Abstract
Background
It is generally believed that there is a beneficial effect of collaterals on death and re-infarction statistics in patients with coronary artery disease (CAD) but studies to date are small and inconsistent.
Objective
To meta-analyse the studies published in this field in order to obtain more powerful information.
Methods
We searched Medline and major journals (2000 to 2011) for studies evaluating the effect of coronary collaterals on mortality. Publication bias, lack of heterogeneity, and lack of robustness were assessed using the standard procedures for such purposes.
Results
A total of 10 studies describing mortality, enrolling 6791 participants, were included in this analysis. In patients with collateralisation a significant relation with reduced mortality was seen compared with those without collateralisation, at an odds ratio of 0.47, p < 0.0001, and a reduction in deaths and re-infarctions at 0.54, p < 0.0001. Some publication bias, some heterogeneity and some lack of robustness were demonstrated. A meta-regression with the odds ratios of the presence of traditional atherosclerotic risk factors as predictors and the odds ratios of mortality and the composite deaths and re-infarctions as outcome showed no relationships.
Conclusions
In CAD patients from the post-percutaneous coronary intervention era the presence of collaterals reduced mortality by 0.47 (p < 0.0001) and deaths and re-infarctions by 0.54 (p < 0.0001). Furthermore, in the present meta-data, the atherosclerotic risk factors were no more present in patients with collaterals than they were in those without.
Keywords: Acute coronary syndromes, Coronary collateral circulation, Mortality, Percutaneous coronary intervention
Introduction
The human coronary circulation is not an end-arterial system. Coronary collateral circulation has been shown to have a significant protective effect on myocardial viability in animal models, but its functional significance and the general impact on mortality in humans is still controversial [1, 2]. The role of coronary collateral circulation to the myocardium at risk in the setting of coronary artery disease (CAD) and acute coronary occlusion has been of special interest in the last decades. Also the Netherlands Heart Journal has given considerable attention to the issue of collaterals and their importance [3–5]. In many studies the presence of angiographically detectable collaterals is seen as a positive predictive and protective factor on enzymatic infarct size and pre- and post-intervention haemodynamic conditions in patients with acute myocardial infarction (MI) treated by primary percutaneous coronary intervention (PCI) [6, 7]. The presence of visible coronary collateral circulation had a protective effect on the jeopardised myocardium and enzymatic infarct size, resulting in a better myocardial reperfusion and short-time clinical outcome and mortality than patients without coronary collateral circulation [8, 9].
However, studies were small, and unequivocal evidence of the effect of collaterals on the risk of deaths and re-infarctions is lacking. In a recent large international study [10] the effect of collaterals on mortality was significantly in favour of collaterals. However, the patient characteristics between the patients with and without collaterals were very different and confounding could thus not be excluded. Indeed, in a multivariable analysis of these data the beneficial effect of the collaterals was lost.
In a recent meta-analysis by Meier et al. [2] a significant advantage of collaterals was established. However, this meta-analysis included both studies from the pre- and post-PCI era.
In the current paper we only include studies published after 2000, all of which include PCI as treatment modality whenever indicated. This makes these studies more homogeneous for pooling. First of all, we will assess both mortality and the composite endpoint deaths and re-infarctions. Studies with significant differences in more than three patient characteristics between the patients with and without collaterals will be considered as lower quality studies, and will, therefore, be used for assessing the robustness of this meta-analysis.
Second, the presence of traditional atherosclerotic risk factors in the patients with and without collaterals will be studied, and their effects on mortality and the composite of deaths and re-infarctions will be assessed using meta-regression.
Methods
A total of nine studies describing mortality, enrolling 6791 participants, were included in this meta-analysis. We included studies from 2000 until now for assuring the comparability in possibility for PCI when needed, where indicated and possible in the Western cardiology departments. We searched Medline, Google, major journals, and PubMed from 2000 through to September 2011, and reference lists of selected articles on the subject.
All studies containing information on the presence of collaterals according to Rentrop’s criteria or positive blush tests from the collaterals into the ischaemic area were included in this analysis. Our search terms were coronary collateral circulation, acute coronary syndrome, PCI and mortality. The endpoint of this analysis was the impact of collateral circulation on all-cause mortality and the combinations ‘all-cause deaths and re-infarctions’.
