Abstract
Objectives
To estimate the prevalence of positive screens for social-emotional problems among preschool-aged children in a low-income clinical population and to explore the family context and receptivity to referrals to help guide development of interventions.
Design
Observational, cross-sectional study.
Setting
Two urban primary care clinics.
Participants
A total of 254 parents of 3- and 4-year-old children at 2 urban primary care clinics.
Main Outcome Measures
Score on a standardized screen for social-emotional problems (Ages and Stages Questionnaire: Social-Emotional) and answers to additional survey questions about child care arrangements, parental depressive symptoms, and attitudes toward preschool and behavioral health referrals.
Results
Twenty-four percent (95% CI, 16.5%-31.5%) of children screened positive for social-emotional problems. Among those screening positive, 45% had a parent with depressive symptoms, and 27% had no nonparental child care. Among parents of children who screened positive for social-emotional problems, 79% reported they would welcome or would not mind a referral to a counselor or psychologist; only 16% reported a prior referral.
Conclusions
In a clinical sample, 1 in 4 low-income preschool-aged children screened positive for social-emotional problems, and most parents were amenable to referrals to preschool or early childhood mental health. This represents an opportunity for improvement in primary prevention and early intervention for social-emotional problems.
Social-Emotional Development has been defined as “the developing capacity of the child from birth through five years of age to form relationships and regulate emotions.”1 In the short term, children who do not experience appropriate social-emotional development are likely to have limitations in their ability to learn and may face exclusion from learning environments.2,3 In the long term, they are at increased risk for mental illness, delinquency, poor achievement in school, and poor physical health in adulthood.4-7 Thus, the American Academy of Pediatrics and Bright Futures recommend “psychosocial/behavioral assessment” during well-child care.8
Despite expert consensus supporting “assessment,” specific clinical protocols for social-emotional screening in the preschool years are lacking. Standardized screening tools exist, and some states require medical providers to administer them as part of the Early Periodic Screening, Diagnosis, and Treatment program. However, the practical implications of standardized screening in primary care (including the proportion of patients who would screen positive, the community resources that may be needed to provide further evaluation based on positive screens, family circumstances that may co-occur and limit referral success, and parents’ receptivity to various types of interventions) have not been studied. Because poverty is a risk factor for both social-emotional problems9 and limited access to mental health services,10 these questions are especially important for low-income children.
Prior studies11-14 of social-emotional problems in preschool-aged children have used a variety of sampling methods and outcome definitions, resulting in a wide range of prevalence estimates (5%-26%). Few such studies have been performed in clinical primary care settings, and those have used more exhaustive assessments of the child’s mental health, rather than a screening tool that is practical for primary care use.12,15,16 Furthermore, to our knowledge, there are no studies of screening for social-emotional problems in urban primary care clinics serving low-income children. The gap in the literature that we sought to address was not the underlying prevalence of psychopathology in this age group, nor the validity of a screening tool, but the potential burden on primary care and referral systems that could be generated by universal screening of low-income children in primary care.
With regard to potential interventions, multiple studies17-26 have demonstrated the effectiveness of high-quality preschool, home visiting, parenting programs, and early childhood mental health services in improving behavioral trajectories. However, primary care doctors’ attempts to connect children with these services often are not successful.15,27-31 The reasons for low rates of completed referrals are not well understood. To develop practical guidelines for screening and intervention, the family and social context of social-emotional problems, as well as parental attitudes toward a physician’s referral to preschool and early intervention services, must be examined.
Beyond referral for assessment and treatment, primary care providers may play a key role in the prevention of social-emotional problems. High-quality child care promotes social-emotional health,17,18,32 and the American Academy of Pediatrics recommends promoting quality child care for all families.33 This may be particularly important for children whose parents report subthreshold levels of problem behaviors using screening instruments.34 An understanding of the full distribution of social-emotional screening scores, along with a picture of current child care use, among low-income children may inform guidelines for addressing social-emotional health across the spectrum of preschooler behavior.
The purposes of our study were to examine the distribution of social-emotional screening scores among 3- and 4-year-old children in a low-income clinical population and to explore the family context for and receptivity to potential interventions that promote healthy social-emotional development.
METHODS
STUDY DESIGN AND SAMPLE
This was a cross-sectional study of 3- and 4-year-old children presenting for well or ill visits to 2 urban primary care clinics in Cincinnati, Ohio, between June and November 2010. Participants were recruited during morning, afternoon, and evening sessions at a large academic hospital–based clinic and during afternoon sessions at a smaller affiliated community health center. A consecutive sample was identified at registration during clinic sessions when study personnel were present. Our study consisted of a written survey completed by parents at the clinic visit and a subsequent chart review. Our study was approved by the institutional review board. Written informed consent was obtained from all participants.
