Abstract
Objective. To determine whether a required interprofessional geriatric medication activity within a senior mentor program changed pharmacy and medical students’ attitudes regarding interprofessional collaboration.
Design. Interprofessional teams, consisting of 1 third-year pharmacy student and 2 second-year medical students, conducted an in-home interview and medication history with a senior mentor (geriatric patient). The team members then collaboratively analyzed and discussed the patient’s medication use and wrote an essay in which they identified the patient’s medication problems and reflected on the interprofessional experience.
Assessment. Students completed a validated survey instrument to measure pharmacist-physician attitudes about interprofessional collaboration before and after the experience. Pharmacy and medical students’ already generally positive attitudes regarding interprofessional relationships were maintained and, in some instances, significantly improved. Students found the activity enhanced their geriatric training and increased their understanding of an interprofessional team.
Conclusion. Incorporation of a geriatric medication activity within a senior mentor program maintained or improved pharmacy and medical students’ positive attitudes about interprofessional collaboration and enhanced geriatric training within the curriculum.
Keywords: interprofessional, senior mentor, geriatric, attitudes
INTRODUCTION
As healthcare evolves into a team-based, patient-centered practice model, interprofessional collaboration is essential to improving patient outcomes. Interprofessional education will prepare future healthcare professionals with the tools needed to provide patient care as part of a collaborative team. Interprofessional education is defined as 2 or more professions learning with, from, and about each other to improve collaboration and quality of care.1-3 National competencies for the delivery of interprofessional education in the United States have been developed.3 The goal of interprofessional education is for students to learn how to function in an interprofessional team and then to carry the knowledge, skills, and attitudes they learn into their practice.2
Geriatric care presents an ideal environment for training in and the provision of interprofessional health care. The geriatric patient population is increasing, and by 2030, 1 in 4 Americans will be over the age of 65 years.4 There is an increasing need for training pharmacy students in geriatric care.5 With the expansion of team-based care, there has been a call for interprofessional teams that include pharmacists to care for geriatric patients.6 The Partnership for Health in Aging and the American Geriatric Society published a position statement and suggested competencies promoting an interprofessional team-based care approach for geriatric patients. The statement suggests development of further training models for health professions students to be competent providers for geriatric patients within an interprofessional team.6,7
To achieve curriculum objectives in geriatrics, colleges of medicine have created senior mentor programs in which elderly community volunteers are paired with medical students to complete assignments relating to topics covered in the classroom.8,9 These senior mentor programs have had positive effects on medical students’ attitudes toward the care of older adults and successfully expanded the geriatric content of the medical curriculum.
To date, limited data have been published regarding senior mentor programs involving both medical and pharmacy students. Two universities have established interprofessional health mentor programs with high student and mentor satisfaction.10-12 However, no programs have described collaboration between medical and pharmacy students and determined the impact of the program on pharmacy education.
The existing senior mentor program at the Medical University of South Carolina College of Medicine was a curricular model in which an interprofessional team approach to geriatrics could be incorporated. Thus, an interprofessional curricular model was used to develop a geriatric medication activity for medical and pharmacy students within the senior mentor program. The US interprofessional education competency domains of (1) values/ethics for interprofessional practice, (2) roles and responsibilities, and (3) teams and teamwork served as the framework for this activity.3 Additionally, the interprofessional activity fulfilled Standard 11 of the Accreditation Council for Pharmacy Education (ACPE) through active-learning strategies and practice-based exercises. Standard 12 of ACPE and the Center for the Advancement of Pharmaceutical Education (CAPE) outcomes also encourages practicing patient-centered care in collaboration with an interprofessional healthcare team.13-14 The objectives of the study were to: (1) evaluate the impact of participation in the geriatric medication activity on pharmacy and medical students’ attitudes toward interprofessional collaboration, and (2) determine student satisfaction with the experience.
DESIGN
Incorporation of a required interprofessional geriatric medication activity within the senior mentor program provided an opportunity for pharmacy students to apply pharmacotherapy principles and interprofessional skills in caring for a geriatric patient (the senior mentor). The specific learning objectives for the activity were: (1) identify pharmacotherapy issues in a geriatric patient, (2) apply geriatric pharmacotherapy principles and interprofessional team skills with a geriatric patient, (3) describe the value of an interprofessional team, and (4) describe roles and responsibilities of a pharmacist and physician within an interprofessional team.