Publication bias will be assessed by Christmas tree plots [11], heterogeneity will be assessed by fixed effect tests for heterogeneity and I-square values (Thompson) [12], and robustness will be assessed by meta-analysing the high-quality and low-quality studies separately.
It was assumed that a log-linear relationship existed between the time of follow-up and the odds of events and that patient stratification with blush and Rentrop criteria would produce similar patterns.
The presence of traditional atherosclerotic risk factors in the patients with and without collaterals were assessed with odds ratios, and their effects on mortality and the composite of deaths and re-infarctions were assessed with meta-regression using a multiple linear regression model with the odds ratios of the risk factors as predictors and the odds ratios of mortality and the composite of deaths and re-infarctions as outcome.
Results
Fifteen studies were initially included. Five of them were excluded because no survival data were reported per group. Of the ten studies included [1, 3, 6, 7, 10–15] nine studies reported mortality during follow-up of 0.6–9 years, while seven studies reported the composite endpoint of deaths and re-infarctions separately for the subgroups. Baseline clinical characteristics of the included trials are listed in Table 1.
Table 1.
Baseline characteristics of included trials
| Study | Year | N | Setting | PCI | Age (years) | Male (%) | Smoking (%) | Hypertension (%) | Hypercholesterolaemia (%) | Diabetes (%) | Previous AMI (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Antoniucci | 2002 | 1164 | Acute MI | Yes | 63 vs 64 | 82 vs 77 | NR | 36 vs 32 | 26 vs 25 | 11 vs 16 | 15 vs 12 |
| Monteiro | 2003 | 70 | Acute MI | Yes | 63.3 vs 65.3 | 89 vs 86 | 46 vs 46 | 57 vs 60 | 43 vs 23 | 17 vs 11 | 37 vs 57 |
| Elsman | 2004 | 1059 | Acute MI | Yes | 59 vs 59 | 83 vs 83 | 48 vs 49 | 25 vs 22 | 21 vs 16 | 5 vs 7 | 13 vs 11 |
| Meier | 2007 | 845 | Elective | Yes | 61 vs 62 | 79 vs 76 | 45 vs 35 | 49 vs 58 | 61 vs 54 | 17 vs 15 | 14 vs 21 |
| Sorajja | 2007 | 318 | Acute MI | Yes | 60 vs 59 | 78.2 vs 8.4 | 41.2 vs 39.2 | 34.5 vs 38.9 | 27.7 vs 25.6 | 15.1 vs 9.5 | 11.8 vs 11.6 |
| Regieli | 2009 | 879 | Elective | Yes | 57 vs 56 | 30 vs 70 | 89 vs 88 | 28 vs 28 | NR | NR | 61 vs 42 |
| Desch | 2010 | 235 | Acute MI | Yes | 64 vs 66 | 74 vs 76 | 46 vs 41 | 65 vs 70 | 84 vs 86 | 33 vs 25 | 14 vs 14 |
| Steg | 2010 | 2173 | Subacute MI | Yes | 57.9 vs 60.4 | 74 vs 80 | 44 vs 26 | 44 vs 57 | 50 vs 52 | 14 vs 30 | 13 vs 14 |
| Ilia | 2011 | 81 | Acute MI | Yes | 54 vs 59 | 35 vs 24 | 20 vs 16 | 16 vs 14 | 24 vs 17 | 10 vs 10 | NR |
Demographics and risk factors are presented for patients with and without coronary collateral circulation, respectively
AMI acute myocardial infarction; MI, myocardial infarction; NR not reported
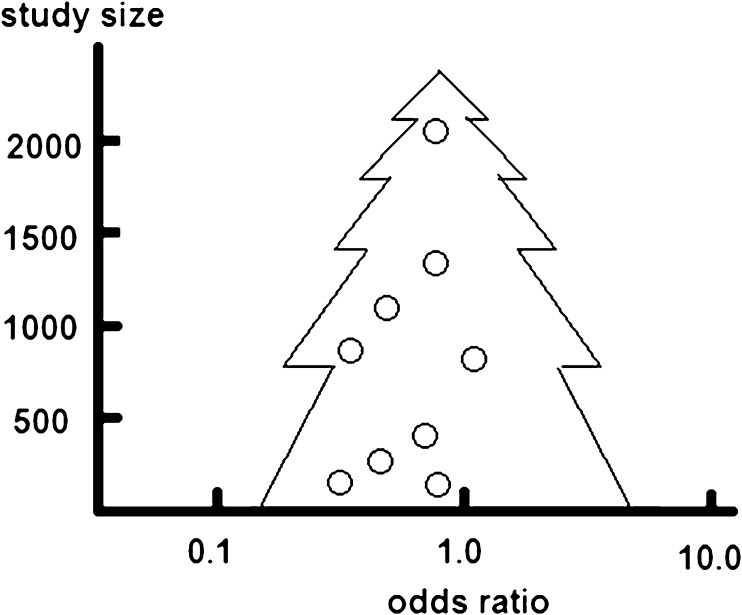
Figure 1 shows a Christmas tree plot: small studies with large odds ratios were not seen. This could mean they are at risk of not being published and, thus, suggests the presence of some publication bias. Table 2 shows that the pooled odds ratio of nine studies equals 0.47, meaning that patients with collaterals have a more than twice reduced risk of dying during a follow-up period of up to 9 years. The validity of this finding is supported by the lack of heterogeneity and an adequate I square value. Table 3 assesses robustness of the above data. After exclusion of two very asymmetric studies the pooled odds ratio is unchanged, indicating that the above meta-analysis is robust against the bias of asymmetry in the given studies.