All 36- to 59-month-old children registering for any primary care visit were eligible, except those who met the following exclusion criteria: (1) Children with severe developmental delay were excluded because their expected social-emotional milestones differ from those of a typically developing child. (2) Children who were in acute distress were excluded to avoid interference with their medical care. (3) Children who had been ill for more than 3 days were excluded because the screening tool had been normed in healthy children. It was reasoned that acute illness may impact the child’s behavior and that the parent may recall the child’s most recent behavior and not the behavior that is typical for the child when healthy. (4) Participants who did not speak English were excluded for feasibility reasons; less than 1% of each clinic population is non–English-speaking. (5) Children who were not accompanied by a parent or legal guardian were excluded.
SURVEY INSTRUMENT AND ADMINISTRATION
Parents completed a written survey, consisting of an age-appropriate Ages and Stages Questionnaire: Social-Emotional (ASQ:SE) and supplemental questions. The ASQ:SE is a standardized screening tool completed by parents. Per the ASQ:SE User’s Guide, parents of children 36 to 41 months old, 42 to 53 months old, and 54 to 60 months old completed the 36-, 48-, and 60-month version of the screen, respectively. The 31 to 33 items on the ASQ:SE ask whether the child “most of the time,” “sometimes,” or “rarely or never” displays behaviors in the domains of self-regulation, compliance, communication, adaptive functioning, autonomy, affect, and interaction with people. Each version of the ASQ:SE has a cutoff score above which further evaluation is recommended, based on receiver operating characteristic analysis.35 The ASQ:SE has a 71% to 85% sensitivity and a 90% to 98% specificity, when compared with the Child Behavior Checklist and professional diagnosis of a social-emotional disability.35,36 Internal consistency, as measured by the Cronbach coefficient α, is 0.67 to 0.91.35 The screen takes 10 to 15 minutes to complete and is written at a fifth- to sixth-grade reading level.
Closed-ended supplemental questions, adapted from national surveys,37-39 addressed prior referrals to developmental or behavioral health services, parental attitudes toward referral to preschool, home visiting, parenting classes, or early childhood mental health services by their child’s physician, current child care arrangements, and demographic information. Parental depressive symptoms were measured with the Mental Health Index–5, a 5-item screening tool that has an area under the receiver operating characteristic curve of 0.892 for detecting major depression40 and a Cronbach α of 0.84.41
Given the prevalence of low literacy in the clinic population, respondents were offered assistance with completing the questionnaire. Two parents received such assistance. For ethical reasons, the principal investigator or research assistant scored each ASQ:SE immediately after completion, explained the child’s score to the parent, and provided a document that included the child’s score, an explanation of the score, and a list of local preschool and behavioral health resources. A copy of this document was scanned into the child’s electronic medical record.
CHART REVIEW
To assess the validity of parent responses to questions about prior referrals, the electronic medical records of patients who screened positive on the ASQ:SE were reviewed for referrals for behavior problems at prior visits. This was done by a review of the assessment and plan section of all visit notes dating back to the child’s first birthday.
An additional chart review assessed whether respondents differed from nonrespondents and whether patients differed between the 2 study sites. We reviewed the charts of a random sample of 100 patients who were 3 to 4 years’ old and seen at the 2 sites during the study period. Race, insurance status, prior diagnosis of a behavior problem, and maternal age were compared with these characteristics in a sample of enrolled patients.
DATA MANAGEMENT AND STATISTICAL ANALYSIS
The distribution of ASQ:SE scores as a continuous variable was described. We also calculated the proportion of children with scores above the established cutoff and the proportion of children with scores between the national median and the established cutoff. If the ASQ:SE was missing greater than 3 answers, it was not included in our analysis.35
For the second part of the survey, summary statistics of parents’ responses were expressed as proportions. Data were entered into and managed by electronic data capture tools (research electronic data capture [REDCap]) hosted at Cincinnati Children’s Hospital Medical Center.42 Data were analyzed using SAS software, version 9.2.43
RESULTS
PARTICIPANT CHARACTERISTICS
Of 295 eligible parents who were approached, 254 (86%) agreed to participate: 231 were recruited from the Pediatric Primary Care Center and 23 from the Hopple Street Neighborhood Health Center. Participant characteristics are shown in Table 1. Participants from the 2 study sites did not differ from each other on any of these characteristics, and the samples were combined. Study patients were not significantly different with respect to race, insurance status, maternal age, and history of diagnosis of a behavior disorder from the sample of non-participants.
