Abstract
Radiological and nuclear devices may be used by terrorists or may be the source of accidental exposure. A tiered approach has been recommended for response to a terrorist event wherein local, regional, state and federal assets become involved sequentially, as the magnitude in severity of the incident increases. State-wide hospital plans have been developed and published for Connecticut, New York and California. These plans address delineation of responsibilities of various categories of health professionals, protection of healthcare providers, identification and classification of individuals who might have been exposed to and/or contaminated by radiation and, in the case of Connecticut response plan, early management of victims. Regional response programs such as the New England Regional Health Compact (consisting of 6 member states) have been developed to manage consequences of radiation injury. The Department of Homeland Security is ultimately responsible for managing both health consequences and the crisis. Multiple US national response assets may be called upon for use in radiological incidents. These include agencies and programs that have been developed by the Department of Energy, the Environmental Protection Agency and the Department of Defense. Coordination of national, regional and state assets with local response efforts is necessary to provide a timely and efficient response.
INTRODUCTION
Exposure to moderate or high-dose ionizing radiation may occur following an accident or an intentional act. Registries of radiation accidents indicate that exposure to radiation predominately involves sealed sources, x-ray devices, accelerators and diagnostic and therapeutic radioisotopes (Ricks 2002; Dainiak and Ricks 2005). Terrorist acts may involve the use of a sealed source, radiological dispersal device (i.e., dirty bomb) or improvised nuclear device, or may involve an attack on a nuclear power plant, transportation vehicle, nuclear stockpile or waste storage site (NCRP 2001; Waselenko et al. 2004).
Intentional exposure to radiation is increasingly recognized as a distinct possibility, as the threat from terrorist activities has been realized following the September 11, 2001 terrorist act in New York City. Radiation is a potentially good option for terrorists, as the general public, news media, early responders and healthcare providers often have misunderstandings and/or an exaggerated fear of radiation. Radiation detection and measurement require special expertise. Since the terrorist’s primary objective is to create fear and panic in a large number of people in order to focus attention on a cause and/or satisfy a demand, radiation is particularly attractive. Confusion between estimates of dose vs. dose rate, lack of knowledge of radiation units of measurement, and misunderstanding of dose-related biological effects, contribute to achieving this objective.
The major goals of a response to a radiological emergency are to protect the public and to protect emergency personnel during the response (IAEA 2006). To achieve these goals, local, regional and national assets may be brought together to address an incident of national significance. Here, the concept of a layered response strategy is reviewed as a function of the magnitude of a radiological event. Also discussed are the roles of resources controlled by the Department of Energy (DOE), Environmental Protection Agency (EPA) and Department of Defense (DOD) as a function of time after an incident has occurred.
LOCAL AND STATE RESPONSE
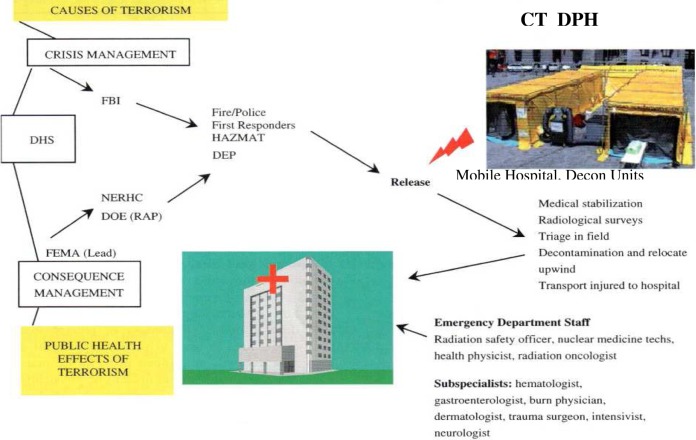
The magnitude and severity of a nuclear/radiological incident determines the type and degree of response. A tiered approach involves sequential activation of local, regional, state and federal resources, as the size of the incident increases (Stangler 2004). Figure 1 provides an overview of early sequential involvement of various agencies whose objectives are to address public health effects (i.e., consequence management) and causes of a terrorist act (i.e., crisis management). Among the earliest responders are members of the hazardous materials (HAZMAT) team, including the local police and fire departments and emergency medical services (Dainiak et al. 2007).