Fig. 1.
Christmas tree plot. Small studies with large odds ratios are not observed. This could mean they are at risk of not being published, and, thus, suggests the presence of some publication bias
Table 2.
Results of meta-analysis of studies investigating effect of collaterals on mortality
| Study | Odds collaterals | Odds no collaterals | N | Odds ratio | 95 % CI | T-value | P-value |
|---|---|---|---|---|---|---|---|
| 1. Antoniucci 2002 | 11/253 | 81/819 | 1164 | 0.44 | 0.23–0.84 | −2.50 | 0.0125 |
| 2. Monteiro 2003 | 4/31 | 6/29 | 70 | 0.62 | 0.16–2.44 | −0.68 | 0.0497 |
| 3. Elsman 2004 | 3/103 | 45/908 | 1059 | 0.59 | 0.18–1.92 | −0.88 | 0.380 |
| 4. Meier 2007 | 25/201 | 170/416 | 812 | 0.30 | 0.19–0.48 | −5.15 | 0.0001 |
| 5. Sorajja 2007 | 3/116 | 8/191 | 318 | 0.62 | 0.16–2.37 | −0.70 | 0.483 |
| 6. Regieli 2009 | 2/261 | 4/612 | 879 | 1.17 | 0.21–6.44 | +0.18 | 0.855 |
| 7. Desch 2010 | 3/66 | 22/144 | 235 | 0.30 | 0.09–1.03 | −1.92 | 0.056 |
| 8. Steg 2010 | 155/1767 | 28/223 | 2173 | 0.70 | 0.46–1.07 | −1.65 | 0.098 |
| 9. Ilia 2011 | 3/44 | 7/27 | 81 | 0.26 | 0.06–1.10 | −1.83 | 0.068 |
| Pooled odds ratio | 6791 | 0.47 | 0.37–0.61 | −5.90 | 0.0001 |
Heterogeneity chi-square value = 9.1724, 8° of freedom, not significant. I-square value = 12.8 % [< 50 % cut-off for no heterogeneity]
Table 3.
Results of meta-analysis of studies investigating effect of collaterals on mortality after exclusion of studies with >3 asymmetric patient characteristics
| Odds collaterals | Odds no collaterals | N | Odds ratio | 95 % CI | T-value | P-value | |
|---|---|---|---|---|---|---|---|
| 1. Antoniucci 2002 | 11/253 | 81/819 | 1164 | 0.44 | 0.23–0.84 | −2.50 | 0.0125 |
| 2. Monteiro 2003 | 4/31 | 6/29 | 70 | 0.62 | 0.16–2.44 | −0.68 | 0.0497 |
| 3. Elsman 2004 | 3/103 | 45/908 | 1059 | 0.59 | 0.18–1.92 | −0.88 | 0.380 |
| 5. Sorajja 2007 | 3/116 | 8/191 | 318 | 0.62 | 0.16–2.37 | −0.70 | 0.483 |
| 6. Regieli 2009 | 2/261 | 4/612 | 879 | 1.17 | 0.21–6.44 | +0.18 | 0.855 |
| 7. Desch 2010 | 3/66 | 22/144 | 235 | 0.30 | 0.09–1.03 | −1.92 | 0.056 |
| 9. Ilia 2011 | 3/44 | 7/27 | 81 | 0.26 | 0.06–1.10 | −1.83 | 0.068 |
| Pooled odds ratio | 3806 | 0.47 | 0.31–0.72 | −3.50 | 0.0005 |
Heterogeneity chi-square value = 2.3064, 6° of freedom, not significant. I-square value = 0.00 % [< 50 % cut-off for no heterogeneity]
After exclusion of the asymmetric studies, the pooled confidence intervals were wider. The t-value was larger and the p-value smaller, indicating some loss of power due to a smaller sample size left in the meta-analysis, whereas the pooled results were unchanged.