Table 1. Characteristics of Enrolled Children Who Responded.
| Characteristic | No. (%) |
|---|---|
| Age of child, y (n=254) | |
| 3 | 130 (51) |
| 4 | 124 (49) |
| Sex of child (n=254) | |
| Female | 132 (52) |
| Male | 122 (48) |
| Respondent is a primary caregiver? (n=254) | |
| Yes | 225 (89) |
| No | 29 (11) |
| Respondent relationship to child (n=236) | |
| Mother | 211 (89) |
| Father | 14 (6) |
| Grandparent | 8 (3) |
| Other relative/foster parent | 3 (1) |
| Age of respondent, y (n=221) | |
| 18-21 | 20 (9) |
| 22-25 | 77 (35) |
| 62-35 | 102 (46) |
| >36 | 22 (10) |
| Race of respondent (n=234) | |
| White, non-Hispanic | 41 (18) |
| Black, non-Hispanic | 183 (78) |
| Hispanic | 1 (0.4) |
| Othera | 9 (4) |
| Highest level of education completed by respondent (n=236) |
|
| <High school | 7 (3) |
| High school | 146 (62) |
| College or more | 83 (35) |
| Insurance status (n=253) | |
| Medicaid | 230 (91) |
| Private | 22 (9) |
| No insurance | 1 (0.4) |
| Child care arrangementsb | |
| Center-based child care or preschool (n=251) | 153 (61) |
| Family child care home (provider not related to child) (n=249) |
30 (12) |
| Care from a relative (in child’s home or relative’s home) (n=247) | 75 (30) |
| No nonparental child care (n=250) | 49 (20) |
One Asian and 8 “other” respondents
Proportions add up to more than 100% because some children had more than 1 child care arrangement or attended more than 1 center.
ASQ:SE SCORES
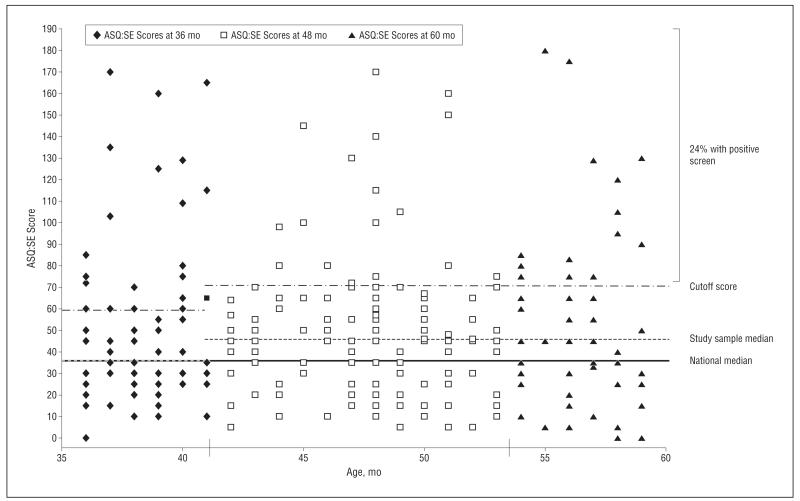
Prevalence of positive screens was 24% (95% CI, 16.5%-31.5%) and did not differ by age. The distribution of ASQ:SE scores is shown in our Figure. Higher scores indicate greater risk for social-emotional problems. For the 36-month version of the ASQ:SE, the median score in our sample was similar to the national median. For the 48- and 60-month versions, the median in our sample was 45 as compared with 36 and 35 in the national normative sample.35 This was statistically significant for the 48-month version (P < .05). Among children screened with the 48- and 60-month versions, 55% scored above the national median, indicating a modest shift in both the body and tail of the distribution.
Figure.
Distribution of Ages and Stages Questionnaire: Social-Emotional (ASQ:SE) scores. The cutoff score was established by developers of the ASQ:SE by using receiver operating characteristic curves. Scores above the cutoff represent positive screens for social-emotional problems. The national median represents the median value in a nationally representative sample used to normalize the ASQ:SE.
FAMILY CHARACTERISTICS OF CHILDREN SCREENING POSITIVE FOR SOCIAL-EMOTIONAL PROBLEMS
Of the 62 children screening positive for social-emotional problems, 43 (69%) had a parent with a high school education or less, and 58 of 61 children (95%) had Medicaid. Almost half (45%) had a parent with depressive symptoms. Child care arrangements varied (Table 2).
