Abstract
Dynamic neuromuscular (core) stability is necessary for optimal athletic performance and is not achieved purely by adequate strength of abdominals, spinal extensors, gluteals or any other musculature; rather, core stabilization is accomplished through precise coordination of these muscles and intra‐abdominal pressure regulation by the central nervous system. Understanding developmental kinesiology provides a framework to appreciate the regional interdependence and the inter‐linking of the skeleton, joints, musculature during movement and the importance of training both the dynamic and stabilizing function of muscles in the kinetic chain. The Dynamic Neuromuscular Stabilization (DNS) approach provides functional tools to assess and activate the intrinsic spinal stabilizers in order to optimize the movement system for both pre‐habilitation and rehabilitation of athletic injuries and performance.
Level of Evidence:
5
Keywords: Core stabilization, developmental kinesiology, dynamic neuromuscular stabilization, integrated spinal stabilizing system
Introduction
Dynamic Neuromuscular Stabilization, or “DNS” as it is commonly referred to, is a manual and rehabilitative approach to optimize the movement system based upon the scientific principles of developmental kinesiology (DK). The developer of DNS is Professor Pavel Kolar, PT, PhD, a Czech physiotherapist who has been influenced by the “greats” of Prague School of Manual Medicine, including Karel Lewit, Vladimir Janda, Vaclav Vojta and Frantisek Vele. DNS is rapidly gaining attention and acceptance in the sports rehabilitation and performance arena for both the recovery from musculoskeletal overuse injuries and in injury prevention. The purpose of this clinical commentary is to discuss the background of Dynamic Neuromuscular Stabilization (DNS) and demonstrate its application in rehabilitation, recovery from overuse injuries, and role in return to athletic performance.
Developmental Influences
The basis for the theories that are included in DK is that development of human motor function in early childhood is genetically pre‐determined and follows a predictable pattern. These motor patterns or programs are formed as the central nervous system (CNS) matures, enabling the infant to control posture, achieve erect posture against gravity, and to move purposefully via muscular activity. DK emphasizes the existence of central movement patterns that are inborn and “hard‐wired”. For example, an infant does not need to be taught when and how to lift its head up, grasp a toy, roll over, creep, or crawl. All these movement patterns or muscular synergies occur automatically in a specific developmental sequence throughout the course of CNS maturation.
There is also a strong synchrony between CNS maturation and structural or anatomical development of bones, muscles, and other soft tissues. In short, maturation of the brain influences development of motor patterns, which in turn, influences structural development. This relationship is very apparent in the presence of a CNS lesion, where this developmental synchrony and muscle coordination are adversely affected. The disturbed muscle coordination, soft tissue, and joint development subsequently alters joint position, morphological development, and ultimately, the entire posture.
The role of intra‐abdominal pressure regulation (IAP) & integrated spinal stabilizing system (ISSS) in functional spinal stability
Stability (or stiffness) of the spine is dependent on the dynamic coordination of numerous synergist and antagonist muscles for precise control of excessive joint motion while allowing for the generation of necessary torques for desired multi‐joint movement. One parameter for influencing spinal mechanics and stiffness is intra‐abdominal pressure (IAP). There is a general consensus that an increase in IAP stabilizes the spine;1,2,3,4,5,6,7 however, the role of IAP in unloading the spine remains controversial. An increase in IAP has been reported to unload the spine during static and dynamic lifting tasks.8,9,10 Conversely, experimental studies demonstrate that an increase in IAP concurrently increases intradiscal pressure during Valsalva maneuvers11,12 and that there was no reduction in paraspinal activity during lifting.13 A kinematic study by Arjman & Shirazi‐Adl14 demonstrated that the unloading effect of IAP is more effective in forward lifting tasks whereas the ability of IAP to unload the spine in upright standing posture holds true only for conditions with very low abdominal co‐activation. This study suggests that the unloading and stabilizing actions of IAP seem to be posture and task specific.
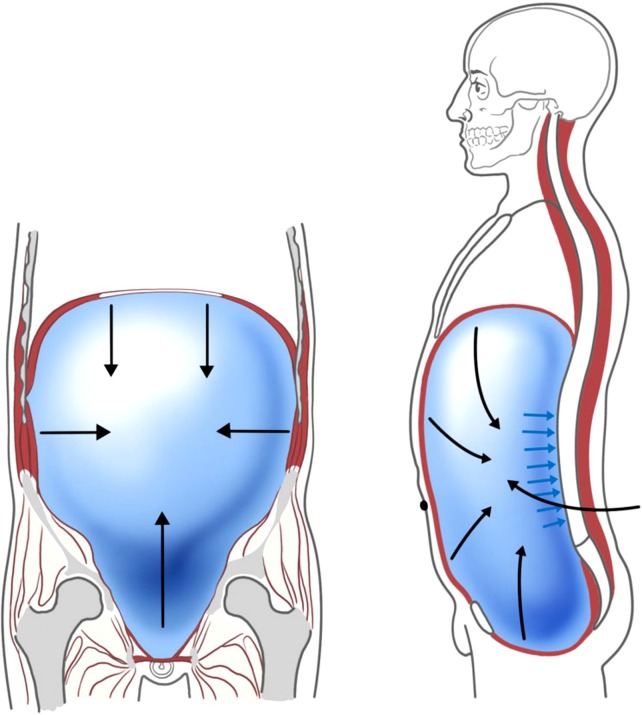
The integrated spinal stabilizing system (ISSS) as described by Kolar,15 is comprised of balanced co‐activation between the deep cervical flexors and spinal extensors in the cervical and upper thoracic region, as well as the diaphragm, pelvic floor, all sections of the abdominals and spinal extensors in the lower thoracic and lumbar region. The diaphragm, pelvic floor and transversus abdominis regulate IAP and provide anterior lumbopelvic postural stability.13,4,6,7,16,17,18,19,20,21 (Fig. 1) These intrinsic spinal stabilizing muscles provide spinal stiffness in coordination with IAP, which serves to provide dynamic stability of the spine. They constitute the “deep core” and operate under the automatic and subconscious “feed‐forward control mechanism,” and precedes any purposeful movement.
