Abstract
Purpose
The revised Tokuhashi score has been widely used to evaluate indications for surgery and predict survival in patients with metastatic spinal disease. Our aim was to analyse the actual survival time of patients treated for metastatic spinal cord compression (MSCC) in comparison with the predicted survival based on the revised Tokuhashi score. This would thereby allow us to determine the overall predictive value of this scoring system.
Methods
This study was a semi-prospective clinical study of all patients with MSCC presenting to our unit over 8 years—data from October 2003 to December 2009 were collected retrospectively and from December 2009, all data collected prospectively to October 2011. Patients were divided into three groups—Group 1 (Tokuhashi score 0–8, n = 84), Group 2 (Tokuhashi score 9–11, n = 83) and Group 3 (Tokuhashi score 12–15, n = 34). Data collected included demographic data, primary tumour histology, surgery type and complications, neurological outcome (Frankel grade) and survival.
Results
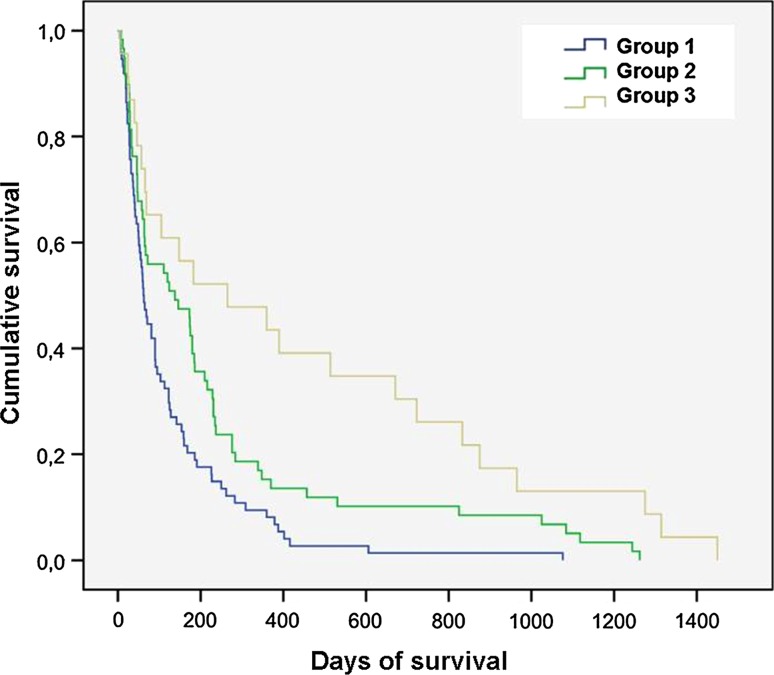
A total of 233 patients with MSCC were managed surgically in our unit during this time. Out of these complete data were available on 201 patients for analysis. Mean age of patients was 61 years (range 18–86; 127 M, 74 F). The primary tumour type was Breast (n = 29, 15 %), Haematological (n = 28, 14 %), Renal (n = 26, 13 %), Prostate (n = 26, 13 %), Lung (n = 23, 11 %), Gastro-intestinal (n = 11, 5 %), Sarcoma (n = 9, 4 %) and others (n = 49, 24 %). All patients included in the study had surgical intervention in the form of decompression and stabilisation. Posterior decompression and stabilisation was performed in 171 patients (with vertebrectomy in 31), combined anterior and posterior approaches were used in 18 patients and 12 had an anterior approach only. The overall complication rate was 19 % (39/201)—the most common being wound infection (n = 15, 8 %). There was no difference in the neurological outcome (Frankel grade) between Groups 1 and 2 (p = 0.34) or Groups 2 and 3 (p = 0.70). However, there was a significant difference between Groups 1 and 3 (p = 0.001), with Group 3 having a significantly better neurological outcome. Median survival was 93 days in Group 1, 229 days in Group 2 and 875 days in Group 3 (p = 0.001). The predictive value between the actual and predicted survival was 64 % (Group 1), 64 % (Group 2) and 69 % (Group 3). The overall predictive value of the revised Tokuhashi score using Cox regression for all groups was 66 %.
Conclusion
We would conclude that although the predictive value of the Tokuhashi score in terms of survival time is at best modest (66 %), the fact that there were statistically significant differences in survival between the groups looked at in this paper indicates that the scoring system, and the components which it consists of, are important in the evaluation of these patients when considering surgery.