Table 2. Family Characteristics of Children Screening Positive for Social-Emotional Problems on Ages and Stages Questionnaire: Social-Emotional.
| Characteristic | No. (%) |
|---|---|
| Highest level of education completed by parent/guardian (n=58) |
|
| High school or less | 43 (74) |
| College or more | 15 (26) |
| Insurance status (n=61) | |
| Medicaid | 58 (95) |
| Private insurance | 2 (3) |
| No insurance | 1 (2) |
| Positive depression screen in parent/guardiana (n=56) | |
| Yes | 25 (45) |
| No | 31 (55) |
| Child care arrangements (n=61) | |
| No nonparental child care | 17 (28) |
| Center-based child care or preschool | 22 (36) |
| Family child care home (provider not related to child) | 4 (6.5) |
| Care from a relative (in child’s home or relative’s home) | 4 (6.5) |
| Multiple child care arrangements | 14 (23) |
Measured with the Mental Health Index–5.
PRIOR REFERRAL AND ATTITUDES TOWARD REFERRAL TO BEHAVIORAL HEALTH SERVICES
No parents reported having been referred previously to parenting classes, and 6 reported a previous referral to a home visiting program. Of the 62 parents of the 62 children who screened positive for social-emotional problems, only 10 (16%) reported that their child had been referred previously to a developmental specialist, counselor, psychologist, or psychiatrist. Chart review showed a similar rate; 13% had a documented referral for a behavior problem prior to the study visit. Attitudes toward potential referrals are shown in Table 3. Seventy-nine percent (44 of 56) of parents of children who screened positive on the ASQ:SE said they “would welcome” or “would not mind” a referral to a counselor or psychologist. Although 11% (6 of 54) “would be very annoyed” by a referral to home visiting, 74% (40 of 54) “would welcome” or “would not mind” such a referral. Only 57% (31 of 54) “would welcome” or “would not mind” a referral to parenting classes, and 20% (11 of 54) reported they “would be very annoyed.”
Table 3. Parents’ Attitudes Toward Potential Referrals When Asked: ”If Your Child’s Doctor Recommended Each of the Following Services, How Do You Think You Would Feel?”.
| No. (%) |
||||
|---|---|---|---|---|
| Children | Would Welcome the Referral |
Would Not Mind at All |
Would Be Mildly Annoyed |
Would Be Very Annoyed |
| Children Who Screened Positive on ASQ:SE (n=54) a | ||||
| Enrolling in parenting classes | 13 (24) | 18 (33) | 12 (22) | 11 (20) |
| Enrolling in a home visiting program | 15 (28) | 25 (46) | 8 (15) | 6 (11) |
| Taking your child to a counselor or psychologist (n=56) | 25 (45) | 19 (34) | 9 (16) | 3 (5) |
|
| ||||
| Children Not Enrolled in Center-based Child Care (n=94) b | ||||
| Enrolling your child in preschool | 80 (85) | 14 (15) | 0 (0) | 0 (0) |
|
| ||||
| Children Who Screened Positive on ASQ:SE and Are Not Enrolled in Center-based Child Care (n=25) c | ||||
| Enrolling your child in preschool | 21 (84) | 4 (16) | 0 (0) | 0 (0) |
Abbreviation: ASQ:SE, Ages and Stages Questionnaire: Social Emotional.
Responses were missing for 8 participants in this category.
Responses were missing for 7 participants in this category.
Responses were missing for 2 participants in this category.
CHILD CARE ARRANGEMENTS AND ATTITUDES TOWARD REFERRAL TO PRESCHOOL
Current child care arrangements are shown in Table 1. Overall, 61% (153 of 251) of parents reported that their children were enrolled in Head Start or another center-based preschool or child care program. Of the 81 children who scored above the median but below the cutoff on the ASQ:SE, 45 (56%) were enrolled in center-based preschool or child care. Many children attended more than 1 center. Of a total of 159 centers attended by participants, 30 (19%) were rated as high quality by the Ohio Department of Job and Family Services. Of the 98 parents whose children were not already enrolled in center-based child care, 100% reported that they would welcome the referral or would not mind if the child’s doctor recommended that the child enroll in preschool (Table 3).
COMMENT
Our findings suggest that 1 in 4 low-income preschool-aged children screens positive for social-emotional problems on a validated instrument. Among children screening positive, only 1 in 6 had been referred previously to behavioral health services. However, a majority of parents indicated receptivity to a referral to a counselor or psychologist. Our findings also demonstrate suboptimal enrollment in high-quality center-based child care or preschool, which can promote healthy social-emotional development for all children. Almost all parents reported that they would welcome or would not mind a physician’s referral to preschool.