Table 4 shows a meta-analysis with the composite of deaths and re-infarctions as endpoint. The odds ratio of deaths and re-infarctions between those with collaterals versus those without was 0.54. Again heterogeneity according to the fixed effects test and the I-square value was small, although a trend to heterogeneity was observed. After the exclusion of the asymmetric studies the odds ratio rose to 0.60, with no more heterogeneity. This suggests that the asymmetric characteristics may have contributed to a lack of homogeneity, and that it was not entirely robust against this potential flaw. A significant reduction of the composite of deaths and re-infarctions with an odds ratio of 0.60 was observed in the analysis of Table 5, albeit with only four studies left in the meta-analysis.
Table 4.
Results of meta-analysis of studies investigating effect of collaterals on deaths and re-infarctions
| Study | Odds collaterals | Odds no collaterals | N | Odds ratio | 95 % CI | T-value | P-value |
|---|---|---|---|---|---|---|---|
| 1. Monteiro 2003 | 6/29 | 11/24 | 70 | 0.45 | 0.15–1.40 | −1.38 | 0.169 |
| 2. Nathou 2006 | 3/173 | 20/365 | 561 | 0.32 | 0.09–1.08 | −1.84 | 0.066 |
| 3. Meier 2007 | 36/190 | 197/389 | 812 | 0.37 | 0.25–0.56 | −4.87 | 0.0001 |
| 4. Sorajja 2007 | 7/112 | 15/184 | 318 | 0.77 | 0.30–1.94 | −0.56 | 0.576 |
| 5. Regieli 2009 | 7/254 | 16/600 | 879 | 1.03 | 0.42–2.54 | +0.07 | 0.944 |
| 6. Desch 2010 | 5/64 | 34/132 | 235 | 0.30 | 0.11–0.81 | −2.38 | 0.018 |
| 7. Steg 2010 | 246/1676 | 42/209 | 2173 | 0.73 | 0.51–1.04 | −1.72 | 0.085 |
| Pooled odds ratio | 5048 | 0.54 | 0.43–0.68 | −5.22 | 0.0001 |
Heterogeneity chi-square value = 10.7317, 6° of freedom, 0.05 < p < 0.10. I-square value = 44.0 % [<50 % cut-off for no heterogeneity]
Table 5.
Results of meta-analysis of studies investigating effect of collaterals on deaths and re-infarctions after exclusion of studies with >3 asymmetric patient characteristics
| Odds collaterals | Odds no collaterals | N | Odds ratio | 95 % CI | T-value | P-value | |
|---|---|---|---|---|---|---|---|
| 1. Monteiro 2003 | 6/29 | 11/24 | 70 | 0.45 | 0.15–1.40 | −1.38 | 0.169 |
| 4. Sorajja 2007 | 7/112 | 15/184 | 318 | 0.77 | 0.30–1.94 | −0.56 | 0.576 |
| 5. Regieli 2009 | 7/254 | 16/600 | 879 | 1.03 | 0.42–2.54 | +0.07 | 0.944 |
| 6. Desch 2010 | 5/64 | 34/132 | 235 | 0.30 | 0.11–0.81 | −2.38 | 0.017 |
| Pooled odds ratio | 1502 | 0.60 | 0.37–0.98 | −2.03 | 0.043 |
Heterogeneity chi-square value = 3.754, 3° of freedom, ns. I-square value = 20.1 % [<50 % cut-off for no heterogeneity]
Table 6 gives the calculated odds ratios of the presence of traditional atherosclerotic risk factors in the patients with and without collaterals, and their linear relationships with the odds ratios of mortality and deaths plus re-infarctions. No significant relationships were observed. When the composite of deaths and re-infarctions was used similarly, no significant relationships were observed.