Figure 1.
IAP Regulation by diaphragm, pelvic floor and transversus abdominis.
The role of anticipatory trunk muscle activity in adults has been widely studied and discussed in an attempt to describe the determinants of spinal stability for movement and musculoskeletal function. In addition, children with developmental coordination disorders22,23 also demonstrate impairments with the anticipatory trunk postural adjustments under the feed‐forward mechanism of control which suggests that training the timing of both proximal and distal muscles should be considered when designing intervention programs. In brief, alterations in anticipatory and reactive neuromuscular activation in both trunk and the extremities may interfere with the initiation and execution of coordinated movement. The DNS approach emphasizes the importance of precise muscular timing and coordination for efficient movement as well as withstand compressive loading, which occurs in static or sustained postures.
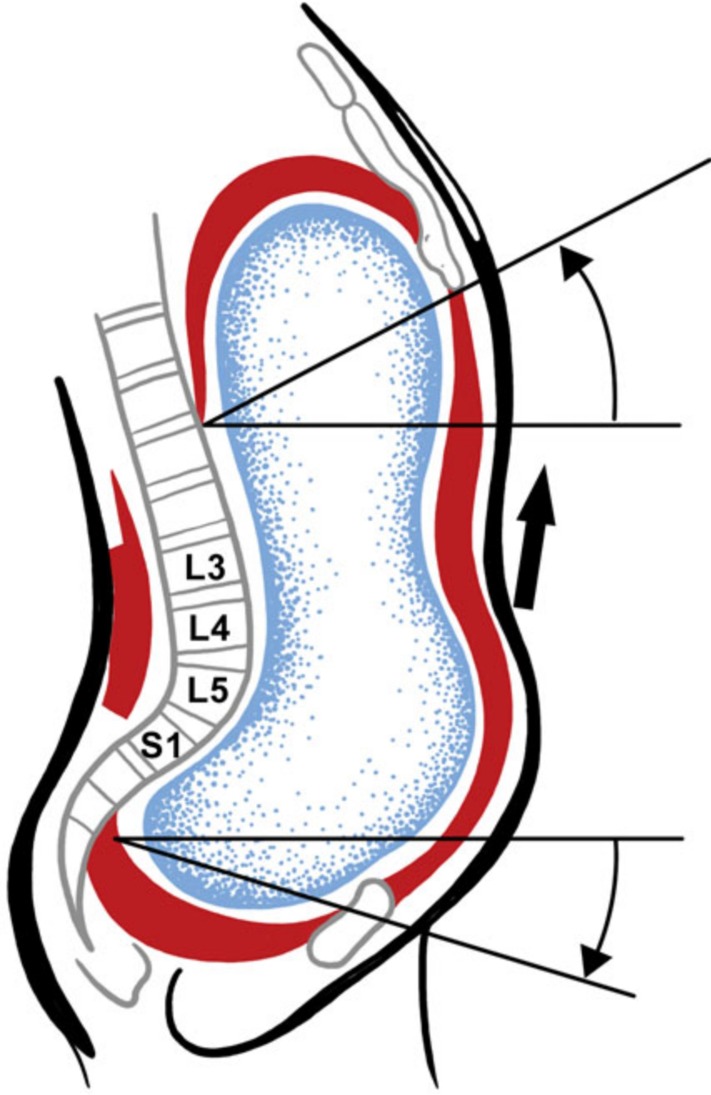
During early postural development, the diaphragm functions primarily as a respiratory muscle. With continued CNS maturation and development to about 4½ months of age, sagittal stabilization of the spine, pelvis, and chest is fully established for subsequent movements that occur in the transverse plane, (e.g rolling, turning, creeping, crawling) and eventually the transition to upright posture. The diaphragm begins to fulfill its dual function as both a respiratory and postural muscle when abdominal breathing is coordinated with chest breathing at about 6 months of age. The dual role of the diaphragm is essential for spinal stability and all resultant movements, especially for the complex tasks that comprise athletic performance.6,19 The stabilizing postural activation of the diaphragm has been studied in lifting tasks10 and activation of the extremities.6,8,17,19,25,26 A recent study by Kolar et al26 demonstrated that abnormal postural activa‐tion of the diaphragm when isometric resistance was applied to the extremities might serve as an underlying mechanism of chronic low back pain due to a great‐er strain on the ventral region of the spinal column. (Fig. 2) According to Kolar,26 IAP regulation & ISSS can be disrupted by insufficient postural function of the diaphragm, often resulting in increased compressive forces on the spine due to compensatory activity of the superficial spinal extensors, and abnormal position of the chest or ribcage due to an imbalance between upper and lower chest musculature.24,25,26
Figure 2.