Keywords: Revised Tokuhashi score, Metastatic spinal cord compression
Introduction
The skeletal system is the third most common site for metastases, behind the pulmonary and hepatic systems [1] and the spine is the commonest site of skeletal metastasis. Post-mortem studies have shown that, depending on the histopathology of the primary site, 30–90 % of patients with terminal cancer have metastatic spinal disease [2, 3]. It is expected that symptomatic metastatic spinal disease will become more prevalent as survival rates for many common cancers improve. metastatic spinal cord compression (MSCC) occurs in 5–10 % of cancer patients (most commonly from breast, prostate and lung cancers) and in up to 40 % of patients who have pre-existing non-spinal bone metastases [4, 5].
The key principles of management of the MSCC include optimum level of surgical intervention in proportion to pathology and prognosis. Such intervention should aim to restore, where possible, ambulatory function and preservation of neurology on a background of a stable, pain-free spinal column. In light of this aim, several scoring systems have been devised to help the surgeon plan the surgical approach and definitive management.
The Tokuhashi score—designed in 1987 and revised in 1998—has been used to determine the prognosis for these patients to guide adequate treatment approaches [6–8]. The scoring system is used to evaluate surgical candidates and is based on six parameters: (1) general condition, (2) number of extraspinal bone metastases, (3) number of metastases in the vertebral body, (4) presence or absence of metastases to major internal organs, (5) site of the primary lesion and (6) severity of palsy. The type of the primary tumour is rated between 0 and 5. All other parameters are rated between 0 and 2, so that the maximum score is 15 (Table 1). According to this score, if the total score is 8 or less, the predicted survival period is less than 6 months, favouring more conservative or palliative procedures. In patients with a total score of 12 or more, there is a predicted survival time of greater than 1 year, and excisional procedures are favoured. Finally, in patients with a score between 9 and 11, decisions are made on an individual basis, taking into account the number of spinal metastases and other metastatic sites.
Table 1.
Revised Tokuhashi evaluation system for the prognosis of metastatic spine tumours
| Characteristic score | |
|---|---|
| General condition (performance status) | |
| Poor (PS 10–40 %) | 0 |
| Moderate (PS 50–70 %) | 1 |
| Good (PS 80–100 %) | 2 |
| No. of extraspinal bone metastases foci | |
| ≥3 | 0 |
| 1–2 | 1 |
| 0 | 2 |
| No. of metastases in the vertebral body | |
| ≥3 | 0 |
| 2 | 1 |
| 1 | 2 |
| Metastases to the major internal organs | |
| Unremovable | 0 |
| Removable | 1 |
| No metastases | 2 |
| Primary site of the cancer | |
| Lung, osteosarcoma, stomach, bladder, oesophagus, pancreas | 0 |
| Liver, gallbladder, unidentified | 1 |
| Others | 2 |
| Kidney, uterus | 3 |
| Rectum | 4 |
| Thyroid, breast, prostate, carcinoid tumour | 5 |
| Palsy | |
| Complete (Frankel A, B) | 0 |
| Incomplete (Frankel C, D) | 1 |
| None (Frankel E) | 2 |
Criteria of predicted prognosis
Total score (TS) 0–8: less than 6 months
TS 9–11: 6–12 months
TS 12–15: greater than 1 year
Only a few reports have been published which have evaluated the revised Tokuhashi scoring system in a mixed population of patients with various forms cancer [8–11]. Furthermore, our own experience suggested that survival in patients was often greater than what was predicted by this scoring system. Our objective was therefore, in a semi-prospective study, to analyse the actual survival time of patients treated for metastatic spinal cord compression (MSCC) in comparison with the predicted survival based on the revised Tokuhashi score. This would thereby allow us to determine the overall predicted value of this scoring system.
Methods
We undertook a review of all patients with MSCC presenting to our unit over 8 years—data from October 2003 to December 2009 were collected retrospectively and from December 2009, all data collected prospectively to October 2011. Patients were managed with the involvement of multidisciplinary teams including oncology as necessary. Following thorough clinical examination, MRI of the whole spine, a staging CT scan and other investigations (e.g. biopsy) as appropriate for the pathology were performed.
