Abstract
Objectives To review the characteristic symptoms of superior semicircular canal dehiscence, testing and imaging of the disease, and the current treatment and surgical options.
Results and Conclusions Symptoms of superior semicircular canal dehiscence (SSCD) include autophony, inner ear conductive hearing loss, Hennebert sign, and sound-induced episodic vertigo and disequilibrium (Tullio phenomenon), among others. Potential etiologies noted for canal dehiscence include possible developmental abnormalities, congenital defects, chronic otitis media with cholesteatoma, fibrous dysplasia, and high-riding jugular bulb. Computed tomography (CT), vestibular evoked myogenic potentials, Valsalva maneuvers, and certain auditory testing may prove useful in the detection and evaluation of dehiscence syndrome. Multislice temporal bone CT examinations are normally performed with fine-cut (0.5- to 0.6-mm) collimation reformatted to the plane of the superior canal such that images are parallel and orthogonal to the plane. For the successful alleviation of auditory and vestibular symptoms, a bony dehiscence can be surgically resurfaced, plugged, or capped through a middle fossa craniotomy or the transmastoid approach. SSCD should only be surgically treated in patients who exhibit clinical manifestations.
Keywords: superior semicircular canal dehiscence syndrome, vertigo, hearing loss, autophony, Tullio phenomenon
Introduction
Vestibular and cochlear symptoms resulting from the communication of the inner ear and its neighboring structures can be caused by semicircular canal dehiscence.1 The dense otic capsule bone, which encases the inner ear, normally has two mobile windows, but an acquired dehiscence in the superior, posterior, or lateral canal may create a “third mobile window” in the inner ear that triggers a variety of symptoms.1,2,3,4,5
A syndrome of vertigo and other vestibular dysfunction due to the thinning or absence of bone overlying the superior semicircular canal has recently been identified.1,3,4,6,7 Superior semicircular canal dehiscence (SSCD) syndrome (SSCDS), which is more clinically common than the lateral or posterior forms,1 was described first by Minor et al in 1998.2,6 The middle fossa and superior semicircular canal communicate abnormally in patients with SSCD, resulting in abnormal vestibular function that is sensitive to bone-transmitted sound and intracranial pressure changes.2 This leads to the “third window effect,” which is characterized by acoustic energy loss and the abnormal stimulation of the vestibular system.2,3,4,5 These physiological effects have been understood more thoroughly through animal models.1,3,8
Symptoms of SSCD include inner ear conductive hearing loss,1,3,5,7 the Hennebert sign, and sound-induced episodic vertigo and disequilibrium (Tullio phenomenon).1,2 Unprovoked drop attacks that were improved after repair of SSCD have also been reported.9,10 Notably, a common clinical manifestation in SSCD patients is the abnormal amplification of certain internal sounds of the body, such as self-generated sounds like the heartbeat and eye movement.9 If an SSCD exists close to the cerebrospinal fluid (CSF) space, the abnormal opening into the inner ear results in the abnormal perception of these sounds.9,11,12
Using asymptomatic subjects, Carey et al found a 0.7% incidence of SSCD in a collection of randomly selected temporal bones from 596 cadavers.13,14 Most people reach middle age by the time they present with any clinical manifestations of SSCDS.3,9,15,16 However, the condition has also been described in the pediatric population.17 Patients with SSCD have been known to experience auditory or vestibular symptoms, which can present together or individually.1 Physiologically, the basis of why signs and symptoms vary between patients with SSCD is not yet fully understood.3,5,7,18 Elements contributing to the differences in vestibular and auditory manifestations may include patency of the cochlear aqueduct and the relative compliance of the round window membrane.3 Oscillopsia and sound or pressure-induced vertigo triggering eye movement in the plane of the superior canal resulted in Minor's initial identification of SSCDS.3 A recent study using temporal bone CT scans found that patients with dehiscence greater than or equal to 2.5 mm mainly experienced both auditory and vestibular abnormalities.1,19
