Abstract
We report a case of a 39-year-old female with a ventricular septal defect (VSD) and a giant appendiform aneurysm of the membranous septum, illustrated by echocardiography and magnetic resonance imaging. From the literature a short review of the prevalence of spontaneous closure of VSDs together with the possible complications of persisting VSDs is presented. Since patients stay at risk in later years, follow-up at regular intervals is advised.
Electronic supplementary material
The online version of this article (doi:10.1007/s12471-012-0343-1) contains supplementary material, which is available to authorized users.
Keywords: Ventricular septal defect, Aneurysm membranous septum, Spontaneous closure, Echocardiography, Magnetic resonance imaging
Case
A 39-year-old female presented to the hospital with palpitations. She was diagnosed at birth with a ventricular septal defect (VSD) for which she received cardiological follow-up until the age of five. On physical examination a late systolic-early diastolic murmur was heard. The electrocardiogram showed sinus rhythm with an incomplete right bundle branch block. On Holter monitoring normal sinus rhythm with sporadic premature atrial and ventricular complexes was seen. The palpitations subsided spontaneously. In the diagnostic workup, echocardiography showed a small isolated VSD with a diameter of 6 millimeter (mm) and a giant aneurysm of the membranous septum (AMS), with a 25 mm long tube, protruding into the right ventricle (RV) with a terminal diameter of 8 mm (Figs. 1a, b, 2a) (also movie). We could not detect a left-to-right (L-R) shunt (Figs. 1c, 2b). Apparently the aneurysm has closed the VSD. There was no obstruction of the right ventricular outflow tract. Otherwise no abnormalities were found on echocardiography, especially no signs of left ventricular (LV) volume overload, pulmonary hypertension or valvular incompetence. Additionally magnetic resonance imaging (MRI) was performed confirming the VSD and the giant appendiform AMS in an otherwise completely normal heart. (Fig. 3)
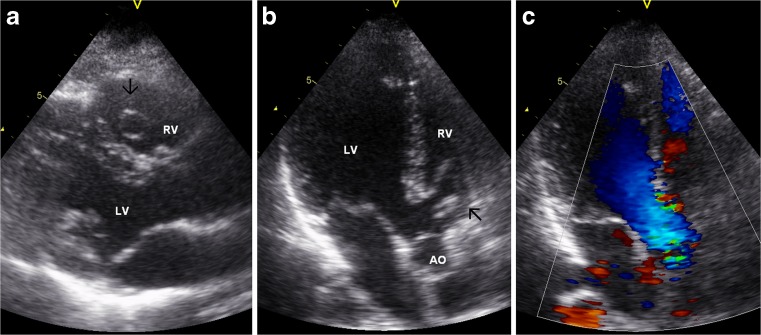
Fig. 1.
Cardiac ultrasound with parasternal (a, left) and apical (b, middle and c, right) views demonstrating an aneurysm (arrow) of the membranous septum, protruding into the RV. RV = right ventricle, LV = left ventricle, AO = aorta
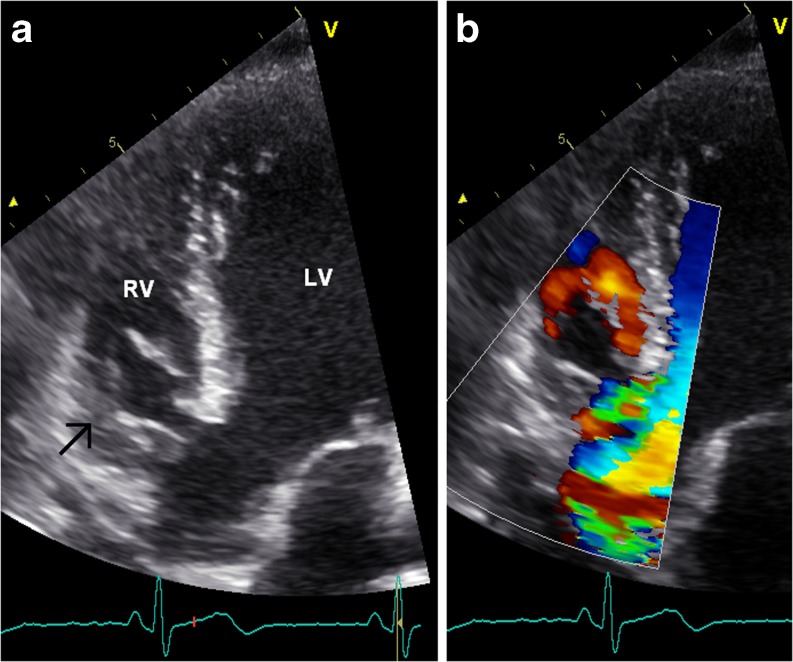
Fig. 2.