The SCCP offers a traditional 4-year doctor of pharmacy (PharmD) program delivered to 180 students per class on 3 campuses. Students receive the same lecture-based curriculum delivered at all campuses via distance education. This paper only addresses the interprofessional senior mentor activity at the MUSC campus (n=79).
The MUSC College of Medicine offers a traditional 4-year doctor of medicine program (MD) delivered to 160 students per class. The MUSC Senior Mentor Program has been a component of the college curriculum since 2003. It is a 4-year program for which a uniprofessional team consisting of 2 medical students is paired with a senior mentor who is a community-dwelling geriatric patient. The students work with the senior mentor to learn various aspects of aging and geriatric medicine. The student team visits the mentor during each of the 4 years of medical school and completes various longitudinal activities (eg, nutritional assessment, fall risk assessment, pharmacotherapy assessment).
Clinical Assessment is a required applications-based course offered during the spring of the third year of the PharmD curriculum. The course consists of lectures and weekly laboratory sessions in which active-learning strategies are used to cover a variety of topics. Pharmacy students enrolled in Clinical Assessment have also completed 3 semesters of pharmacotherapy courses, including a module focusing on geriatrics. In addition to weekly laboratory sessions, students are required to complete a few assignments outside of class and laboratory time, including the mentoring activity.
The geriatric medication activity was incorporated into an existing senior mentor program as the initial step toward making the program an interprofessional experience. One third-year pharmacy student was added to each team of 2 medical students for the activity. The 3-member interprofessional teams were provided with objectives and instructions for completing the activity longitudinally during the semester.
Prior to the interprofessional team meeting with their assigned senior mentor, the medical students briefed the pharmacy students on the mentors’ past medical, family, and social history. The medical students knew this information because they had met with the mentor to complete activities during the previous 3 semesters. Once the pharmacy student was briefed, the interprofessional team completed an in-home interview with the senior mentor and obtained a medication history.
After the in-home visit, the teams met to review the information and identify medication-related issues for the senior mentor. The interprofessional teams were grouped into 5 groups of about 50 students, and participated in an interactive discussion of their mentors’ medications that highlighted geriatric pharmacotherapy principles and interprofessional team-based care of geriatric patients. The discussions were led by an interprofessional teaching pair (1 medicine and 1 pharmacy faculty member).
Each interprofessional team had to record its findings and reflect on them in a brief collaborative essay. This essay assignment was used for formative evaluation and the students either passed or failed based on participation as assessed by the faculty members (Table 1).
Table 1.
Logistics of the Semester-Long Interprofessional Geriatric Medication Activity Incorporated Into a Senior Mentor Program
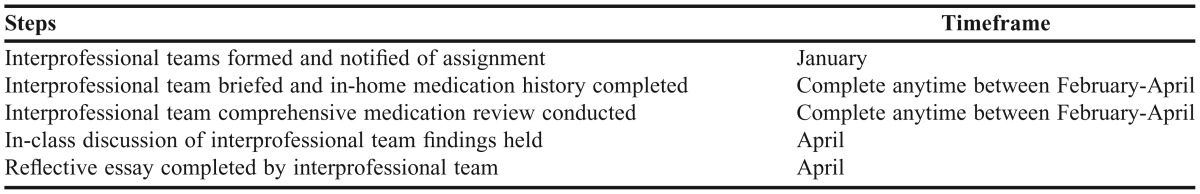
The time required for teams to complete the geriatric medication activity varied depending on the team members and the pharmacotherapy issues of their senior mentor. Students had to work through scheduling conflicts among team members and the mentor to find available meeting times outside of class. On average, the total time the students spent completing the activity over the course of the semester was 4 hours. Faculty time spent in developing the activity, facilitating small-group discussions, and grading the team essays was an average of 8 hours for the semester. Required time for the faculty members was minimized because they were not directly involved with coordinating the student teams, recruiting senior mentors, and solving scheduling conflicts, all of which were coordinated by the senior mentor program in the college of medicine.
EVALUATION AND ASESSMENT
The learning objectives for the activity were evaluated by several methods. Changes in student attitudes toward interprofessional collaboration were assessed by administering a survey instrument before and after the experience. Qualitative comments regarding interprofessional collaboration, including specifics on team-based care for geriatric patients were collected from the collaborative team essays. Student satisfaction with the activity was qualitatively evaluated by assessing student responses to post-activity survey questions. These assessment measures were directly related to the objectives of the study and the learning objectives of the activity.