Potential etiologies noted for canal dehiscence include developmental abnormalities, congenital defects, chronic otitis media with cholesteatoma, fibrous dysplasia, or a high-riding jugular bulb.1 Yet the cause of SSCD remains unclear in the majority of cases.20 A possible genetic factor has been suggested due to the reported cases of affected siblings.7,21,22,23,24 Moreover, the onset of SSCDS rarely occurs before age 20, beginning instead at an average age of 43 years.1,23
Also, because SSCDS is bilateral in about one third of cases and CT studies have shown that the overlying bone of the contralateral superior canal is unusually thin in cases of unilateral superior canal dehiscence, an underlying developmental or congenital cause has been implicated for the syndrome.1,22,25 It is possible that the prematurely arrested development of the bone overlying the superior canal, a bone that develops from birth until 3 years of age, may cause SSCDS.1 However, the existence of pressure transmission through a dehiscence is also necessary for the presentation of the clinical syndrome, and such transmission may be dependent upon thin bone or inelastic dura residing at the floor of the middle fossa.1
Therefore, it follows that signs of SSCDS may not appear until adulthood despite an existing congenital thinning or defect. Pressure from the overlying temporal bone or dura may erode congenitally thin bone with the passage of time, and trauma may also disturb the abnormally thin bone layer.1 Such patients may not experience any typical symptoms of SSCDS beforehand.1 Moreover, a patient with completely absent bone could experience no symptoms until the dura is elastic enough for pressure between the middle fossa and inner ear to be transmitted.1
However, contrary to implications of a congenital basis for SSCD syndrome, Nadgir et al concluded in 2011 that, after a review of 306 consecutive temporal bone CT examinations, SSCD seems to be more commonly acquired instead of due to a congenital abnormality.26 Their results demonstrated that the prevalence of dehiscence increased with increasing age and that this relationship was statistically significant.26
Testing and Imaging
CT, vestibular evoked myogenic potentials, Valsalva maneuvers, and certain auditory testing may prove useful in the detection and evaluation of dehiscence syndrome. It is not likely that vestibular assessments conducted routinely, including electronystagmography, rotary chair examination, and calorimetry, would be beneficial in discovering any existing abnormalities in patients with dehiscences.13,23
CT Scans
High-resolution CT scans of the temporal bone provides one of the most important confirmations of SSCDS, and they remain crucial for locating dehiscences prior to treatment (Fig. 1).9 Multislice temporal bone CT examinations are normally performed with fine-cut (0.5- to 0.6-mm) collimation reformatted to the plane of the superior canal such that images are parallel (Poschl's view) and orthogonal (Stenver's view) to the plane (Figs. 2 and 3).1,27 Note that partial volume averaging results in a high number of false-positives for conventional CT scans of 1.0-mm collimation when used for SSCD identification.1 Reformatting to the canal plane and the 0.5-mm collimation improves specificity and positive predictive value.1,3,28,29
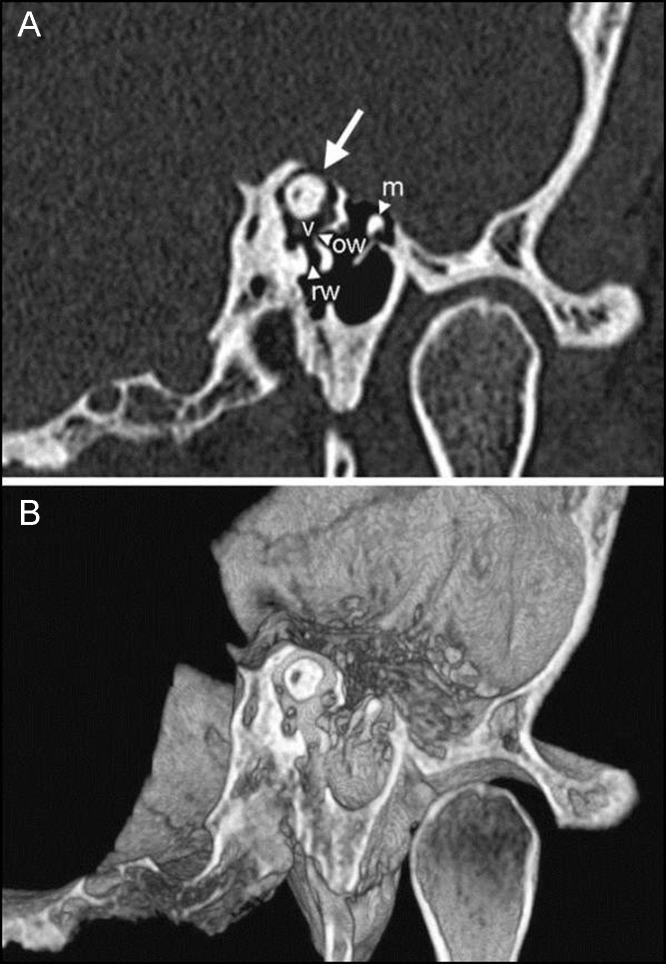
Figure 1.