Impaired ISSS resulting in anterior shear stresses on lumbar segments.
The ISSS provides the “punctum fixum” (fixed stable base) from which muscles can generate movement. For example, psoas major functions as a hip flexor with minimal mechanical impact on the spine when the ISSS is functioning sufficiently;15 however, in the event of inadequate ISSS, the pull of the psoas major may result in anterior shear stresses on the lumbar segments. This neuromuscular strategy is not static but is dynamic in nature in order to provide a functionally “neutral or centered” joint which is described by Kolar as joint centration.26 Joint centration or neutral joint position occurs when joint surface congruency and muscles that support the joint are at their optimal mechanical advantage throughout the range of motion and thus are able to produce varying forces according to the required skill. The centrated joint allows for optimal load transference of muscular forces across the joint and along the kinetic chain, with minimal mechanical stress on the passive structures such as ligaments, capsule, cartilage, and joint surfaces. Inadequate proportional activation of the stabilizing muscles may place internal stresses within the body, and can compromise posture and resultant movement of the extremities, highlighting the effect of regional interdependence. A deficient ISSS may result in greater activity of its associated muscles, likely leading to strain or overuse due to compensatory movements.
Influence of the kinetic chain and regional interdependence
It is critical that all stabilizers are proportionally activated in order to ensure good movement patterns for functional activities or skill execution. If one link (muscle or a portion of a muscle) is insufficient and/or weak, another muscle(s) in the kinetic chain may be recruited to make up for the loss of stability or movement. If the muscle imbalance is not addressed through careful analysis and rehabilitation, this may lead to persistent and fixed suboptimal motor programs in the CNS, chronic pain and/or poor performance.21,27,28,29 Hence, corrective stabilization strategies should always be the foundational tenet of any training program.
Panjabi30,31 described the stabilizing system of the spine as a 3‐way interaction between the neural (CNS), active (musculature) and passive (bones, joints) systems. Many clinicians who have primarily focused treatment on muscles and joints are increasingly recognizing the importance of “training the brain” by addressing motor control mechanisms at the CNS level. DK and DNS “bridge the gap” to understanding this 3‐way interaction. It is the opinion of the authors that the majority of the dysfunctions commonly seen may be more related to CNS or “motor control dysfunction” than local joint or muscle dysfunction. Given that CNS is the ultimate “driver”, attention must be paid to muscular co‐activation patterns that occur with movement in order to provide joint stability. For example, if a person has difficulty performing a squat, rather than focusing on the local “tight” or “weak” muscles, one may need to recognize that this inadequacy may be a dysfunctional ISSS pattern at the brain level. In another example, when rehabilitating a rotator cuff impingement of a baseball pitcher, one should not just focus on merely stretching or mobilizing a tight glenohumeral capsule/joint and strengthening the rotator cuff muscles, but one may need to ask the question of “why” the rotator cuff is being impinged. Analysis of the movement pattern (e.g arm elevation or the throwing mechanics) must be performed, in order to determine whether the ISSS is adequate and/or if a “weak link” in the kinetic chain is present. Such weak links may include poor scapular dynamic stability, impaired lower extremity mobility, stability and/or proprioception, and poor trunk mobility or stability.32,33
The body functions as a single unit rather than in segments during any complex movement such as those encountered in sports training and athletic performance. These complex movements require both local and global synergistic coordination of various muscle groups necessary for multi‐joint coordination of movement. In the event where stability, mobility and/or balance of these muscle groups become compromised, the ability to transfer force efficiently through the trunk to the extremities is often adversely affected. Hence, core stabilization has become the key tenet of any training and conditioning program.
The DNS approach
A key premise of the DNS approach is that every joint position depends on stabilizing muscle function and coordination of both the local and distant muscles in order to ensure neutral or centered position of joints in the kinetic chain. The quality of this coordination is critical for joint function and influences not only local, but also regional and global anatomical and biomechanical parameters in the kinetic chain. Although there are limited objective measurements of neuromuscular impairments, the DNS approach is based on comparing the athlete's stabilizing pattern with the stabilization developmental pattern of a healthy baby with the intent of directing treatment to restore the impaired stabilizing pattern to as close as possible those ideal patterns as defined by DK. The DNS approach seeks to activate the ISSS and restore ideal IAP regulation in order to optimize efficiency of movement and to prevent overloading of joints.
DNS presents a set of functional tests to assess the ISSS and to assist in finding the “key link” of the dysfunction, such as diaphragm activation, supine arm elevation, head flexion, and prone head extension, to name a few. The seated diaphragm test is shown in Figure 3 and is described below. During the inspiratory phase of tidal breathing, the descent of the diaphragm increases the IAP, given that that the abdominal wall and pelvic floor maintain their respective tension. Observable movements of the chest would be expansion in the chest and abdominal regions in an anterior‐posterior direction, lateral lower ribcage expansion and minimal superior movements of the chest. During expiratory phase of tidal breathing, one should observe the ribcage returning to its resting state.