Prior studies13,14 of preschool-aged children have shown a prevalence of 1% to 13% for specific psychiatric disorders such as depression, attention-deficit/hyperactivity disorder, and oppositional defiant disorder. For social-emotional problems in general, prior studies have estimated that the prevalence is 13% (as measured by full evaluation by a psychologist) in a sample of 2- to 5-year-old children from pediatric private practices12 and 24% (as measured by the ASQ:SE) in foster children aged 6 months to 5 years.44 Although we would expect that a sample of foster children would be at higher risk for social-emotional problems than our sample, the equal prevalence is not surprising because the study of foster children included younger children who were less likely to screen positive. Our study, the first to assess prevalence in an urban primary care sample of 3- and 4-year-old children, shows that social-emotional screening would create a heavy burden on an urban pediatric practice, without partnering closely with families and communities and developing efficient office systems to facilitate those partnerships. Office systems must exist for collecting information from family members and child care providers to aid in interpretation of the screen, for staying apprised of the capacity and referral criteria of community behavioral health services, and for making referrals in ways that lead to successful connection with services.
Although positive social-emotional screens cannot be interpreted in isolation and should not always lead to referral, our study suggests that social-emotional problems in this age group are likely underidentified and undertreated because only 16% of children with positive social-emotional screens had been previously referred to a home visiting, parenting, or early childhood mental health program. The 79% of parents that reported receptivity to a referral to a counselor or psychologist represent a potential opportunity for connection with helpful services. Parents were less receptive to referrals to home visiting and parenting programs, suggesting that further research is needed to identify reasons for resistance and to increase acceptability of these services.
In addition to being shaped by parents’ receptivity to interventions, protocols for addressing social-emotional problems should consider the family context in which they occur. Almost half of the children screening positive for social-emotional problems in our sample had a parent with depressive symptoms. Maternal depression is a predictor of poor compliance with both well-child visits and mental health visits.45,46 Therefore, although the association between maternal depression and child social-emotional problems has been shown previously, our findings emphasize the need to consider parental mental health in devising approaches that reliably connect children with needed services and that encourage parents to seek care for themselves.47,48 Future research should explore other barriers to successful referrals, as well as the effectiveness of various strategies to facilitate referrals, such as those that have shown promise in connecting families to Help Me Grow27 or social services.49
In addition to the higher prevalence of positive screens in our sample compared with national norms, we also noted a modest but significantly higher median ASQ:SE score for children taking the 48-month version. Although the clinical significance of a subthreshold but higher-than-median score is unknown, this group of children may be important to consider when devising strategies for promoting social-emotional health. Further studies are needed in behavioral trajectories and management of children who do not screen positive but exhibit a number of symptoms suggestive of social-emotional problems. Strategies to shift the curve of a population distribution, in addition to focusing on the tail, can have an important public health impact overall.50
High-quality center-based preschool programs are known to promote healthy social-emotional development, and promoting such programs may be one useful strategy for shifting the distribution.17,18,34 Given that all parents of children who were not already in preschool reported that they would be receptive to a physician’s referral, our study demonstrates that there is opportunity for the physician to play a role in improving enrollment rates and promoting social-emotional health. Studies by Silverstein et al51 have shown that 77% of pediatricians are willing to help with preschool enrollment and that a clinic-based referral system can increase enrollment rates in Head Start.30
Our study had some limitations. Although our chart review showed no differences between respondents and nonrespondents, it remains a possibility that there was some nonresponse bias. Parents who agreed to participate may have been more likely to have concerns about their children’s behavior than those who declined. Similarly, our chart review showed no differences between random samples from the 2 clinics, but we were able to obtain only a small sample from the community health center, and parents who seek care for their children there may have different characteristics from those at the academic health center. Social desirability bias may have falsely inflated the rates at which parents reported receptivity to a referral. In addition, the rate of previous referral was obtained by parent report, which may be inaccurate, and by chart review, which only included referrals that were documented by the physician. Despite this limitation, the low referral rate remains important because a referral not remembered by the parent is unlikely to have led to a successful intervention. Also, the rate of prior referrals did not include referrals made at the visit at which the parent completed the survey. Therefore, the number of children who screened positive on the ASQ:SE but had not been previously referred may include children whose behavior problems had only recently begun and were appropriately identified and addressed at the study visit via the current standard of care.
Positive screens for social-emotional problems, using an instrument that is becoming widely used in primary care, are prevalent in a low-income clinical population. This finding emphasizes the need for clear guidelines for screening in primary care and a systematic approach to addressing positive screens. Furthermore, clinicians should be attentive to more universal strategies to prevent social-emotional problems, such as referral to high-quality center-based child care or preschool.
In counseling parents, clinicians should be encouraged that most parents would welcome a referral to behavioral health services or preschool. Future research should work to explain and close the gap between the percentage of families that need and want preventive or early intervention services and the percentage of families that actually enroll in such programs. To create optimal systems for promoting social-emotional development, a more complete understanding is needed not only of physician barriers to providing referrals and of families’ barriers to follow-up, but also of the potential role of collaboration with the community in detecting, assessing, and treating social-emotional problems.