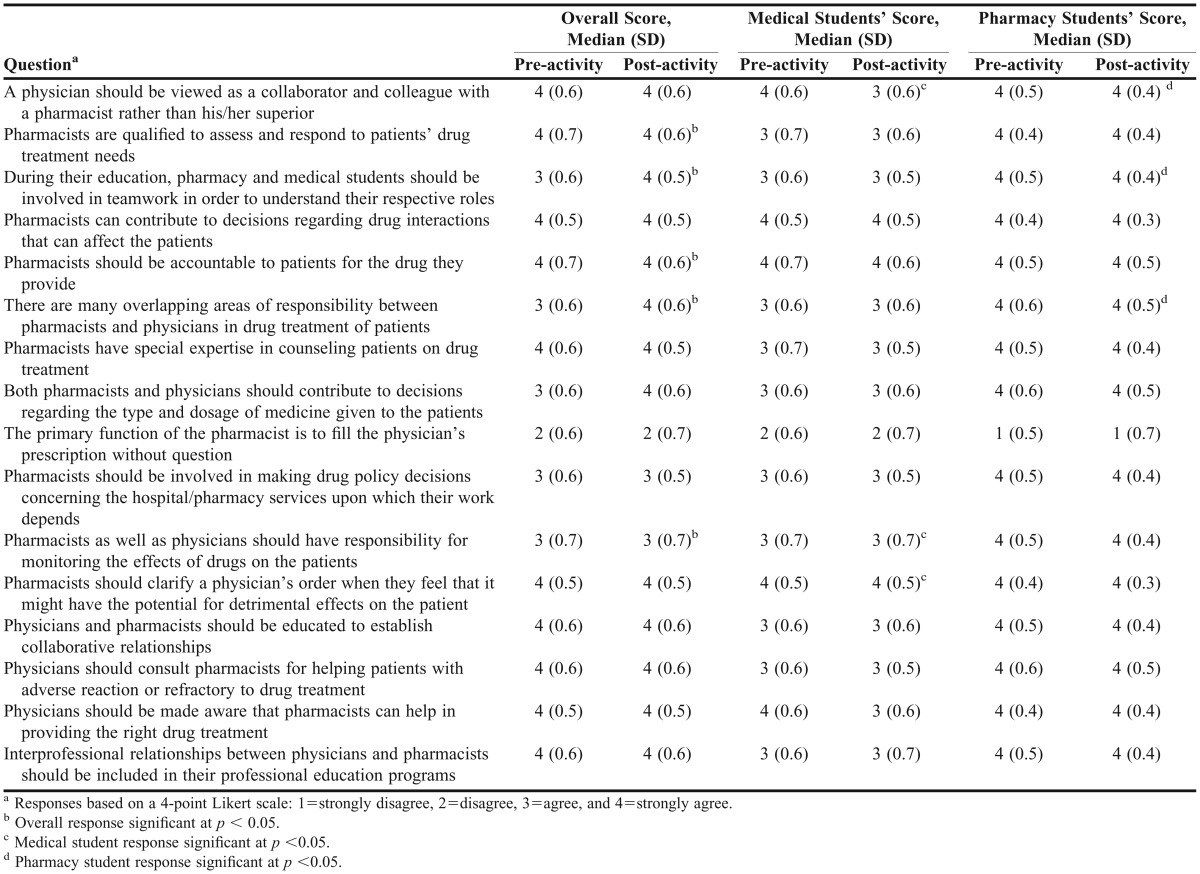
Pharmacy and medical students’ attitudes toward interprofessional collaboration were assessed using a validated questionnaire. The Scale of Attitudes Toward Physician-Pharmacist Collaboration (SATP2C) instrument can be used to evaluate licensed healthcare professionals as well as students in these disciplines. The questionnaire contains 16 items constructed around 3 factors: responsibility and accountability, shared authority, and interdisciplinary education regarding pharmacist-physician collaboration.15,16 The anonymous, voluntary SATP2C questionnaires were administered before and after the interprofessional geriatric medication activity using SurveyMonkey (SurveyMonkey, Inc., Palo Alto, CA). Each student was provided an anonymous code which was used to match responses before and after the experience, and given a week to complete each survey instrument. Responses were indicated using a 4-item Likert scale (ranging from 1 = strongly disagree to 4 = strongly agree). Results from the overall cohort of students included both medical and pharmacy students. In addition, individual student group responses (eg, pharmacy student cohort) were collected.