Coronal view of a patient with a high-resolution computed tomography scan and an arrow pointing to the superior semicircular canal dehiscence.
Figure 2.
The computed tomography scan reconstructions of a 39-year-old male patient with left-sided superior semicircular canal dehiscence who, along with experiencing other symptoms, could hear his heartbeat in the left ear and experienced oscillopsia after coughing, sneezing, or hearing loud noises in the affected ear. The scans pass through the plane of the left superior canal and are in two and three dimensions for images A and B, respectively. The white arrow indicates the dehiscence of the superior canal into the middle cranial fossa. (m, malleus head; ow, oval window; rw, round window; v, vestibule) (Reprinted with permission from Minor LB. Clinical manifestations of superior semicircular canal dehiscence. The Laryngoscope 2005;115:1717–1727.)
Figure 3.
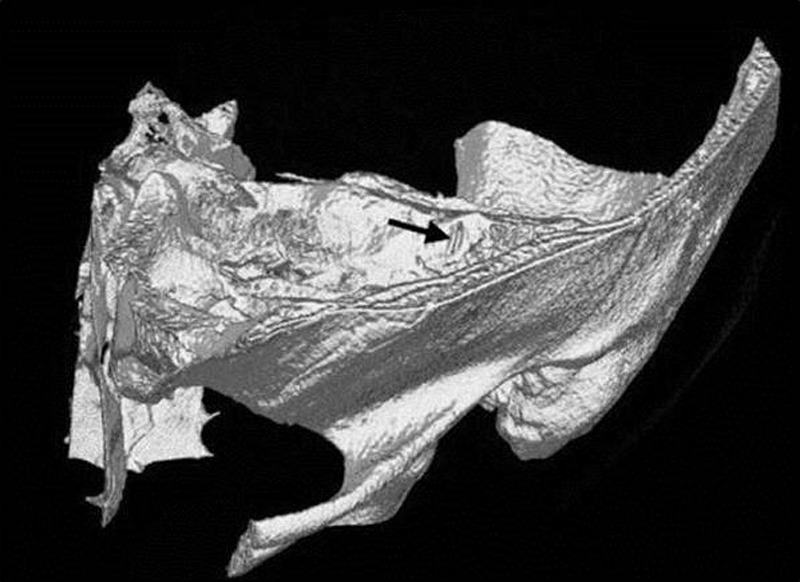
The arrow indicates the dehiscence observed in this computed tomography image from reconstructions in the plane of the left superior canal. The patient is the 39-year-old male described in Fig. 2. (Reprinted with permission from Minor LB. Clinical manifestations of superior semicircular canal dehiscence. The Laryngoscope 2005;115:1717–1727.)
However, significant differences have been found between pathologically detected versus CT-detected SSCD.9,29,30,31,32,33,34 Stimmer et al analyzed 700 high-resolution multislice CT exams and compared them to existing histologic studies, which showed a substantial risk of SSCD overestimation.9 The CT scans (Fig. 4) showed SSCD in 8% of the 700 temporal bone exams,9 whereas histologic exams performed on a greater number of bones showed SSCD in only 0.5 to 0.6%.15,29,34 Stimmer et al also noted that even the latest high-resolution CT technology might be unable to detect slight labyrinthine structures covered by thin tissue. Furthermore, clinical CT scans may overestimate superior canal dehiscence size as a result of the partial volume effect.27,28,34,35
Figure 4.