Acknowledgments
Funding/Support: This project was supported by funds from the Bureau of Health Professions, the Health Resources and Services Administration, and the Department of Health and Human Services, under a Ruth L. Kirschstein National Research Service Award (T32 HP10027-12-00). Biostatistical and data management support was provided in part by an Institutional Clinical and Translational Science Award (National Institutes of Health/National Center for Research Resources grant 5UL1RR026314-3).
Footnotes
Author Contributions: Dr Brown had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Brown, Copeland, and Kahn. Acquisition of data: Brown. Analysis and interpretation of data: Brown, Copeland, Sucharew, and Kahn. Drafting of the manuscript: Brown and Kahn. Critical revision of the manuscript for important intellectual content: Brown, Copeland, Sucharew, and Kahn. Statistical analysis: Brown and Sucharew. Administrative, technical, and material support: Brown and Copeland. Study supervision: Copeland and Kahn.
Financial Disclosure: None reported.
Online-Only Material: Listen to an author interview about this article, and others, at http://bit.ly/L4By6t.
Additional Contributions: We thank Peter Margolis, MD, PhD, for guidance and suggestions and Shelby Brauer, BSN, for assistance with data collection.
Contributor Information
Dr Courtney M. Brown, Division of General and Community Pediatrics, Cincinnati Children’s Hospital Medical Center, Ohio.
Dr Kristen A. Copeland, Division of General and Community Pediatrics, Cincinnati Children’s Hospital Medical Center, Ohio.
Dr Heidi Sucharew, Department of Biostatistics and Epidemiology, Cincinnati Children’s Hospital Medical Center, Ohio.
Dr Robert S. Kahn, Division of General and Community Pediatrics, Cincinnati Children’s Hospital Medical Center, Ohio.
REFERENCES
- 1. [Accessed December 9, 2009];Center on the Social and Emotional Foundations for Early Learning website. http://www.vanderbilt.edu/csefel/index.html.
- 2.Rhoades BL, Warren HK, Domitrovich CE, Greenberg MT. Examining the link between preschool social-emotional competence and first grade academic achievement: the role of attention skills. Early Child Res Q. 2010;26(2):182–191. doi:10.1016/j.ecresq.2010.07.003. [Google Scholar]
- 3.Gilliam WS. [Accessed December 9, 2009];Prekindergarteners left behind: expulsion rates in state prekindergarten systems. Foundation for Child Development website. http://fcd-us.org/resources/prekindergartners-left-behind-expulsion-rates-state-prekindergarten-programs. Published May 1, 2005.
- 4.Essex MJ, Kraemer HC, Armstrong JM, et al. Exploring risk factors for the emergence of children’s mental health problems. Arch Gen Psychiatry. 2006;63(11):1246–1256. doi: 10.1001/archpsyc.63.11.1246. [DOI] [PubMed] [Google Scholar]
- 5.Lavigne JV, Arend R, Rosenbaum D, Binns HJ, Christoffel KK, Gibbons RD. Psychiatric disorders with onset in the preschool years: I, stability of diagnoses. J Am Acad Child Adolesc Psychiatry. 1998;37(12):1246–1254. doi: 10.1097/00004583-199812000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Briggs-Gowan MJ, Carter AS. Social-emotional screening status in early childhood predicts elementary school outcomes. Pediatrics. 2008;121(5):957–962. doi: 10.1542/peds.2007-1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 8.Recommendations for Preventive Pediatric Healthcare [Accessed July 5, 2011];Bright Futures/American Academy of Pediatrics website. http://brightfutures.aap.org/pdfs/AAP%20Bright%20Futures%20Periodicity%20Sched%20101107.pdf.