Figure 3.

Seated diaphragm test. Clinician palpates for adequate lateral excursion of rib cage and lateral abdominal activation; and excessive superior excursion of rib cage and overactivity of paraspinals.
The clinician's places his 2nd and 3rd fingers lightly on the athlete's lower ribs to detect movement of the rib cage during respiration, while the thumbs on the thoracolumbar paraspinal muscles monitor the intensity of their contraction. The 4th and 5th fingers are placed lightly on lateral abdominal wall to monitor the resistance (eccentric contraction) of the abdominal wall against IAP changes during respiration. As the athlete breathes in and out, the clinician observes the global posture in addition to monitoring movements at the ribcage and abdominal wall. Although objective measures are Iimited; some common observable and palpable faulty movement patterns include: 1. Cranial excursion of the rib cage or shoulder elevation secondary to compensation of accessory muscles of respiration to make up for inadequate diaphragm activity, 2. Excessive contraction of paraspinal muscles, 3. Inadequate lateral rib cage expansion or resistance of the abdominal wall against IAP changes, and 4. The inability to maintain the upright spinal alignment (either into flexion or extension). These faulty patterns are often magnified if the athlete is cued to lightly brace his or her abdominals. These faulty patterns may be bilateral or unilateral; if unilateral, the impairments are often on the side of dysfunction.
For example, these faulty patterns are sometimes seen in an athlete with a positive right shoulder impingement test and a painful arc during shoulder elevation. When the diaphragm test is administered, the athlete presents with insufficient right lateral rib cage excursion, excessive right shoulder girdle elevation, or insufficient right lateral abdominal wall activation while performing this test. The clinician could then test her hypothesis of insufficient ISSS contributing to the right shoulder impingement symptoms. The clinician would cue the athlete to increase abdominal activation on the right and the clinician could re‐test the athlete for painful arc during reaching or positive impingement tests. If the athlete's shoulder impingement signs are improved or eliminated, this could direct the clinician to focus treatment on improving the ISSS rather than merely focusing on the shoulder joint.
DNS Treatment Approach
The DNS treatment approach is based on careful assessment of the quality of stabilization and/or movement with the goal of restoring the ISSS via specific functional exercises based on developmental kinesiological positions exhibited by a healthy baby. These exercises should activate the optimal patterns necessary for stabilization (support) in the closed kinetic chain, as well as the dynamic movements in the open kinetic chain, which occur during reaching, throwing, stepping forward, or kicking.
Essentially, “every developmental position is an exercise position”15 however, each exercise must follow some basic principles: 1. Restore proper respiratory pattern and IAP regulation; 2. Establish a good quality of support for any dynamic movement of the extremities; and 3. Ensure that all joints are well centered throughout the movement. Resistance or load should be matched to the athlete's ability to maintain proper form during the exercise or drills.
The ultimate strategy is to “train the brain” to maintain central control, joint stability and ideal quality of movement that is achieved through guidance from the clinician. Eventually, through repetition of the exercises, the central control establishes an automatic model that becomes a fundamental part of everyday movement and skills. Integration of an ideal pattern of stabilization in sport activities would not only reduce the risk of injuries and secondary pain syndromes resulting from overloading, but may also improve sport performance. See Figures 4‐10 for examples of exercises corresponding to developmental positions.
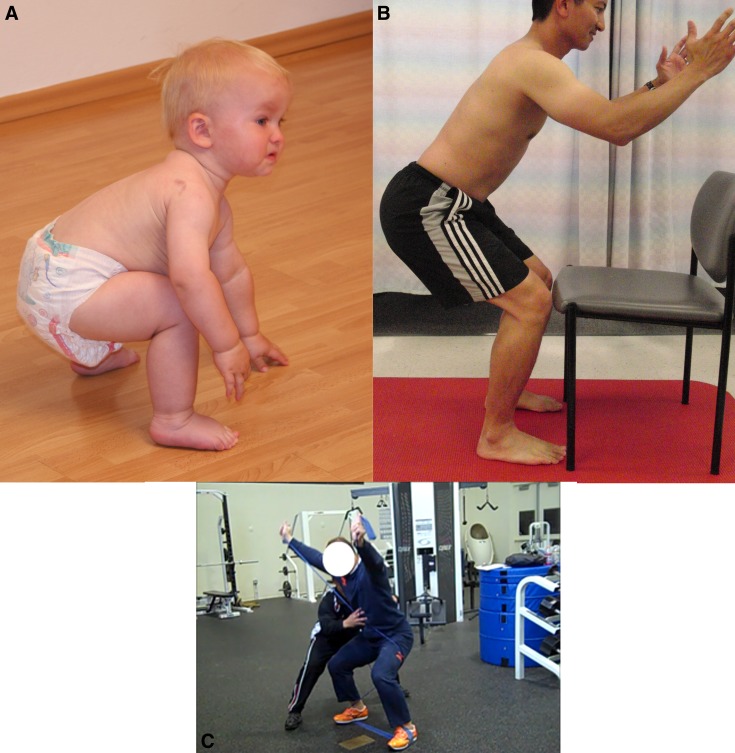
Figure 4.