Data collected included demographic data, primary tumour histology, surgery type and complications, neurological outcome (Frankel grade) and survival. Additional details obtained were site of primary tumour, histology, Karnofsky-index, pre-operative and post-operative neurological status as well as number and operability of spinal metastases. Based on these figures we generated the revised Tokuhashi score for each patient. Patients were divided into three groups—Group 1 (Tokuhashi score 0–8), Group 2 (Tokuhashi score 9–11) and Group 3 (Tokuhashi score 12–15). The date of death was available for all deceased patients. The results were then compared with the predicted survival time estimated by the revised Tokuhashi score.
All patients included only those undergoing urgent or semi-urgent surgical intervention for MSCC. Patients younger than 18 years and those managed by non operative means were excluded from the study. Research approval was not required as this study was conducted for ‘service evaluation’ as per our hospitals’ guidelines.
Statistics
All data were stored in Excel database (Microsoft corp, Redmond, WA, USA). Statistical analysis was carried out using SPSS-Software. Statistical significance was determined as a p value less than or equal to 0.05. Descriptive statistics and measurement of skewness and kurtosis were performed. All the data did not follow the normal distribution and therefore non-parametric tests were used. For the measurement of statistical significance between the Frankel scores the Wilcoxon signed ranks test was used. For the control of data distribution for survival, in addition to the measurement of skewness and kurtosis, histograms and the Kolmogorov–Smirnov (K–S) test were used. Since the survival data were very skewed (1.2–1.5) and the K–S showed abnormal distribution in all groups (p = 0.000 to p = 0.001), we report our data using median and we used non-parametric tests to look for statistical significance. More specifically, the Kruskal–Wallis and the median tests were used, since both are robust when violations of normality exist and are less sensitive to extreme outliers in the data. The strength of association between the real and the predicted survival time according to the revised Tokuhashi score was calculated using Cox regression analysis and Kaplan–Meier survival plots were created for all three groups. For this we used the mean survival times (as this is what is predicted by the revised Tokuhashi score).
Results
During the 8-year study period, a total of 233 patients with MSCC were managed surgically in our unit. We were able to obtain complete information for 201 patients and these formed the analysed cohort. The mean age of the patients at the time of the surgical procedure was 61 years (range 18–86; 127 M, 74 F). The primary tumour type was breast (n = 29, 15 %), haematological (n = 28, 14 %), renal (n = 26, 13 %), prostate (n = 26, 13 %), lung (n = 23, 11 %), gastro-intestinal (n = 11, 5 %), sarcoma (n = 9, 4 %) and others (n = 49, 24 %).
All patients included in the study had surgical intervention in the form of decompression and stabilisation. Posterior decompression and stabilisation was performed in 171 patients (with vertebrectomy in 31), combined anterior and posterior approaches were used in 18 patients and 12 had an anterior approach only.
The overall complication rate in this study was found to be 19 % (39/201). The most common complication was wound infection (n = 15, 8 %). Other complications included chest infection (n = 8, 4 %), neurological worsening (n = 4, 2 %), failure of the metal work (n = 4, 2 %) and pulmonary embolisation (n = 3, 1.5 %).
At presentation, the neurology was Frankel A in 9 (4 %), B in 6 (3 %), C in 33 (16 %), D in 107 (53 %) and E in 46 (23 %) patients. Post operatively, the neurology was Frankel grade A in 8 (4 %), B in 9 (4 %), C in 31 (15 %), D 78 (39 %) and E in 75 (37 %) patients. For Group 1, most of the patients had a post-operative Frankel score C (n = 20, 24 %), D (n = 33, n = 39 %) and E (n = 23, 27 %). For Group 2, most had scores Frankel D (n = 35, 42 %) and E (n = 31, 37 %). For Group 3, most had Frankel D (n = 10, 29 %) and E (n = 21, 62 %). Using the Wilcoxon signed ranks test, we found no significant difference between the outcome scores of Groups 1 and 2 (p = 0.34), or between Groups 2 and 3 (p = 0.70). However, there was a significant difference between Groups 1 and 3 (p = 0.0001; Table 2).
Table 2.