- 9.Duncan GJ, Brooks-Gunn J, Klebanov PK. Economic deprivation and early childhood development. Child Dev. 1994;65(2 spec no):296–318. [PubMed] [Google Scholar]
- 10.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood) 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 11.Brauner CB, Stephens CB. Estimating the prevalence of early childhood serious emotional/behavioral disorders: challenges and recommendations. Public Health Rep. 2006;121(3):303–310. doi: 10.1177/003335490612100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lavigne JV, Binns HJ, Christoffel KK, et al. Pediatric Practice Research Group Behavioral and emotional problems among preschool children in pediatric primary care: prevalence and pediatricians’ recognition. Pediatrics. 1993;91(3):649–655. [PubMed] [Google Scholar]
- 13.Lavigne JV, Lebailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. J Clin Child Adolesc Psychol. 2009;38(3):315–328. doi: 10.1080/15374410902851382. [DOI] [PubMed] [Google Scholar]
- 14.Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. J Child Psychol Psychiatry. 2006;47(3-4):313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- 15.Lavigne JV, Arend R, Rosenbaum D, et al. Mental health service use among young children receiving pediatric primary care. J Am Acad Child Adolesc Psychiatry. 1998;37(11):1175–1183. doi: 10.1097/00004583-199811000-00017. [DOI] [PubMed] [Google Scholar]
- 16.Lavigne JV, Gibbons RD, Arend R, Rosenbaum D, Binns HJ, Christoffel KK. Rational service planning in pediatric primary care: continuity and change in psychopathology among children enrolled in pediatric practices. J Pediatr Psychol. 1999;24(5):393–403. doi: 10.1093/jpepsy/24.5.393. [DOI] [PubMed] [Google Scholar]
- 17.Palfrey JS, Hauser-Cram P, Bronson MB, Warfield ME, Sirin S, Chan E. The Brookline Early Education Project: a 25-year follow-up study of a family-centered early health and development intervention. Pediatrics. 2005;116(1):144–152. doi: 10.1542/peds.2004-2515. [DOI] [PubMed] [Google Scholar]
- 18.Zoritch B, Roberts I, Oakley A. Day care for pre-school children. Cochrane Database Syst Rev. 2000;(2):CD000564. doi: 10.1002/14651858.CD000564. [DOI] [PubMed] [Google Scholar]
- 19.Baker AJ, Piotrkowski CS, Brooks-Gunn J. The home instruction program for preschool youngsters (HIPPY) Future Child. 1999;9(1):116–133. 192–194. [PubMed] [Google Scholar]
- 20.Fergusson DM, Grant H, Horwood LJ, Ridder EM. Randomized trial of the Early Start program of home visitation. Pediatrics. 2005;116(6):e803–e809. doi: 10.1542/peds.2005-0948. [DOI] [PubMed] [Google Scholar]
- 21.Webster-Stratton C, Jamila Reid M, Stoolmiller M. Preventing conduct problems and improving school readiness: evaluation of the Incredible Years Teacher and Child Training Programs in high-risk schools. J Child Psychol Psychiatry. 2008;49(5):471–488. doi: 10.1111/j.1469-7610.2007.01861.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Upshur C, Wenz-Gross M, Reed G. A pilot study of early childhood mental health consultation for children with behavioral problems in preschool. Early Child Res Q. 2009;24(1):29–45. doi:10.1016/j.ecresq.2008.12.002. [Google Scholar]
- 23.Minde K, Roy J, Bezonsky R, Hashemi A. The effectiveness of CBT in 3-7 year old anxious children: preliminary data. J Can Acad Child Adolesc Psychiatry. 2010;19(2):109–115. [PMC free article] [PubMed] [Google Scholar]
- 24.Lyons-Ruth K, Melnick S. Dose-response effect of mother-infant clinical home visiting on aggressive behavior problems in kindergarten. J Am Acad Child Adolesc Psychiatry. 2004;43(6):699–707. doi: 10.1097/01.chi.0000122730.72597.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landry SH, Smith KE, Swank PR, Guttentag C. A responsive parenting intervention: the optimal timing across early childhood for impacting maternal behaviors and child outcomes. Dev Psychol. 2008;44(5):1335–1353. doi: 10.1037/a0013030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bagner DM, Sheinkopf SJ, Vohr BR, Lester BM. Parenting intervention for externalizing behavior problems in children born premature: an initial examination. J Dev Behav Pediatr. 2010;31(3):209–216. doi: 10.1097/DBP.0b013e3181d5a294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKay K, Shannon A, Vater S, Dworkin PH. ChildServ: lessons learned from the design and implementation of a community based developmental surveillance program. Infants Young Child. 2006;19(4):371–377. doi:10.1097/00001163-200610000-00008. [Google Scholar]
- 28.King TM, Tandon SD, Macias MM, et al. Implementing developmental screening and referrals: lessons learned from a national project. Pediatrics. 2010;125(2):350–360. doi: 10.1542/peds.2009-0388. [DOI] [PubMed] [Google Scholar]
- 29.Pavuluri MN, Luk SL, McGee R. Help-seeking for behavior problems by parents of preschool children: a community study. J Am Acad Child Adolesc Psychiatry. 1996;35(2):215–222. doi: 10.1097/00004583-199602000-00015. [DOI] [PubMed] [Google Scholar]
- 30.Silverstein M, Mack C, Reavis N, Koepsell TD, Gross GS, Grossman DC. Effect of a clinic-based referral system to head start: a randomized controlled trial. JAMA. 2004;292(8):968–971. doi: 10.1001/jama.292.8.968. [DOI] [PubMed] [Google Scholar]
- 31.Rushton J, Bruckman D, Kelleher K. Primary care referral of children with psychosocial problems. Arch Pediatr Adolesc Med. 2002;156(6):592–598. doi: 10.1001/archpedi.156.6.592. [DOI] [PubMed] [Google Scholar]
- 32.Gormley WT, Jr, Phillips DA, Newmark K, Welti K, Adelstein S. Social-emotional effects of early childhood education programs in Tulsa. Child Dev. 2011;82(6):2095–2109. doi: 10.1111/j.1467-8624.2011.01648.x. [DOI] [PubMed] [Google Scholar]
- 33.American Academy of Pediatrics Committee on Early Childhood, Adoption, and Dependent Care Quality early education and child care from birth to kindergarten. Pediatrics. 2005;115(1):187–191. doi: 10.1542/peds.2004-2213. [DOI] [PubMed] [Google Scholar]
- 34.Pluess M, Belsky J. Differential susceptibility to parenting and quality child care. Dev Psychol. 2010;46(2):379–390. doi: 10.1037/a0015203. [DOI] [PubMed] [Google Scholar]
- 35. [Accessed October 2, 2009];Technical report on ASQ:SE. Brookes Publishing Co website. http://www.agesandstages.com.