Table 6.
Results of meta-regression
| Study | Diabetes | Hypertension | Hypercholesterolaemia | Smoking |
|---|---|---|---|---|
| 1. Monteiro 2003 | 1.61 | 1.12 | 2.56 | 0.93 |
| 2. Elsman 2004 | 0.62 | 1.10 | 1.35 | 0.93 |
| 3. Meier 2004 | 1.13 | 0.69 | 1.33 | 1.85 |
| 4. Nahoe 2006 | 0.76 | 0.85 | 1.34 | 0.78 |
| 5. Sorajja 2007 | 1.69 | 0.83 | 1.11 | 1.09 |
| 6. Regielia 2009 | NR | 1.02 | NR | 1.28 |
| 7. Steg 2010 | 0.13 | 0.17 | 0.21 | 0.27 |
| 8. Desch 2010 | 1.52 | 0.79 | 0.85 | 1.25 |
| 9. Ilia 2011 | 0.65 | 0.74 | 1.04 | 0.83 |
| Meta-regression between odds ratios of risk factors and those of mortality | ||||
| F-value | 0.134 | 0.242 | 0.022 | 0.204 |
| P-value | 0.733 | 0.640 | 0.889 | 0.667 |
| Multiple regression with all of the risk factors tested simultaneously | ||||
| F-value | 0.442 | |||
| P-value | 0.780 | |||
| Meta-regression between odds ratios of risk factors and those of the composite endpoint of deaths and re-infarctions | ||||
| F-value | 0.134 | 0.007 | 0.587 | 0.156 |
| P-value | 0.733 | 0.938 | 0.486 | 0.709 |
| Multiple regression with all of the risk factors tested simultaneously | ||||
| F-value | 0.523 | |||
| P-value | 0.761 | |||
aNo qualitative data of diabetes and cholesterol were reported in this study. Presence of traditional risk factors in patients with collaterals versus those without collaterals in the various studies. Meta-regression between the odds ratios of the traditional risk factors and those of mortality and the composite endpoint ‘deaths and re-infarctions’. NR indicates not reported
Discussion
This meta-analysis of nine studies comprising 6791 patients shows that the coronary collateral circulation is associated with relevantly improved survival and fewer re-infarctions. The studies with major asymmetries in the patient characteristics were partly responsible for some trend to heterogeneity between the studies. However, the meta-analysis showed a significant reduction of mortality by 0.47 (p < 0.0001) and reduction of deaths and re-infarctions by 0.54 (p < 0.0001). These results are, obviously, not in line with the results of the recently published large study by Steg et al.[10] However, the latter study, although adequately powered, did suffer from major asymmetries in the patient characteristics.
The coronary collateral circulation may have a complex role in modifying the risk of cardiovascular morbidity and mortality in ischaemic heart disease. While the protective effect of collaterals may theoretically be reduced with a more extensive burden of ischaemic heart disease, the impact on cardiovascular risk appears to remain present in patients with marked disease [13]. It has been hypothesised based on small observational studies[14] that atherosclerosis may trigger the formation of coronary collaterals. If this is true, then the atherosclerotic risk factors should be more often present in patient with collaterals than in those without. This is, however, not supported by the rather symmetric pattern of patient characteristics in most studies as meta-analysed in the current study [1, 6, 9, 10, 13, 15–19]. To assess this issue in a wider perspective, meta-regression was performed. No significant relationships between the single risk factors and the endpoints were observed, neither tested separately nor tested simultaneously. This does not support the aforementioned trigger hypothesis and supports an overall benefit in patients with collaterals irrespective of their risk factor profile. In this regard, it is of considerable importance to study the clinical benefits of collaterals in balanced studies, and that studies with asymmetric patient characteristics are of a lesser quality for that purpose. However, it must be noted that the main determinant of collateralisation is the degree of coronary stenosis. Unfortunately, however, not all of the incorporated studies in the current meta-analysis reported Rentrop scores or reported on diameter stenosis. For example, Meier et al. [2], Elsman et al. [6] and Sorajja et al. [1] used positive blush grades instead of Rentrop flow grading. Therefore, we were unable to assess Rentrop scores in relation to disease severity.