Neurological outcome of patients based on the revised Tokuhashi score
| Frankel Grade | Prognostic group | p value | |||||
|---|---|---|---|---|---|---|---|
| Group 1 (0–8) | Group 2 (9–11) | Group 3 (12–15) | |||||
| Pre-op | Post-op | Pre-op | Post-op | Pre-op | Post-op | ||
| A | 6 | 2 | 3 | 6 | 0 | 0 | Group 1 vs. 2 |
| B | 4 | 6 | 1 | 2 | 1 | 1 | p = 0.34 |
| C | 16 | 20 | 13 | 9 | 4 | 2 | Group 2 vs. 3 |
| D | 40 | 33 | 50 | 35 | 17 | 10 | p = 0.70 |
| E | 18 | 23 | 16 | 31 | 12 | 21 | Group 1 vs. 3 p = 0.001 |
Group 1 [revised Tokuhashi score 0–8 (Table 3)]
Table 3.
Survival of patients in the three groups based on the revised Tokuhashi score
| Parameter | Prognostic group | p value | ||
|---|---|---|---|---|
| 0–8 | 9–11 | 12–15 | ||
| No. | 84 | 83 | 34 | |
| Mean survival (days) | 350 | 439 | 922 | p = 0.001 |
| Range | 5–2,256 | 8–1,902 | 6–2,222 | |
| Median | 93 | 229 | 875 | p = 0.001 |
| Predictive value | 64 % | 64 % | 69 % | |
| Overall predictive value | 66 % | |||
The median survival was 93 days (5–2,567, SD ± 715, K–S: p = 0.0001) in the 0–8 Group. The predictive value between the prognostic score and actual survival was 64 %.
Group 2 [revised Tokuhashi score 9–11 (Table 3)]
The median survival was 229 (8–1,902, SD ± 971, K–S: p = 0.0001) days in the 9–11 Group. The predictive value between the prognostic score and actual survival was 64 % in the second Group.
Group 3 [revised Tokuhashi score 12–15 (Table 3)]
The median survival was 875 (6–2,222, SD ± 993, K–S: p = 0.001) days in the 12–15 Group. The predictive value between the prognostic score and actual survival was 69 % in this group with the best prognosis.
Overall validity of the revised Tokuhashi score
The overall predictive value of the revised Tokuhashi score using Cox regression for all groups was 66 %. Only five patients had received preoperative radiotherapy (for lung, breast and prostate primaries) and thus it is not really possible to make any useful conclusions with regard to the influence of preoperative radiotherapy on complications or mortality.
At the time of final review, 34/201 (17 %) were still alive—Group 1: 5/84 (6 %), Group 2: 17/83 (20 %), Group 3 12/34 (35 %). Figure 1 shows the Kaplan–Meier survival curve for all three groups for the 167 patients who were deceased at the final review. Additionally, using the Kruskal–Wallis test, a statistically significant difference between the survival in all groups was found (H(2) = 24.6, p = 0.001) with a mean rank of 75.33 for Group 1, 99.5 for Group 2 and 130.2 for Group 3. Using the median test which is more robust for extreme outliers and violations of homogeneity equally significant results were found (H(2) = 21.3, p = 0.001). For Group 1, 55 cases were below the median; for Group 2, 32 cases; and for Group 3, 7 cases. Finally, on the Kaplan–Meier survival curve, the lower bound 95 % confidence interval (CI) for Group 1 was 93 and the upper 249; for Group 2 the same intervals were 155 and 317; for Group 3 these intervals were 261 and 643, respectively.
Fig. 1.
Kaplan Meier survival curve for all three groups
Discussion
We found that although there was a significant difference in the mean survival between groups, there was only a modest predictive value between the predicted and actual survival in this study (66 %). The prognostic criteria using the revised Tokuhashi scoring system was only moderately useful in predicting actual survival.
The treatment aims for MSCC are to restore or preserve neurological function, restoration or maintenance of spinal stability, pain control and improving the quality of life. Surgical indications include the need to establish a diagnosis, spinal instability and epidural cord compression with cord dysfunction from bone or from tumour that is not highly radiation sensitive. It can be argued that despite the use of aggressive surgical techniques the treatment of MSCC is largely palliative in most cases. Patchell et al. [12] found that patients who underwent surgical treatment followed by radiotherapy for metastatic epidural spine compression had a significantly better outcome with regard to survival, mobility, incontinence and reduced opioid requirement than patients who were treated conservatively with radiotherapy and steroids alone.