Qualitative data from the collaborative interprofessional team essays and subjective comments from an open-ended student satisfaction survey instrument were also collected. Themes were identified from the essays to gather further insight into students’ reflections regarding interprofessional collaboration and geriatric care. Student satisfaction data were collected to gage the value of the experience and collect comments for future improvement.
Statistical analyses were performed using SAS, version 9.2 (SAS Institute, Inc. Cary, NC). Pre- and post-activity survey results were analyzed using the Wilcoxon signed rank test. Descriptive statistics were used to illustrate demographic data and qualitative student comments. This project was approved as exempt research by the Institutional Review Board.
Two hundred forty-one students (n=79 pharmacy students and n=162 medical students) participated in the required interprofessional activity. One hundred fifty-six students (n=55 pharmacy students and n=101 medical students) completed both the pre- and post-activity SATP2C survey instrument (65% response rate for matched results). The cohort consisted of 52% male and 48% female students. However, a larger percent of medical students than pharmacy students were male (58% vs 40%, respectively). The mean age of the students was 25 years and was similar between groups. The demographic data were representative of the entire class.
When comparing the matched results of the SATP2C instrument for the entire student cohort, there were significant improvements in students’ responses reflecting their attitudes toward interprofessional collaboration between pharmacists and physicians in 5 out of 16 questions after completing the interprofessional geriatric medication activity. The remaining 11 questions did not change, however, they remained consistently positive (based on a Likert scale response of either 3 or 4) before and after the interprofessional activity. The matched results also were compared within each specific profession. Medical students’ responses to the survey instrument before and after the activity resulted in 1 decreased and 2 significantly improved changes in attitudes toward interprofessional collaboration. In contrast, the pharmacy students’ responses to the survey instrument resulted in 3 significantly improved changes after having completed the activity (Table 2).
Table 2.
Comparison of Pre-activity Survey Results and Post-activity Survey Results for Students Participating in an Interprofessional Geriatric Medication Activity (N=156)
Qualitative reflective data were collected from the collaborative team essays regarding learning objectives of the activity. The most common themes that emerged included: (1) overall value of interprofessional collaboration; (2) value of interprofessional teams, particularly with regard to polypharmacy issues encountered in the geriatric patient population; and (3) professional role identity, ie, learning the unique skills that pharmacists and medical doctors provide within a healthcare team. Student satisfaction responses were similar to the essay themes; overall the students were satisfied with the interprofessional learning experience. In addition to student satisfaction with the interprofessional team, they appreciated the opportunity to apply geriatric pharmacotherapy/pharmacology principles and valued working with a patient. The most common student comments regarding future improvements for the activity included: (1) continuing to work through the scheduling conflicts of the 2 colleges and (2) integrating pharmacy students into the senior mentor program earlier so that more interprofessional activities would be possible.
DISCUSSION
Incorporation of an interprofessional geriatric medication activity within an existing senior mentor program as a requirement for pharmacy and medical students fulfilled US interprofessional education competencies and significantly improved students’ attitudes toward interprofessional collaboration. Students reported that after completing the activity they valued interprofessional collaboration, were more knowledgeable about other team members’ roles, and enjoyed working with a geriatric patient to apply teamwork skills. The majority of students were highly satisfied with the experience.