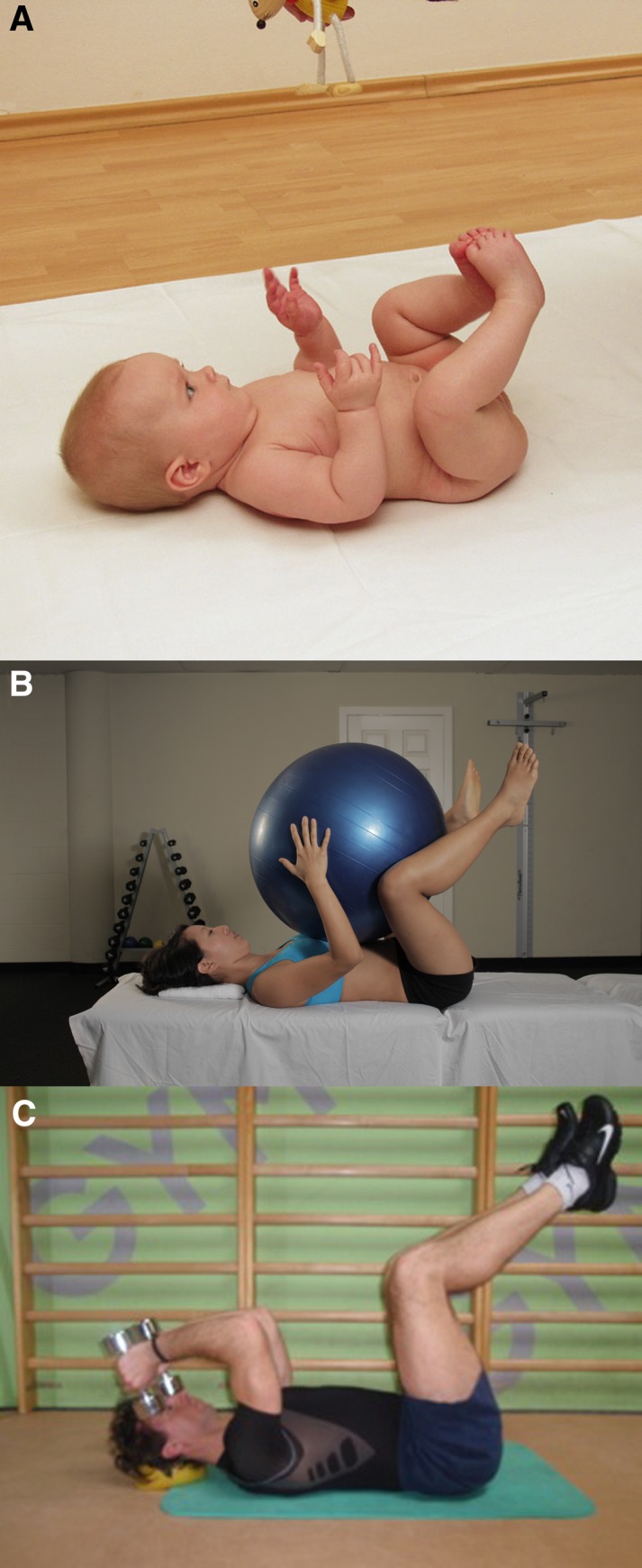
(A) Establishment of ideal ISSS and IAP regulation in a 4½ month old baby. (B) Training of ISSS & IAP regulation with hips and knees in 90° flexion. Rolling from side to side can be incorporated with or without the ball to facilitate oblique muscle chain activation, while maintaining proper form. (C) Maintaining good respiration and IAP regulation with increased load
Figure 10.
(A) Deep Squat position corresponding to 16 months of age. (B) Training for good squat pattern to avoid “quad dominant” pattern where the knees move anterior of the feet. (C) Squat & reach with Thera-Band resistance. Focus is on good IAP regulation and ideal coordination of ISSS.
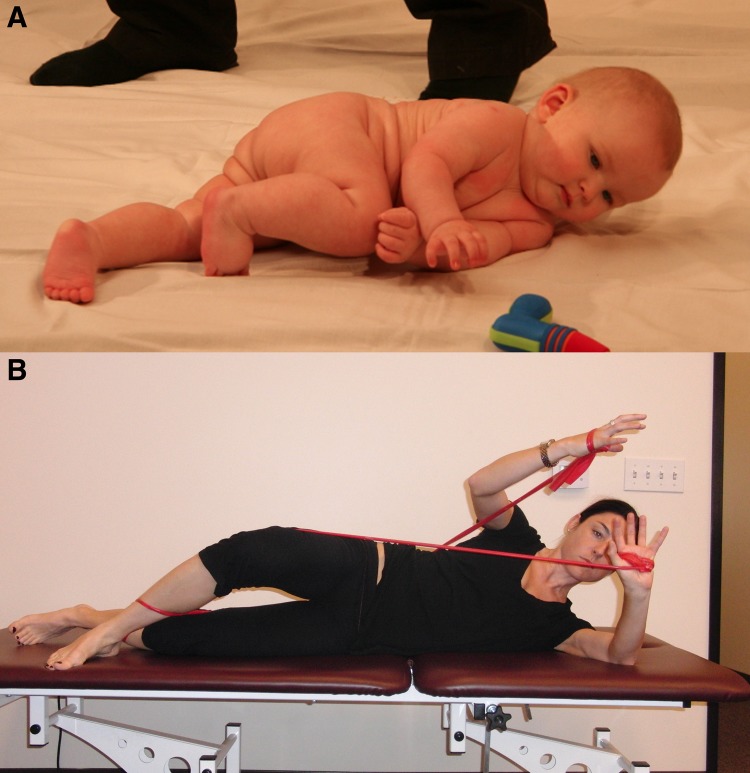
Figure 5.