The revised Tokuhashi score is considered to be a reasonable tool for predicting the prognosis of patients’ life expectancy as has been confirmed by numerous authors [8–14]. In a retrospective review of 246 patients, Tokuhashi and colleagues showed a predictive value of 85.3 % in the group with a score of 0–8, 73.1 % with a score of 9–11 and 95.4 % in the 12–15 group. The predictive value between the predicted prognosis from the criteria of the total scores and the actual survival period was high in patients in each group—86.4 % in the 118 patients evaluated prospectively after 1998 and 82.5 % in all 246 patients evaluated retrospectively [7].
In our study, the actual survival after surgery was greater than that predicted by the revised Tokuhashi score. This improved survival following surgical intervention was also seen by Majeed et al. [13] in their relatively small series of 55 patients. Surgery has a positive impact on improvement in patients’ neurological status and Sioutos et al. [14] demonstrated that patients who were ambulatory pre-operatively and those with only one vertebral involvement survived statistically longer than patients who were non-ambulatory and with multilevel disease.
An accurate point-based system could help to strategise the management plan more comprehensively. In a prospective study, Yamashita et al. [11] found in a study of patients with MSCC that the actual survival matched the predicted based on the revised Tokuhashi score in 79 %. In a retrospective study of 217 patients, Ulmar et al. [9] concluded that this score showed the highest reliability between the real and predicted survival, with a predictive value of 70.9 %. In another retrospective study of 109 patients, Mollahoseini et al. [15] found the revised Tokuhashi scoring system to be highly predictive of the survival in patients with spinal metastases in Iran although the predicted value for the individual scoring groups was not calculated in this study. Pointillart et al. [16] concluded from a prospective study that neither the original nor revised Tokuhashi scores were reliable in predicting survival in their European population. The predictive value for the revised Tokuhashi scoring system was found to be less than 60 %. Padalkar and Tow [17] concluded from their retrospective study that the Tomita score correlated more closely with survival than the Tokuhashi score. The type of primary tumour was not found to be significantly associated with survival in their study. Leithner et al. [18] concluded from their retrospective study comparing seven similar scoring systems that the original Bauer score and a modified Bauer score without scoring for pathologic fracture were practicable and highly predictive for outcome and survival.
In our study, patients undergoing conservative or palliative treatment were not included as all patients underwent decompression and stabilisation surgery. Yet, there was a significant difference in the mean survival between groups. This suggests that despite surgical treatment, patients with a low revised Tokuhashi score are still likely to have a shorter survival when compared with patients with a higher score. A limitation in our study is that it is a semi-prospective design (with patients included both retrospectively as well as prospectively). We have also only included patients with MSCC—our analysis may have been different had spinal metastases patients with pain/instability/pathological fracture without cord compression also been included.
From our study, the revised Tokuhashi score had only a moderate predicted value in predicting the survival in patients with MSCC and thus offering some, but incomplete, guidance in the management of these patients. The actual survival in our cohort group matched the predicted survival in 66 % patients. This would suggest that certain patients may be refused surgical intervention if the revised Tokuhashi scoring system alone is utilised in deciding whether surgery (and indeed the type) should be undertaken or not. Also, the score can be used only on patients with metastasis with symptomatic cord compression but does not help plan the management of asymptomatic patients [6].
With the recent advances in oncology treatment, regional variations and dissimilar behaviour of different primaries, especially those responsive to hormonal treatment (like prostate and breast), a constant evaluation and evolution of such a system is mandatory. Tokuhashi himself has suggested that flexible revisions are necessary (to the scoring system) for an improved prognostic evaluation system based on the effects of new treatment methods in various fields [19]. We would conclude that although the predictive value of the Tokuhashi score in terms of survival time is at best modest, the fact that there were statistically significant differences in survival between the groups looked at in this paper indicates that the scoring system, and the components which it consists of are important in the evaluation of these patients when considering surgery.
Conflict of interest
None.