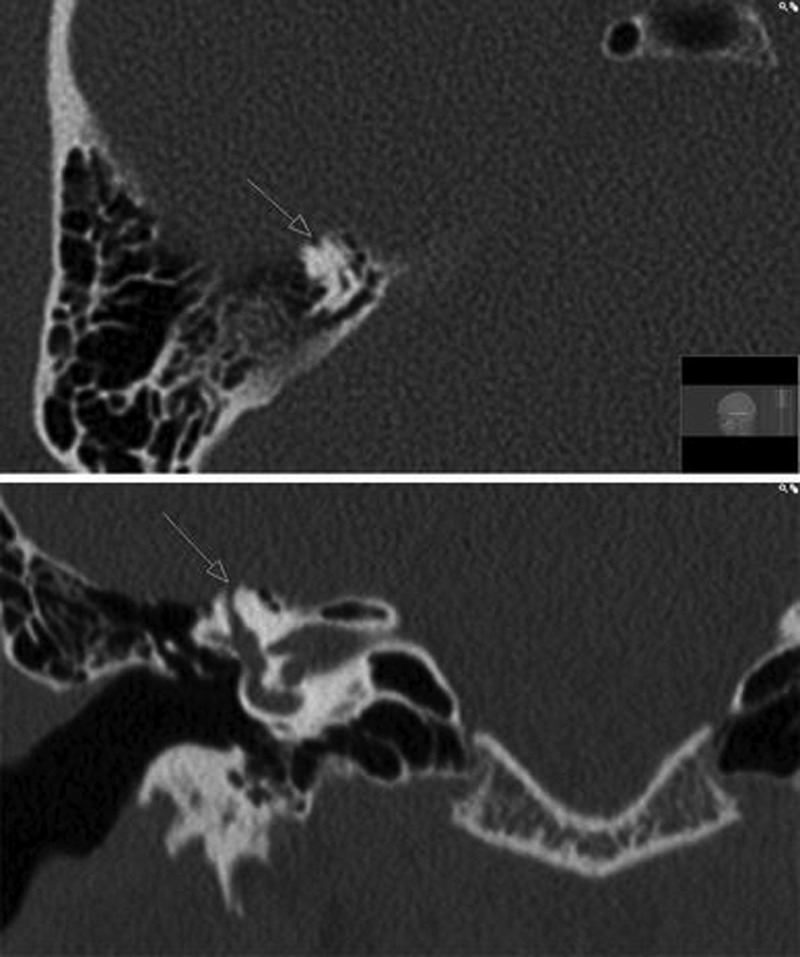
Computed tomography scan of a superior semicircular canal dehiscence in the right ear. The axial view is displayed above the coronal view. (Reprinted with permission from Stimmer H, Hamann KF, Zeiter S, Naumann A, Rummeny EJ. Semicircular canal dehiscence in HR multislice computed tomography: distribution, frequency, and clinical relevance. Eur Arch Otorhinolaryngol 2012;269:475–480.)
Although a 4% prevalence of SSCD was found in 581 temporal bone CT scans,27,34 a 0.5% prevalence was observed in a study of 1000 bones assessed for SSCD histologically.14,27 Sequeira et al reported that smaller dehiscences tend to be overestimated by clinical CT scans, especially when the SSCD is under 3 mm. Thus, in cases of small SSCD, no dehiscence may be found despite radiographic evidence to the contrary. Moreover, clinical CT scans reformatted orthogonally to the canal plane were found to falsely demonstrate dehiscence more often in thin bone than CT images reformatted parallel to the plane.27 As a result, conducting clinical and neurophysiological testing may be necessary to corroborate radiographic findings.9,27
Vestibular-Evoked Myogenic Potential Testing
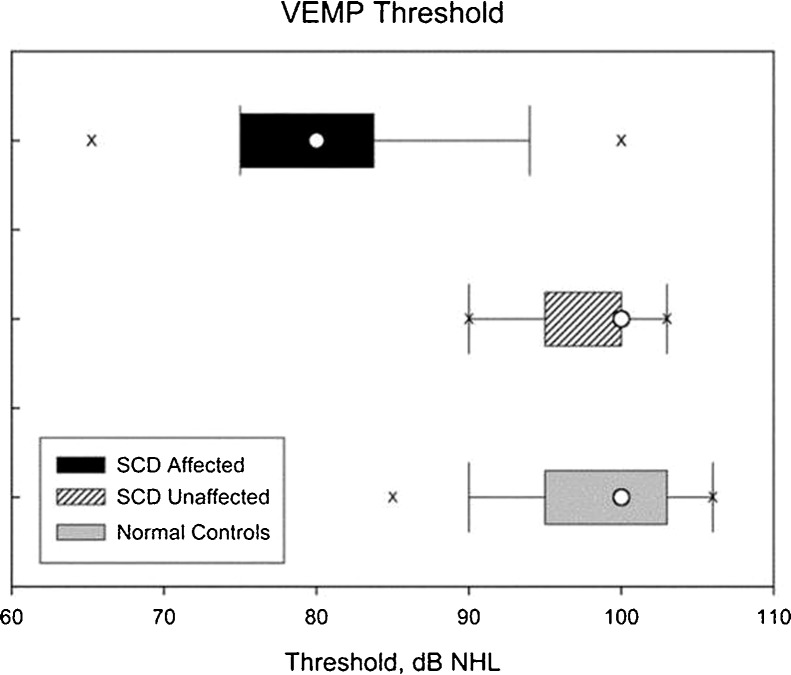
Vestibular-evoked myogenic potential (VEMP) responses have been a useful assessment technique for confirming the suspected presence of SSCD1,3,24,36,37,38 because patients with the syndrome have reduced thresholds for VEMP response in the affected ear for both air and bone conduction1,2,24,36,37,38,39 as well as larger VEMP amplitudes2,24,36 with 80% sensitivity and specificity.2,40 In testing 141 ears, Minor found that though there was no difference between VEMP thresholds of normal ears or unaffected ears in patients with SSCD on the contralateral side, thresholds in ears affected with SSCDS were significantly different from those of control ears and of unaffected ears (Fig. 5).3
Figure 5.
Thresholds for vestibular-evoked myogenic potential response elicitation were recorded in 141 ears: 51 ears affected by superior semicircular canal dehiscence (SSCD), 30 normal ears in patients with SSCD in the contralateral ear, and 60 unaffected ears as controls. The boxes for these three groups represent the interquartile range, which spans from the 25th to 75th percentile. The whiskers represent the 10th to 90th percentile range, and the two lowercase Xs signify the 5th and 95th percentile range. The median threshold is indicated by the white circle. (Reprinted with permission from Minor LB. Clinical manifestations of superior semicircular canal dehiscence. The Laryngoscope 2005;115:1717–1727.)
In ocular VEMPs, surface electrodes placed below the eye record excitatory responses to clicks or tone bursts, whereas cervical VEMPs record the same responses from surface electrodes placed over the ipsilateral sternocleidomastoid muscle as it tonically contracts.1,41,42