Although the exact mechanisms underlying the protective effects of the presence of collaterals are unclear, several factors might play a role. The collateral circulation has demonstrated clinical benefit regarding smaller infarct size, preservation of cardiac function after acute (re-) infarctions, and reduction in post-infarct ventricular dilatation [14–22]. Following a total coronary occlusion, residual perfusion to the myocardium persists through native coronary collaterals that open when an intercoronary pressure gradient between the source and recipient vessel develops. In animals, the native collateral flow during occlusion is less than 10 % of the resting flow levels and is insufficient to maintain tissue viability for longer than 20 min. In the absence of coronary collaterals, coronary pressure during balloon angioplasty occlusion falls to similar pressures (10–20 mmHg). There is tremendous individual variability in the function of coronary collaterals among patients with chronic stenoses. Ischaemia does not develop during PCI balloon occlusion when fractional flow reserve (based on coronary wedge pressure during occlusion minus venous pressure) is greater than 0.25 cm [19]. Thus, collaterals sometimes prevent stress-induced ischaemia at submaximal cardiac workloads. Haemodynamic factors may also induce the growth of collaterals [11].
In a recent meta-analysis by Meier et al. [2] a significant advantage of collaterals was established. However, there were several limitations to consider. First, a considerable number of studies from the pre-PCI era were included (earlier than 2000), while currently most Western cardiology departments routinely include the possibility of acute PCI for patients with acute coronary syndrome based on well-defined criteria. In this way the differences created by stenting or balloon angioplasty in haemodynamic conditions may be seen clearly. For long-term follow-up it makes sense to compare patients with both acute and non-acute myocardial infarctions in the presence of coronary collaterals after mechanical reperfusion. Second, as the studies included were heterogeneous, the tests for heterogeneity were consistently positive. Thus, the generalisability of the results was limited. Third, the authors used risk ratios instead of odds ratios in their analyses. In observational studies with relatively common estimators such as collaterals and deaths in patients with CAD, risk ratios are biased estimators of the real relative risks. In this regard, the relative risk underestimates the real risk, and the odds ratio is a better estimator for that purpose, since the numbers of no-deaths is not relevant, but rather the ratio is relevant.
Conclusions
In 6791 CAD patients from the post-PCI era the presence of collaterals may reduce mortality by 0.47 (p < 0.0001) and deaths plus re-infarctions by 0.54 (p < 0.0001).
Many studies in the past were negative due to confounding as a consequence of asymmetric patient characteristics.
In the present meta-data, the atherosclerotic risk factors were no more present in the patients with collaterals than they were in those without.
Acknowledgments
Funding
This article was prepared without external sponsoring.
Conflict of interest
No conflicts of interest.
References
- 1.Sorajja P, Gersh BJ, Mehran R, et al. Impact of collateral flow on myocardial reperfusion and infarct size in patients undergoing primary angioplasty for acute myocardial infarction. Am Heart J. 2007;154(2):379–84. doi: 10.1016/j.ahj.2007.04.034. [DOI] [PubMed] [Google Scholar]
- 2.Meier P, Hemingway H, Lansky AJ, et al. The impact of the coronary collateral circulation on mortality: a meta-analysis. Eur Heart J. 2012;33(5):614–21. doi: 10.1093/eurheartj/ehr308. [DOI] [PubMed] [Google Scholar]
- 3.Bufe A, Haltern G, Dinh W, et al. Recanalisation of coronary chronic total occlusions with new techniques including the retrograde approach via collaterals. Neth Heart J. 2011;19(4):162–7. doi: 10.1007/s12471-011-0091-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rasoul S, Dambrink JH, Breeman A, et al. The relation between myocardial blush grade and myocardial contrast echocardiography: which one is a better predictor of myocardial damage? Neth Heart J. 2010;18(1):25–30. [PMC free article] [PubMed] [Google Scholar]