FIGURE 1.
Initial response to a radiologic incident. Among those arriving at the scene of a radiological incident are members of the Hazards Materials (HAZMAT) Team, including first responders, and fire and police personnel. In some states such as Connecticut, members of the Department of Environmental Protection (DEP) are part of the first-responder team. DEP personnel have the training and expertise to conduct and interpret radiological surveys. The incident commander in the field may request additional help from the New England Regional Health Compact (NERHC) for state members of this compact. Help may also be requested from the Department of Energy (DOE), including its Radiological Assistance Program (RAP), to manage public health consequences, as well as from the Federal Bureau of Investigation (FBI) to manage causes of the crisis. Activities of all agencies are coordinated through the Department of Homeland Security (DHS). Victims are triaged in the field where they are decontaminated, if medically stable. Medically unstable individuals are immediately transported to an area hospital where the Emergency Department Staff responds, together with individuals who are familiar with radiation measurements and medical and surgical subspecialists. Reproduced from Dainiak et al. (7).
Members of the state Department of Environmental Protection (DEP) may also respond as part of the HAZMAT team, providing on site radiological surveys and advice to the incident commander regarding the need to involve additional resources. For example, the New England Regional Health Compact (NERHC) may be called upon to provide additional manpower for assessing an incident occurring in Connecticut, Massachusetts, Rhode Island, New Hampshire, Vermont or Maine. Radiation drills are conducted in order to achieve rapid response from neighboring states. Other regions of the country may have a similar arrangement with neighboring states.
Victims are triaged in the field and assessed for medical condition and contamination. If medically stable, victims should be decontaminated on site and relocated upwind or transported to a hospital, depending upon medical needs. Many of these individuals may require follow-up in an ambulatory treatment center or other outpatient setting for a minor injury, neuropsychiatic assessment or a behavioral disorder. If medically unstable, victims are stabilized and immediately transported to a hospital where definitive medical care is provided. Decontamination is performed after medical stabilization has been achieved.
Healthcare facilities are required to develop medical response plans as part of their disaster planning effort (JCAHCO 2005). State-wide hospital plans have been developed for addressing radiologic emergencies for states, including Connecticut (Dainiak et al. 2006), California (Bushberg 2007), and New York (DOHMH 2007). Mass casualty disaster drills involving radiologic materials are being planned and conducted at increasing frequency (Schleipman et al. 2004; Albanese et al. 2007; Wilkinson et al. 2007). Surge capacity for biodosimetry laboratories has been recently addressed as well (Albanese et al. 2007; Wilkinson et al. 2007). Recommendations of the Connecticut plan include delineation of responsibilities of different categories of healthcare professionals involved in the response, protection of healthcare providers, identification and classification of victims, and early management of individuals who have had or might have had a radiologic exposure (Dainiak et al. 2006). Resuscitation and medical stabilization of the patient with definitive treatment of serious injuries takes precedence over decontamination of the skin, treatment of minor injuries and containment of the treatment area (NCRP 2001; Dainiak et al. 2006). Clinicians must wear appropriate protective clothing (i.e. gown, gloves, masks, eye protection, and head and shoe covers). Depending on the nature of the injuries, it may be necessary to have evaluations performed by subspecialists, including a hematologist, burn physician, trauma surgeon, intensivist and/or dermatologist.