Apical views of the echocardiogram showing the AMS (arrow, a, left). Colour Doppler (b, right) visualising flow in the RV around the AMS but not through the VSD
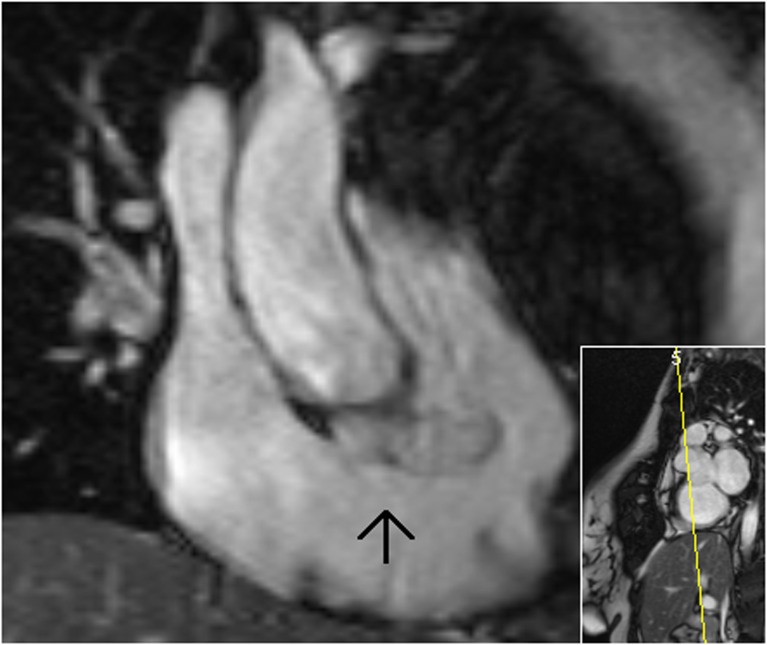
Fig. 3.
Coronal view of a cardiac MRI image displaying a giant appendiform aneurysm (arrow) protruding into the right ventricle
Discussion
Isolated VSDs are the most common congenital heart malformation at birth, around 30–40 %, if bicuspid aortic valve is not counted [1]. VSD is the most frequent main diagnosis in the CONCOR database, the Dutch registry of adults with congenital heart disease [2]. In membranous VSDs spontaneous closure is frequent. During childhood, 23 % (0–33 %) of the small membranous VSDs close spontaneously [3] and after the age of 17, a smaller portion of 4–10 % close spontaneously [4, 5]. Complete or partial closure may occur by adhesion of the septal leaflet of the tricuspid valve to the edge of the defect, often with formation of an aneurysm. The prevalence of an AMS in patients with a membranous VSD is reported by the earlier-mentioned studies of Miyake et al. and Neumayer et al. to be as high as 48 % during childhood [3] and 10 % above 17 years of age [4].
Although the majority of patients with a small VSD and an insignificant L-R shunt, without LV volume overload or pulmonary hypertension, usually remain asymptomatic and do not require surgical or catheter intervention [1, 6], serious complications can occur. Infective endocarditis is reported in 4–11 % [4, 5, 7], progressive aortic regurgitation in 5 % [4] and because of progressive volume overload a closure procedure may be needed in up to 7–10 % of the cases [4, 5].