- 36.Squires J, Bricker D, Heo K, Twombly E. Identification of social-emotional problems in young children using a parent-complete screening measure. Early Child Res Q. 2001;16(4):405–419. doi:10.1016/S0885-2006(01)00115-6. [Google Scholar]
- 37.Blumberg SJ, Halfon N, Olson LM. The National Survey of Early Childhood Health. Pediatrics. 2004;113((6)(suppl)):1899–1906. [PubMed] [Google Scholar]
- 38. [Accessed December 9, 2009];Early Childhood Longitudinal Study (ECLS). Birth Cohort (ECLS-B): instruments and assessments. Institute of Education Sciences website. http://nces.ed.gov/ecls/birthinstruments.asp.
- 39.The Commonwealth Fund Survey of Parents with Young Children [Accessed December 2, 2009];The Commonwealth Fund website. http://www.commonwealthfund.org/Content/Surveys/1995/The-Commonwealth-Fund-Survey-of-Parents-with-Young-Children.aspx.
- 40.Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29(2):169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 41.McCabe CJ, Thomas KJ, Brazier JE, Coleman P. Measuring the mental health status of a population: a comparison of the GHQ-12 and the SF-36 (MHI-5) Br J Psychiatry. 1996;169(4):516–521. doi: 10.1192/bjp.169.4.516. [DOI] [PubMed] [Google Scholar]
- 42.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.SAS [computer program]. Version 9.2. SAS Institute Inc; Cary, NC: 2008. [Google Scholar]
- 44.Jee SH, Conn AM, Szilagyi PG, Blumkin A, Baldwin CD, Szilagyi MA. Identification of social-emotional problems among young children in foster care. J Child Psychol Psychiatry. 2010;51(12):1351–1358. doi: 10.1111/j.1469-7610.2010.02315.x. [DOI] [PubMed] [Google Scholar]
- 45.Jhanjee I, Saxeena D, Arora J, Gjerdingen DK. Parents’ health and demographic characteristics predict noncompliance with well-child visits. J Am Board Fam Pract. 2004;17(5):324–331. doi: 10.3122/jabfm.17.5.324. [DOI] [PubMed] [Google Scholar]
- 46.Gordon M, Antshel KM, Lewandowski L, Seigers D. Economic grand rounds: predictors of missed appointments over the course of child mental health treatment. Psychiatr Serv. 2010;61(7):657–659. doi: 10.1176/ps.2010.61.7.657. [DOI] [PubMed] [Google Scholar]
- 47.Whitaker RC, Orzol SM, Kahn RS. Maternal mental health, substance use, and domestic violence in the year after delivery and subsequent behavior problems in children at age 3 years. Arch Gen Psychiatry. 2006;63(5):551–560. doi: 10.1001/archpsyc.63.5.551. [DOI] [PubMed] [Google Scholar]
- 48.Weissman MM, Pilowsky DJ, Wickramaratne PJ, et al. STAR*D-Child Team. Remissions in maternal depression and child psychopathology: a STAR*D-child report. JAMA. 2006;295(12):1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- 49.Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE Project. Pediatrics. 2007;120(3):547–558. doi: 10.1542/peds.2007-0398. [DOI] [PubMed] [Google Scholar]
- 50.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14(1):32–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 51.Silverstein M, Grossman DC, Koepsell TD, Rivara FP. Pediatricians’ reported practices regarding early education and Head Start referral. Pediatrics. 2003;111(6, pt 1):1351–1357. doi: 10.1542/peds.111.6.1351. [DOI] [PubMed] [Google Scholar]