Following medical stabilization, the patient is classified based on presence or absence of physical injury, exposure and/or contamination (Dainiak et al. 2006). Decontamination may be performed by removal of clothing (resulting in approximately 90% decontamination) and showering (resulting in removal of approximately 90% of the remaining contamination). The use of soap and shampoo facilitates decontamination of the skin and hair. Patients are triaged to the OR, routine care floor, critical care area or ambulatory setting for treatment and/or monitoring (Dainiak et al. 2006). If surgery is required, it should be performed within 36–48 hours after exposure (NCRP 2001). This time window is critical since significant exposures will result in leukopenia and immune suppression, thereby predisposing patients to infection. Laboratory monitoring includes obtaining a complete blood count (with a focus on the absolute lymphocyte count, polymorphonuclear cell count and platelet count), obtaining a peripheral blood sample for cytogenetics testing and consideration of internal contamination (Waselenko et al. 2004). The rate of decline in absolute lymphocyte count correlates with whole-body estimated dose and overall prognosis (Flynn and Goans 2006). Assessment for chromosomal aberrations (i.e., ring forms and dicentrics) is the “gold standard” of individual biodosimetry. A recent comparative study in five laboratories confirmed the validity and accuracy of the dicentric chromosome assay (Wilkins et al. 2008). Chromosome analysis may be performed urgently or at a later period of time, depending on the needs and circumstances of the situation. Assessment of prognosis and clinical decision making are based upon radiation dose estimates and the presence of certain clinical signs and symptoms, such as time to onset of nausea and vomiting, rate of decline in absolute lymphocyte count, cutaneous lesions and neurovascular changes, including hypotension, tachycardia, fever and neurological and cognitive deficits (Dainiak et al. 2011a; Dainiak et al. 2011b).
Special decontamination areas include localized skin contamination, contamination of the eyes and wound contamination. Patients with wound contamination must be considered to have internal contamination (DOHMH 2007). Radioactive (i.e. hot) particles should be removed with a long forceps. Internal decontamination should be considered when an individual may have inhaled, ingested or injected radioactive material. Assessment for internal contamination is a complex process that requires specialized expertise (NCRP 1980). Internal decontamination with blocking or diluting agents, chelating agents and other specific agents (for example, Prussian blue) should be considered after consultation with professionals who are familiar with their use in radiation victims.
FEDERAL ASSETS
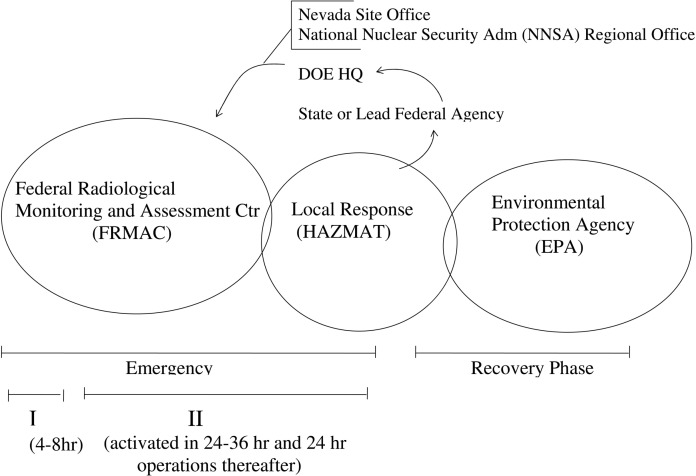
Activation of a federal response may be triggered by a state or lead federal agency. The Department of Energy (DOE) Headquarters is notified, and together with the DOE/Nevada Site Office and the National Nuclear Security Administration (NNSA) Regional Coordinating Office, a decision will be made regarding activation of the Federal Radiological Monitoring and Assessment Center (FRMAC). While FRMAC is involved in the emergency response, the Environmental Protection Agency (EPA) is involved predominately in the recovery phase of an incident. This sequence of activating a radiation response at the federal level is diagramed in Figure 2.
FIGURE 2.
Activation of radiation response assets. A state or lead federal agency may request DOE Headquarters to respond to a radiologic incident. A decision to respond will be made in consultation with the Nevada Site Office and the NNSA Regional Office. During the emergency phase of a response, FRMAC assets are activated. During phase 1 of the emergency phase, on-site help is expected within approximately 4–8 hours. FRMAC should be activated within 24–36 hours, and operational approximately 24 hours thereafter. The EPA is involved in the recovery phase of the response.