The formation of AMS has often been considered to be benign but it may, besides the above-mentioned complications, lead to tricuspid regurgitation and rarely to a rupture of the aneurysm or a late right ventricular outflow tract obstruction [8]. The treatment of VSDs, with or without an AMS, is expectative in patients without symptoms. When symptoms do occur, surgical [1, 8, 9] or percutaneous [1, 9, 10] closure may be necessary. Because of these possible complications, the European Society of Cardiology (ESC) states that follow-up at 3 to 5 year intervals may be reasonable [1].
In our case, the aneurysm is formed into a tube, protruding deeply into the right chamber. Possible mechanisms of this process, besides the above-mentioned tricuspid septal leaflet involvement, are deposition of fibrin over the margins of the VSD in the presence of a left-to-right shunt flow jet [11]. Though there were no symptoms, apart from the palpitations at presentation, and cardiac function was adequate, progressive growth of the aneurysm can occur and may lead to complications in the future.
Conclusion
Although small ventricular septal defects seem innocent, the clinical course is not necessarily benign during adult life, even in the absence of symptoms, as pointed out by the presented case. Therefore regular follow-up is indicated, as the ESC recommends.
Electronic supplementary material
(AVI 135053kb)
Acknowledgments
We would like to thank Mrs B. Feyen from the Echocardiography Department, Mr R. Dragt from the Radiology Department and Mr A. Becht, clinical physicist for their technical help.
Disclosures
None
References
- 1.Baumgartner H, Bonhoeffer P, de Groot NM, et al. ESC Guidelines for the management of grown-up congenital heart disease. Eur Heart J. 2010;31:2915–2957. doi: 10.1093/eurheartj/ehq249. [DOI] [PubMed] [Google Scholar]
- 2.CONCOR Data Monthly publication. Neth Heart J. 2010;18:106. [Google Scholar]
- 3.Miyake T, Shinohara T, Fukuda T, et al. Spontaneous closure of perimembranous ventricular septal defect after school age. Pediatr Int. 2008;50:632–635. doi: 10.1111/j.1442-200X.2008.02642.x. [DOI] [PubMed] [Google Scholar]
- 4.Neumayer U, Stone S, Somerville J. Small ventricular septal defects in adults. Eur Heart J. 1998;19:1573–1582. doi: 10.1053/euhj.1998.1083. [DOI] [PubMed] [Google Scholar]
- 5.Soufflet V, Van de Bruaene A, Troost E, et al. Behavior of unrepaired perimembranous ventricular septal defect in young adults. Am J Cardiol. 2010;105:404–407. doi: 10.1016/j.amjcard.2009.09.047. [DOI] [PubMed] [Google Scholar]
- 6.Gabriel HM, Heger M, Innerhofer P, et al. Long term outcome of patients with ventricular septal defects considered not to require surgical closure during childhood. J Am Coll Cardiol. 2002;39:1066–1071. doi: 10.1016/S0735-1097(02)01706-0. [DOI] [PubMed] [Google Scholar]
- 7.CONCOR Data Monthly publication. Neth Heart J. 2009;18:36. [Google Scholar]
- 8.Yilmaz AT, Ozal E, Arslan M, et al. Aneurysm of the membranous septum in adult patients with perimembranous ventricular septal defect. Eur J Cardiothorac Surg. 1997;11:307–311. doi: 10.1016/S1010-7940(96)01058-5. [DOI] [PubMed] [Google Scholar]
- 9.Prasad S. Ventricular septal defect. In: Gatzoulis MA WG, Daubeney PEF, editors. Diagnosis and management of adult congenital heart disease. Philadelphia: Churchill Livingstone; 2003. pp. 171–178. [Google Scholar]
- 10.Bian C, Ma J, Wang J, et al. Perimembranous ventricular septal defect with aneurysm: two options for transcatheter closure. Tex Heart Inst J. 2011;38:528–532. [PMC free article] [PubMed] [Google Scholar]
- 11.Takaki A, Ogawa H, Wakeyama T, et al. Tricuspid pouch can cause systemic embolization in adulthood. Circ J. 2006;70:631–633. doi: 10.1253/circj.70.631. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(AVI 135053kb)