Because VEMP responses vanish after vestibular neurectomy yet remain in deaf patients with conserved vestibular function, these responses are thought to be vestibular in origin.3,41,43,44 The hypothesis that VEMP responses originate from the saccule has also been supported,3,45,46 and the inferior vestibular nerve has been implicated in the responses as well.3,47
Moreover, VEMP testing responses are particularly useful in determining whether a patient presenting with conductive hearing loss has a dehiscence or true ossicular disease.48 Instead of the typically lowered threshold due to dehiscence, VEMP testing responses are either absent or show elevated thresholds in cases of ossicular disease.48
Audiometric Manifestations and Testing
For patients experiencing auditory manifestations of SSCD, which can occur without vestibular signs and symptoms, the Weber tuning fork test usually lateralizes to the affected ear.1,3 Moreover, such patients may be capable of hearing a tuning fork placed on the lateral malleolus of the foot.1,3,36 Acoustic effects include a greater than normal sensitivity to bone-conducted sound and autophony. Minor noted the importance of recognizing these effects in the context of superior canal dehiscence to avoid attributing them to a middle ear abnormality.3
Treatment and Surgical Approaches
Conservative treatment for superior canal dehiscence best benefits patients with mild or no symptoms2; it may even be sufficient for patients to simply avoid symptom triggers.3 For patients enduring primarily pressure-induced symptoms, placing a tympanostomy tube may be advantageous but is highly variable in its efficacy.1
For the successful alleviation of auditory and vestibular symptoms, a bony dehiscence can be surgically resurfaced, plugged, or capped.1,2,5,6,23,49,50 SSCD should only be surgically treated in patients who exhibit clinical manifestations.3
In such cases, the two main methods include the transmastoid approach or a middle fossa craniotomy.2 The middle fossa approach has also been reported to be effective in alleviating debilitating vestibular issues1,6,23,24,51 and provides the advantage of direct visualization of the bony dehiscence. In the transmastoid approach, a low-lying tegmen can limit access to the dehiscence.3 In addition, the existence of a dehiscence cannot be visually identified and confirmed while using the transmastoid approach.1 Nevertheless, the transmastoid approach is more familiar to most otologists and confers a slightly lower risk of CSF leak and intracranial complications.2
Both plugging and resurfacing for cases of SCCD have reported benefits and disadvantages. Plugging the canal lumen with bone wax or fascia and bone dust stops endolymph flow, whereas resurfacing halts any communication between the brain and labyrinth by covering the dehiscence with native tissue.2 Although plugging of dehiscences can be performed via the middle fossa2,7,23,52,53 or transmastoid approach,2,51 resurfacing requires a middle fossa approach.2 However, the vestibular and cochlear structures are more likely to be harmed by plugging through a transmastoid approach, which presents a greater risk of causing permanent hearing loss.2,54 Plugging of the semicircular canal also carries a small risk of global vestibular hypofunction and a risk of sensorineural hearing loss, the latter of which developed in one of two patients described by Brantberg et al who underwent transmastoid superior canal occlusion.2,24 Middle cranial fossa resurfacing does require retraction of the temporal lobe and carries a slightly higher risk of seizure than the transmastoid approach.2