This study adds to the current literature in multiple areas. This activity went beyond a descriptive approach and used validated assessment data in addition to student satisfaction reports. Integrating the activity into an existing senior mentor program and transitioning the program from uniprofessional to interprofessional was a new method to deliver interprofessional education within the pharmacy curriculum at our institution. The majority of information published on senior mentor programs only includes data from colleges of medicine.8,9 Our work builds on the limited data reported for successful interprofessional senior/health mentor programs.10-12 This activity used the US interprofessional education competencies as a framework and also fulfilled ACPE and CAPE outcomes for pharmacy education.3,13,14 It met a perceived need in pharmacy education by increasing exposure to geriatrics within the curriculum. In addition, the activity allowed students to learn the value of interprofessional team-based care specifically for the geriatric population; a concept that has been discussed at a national level in the United States.5,6,13
To our knowledge, this is the first reported interprofessional education activity associated with a senior mentor program that examined the collaborative relationship between pharmacy and medical students. The psychometrically validated SATP2C instrument was used to evaluate this required activity in a large cohort of students. Use of the SATP2C instrument is a strength of this study because it is the only validated instrument that is specific for pharmacist and physician collaboration. Our study demonstrated that the interprofessional activity positively influenced the students’ attitudes toward collaboration. Students’ responses to 5 of 16 questions were significantly more positive on the post-activity survey instrument compared with pre-activity survey results. However, responses to 11 of 16 questions did not significantly improve, and there was no change in student attitudes regarding the 3 factors on the questionnaire. When the results were separated by profession, there were 3 positive changes for pharmacy students and 2 positive changes for medical students. In addition, there was 1 negative change among medical students. This negative change in attitude is difficult to explain as it does not trend along with the remaining data. Despite the negative change in attitude reflected in student responses to this single question, responses were still positive overall. These findings are similar to other reports in the literature for interprofessional education activities. It is difficult to observe major changes in attitudinal surveys because of the positive attitudes most students report on pre-survey instruments. In addition, health professions’ students other than medical students (eg, pharmacy students, nursing students) tend to have more positive attitudes regarding interprofessional teamwork and collaboration.15,17,18 This goes along with the principle of least interest, where traditionally the group with the most power is typically least interested in collaboration.15,19 These remain issues that should continue to be addressed in development and delivery of interprofessional education models.
Although our findings add to the literature and address a curricular need, our study has limitations. The overall response rate to the survey instruments was 65% and must be considered when generalizing the results. The matching of pre- and post-activity survey responses hindered the response rate, but strengthened the study design.
Further statistical testing of the results from the SATP2C instrument, including reliability testing and emerging constructs, could have added to the results. Additionally, the only significant changes in students’ responses occurred on individual survey questions and not within the 3 factors covered on the questionnaire, which should be considered when interpreting the results.
The activity described was a single assignment implemented longitudinally over 1 semester at 1 institution. Evaluating an entire interprofessional senior mentor program with multiple activities implemented over 4 years of the curriculum may have strengthened the results and had a larger impact on students. Using a control group in the study design may have changed the results; however, for purposes of this study the pre- and post-activity design was necessary because all students had to have an equivalent educational experience.
Other activities in which the students were involved over the course of the semester (eg, interprofessional electives, volunteering at interprofessional student-run free clinics) may have confounded the results. The clinical/educational significance is also a limitation. Although positive changes were seen in responses to 5 of 16 questions regarding attitudes about interprofessional collaboration, in many instances those changes were limited to a smaller standard deviation or an improvement of only 1 point on the Likert scale. However, as previously discussed, students already had positive attitudes about interprofessional collaboration prior to the activity, so meaningful changes were difficult to document/quantify. Finally, while the study moved beyond satisfaction data to evaluate attitudes, determining the effects of the activity on student behavior and patient outcomes would have strengthened the results. All of these limitations should be considered as future areas of research for interprofessional education.
This required interprofessional geriatric medication activity has been continued as part of the senior mentor program and embedded into the curriculum for pharmacy and medical students. Based on student satisfaction data, the next step at MUSC is to determine how pharmacy students can be integrated into all 4 years of the senior mentor program. Transitioning the senior mentor program to a fully interprofessional experience and expanding it to include students from other health disciplines such as nursing and physical therapy is being considered. Other colleges and schools of pharmacy could consider implementing this required interprofessional activity to help fulfill ACPE standards and US interprofessional education competencies. Because of the resources required for this activity, it would be easiest to implement at a college or school of pharmacy associated with a medical school that already has a senior mentor program established.
SUMMARY
Incorporation of a geriatric medication activity within a senior mentor program significantly improved pharmacy and medical students’ attitudes about interprofessional collaboration. Students improved their attitudes based on 5 out of 16 questions regarding interprofessional collaboration after completing the required activity. However, the remaining questions as well as the 3 factors of the survey instrument were not improved, but the students had a high regard for collaboration at baseline and maintained their positive attitude. This activity fulfilled US interprofessional education competencies and pharmacy education standards. In addition to demonstrating positive interprofessional outcomes, it also enhanced geriatric training within the curriculum. Students were satisfied with the activity and other colleges and schools of pharmacy could consider implementing similar activities with senior mentor programs to fulfill curricular needs.
