative care, long-term effects, and complementary and alternative medicine (Table 1). The learning objectives of the class were for students to be able to: (1) design and/or evaluate a specific pharmaceutical care plan for the management of major disease processes and provide alternative treatment measures based upon clinical and demographic characteristics; (2) identify potential drug- or disease-induced problems and adverse effects and their incidence, significance, and management; (3) retrieve, integrate, and apply information acquired across the pharmacy curriculum into patient care and management; (4) appreciate the interrelationship of medical, psychosocial, and spiritual issues cancer patients face; and (5) determine how they may impact cancer patients in their community and through their profession. The Mann-Whitney U test was used to compare Pharmacotherapeutics examination scores between students who took and did not take the elective course.
Creighton University School of Pharmacy and Health Professions has both campus and distance pathways, and students from both were allowed to enroll in the elective course.13 The class met for 1 hour each week and attendance was required. The majority of the lectures were provided by 2 faculty members, but guest speakers taught several of the topics (Table 1). Lectures were captured by the software Echo360 (Echo360, Inc., Dulles VA), and the podcast and vodcast were posted for the distance students on the same day the class was held. Although the pathways are asynchronous, the distance students were required to watch the lecture captured in class each week and complete an online post about the lecture prior to the following lecture/discussion to verify “attendance.” They were also required to remotely attend 2 campus classes during the semester using the software Wimba Classroom (Wimba, Inc, New York, NY). Wimba Classroom allows distance students to log into their computer and actively participate in classes. In this classroom environment, the distance students can hear anything that is said by means of a microphone in the classroom and can raise their hands and ask questions just as the campus students can.
Each year, 2 to 4 cancer survivors with various cancers were invited to come into the classroom for an interactive discussion. Students were expected to ask the survivors questions about their diagnoses, treatments, and other relevant topics. These visits were scheduled at the end of the semester to provide the students background on both the physical and psychosocial issues cancer patients may face. Further, the survivors allowed students to see firsthand the effects a cancer diagnosis and treatment can have on a person’s quality of life. Distance students participated synchronously using Wimba Classroom.
Students were informed on the first day of class that they were required to complete an oncology-related service-learning project by the end of the semester and write a 1-page meaningful reflection on what they learned from their volunteer experience. Opportunities consistently available to the campus students included helping with nonprofit organizational fundraising events, such as the Light the Night walk and Race for the Cure, volunteering at the American Cancer Society or the Leukemia/Lymphoma Society, or working at a local health fair. Distance students were responsible for finding their own opportunities, but were encouraged to consider activities associated with or sponsored by these or other established organizations. This requirement also gave students the opportunity to interact with cancer survivors and their families outside of the classroom and helped personalize the disease.
Students were required to reflect on and respond to a weekly question within the course using the school’s learning management system, referred to as Blueline (Blackboard Learn, Washington, DC). Questions may have been related to the topic presented in class, or students may have been assigned to read an article and reflect on what they learned from it. This requirement allowed instructors to track whether distance students were keeping up with assignments and also gave the students an opportunity to think about how they would respond to cancer patients once they are practicing pharmacists. A meaningful reflection is considered integral to the University’s Jesuit values and a key component of the curriculum. For example, during 1 week, students were required to read an article entitled “Letting Go: What Should Medicine Do When It Can’t Save Your Life?” by Atul Gawande, and reflect on it.14
The oncology elective course has grown since 2008, particularly in the distance pathway, a mentor was added in 2011. The mentor is a licensed pharmacist practicing in the area of oncology whose role was to grade the weekly reflections, provide feedback to the students, and track their scores in Blueline. An instructor spoke with the mentor every other week to discuss any issues that may have arisen and any concerns the mentor might have had with individual students.
EVALUATION AND ASSESSMENT
Because the oncology elective course was first offered in 2008, enrollment has grown from 27 students to 45 in 2011, with the majority of growth represented by students in the distance program (4 students in 2008; 19 in 2011). In the fall semester of 2012, the capped enrollment of 52 students was reached. The number of male students averages about 27%. This percentage is consistent with the overall pharmacy school enrollment, which has remained constant over this period.
Students were assessed with 2 open-note quizzes worth 100 points each, a service-learning project with a 1-page reflection worth 100 points, and weekly reflections worth a total of 50 points. The student reflections were thoughtful and allowed them to contemplate situations they may face on both a personal and professional level, such as making a decision to move a loved one or patient to hospice, or how, as future pharmacists, they can contribute to enhancing a patient’s quality of life.