Conclusion
Described first in 1998, SSCDS is a relatively new and unexamined syndrome of the inner ear. Its identification normally depends on CT, VEMP testing, Valsalva maneuvers, auditory testing, and the presentation of symptoms such as autophony and oscillopsia. Treating the dehiscence in its more severe forms may require surgical resurfacing, plugging, or capping, whereas the milder cases with no clinical manifestations should be managed conservatively.
Acknowledgments
Marko Spasic (third author) was partially supported by an American Association of Neurological Surgeons Fellowship and by an Alpha Omega Alpha Carolyn L. Kuckein Student Research Fellowship. Isaac Yang (senior author) was partially supported by an Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research UCLA Scholars in Translational Medicine Program Award, Visionary Fund Grant, the Stein Oppenheimer Endowment Award, and the STOP Cancer Jason Dessel Memorial Seed Grant.
References
- 1.Chien W W, Carey J P, Minor L B. Canal dehiscence. Curr Opin Neurol. 2011;24:25–31. doi: 10.1097/WCO.0b013e328341ef88. [DOI] [PubMed] [Google Scholar]
- 2.Amoodi H A, Makki F M, McNeil M, Bance M. Transmastoid resurfacing of superior semicircular canal dehiscence. Laryngoscope. 2011;121:1117–1123. doi: 10.1002/lary.21398. [DOI] [PubMed] [Google Scholar]
- 3.Minor L B. Clinical manifestations of superior semicircular canal dehiscence. Laryngoscope. 2005;115:1717–1727. doi: 10.1097/01.mlg.0000178324.55729.b7. [DOI] [PubMed] [Google Scholar]
- 4.Friedland D R, Michel M A. Cranial thickness in superior canal dehiscence syndrome: implications for canal resurfacing surgery. Otol Neurotol. 2006;27:346–354. doi: 10.1097/00129492-200604000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Minor L B, Carey J P, Cremer P D, Lustig L R, Streubel S O, Ruckenstein M J. Dehiscence of bone overlying the superior canal as a cause of apparent conductive hearing loss. Otol Neurotol. 2003;24:270–278. doi: 10.1097/00129492-200303000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Minor L B, Solomon D, Zinreich J S, Zee D S. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Head Neck Surg. 1998;124:249–258. doi: 10.1001/archotol.124.3.249. [DOI] [PubMed] [Google Scholar]
- 7.Mikulec A A, McKenna M J, Ramsey M J. et al. Superior semicircular canal dehiscence presenting as conductive hearing loss without vertigo. Otol Neurotol. 2004;25:121–129. doi: 10.1097/00129492-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Hirvonen T P, Carey J P, Liang C J, Minor L B. Superior canal dehiscence: mechanisms of pressure sensitivity in a chinchilla model. Arch Otolaryngol Head Neck Surg. 2001;127:1331–1336. doi: 10.1001/archotol.127.11.1331. [DOI] [PubMed] [Google Scholar]