(A) Rolling pattern of a 5-6 month old baby. (B) Exercise with elastic band corresponding to rolling pattern of a 5-6 month old baby.
Figure 6.
(A) Oblique sit position corresponding to 7½ months of age. (B) Rotator cuff strengthening of right shoulder while training the stabilizing function of the left shoulder in a modified oblique sit/side plank position, while maintaining good IAP regulation.
Figure 7.
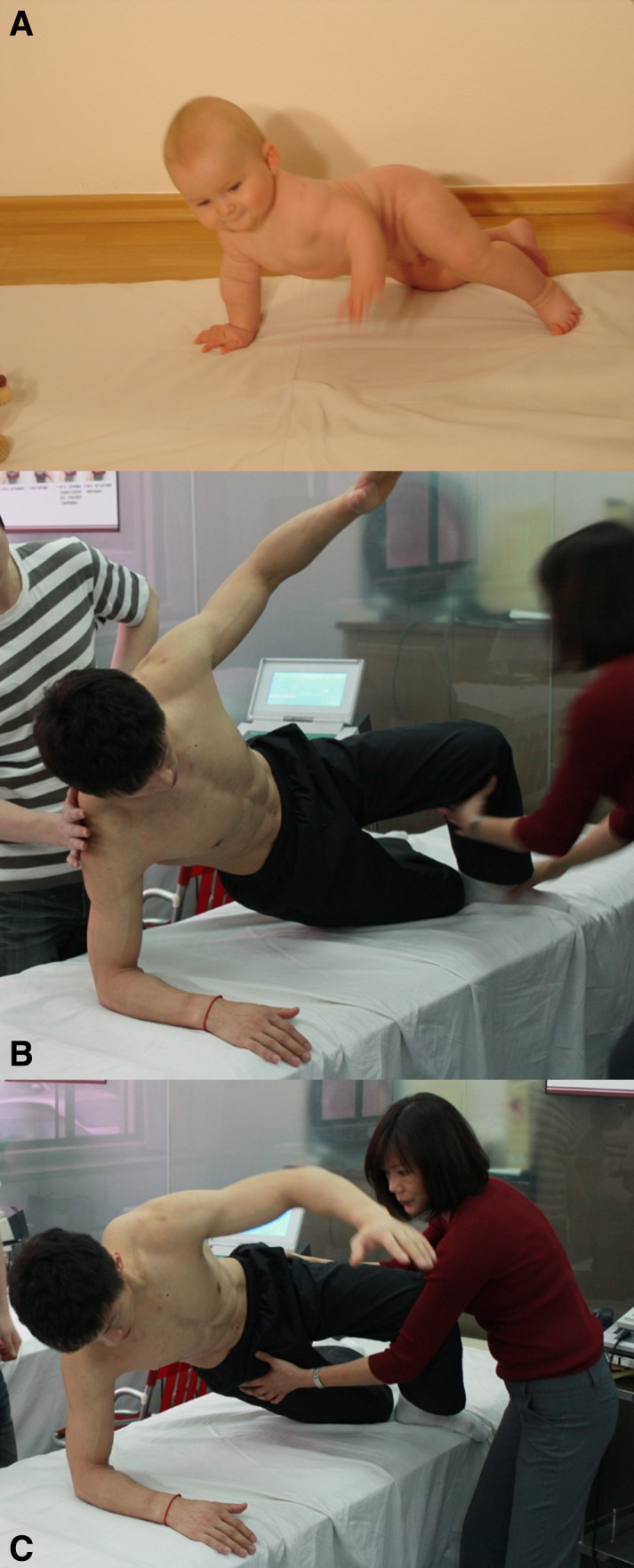
(A) Oblique sit position transitioning towards a quadruped position. (B) Training an athlete in an oblique sit position focusing on stabilizing function of right shoulder and dynamic function of the top reaching arm. (C) Training an athlete transitioning from oblique sit position to a quadruped position. Emphasis is on stabilizing function of the right shoulder where the glenoid fossa is rotating over a fixed/stable humerus and dynamic function of the left reaching arm where the humerus is rotating over a fixed/stable glenoid fossa.
Figure 8.
(A) Sitting posture of a 8-9 month old baby with well balanced ISSS and IAP regulation. (B) Training proper respiration and IAP regulation in seated position with tactile feedback. (C) Utilizing proper respiration and IAP regulation when exercising with load in the gym.
Figure 9.