Attendance was mandatory for both campus and distance students. To verify attendance for each class, campus students were required to sign in, and distance students had to write a short reflection on what they learned from the class. Students completed an anonymous, electronic evaluation at the end of the year. To obtain additional verbal feedback from the students, students discussed their service projects and gave the instructors feedback about the course on the last day of class. Students were told prior to the class that they would be asked for feedback during the class so they could reflect on what they thought went well and could be improved. These course and service-learning reflections, in which distance students participated in using Wimba Classroom, were facilitated by the school’s chaplain when possible.
Requiring dual, synchronous participation for the survivors’ discussion and the reflection discussion has been successful. Evaluations from the course suggest that students find this class time the most meaningful, as it ties the semester together for them. Student evaluations for the overall course have been extremely positive. Student comments included that they were pleasantly surprised with the psychosocial aspects of the class, that they enjoyed the service-learning project because it allowed them to interact with cancer survivors, and that the survivors helped personalize the information they had learned in class. When asked if they would retake the class, 96% said they would, and 94% said they would recommend the class to a friend.
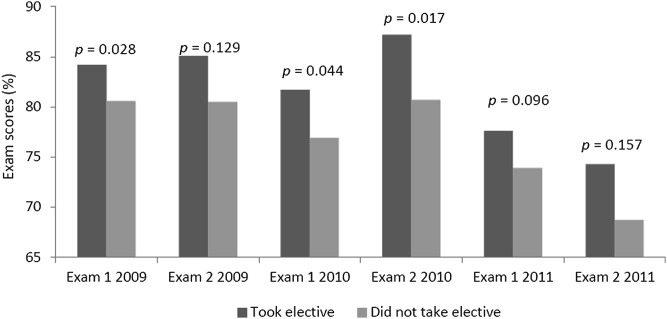
We also assessed scores in the pharmacotherapeutics course to determine if students taking the oncology elective course performed better in the oncology section. The oncology content was spread over 2 examinations during the spring semester. Students who were enrolled in the elective course had higher scores on all of the Pharmacotherapeutics course examinations than did those who did not take the elective course. The Mann-Whitney U test showed significantly higher examination scores for 3 out of 6 examinations: examination 1 in 2009 (p = 0.028), examination 1 in 2010 (p = 0.044) and examination 2 in 2010 (p =0.017) (Figure 1). Examination scores of distance students in 2009 and 2010 were not assessed because they were unavailable.
Figure 1.
Examination Scores in the Oncology Section of the Pharmacotherapeutics Course
DISCUSSION
To our knowledge, no reports on an oncology elective course in a pharmacy curriculum have been published. In 2001, Jazieh and associates published results of a 10-week summer oncology elective course for medical and pharmacy students and undergraduate biology majors.15 Twenty-four students were enrolled in the summer of 1999, and a pretest and posttest showed an improvement in mean test scores from 46.6% to 53% (p = 0.001), which correlated with an improvement in general cancer knowledge as well as knowledge for breast, gastrointestinal, and skin cancers.
During the first year this elective course was offered, we spent minimal time lecturing on topics that would be covered in Pharmacotherapeutics. Feedback from students indicated that they took the elective course to better prepare them for Pharmacotherapeutics, but taking the elective course did not better prepare them to understand the pharmacotherapeutics lectures. With that information, we introduced more topics from the pharmacotherapeutics class and reduced the amount of psychosocial topics so that both areas are covered equally. The most current class topics can be found in Table 1.
Students consistently have questions about the elective course when they are enrolling for fall semester, and unless they know someone who took the course, are not sure what the course offers. To answer some of these questions and help the students make an informed decision when registering, a YouTube video was developed by 1 of the instructors in spring 2012 to tell students about the elective course.16
An unexpected benefit of the class was an increase in the number of requests for both oncology practice experiences in general and the oncology practice experience precepted by the authors. In 2008, 2009, and 2010, there were 14, 23, and 32 requests, respectively, for our oncology practice experience. Among students who took the elective course, the percentages requesting an oncology practice experience in 2008, 2009, 2010, and 2011 were 52%, 42%, 58%, and 68%, respectively. Additionally, 92% of our campus students requested an oncology practice experience in 2011. Thus, with the exception of 2009, the increased number of requests for the oncology practice experience correlates with the increased percentage of our elective course students requesting an oncology practice experience. Further, the class has also enhanced student interest in pursuing a career in oncology pharmacy. Ninety-two percent either strongly agreed (35%) or somewhat agreed (57%) that the class increased their interest in oncology pharmacy. Several former students have completed or are completing specialty residencies in oncology.