Details of national response assets for radiological incidents are reviewed in a recent publication by Remick and colleagues (Remick et al. 2005). During the phase I of an emergency response (the initial 4–8 hours), the Consequence Management Response Team (CMRT) is activated. During the initial 24–36 hours (phase II), the CMRT response initiates 24 hour operations. The Radiological Assistance Program (RAP) is a DOE resource that may be activated for monitoring operations and provision of additional support personnel to enhance radiologic assessment, health and safety issues, and logistics (Remick et al. 2005). RAP regional offices are located in Washington, D.C., Upton, Long Island, NY, Oak Ridge, TN, Aiken, SC, Albuquerque, NM, Argomne, IL, Idaho Falls, ID, Oakland, CA and Richland, WA (NCRP 2001; Stangler 2004; Remick et al. 2005). The regional office closest to the radiological incident may or may not be involved in the response.
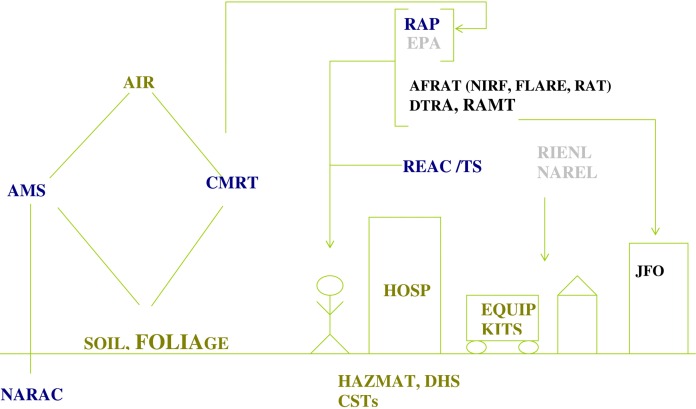
Figure 3 provides a overview of response efforts by the DOE, EPA and Department of Defense (DOD). Sampling of air, soil and foliage may be made by several DOE assets, including the CMRT, the Ariel Measuring System (AMS) and the National Atmospheric Release Advisory Center (NARAC). A three-dimensional model for particle movement is used to calculate real-time estimates of transport and dispersion of radioactive material, using current patterns of weather and assessment of terrain. DOE assets also include the Radiation Emergency Assistance Center/Training Site (REAC/TS) located in Oak Ridge, TN. REAC/TS provides around the clock medical consultants for both clinical and health physics issues. In addition to having clinicians, health physicists and radiobiologists, REAC/TS has the capacity to measure radioactivity using radiological, biological and cytogenetic methods. Its staff is available for triage, external and internal decontamination, prognostic assessments and radiation dose assessment. REAC/TS also offers radiation accident training classes for national and foreign medical, paramedical and health physics professionals. Training courses may be requested by professional groups (Dainiak et al. 2006).
FIGURE 3.
Local and national emergency response. The local response (green) includes activation of HAZMAT units and Civil Support Teams (CSTs). It is coordinated by the Department of Homeland Security (DHS). The national response provides resources to conduct radiation measurements on samples of air, soil and foliage. DOE response (dark blue) includes activation of the Aerial Measuring System (AMS), the National Atmospheric Release Advisory Center (NARAC) and the Consequence Management Response Team (CMRT). The Radiological Assistance Program (RAP) and the Radiation Emergency Assistance Center/Training Site (REAC/TS) are deployable DOE resources that may provide personnel to assist in mitigating an event. EPA assets (gray) include two mobile laboratories (the Radiation and Indoor Environment National Laboratory or RIENL, and the National Air and Radiation Environmental Laboratory or NAREL) that provide expertise and equipment for sample preparation. The Department of Defense may elect to engage in the response (black) through activation of its Air Force Radiation Assessment Team (AFRAT), the Defense Threat Reduction Agency (DTRA) and the Radiological Advisory Medical Team (RAMT). It may be elected to also assign a Joint Field Office (JFO) as a point of contact for the DOD.
NIRF: Nuclear Incident Response Force. FLARE: Field Laboratory for Assessment of Radiation Exposure Team. RAT: Radioanalytical Team. HOSP: hospital.