- 5.Scholzel BE, Endeman H, Dewilde W, et al. Cardiac surgery in a patient with essential thrombocythemia: a case report. Neth Heart J. 2010;18(7–8):378–80. doi: 10.1007/BF03091797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elsman P, van ’t Hof AW, de Boer MJ, et al. Role of collateral circulation in the acute phase of ST-segment-elevation myocardial infarction treated with primary coronary intervention. Eur Heart J. 2004;25(10):854–8. doi: 10.1016/j.ehj.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Yoon SJ, Ko YG, Kim JS, et al. Impact of coronary artery collaterals on infarct size assessed by serial cardiac magnetic resonance imaging after primary percutaneous coronary intervention in patients with acute myocardial infarction. Coron Artery Dis. 2009;20(7):440–5. doi: 10.1097/MCA.0b013e328330c930. [DOI] [PubMed] [Google Scholar]
- 8.Albertal M, Cura F, Escudero AG, et al. Relationship between collateral circulation and successful myocardial reperfusion in acute myocardial infarction: a subanalysis of the PREMIAR trial. Angiology. 2008;59(5):587–92. doi: 10.1177/0003319707308725. [DOI] [PubMed] [Google Scholar]
- 9.Ilia R, Wolak A, Amit G, et al. Collateral blood flow can predict myocardial blush grade in primary coronary intervention. Catheter Cardiovasc Interv. 2012;80(1):67–70. doi: 10.1002/ccd.23169. [DOI] [PubMed] [Google Scholar]
- 10.Steg PG, Kerner A, Mancini GB, et al. Impact of collateral flow to the occluded infarct-related artery on clinical outcomes in patients with recent myocardial infarction: a report from the randomized occluded artery trial. Circulation. 2010;121(25):2724–30. doi: 10.1161/CIRCULATIONAHA.109.933200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cleophas TJ, Zwinderman AH. Meta-analysis. Circulation. 2007;115(22):2870–5. doi: 10.1161/CIRCULATIONAHA.105.594960. [DOI] [PubMed] [Google Scholar]
- 12.Thompson S. Why source of heterogeneity should be investigated. Systematic reviews London: BMJ Publishing Group, London, UK; 1995. p. 48-63.
- 13.Regieli JJ, Jukema JW, Nathoe HM, et al. Coronary collaterals improve prognosis in patients with ischemic heart disease. Int J Cardiol. 2009;132(2):257–62. doi: 10.1016/j.ijcard.2007.11.100. [DOI] [PubMed] [Google Scholar]
- 14.Turgut O, Yilmaz MB, Yalta K, et al. Prognostic relevance of coronary collateral circulation: clinical and epidemiological implications. Int J Cardiol. 2009;137(3):300–1. doi: 10.1016/j.ijcard.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 15.Desch S, de Waha S, Eitel I, et al. Effect of coronary collaterals on long-term prognosis in patients undergoing primary angioplasty for acute ST-elevation myocardial infarction. Am J Cardiol. 2010;106(5):605–11. doi: 10.1016/j.amjcard.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Nathoe HM, Koerselman J, Buskens E, et al. Determinants and prognostic significance of collaterals in patients undergoing coronary revascularization. Am J Cardiol. 2006;98(1):31–5. doi: 10.1016/j.amjcard.2006.01.050. [DOI] [PubMed] [Google Scholar]
- 17.Meier P, Gloekler S, Zbinden R, et al. Beneficial effect of recruitable collaterals: a 10-year follow-up study in patients with stable coronary artery disease undergoing quantitative collateral measurements. Circulation. 2007;116(9):975–83. doi: 10.1161/CIRCULATIONAHA.107.703959. [DOI] [PubMed] [Google Scholar]
- 18.Antoniucci D, Valenti R, Moschi G, et al. Relation between preintervention angiographic evidence of coronary collateral circulation and clinical and angiographic outcomes after primary angioplasty or stenting for acute myocardial infarction. Am J Cardiol. 2002;89(2):121–5. doi: 10.1016/S0002-9149(01)02186-5. [DOI] [PubMed] [Google Scholar]
- 19.Monteiro P, Antunes A, Goncalves LM, et al. Long-term clinical impact of coronary-collateral vessels after acute myocardial infarction. Rev Port Cardiol. 2003;22(9):1051–61. [PubMed] [Google Scholar]
- 20.Berry C, Balachandran KP, L’Allier PL, et al. Importance of collateral circulation in coronary heart disease. Eur Heart J. 2007;28(3):278–91. doi: 10.1093/eurheartj/ehl446. [DOI] [PubMed] [Google Scholar]
- 21.Seiler C. Collective prognostic relevance. Collateral Circulation of the Heart. London: Springer; 2009.
- 22.Kern MJ, Lerman A, Bech JW, et al. Physiological assessment of coronary artery disease in the cardiac catheterization laboratory: a scientific statement from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Circulation. 2006;114(12):1321–41. doi: 10.1161/CIRCULATIONAHA.106.177276. [DOI] [PubMed] [Google Scholar]