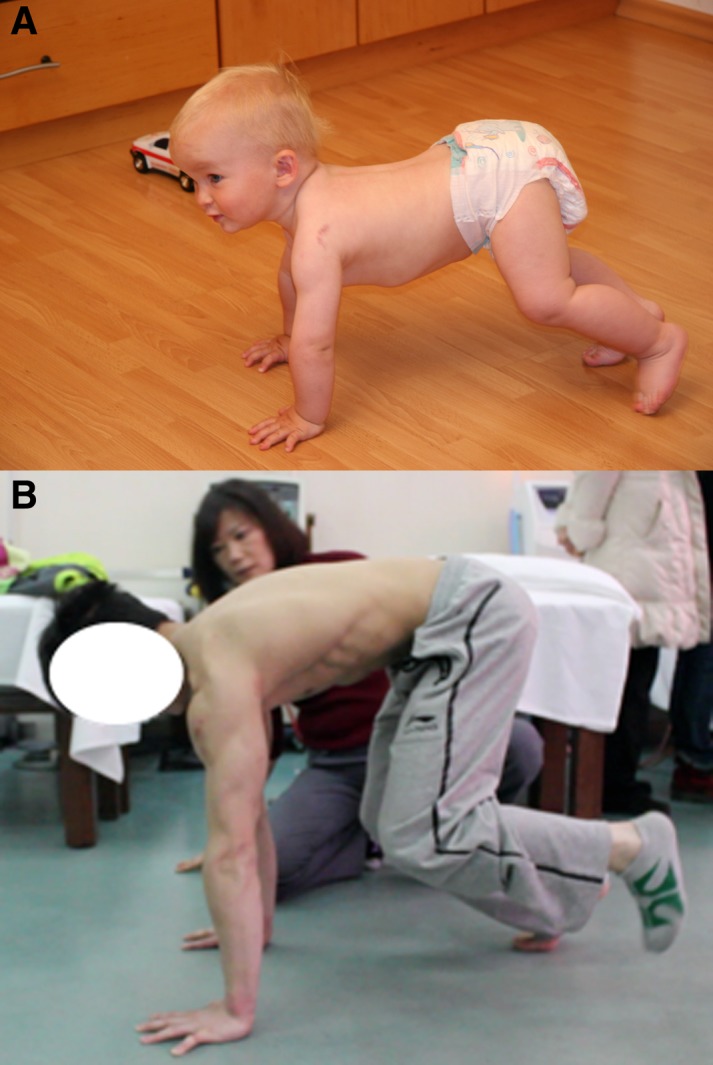
(A) Bear position corresponding to 14 months of age. (B) Training of an athlete in a bear position from 4 to 3 points of support when he lifts his left foot off the ground. This exercise can be progressed to 2 point support where contralateral extremities lift off the ground to crawl forward.
CONCLUSION
Dynamic core stability for optimal athletic performance is not achieved purely by adequate strength of abdominals, back extensors, gluteals or any others muscles in isolation, but is accomplished through precise coordination of the ISSS and IAP regulation. Rehabilitation of athletic injuries and performance training should not only focus on training muscles in their dynamic anatomical function but also should address their stabilizing function. The DNS approach serves as an important method for both assessment and training of muscles in all facets of their physiological function (purposeful movement and stabilization functions) by using positions determined by developmental kinesiology.
REFERENCES
- 1.Cholewicki J, Juluru K, McGill SM. Intra-abdominal pressure mechanism for stabilizing the lumbar spine. J. Biomech. 1999a;32(1):13–17 [DOI] [PubMed] [Google Scholar]
- 2.Cholewicki J, Juluru K, Radebold A, Panjabi MM, McGill SM. Lumbar spine stability can be augmented with an abdominal belt and/or increased intra-abdominal pressure. Eur Spine J. 1999;8(5):388–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cresswell AG, Grundström H, Thorstensson A. Observations on intra-abdominal pressure and patterns of abdominal intra-muscular activity in man. Acta Physiol. Scand. 1992;144(4):409–18 [DOI] [PubMed] [Google Scholar]
- 4.Gardner‐Morse MG, Stokes IAF. The effects of abdominal muscle co-activation on lumbar spinestability. Spine. 1998;23(1):86–92 [DOI] [PubMed] [Google Scholar]
- 5.Hodges PW, Eriksson AE, Shirley D, et al. Intra-abdominal pressure increases stiffness of the lumbar spine. J Biomech. 2005;38(9):1873–80 [DOI] [PubMed] [Google Scholar]
- 6.Hodges PW, Gandevia SC. Changes in intra-abdominal pressure during postural and respiratory activation of the human diaphragm. J Appl Physiol 2000;89(3):967–976 [DOI] [PubMed] [Google Scholar]
- 7.Shirley D, Hodges PW, Eriksson Ae, Gandevia SC. Spinal stiffness changes throughout the respiratory cycle. J Appl Physiol. 2003;95:1467–1475 [DOI] [PubMed] [Google Scholar]
- 8.Hodges PW, Gandevia SC. Activation of the human diaphragm during a repetitive postural task. J Appl Physiol. 2000;522:165–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daggfeldt K, Thorstensson A. The mechanics of back-extensor torque production about the lumbar spine. J Biomech 2003;36:815–825 [DOI] [PubMed] [Google Scholar]
- 10.Hagins M, Lamberg EM. Individuals with low back pain breathe differently than healthy in-dividuals during a lifting task. J Orthop Sports Phys Ther. 2011;41:141–148 [DOI] [PubMed] [Google Scholar]
- 11.Bartelink DL. The role of abdominal pressure in relieving the pressure on the lumbar intervertebral discs. J Bone Joint Surg Br. 1957;9:718–725 [DOI] [PubMed] [Google Scholar]
- 12.Nachemson AL, Andersson GBJ, Schultz AB. Valsalva maneuver biomechanics Effects on lumbar trunk loads of elevated intraabdominal pressures. Spine. 1986;11:476–479 [PubMed] [Google Scholar]
- 13.McGill SM, Norman RW, Sharratt MT. The effect of an abdominal belt on trunk muscle activity and intraabdominal pressure during squat lifts. Ergonomics. 1990;33:147–60 [DOI] [PubMed] [Google Scholar]