The EPA may employ several assets to provide expertise in equipment for dealing with sample preparation (see Figure 3). This includes the Radiation and Indoor Environment National Laboratory (RIENL) located in Las Vegas, Nevada, and the National Air and Radiation Environment Laboratory (NAREL) (Remick et al. 2005). These laboratories provide expertise in equipment to prepare samples. They also provide a mobile command post with satellite communications. Both laboratories provide sample survey kits and air samplers, as well as pop-up tents and cargo trailers.
A system of Nuclear Emergency Support Team has been developed to deal with search and identification of nuclear materials and nuclear devices. This includes the Nuclear Emergency Support Team (NEST), Search Response Team (SRT) and Search Augmentation Team (SAT). In addition, the Nuclear/Radiological Advisory Team (NRAT) may be deployed for overseas incidents. Civil support teams are organized as 22-member units of the full-time National Guard. These units have a specialized expertise in communications and technical training in radiological, chemical and biologic incidents.
The National Response Plan (NRP) establishes a strategy for coordinating the national response to a significant incident. Its agencies include the Department of Homeland Security (DHS) and FEMA. Response from the DOD is made after a request for assistance has been made. Depending on the legality, lethality risk and appropriateness of the incident, the Secretary of Defense may delegate a unified combatant commander.
As shown in Figure 3, a Joint Field Office (JFO) may be established and agencies may be mobilized, including the Defense Threat Reduction Agency (DTRA), the Consequence Management Advisory Team (CMAT) and the Air Force Radiation Assessment Team (AFRAT). AFRAT deploys in an effort to provide radiological risk assessment and site recovery. Teams include the Nuclear Incident Response Force (NIRF), the Field Laboratory for Assessment of Radiation Exposure (FLARE) and the Radioanalytical Team (RAT).
CONCLUSION
Response to a significant radiological incident is based upon a layered strategy wherein local, state, regional and national resources are deployed. The degree to which various agencies are activated depends on the magnitude of the radiological event. Roles have been determined for the DOE, EPA and DOE in responding to a nuclear incident. Coordination of a multitude of local and national agencies is critical for a timely, efficient response and for achieving optimal outcomes for victims of an incident.
REFERENCES
- Albanese J, Martens K, Arnold JL, Kelley K, Kristie V, Forte E, Schneider M, Dainiak N. Building Connecticut’s clinical biodosimetry laboratory surge capacity to mitigate the health consequences of radiological and nuclear disasters: a collaborative approach between the state biodosimetry laboratory and Connecticut’s medical infrastructure. Radiation Measurements. 2007;42:1138–1142. [Google Scholar]
- Bushberg JT, Kroger LA, Hartman MB, Leidholdt EM, Miller KL, Derlet R, Wraa C. Nuclear/radiological terrorism:emergency department management of radiation casualties. J Emerg Med. 2007;32:71–85. doi: 10.1016/j.jemermed.2006.05.034. [DOI] [PubMed] [Google Scholar]
- Dainiak N, Ricks RC. The evolving role of haematopoietic cell transplantation in radiation injury: potentials and limitations. Brit J Radiol Supple. 2005;27:169–174. [Google Scholar]
- Dainiak N, Delli Carpini D, Bohan M, Werdmann M, Wilds E, Barlow A, Beck C, Cheng D, Daly N, Glazer P, Mass P, Nath R, Piontek G, Price K, Albanese J, Roberts K, Salner A, Rockwell S. Development of a statewide hospital plan for radiologic emergencies. Int J Radiation Oncology Biol Phys. 2006;65:16–24. doi: 10.1016/j.ijrobp.2005.12.047. [DOI] [PubMed] [Google Scholar]