REFERENCES
- 1.Center for Advancement of Interprofessional Education (CAIPE) 20022012 http://www.caipe.org.uk/about-us/the-definition-and-principles-of-interprofessional-education/. Accessed April 12. [Google Scholar]
- 2.Buring S, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. 2009;73(3):Article 29. doi: 10.5688/aj730459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, DC: Interprofessional Education Collaborative; 2011. [Google Scholar]
- 4.Day JC. Population Projections of the United States, by Age, Sex, Race, and Hispanic Origin: 1995-2050. Current Population Reports Series. P25, No. 1130. Washington, DC: U.S. Government Printing Office; 1996. [Google Scholar]
- 5.Odegard PS, Breslow RM, Koronkowski MJ, Williams BR, Hudgins GA. Geriatric pharmacy education: strategies for the future. Am J Pharm Educ. 2007;71(3):Article 47. doi: 10.5688/aj710347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Partnership for Health in Aging Workgroup on Interdisciplinary Team Training. Position statement on interdisciplinary team training in geriatrics: an essential component of quality healthcare for older adults. 2010 doi: 10.1111/jgs.12822. http://www.americangeriatrics.org/files/documents/pha/PHA_Full_IDT_Statement.pdf. Accessed April 12, 2012. [DOI] [PubMed] [Google Scholar]
- 7.Partnership for Health in Aging Workgroup on Multidisciplinary Competencies in Geriatrics. Multidisciplinary competencies in the care of older adults at the completion of the entry-level health professional degree. 2010 http://www.americangeriatrics.org/files/documents/pha/PHAMultidiscComps.pdf. Accessed April 12, 2012. [Google Scholar]
- 8.Eleazer GP, Wieland D, Roberts E, Richeson N, Thornhill J. Preparing medical students to care for the older adults: the impact of a senior mentor program. Acad Med. 2006;81(4):393–398. doi: 10.1097/00001888-200604000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Eleazer GP, Stewart TJ, Weiland D, Anderson MB, Simpson D. The national evaluation of senior mentor programs: older adults in medical education. J Am Geriatr Soc. 2009;57(2):321–326. doi: 10.1111/j.1532-5415.2008.02100.x. [DOI] [PubMed] [Google Scholar]
- 10.Collins L, Arenson C, Rattner S, et al. The health mentors program: a longitudinal chronic illness mentorship program. 2012 MedEdPORTAL; 2009. www.mededportal.org/publication/4062. Accessed April 12. [Google Scholar]
- 11.Collins L, Arenson C, Jerpbak C, Kane P, Dressel R, Antony R. Transforming chronic illness care education: a longitudinal interprofessional mentorship curriculum. J Interprof Care. 2011;25(3):228–230. doi: 10.3109/13561820.2011.552815. [DOI] [PubMed] [Google Scholar]
- 12.Doucet S, Andrews C, Godden-Webster A, Lauckner H, Nasser S. The Dalhousie health mentors program: introducing students to collaborative patient/client-centered practice. J Interprof Care. 2012;26(4):Epub. doi: 10.3109/13561820.2012.680631. [DOI] [PubMed] [Google Scholar]
- 13.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines 2011. 2012 https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed April 12. [Google Scholar]
- 14.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education educational outcomes 2004. 2012 http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed April 12. [Google Scholar]
- 15.Van Winkle LJ, Fjortoft N, Hojat M. Validation of an instrument to measure pharmacy and medical students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Educ. 2011;75(9):Article 178. doi: 10.5688/ajpe759178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hojat M, Gonnella JS. An instrument for measuring pharmacist and physician attitudes towards collaboration: preliminary psychometric data. J Interprof Care. 2011;25(1):66–72. doi: 10.3109/13561820.2010.483368. [DOI] [PubMed] [Google Scholar]
- 17.Whitehead C. The doctor dilemma in interprofessional education and care: how and why will physicians collaborate? Med Educ. 2007;41(10):1010–1016. doi: 10.1111/j.1365-2923.2007.02893.x. [DOI] [PubMed] [Google Scholar]
- 18.Ginsburg L, Tregunno D. New approaches to interprofessional education and collaborative practice: lessons from the organizational change literature. J Interprof Care. 2005;19(Suppl):177–187. doi: 10.1080/13561820500083105. [DOI] [PubMed] [Google Scholar]
- 19.Waller W, Hill R. The Family: A Dynamic Interpretation. Dryden; New York: 1951. [Google Scholar]