An indirect benefit from this elective course was improvement in the quality of lectures in the pharmacotherapeutics course. In the elective course, we consolidated information on certain topics in order to briefly introduce each for 30 to 50 minutes (Table 1), which forced us to deliver the information in an even more organized manner. When making these revisions to the pharmacotherapeutics course, lectures were often shortened with an emphasis on the larger scope of the disease or treatment. Subsequently, Pharmacotherapeutics mentors expressed how much easier the lectures were to follow.
CONCLUSIONS
The oncology elective course has received positive feedback from students, and enrollment continues to increase from positive word-of-mouth from students who have completed the course. The course has resulted in higher Pharmacotherapeutics examination scores in the oncology section and has increased student interest in pursuing a career in oncology pharmacy. We will continue to offer this course to students and plan to expand the offering to visiting students as well.
REFERENCES
- 1.National Cancer Institute. US cancer survivors grow to nearly 12 million. http://www.cancer.gov/newscenter/pressreleases/2011/survivorshipMMWR2011. Accessed August 14, 2012.
- 2.American Cancer Society. Cancer Facts & Figures 2012. Atlanta: American Cancer Society; 2012. [Google Scholar]
- 3.Edwards BK, Howe HL, Ries LA, et al. Annual report to the nation on the status of cancer, 1973-1999, featuring implications of age and aging on US cancer burden. Cancer. 2002;94(10):2766–2792. doi: 10.1002/cncr.10593. [DOI] [PubMed] [Google Scholar]
- 4.American Society of Clinical Oncology. Forecasting the supply of and demand for oncologists: a report to the American Society of Clinical Oncology (ASCO) from the AAMC Center for Workforce Studies. http://www.asco.org/ASCO/Downloads/Cancer%20Research/Oncology%20Workforce%20Report%20FINAL.pdf. Accessed August 14, 2012.
- 5.Board of Pharmacy Specialties. Board of Pharmacy Specialties announces results of 2011 certification and recertification exams. http://www.bpsweb.org/news/pr_031312.cfm. Accessed July 31, 2012.
- 6.Occupational Employment Statistics, Pharmacists May. 2011 (Last modified 3/27/12). Bureau of Labor statistics. http://www.bls.gov/oes/current/oes291051.htm#(1). Accessed August 6, 2012. [Google Scholar]
- 7.Epstein R, Street RL., Jr . Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. Bethesda, MD: National Cancer Institute; 2007. NIH publication. [Google Scholar]
- 8.Anderson C, Plevin DM, McKinnon RA. Educating our students about pharmaceutical care for those living with cancer. Am J Pharm Educ. 2012;76(7):Article 119. doi: 10.5688/ajpe767119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheung WY, Fishman PN, Verma S. Oncology education in Canadian undergraduate and postgraduate training programs. J Cancer Educ. 2009;24(4):284–290. doi: 10.1080/08858190902973143. [DOI] [PubMed] [Google Scholar]
- 10.Smith AP, Lichtveld MY. A competency-based approach to expanding the cancer care workforce. Medsurg Nurs. 2007;16(2):109–118. [PubMed] [Google Scholar]
- 11.Smith AP, Lichtveld MY, Miner KR, Tyus SL, Gase LN. A competency-based approach to expanding the cancer care workforce: proof of concept. Medsurg Nurs. 2009;18(1):39–49. [PubMed] [Google Scholar]
- 12.Peters AS, Schimpfhauser FT, Cheng J, Kostyniak PJ. Effects of a course in cancer prevention on students’ attitudes and clinical behavior. J Med Educ. 1987;62(7):592–600. doi: 10.1097/00001888-198707000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Lenz TL, Monaghan MS, Wilson AF, Tilleman JA, Jones RM, Hayes MM. Using performance-based assessments to evaluate parity between a campus and distance education pathway. Am J Pharm Educ. 2006;70(4):Article 90. doi: 10.5688/aj700490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gawande A. Letting go: what should medicine do when it can’t save your life. The New Yorker. August 2, 2010 http://www.newyorker.com/reporting/2010/08/02/100802fa_fact_gawande. Accessed July 30, 2012. [Google Scholar]
- 15.Jazieh AR, Henle K, Deloney LA, Savidge M, Fulper-Smith M, Nicholas R. The impact of a cancer education program on the knowledge base of participating students. J Cancer Educ. 2001;16(1):8–10. doi: 10.1080/08858190109528715. [DOI] [PubMed] [Google Scholar]
- 16.Pick AM. Welcome to PHA 481. February 13, 2012 Online video clip. YouTube. http://www.youtube.com/watch?v=W0rmZfv4Gg4. Accessed June 20, 2012. [Google Scholar]