- Dainiak N, Berger P, Albanese J. Relevance and feasibility of multi-parameter assessment for management of mass casualties from a radiological event. Exp Hematol. 2007;35:17–23. doi: 10.1016/j.exphem.2007.01.007. [DOI] [PubMed] [Google Scholar]
- Dainiak N, Gent RN, Carr Z, Schneider R, Bader J, Buglova E, Chao N, Coleman CN, Ganser A, Gorin C, Hauer-Jensen M, Huff LA, Lillis-Hearne P, Maekawa K, Nemhauser J, Powles R, Schunemann H, Shapiro A, Stenke L, Valverde N, Weinstock D, White D, Albanese J, Meineke V. First global consensus for evidence-based management of the hematopoietic syndrome resulting from exposure to ionizing radiation. Disaster Med Public Health Preparedness. 2011a;5:202–212. doi: 10.1001/dmp.2011.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dainiak N, Gent RN, Carr Z, Schneider R, Bader J, Buglova E, Chao N, Coleman CN, Ganser A, Gorin C, Hauer-Jensen M, Huff LA, Lillis-Hearne P, Maekawa K, Nemhauser J, Powles R, Schunemann H, Shapiro A, Stenke L, Valverde N, Weinstock D, White D, Albanese J, Meineke V. Literature review and global consensus on management of acute radiation syndrome affecting nonhematopoietic organ systems. Disaster Med Public Health Preparedness. 2011b;5:183–201. doi: 10.1001/dmp.2011.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DOHMH . Contaminating Radiological Incidents: A Hospital Planner’s Manual. New York: 2007. [Google Scholar]
- Flynn DF, Goans RE. Nuclear terrorism: triage and medical management of radiation and combined-injury casualties. Surg Clin N Am. 2006;86:601–636. doi: 10.1016/j.suc.2006.03.005. [DOI] [PubMed] [Google Scholar]
- IAEA . Manual for First Responders to a Radiological Emergency. Vienna: 2006. [Google Scholar]
- JCAHCO Oakbrook Terrace. 2005. p. EC-17.
- NCRP . Management of Persons Accidentally Contaminated with Radionuclides. Bethesda: 1980. NCRP Report No. 65. 1079. [Google Scholar]
- NCRP . Bethesda: 2001. Management of Terrorist Events Involving Radioactive Material. NCRP Report No. 138. [Google Scholar]
- Remick AL, Carpo JL, Woodruff CR. U.S. national response assets for radiological incident. Health Phys. 2005;89:471–484. doi: 10.1097/01.hp.0000175447.43906.54. [DOI] [PubMed] [Google Scholar]
- Ricks RC. The radiation-accident patient in the new millennium: past history and future threats. In: Ricks RD, Berger ME, O’Hara FM, editors. The Medical Basis for Radiation-Accident Preparedness: the Clinical Care of Victims. The Parthenon Publishing Group; Boca Raton: 2002. pp. 1–9. [Google Scholar]
- Schleipman AR, Gerbando VH, Castronovo FP. Radiation disaster response: preparation and simulation experience at an academic medical center. J Nucl Med Technol. 2004;32:22–27. [PubMed] [Google Scholar]
- Stangler MJ. Summary of federal and state resources for recovery. In: Brodsky A, Johnson RH Jr, Goans RE, editors. Public Protection from Nuclear, Chemical and Biological Terrorism. Medical Physics Publishing; Madison: 2004. pp. 115–133. [Google Scholar]
- Waselenko JK, MacVittie TJ, Blakely WF, Pesik N, Wiley AL, Dickerson WE, Tsu H, Confer DL, Coleman CN, Seed T, Lowry P, Armitage JO, Dainiak N. Medical Management of the Acute Radiation Syndrome: Recommendations of the Strategic National Stockpile Radiation Working Group. 2004. [DOI] [PubMed]
- Wilkins RC, Romm H, Kao T-C, Awa AA, Yoshida MA, Livingston GK, Jenkins MS, Oestreicher U, Pellmar TC, Prasamar PGS. Interlaboratory comparison of the dicentric chromosome assay for radiation biodosimetry in mass casualty events. Radiat Res. 2008;169:551–560. doi: 10.1667/RR1272.1. [DOI] [PubMed] [Google Scholar]
- Wilkinson D, Segura T, Pru’homme-Lalonde L, Mullins D, Lachapelle S, Qutob S, Thorleifson E, Wilkins R, Morrison D, Dolling J-A, Boreham D. Canadian biodosimetry capacity for response to radiation emergencies. Radiation Measurements. 2007;42:1128–1132. [Google Scholar]