References
- 1.Aaron AD. The management of cancer metastatic to bone. JAMA. 1994;272:1206–1209. doi: 10.1001/jama.1994.03520150074040. [DOI] [PubMed] [Google Scholar]
- 2.Cobb CA, et al. Indications for nonoperative treatment of spinal cord compression due to breast cancer. J Neurosurg. 1997;47:653–658. doi: 10.3171/jns.1977.47.5.0653. [DOI] [PubMed] [Google Scholar]
- 3.Wong DA, et al. Spinal metastases: the obvious, the occult, and the imposters. Spine. 1990;15:1–4. doi: 10.1097/00007632-199001000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Barron KD, et al. Experiences with metastatic neoplasms involving the spinal cord. Neurology. 1959;9:91–106. doi: 10.1212/WNL.9.2.91. [DOI] [PubMed] [Google Scholar]
- 5.Schaberg J, Gainor BJ. A profile of metastatic carcinoma of the spine. Spine. 1985;10:19–20. doi: 10.1097/00007632-198501000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Tokuhashi Y, Matsuzaki H, Toriyama S, Kawano H, Ohsaka S. Scoring system for the preoperative evaluation of metastatic spine tumour prognosis. Spine. 1990;15:1110–1113. doi: 10.1097/00007632-199011010-00005. [DOI] [PubMed] [Google Scholar]
- 7.Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumour prognosis. Spine. 2005;30:2186–2191. doi: 10.1097/01.brs.0000180401.06919.a5. [DOI] [PubMed] [Google Scholar]
- 8.Tokuhashi Y, Yasumitsu A, Umezawa N. Outcome of treatment for spinal metastases using scoring system for preoperative evaluation of prognosis. Spine. 2009;34:69–73. doi: 10.1097/BRS.0b013e3181913f19. [DOI] [PubMed] [Google Scholar]
- 9.Ulmar B, Huch K, Naumann U, et al. Evaluation of the Tokuhashi prognosis score and its modifications in 217 patients with vertebral metastases. Eur J Surg Oncol. 2007;33(7):914–919. doi: 10.1016/j.ejso.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 10.Putz C, Wiedenhöfer B, Gerner HJ, Fürstenberg CH. Tokuhashi prognosis score: an important tool in prediction of the neurological outcome in metastatic spinal cord compression: a retrospective clinical study. Spine. 2008;33(24):2669–2674. doi: 10.1097/BRS.0b013e318188b98f. [DOI] [PubMed] [Google Scholar]
- 11.Yamashita T, Siemionow KB, Mroz TE, Podichetty V, Lieberman IH. A prospective analysis of prognostic factors in patients with spinal metastases: use of the revised Tokuhashi score. Spine (Phila Pa 1976) 2011;36(11):910–917. doi: 10.1097/BRS.0b013e3181e56ec1. [DOI] [PubMed] [Google Scholar]
- 12.Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643–648. doi: 10.1016/S0140-6736(05)66954-1. [DOI] [PubMed] [Google Scholar]
- 13.Majeed H, Kumar S, Bommireddy R, Klezl Z, Calthorpe D. Accuracy of prognostic scores in decision making and predicting outcomes in metastatic spine disease. Ann R Coll Surg Engl. 2012;94(1):28–33. doi: 10.1308/003588412X13171221498424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sioutos PJ, Arbit E, Meshulam CF, Galicich JH. Spinal metastases from solid tumours. Analysis of factors affecting survival. Cancer. 1995;76:453–459. doi: 10.1002/1097-0142(19951015)76:8<1453::AID-CNCR2820760824>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 15.Mollahoseini R, Farhan F, Khajoo A, Jouibari MA, Gholipour F. Is Tokuhashi score suitable for evaluation of life expectancy before surgery in Iranian patients with spinal metastases? J Res Med Sci. 2011;16(9):1183–1188. [PMC free article] [PubMed] [Google Scholar]
- 16.Pointillart V, Vital JM, Salmi R, Diallo A, Quan GM. Survival prognostic factors and clinical outcomes in patients with spinal metastases. J Cancer Res Clin Oncol. 2011;137(5):849–856. doi: 10.1007/s00432-010-0946-0. [DOI] [PubMed] [Google Scholar]
- 17.Padalkar P, Tow B. Predictors of survival in surgically treated patients of spinal metastasis. Indian J Orthop. 2011;45(4):307–313. doi: 10.4103/0019-5413.82333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leithner A, Radl R, Gruber G, Hochegger M, Leithner K, Welkerling H, Rehak P, Windhager R. Predictive value of seven preoperative prognostic scoring systems for spinal metastases. Eur Spine J. 2008;17(11):1488–1495. doi: 10.1007/s00586-008-0763-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tokuhashi Y, Ajiro Y, Umezawa N. Outcome of treatment for spinal metastases using scoring system for preoperative evaluation of prognosis. Spine. 2008;34(1):69–73. doi: 10.1097/BRS.0b013e3181913f19. [DOI] [PubMed] [Google Scholar]