- 14.Arjmand N, Shirazi Adl A. Role of intra-abdominal pressure in the unloading and stabilization of the human spine during static lifting tasks. Eur Spine J 2006;15:1265–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kolar P: Facilitation of Agonist-Antagonist Co-activation by Reflex Stimulation Methods In: Craig Liebenson: Rehabilitation of the Spine – A Practitioner's Manual. Lippincott Williams & Wilkins; 2nd edition 2006531–565 [Google Scholar]
- 16.Hodges PW, Cresswell AG, Daggfeldt K, Thorstensson A. In vivo measurement of the effect of intraabdominal pressure on the human spine. J Biomech. 2001;34:347–353 [DOI] [PubMed] [Google Scholar]
- 17.Hodges P, Kaigle‐Holm A, Holm S, Ekström L, Cresswell A, Hansson T, Thorstensson A. Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies. Spine. 2003;28(23):2594–601 [DOI] [PubMed] [Google Scholar]
- 18.Kavcic N, Grenier S, McGill SM. Determining the stabilizing role of individual torso muscles during rehabilitation exercises. Spine. 2004; 29(11):1254–65 [DOI] [PubMed] [Google Scholar]
- 19.Hodges PW, Heijnen I, Gandevia SC. Postural activity of the diaphragm is reduced in humans when respiratory demand increases. J Physiol. 2001;537(Pt 3): 999–1008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gandevia SC, Butler JE, Hodges PW, et al. Balancing acts: respiratory sensations, motor control and human posture. Clin Exp Pharmacol Physiol. 2002;29(1‐2):118–21 [DOI] [PubMed] [Google Scholar]
- 21.McGill SM, Grenier S, Kavcic N, Cholewicki J. Coordination of muscle activity to assure stability of the lumbar spine. J Electromyogr Kinesiol. 2003;13(4):353–359 [DOI] [PubMed] [Google Scholar]
- 22.Kane K, Barden J. Contributions of trunk muscles to anticipatory postural control in children with and without developmental coordination disorder. Hum Mov Sci. 2012;31(3):707–720 [DOI] [PubMed] [Google Scholar]
- 23.Johnston LM, Burns YR, Brauer SG, Richardson CA. Differences in postural control and movement performance during goal directed reaching in children with developmental coordination disorder. Human Movement Science. 2002;21:583–601 [DOI] [PubMed] [Google Scholar]
- 24.Kolar P, Sulc J, Kyncl M, et al. Stabilizing function of the diaphragm: dynamic MRI and synchronized spirometric assessment. J Appl Physiol. 2010;109:1064–1071 [DOI] [PubMed] [Google Scholar]
- 25.Kolar P, Neuwirth J, Sanda J, Suchanek V, Svata Z, Vojejnik J, Pivec M. Analysis of diaphragm movement, during tidal breathing and during its activation while breath holding, using MRI synchronized with spirometry. Physiol Res. 2009;58: 383–92 [DOI] [PubMed] [Google Scholar]
- 26.Kolar P, Sulc J, Kyncl M, Sanda J, Cakrt O, Andel R, Kumagai K, Kobesova A. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012;42(4):352–62 [DOI] [PubMed] [Google Scholar]
- 27.Janda V. Muscles, central nervous regulation and back problems. In: Korr IM. (ed). Neurobiological mechanisms in manipulative therapy. Plenum Press, New York, 1978, pp 27–41 [Google Scholar]
- 28.Janda V. Muscles and motor control in cervicogenic disorders. In: Grant R (ed). Physical therapy of the cervical and thoracic spine. 1st edition Churchill Livingstone, Edinburgh; 1994, pp 195–215 [Google Scholar]
- 29.Page P, Frank C, Lardner R: Asessement & Treatment of Muscle Imbalances. The Janda Approach. Human Kinetics. 2010. [Google Scholar]
- 30.Panjabi MM. The stabilizing function of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5(4):383–9; discussion 397 [DOI] [PubMed] [Google Scholar]
- 31.Panjabi MM. The stabilizing function of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 1992;5(4):390–6; discussion 397 [DOI] [PubMed] [Google Scholar]
- 32.Kibler WB. Biomechanical Analysis of the shoulder during tennis. Clinics in Sports Medicine 1995;14(1):79–85 [PubMed] [Google Scholar]
- 33.Kibler WB. The role of the scapular in athletic shoulder function. Am J Sports Med. 1998;26(2):325–336 [DOI] [PubMed] [Google Scholar]