- 9.Stimmer H, Hamann K F, Zeiter S, Naumann A, Rummeny E J. Semicircular canal dehiscence in HR multislice computed tomography: distribution, frequency, and clinical relevance. Eur Arch Otorhinolaryngol. 2012;269:475–480. doi: 10.1007/s00405-011-1688-6. [DOI] [PubMed] [Google Scholar]
- 10.Brantberg K, Ishiyama A, Baloh R W. Drop attacks secondary to superior canal dehiscence syndrome. Neurology. 2005;64:2126–2128. doi: 10.1212/01.WNL.0000165953.48914.B0. [DOI] [PubMed] [Google Scholar]
- 11.Songer J E, Rosowski J J. The effect of superior canal dehiscence on cochlear potential in response to air-conducted stimuli in chinchilla. Hear Res. 2005;210:53–62. doi: 10.1016/j.heares.2005.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmuziger N, Allum J, Buitrago-Téllez C, Probst R. Incapacitating hypersensitivity to one's own body sounds due to a dehiscence of bone overlying the superior semicircular canal. A case report. Eur Arch Otorhinolaryngol. 2006;263:69–74. doi: 10.1007/s00405-005-0939-9. [DOI] [PubMed] [Google Scholar]
- 13.Krombach G A, DiMartino E, Schmitz-Rode T. et al. Posterior semicircular canal dehiscence: a morphologic cause of vertigo similar to superior semicircular canal dehiscence. Eur Radiol. 2003;13:1444–1450. doi: 10.1007/s00330-003-1828-5. [DOI] [PubMed] [Google Scholar]
- 14.Carey J P, Minor L B, Nager G T. Dehiscence or thinning of bone overlying the superior semicircular canal in a temporal bone survey. Arch Otolaryngol Head Neck Surg. 2000;126:137–147. doi: 10.1001/archotol.126.2.137. [DOI] [PubMed] [Google Scholar]
- 15.Strupp M, Eggert T, Straube A, Jäger L, Querner V, Brandt T. [“Inner perilymph fistula” of the anterior semicircular canal. A new disease picture with recurrent attacks of vertigo] Nervenarzt. 2000;71:138–142. doi: 10.1007/s001150050021. [DOI] [PubMed] [Google Scholar]
- 16.Zhou G, Gopen Q, Poe D S. Clinical and diagnostic characterization of canal dehiscence syndrome: a great otologic mimicker. Otol Neurotol. 2007;28:920–926. [PubMed] [Google Scholar]
- 17.Lee G S, Zhou G, Poe D. et al. Clinical experience in diagnosis and management of superior semicircular canal dehiscence in children. Laryngoscope. 2011;121:2256–2261. doi: 10.1002/lary.22134. [DOI] [PubMed] [Google Scholar]
- 18.Rosowski J J, Songer J E, Nakajima H H, Brinsko K M, Merchant S N. Clinical, experimental, and theoretical investigations of the effect of superior semicircular canal dehiscence on hearing mechanisms. Otol Neurotol. 2004;25:323–332. doi: 10.1097/00129492-200405000-00021. [DOI] [PubMed] [Google Scholar]
- 19.Pfammatter A, Darrouzet V, Gärtner M. et al. A superior semicircular canal dehiscence syndrome multicenter study: is there an association between size and symptoms? Otol Neurotol. 2010;31:447–454. doi: 10.1097/MAO.0b013e3181d27740. [DOI] [PubMed] [Google Scholar]
- 20.Crane B T, Carey J P, McMenomey S, Minor L B. Meningioma causing superior canal dehiscence syndrome. Otol Neurotol. 2010;31:1009–1010. doi: 10.1097/MAO.0b013e3181a32d85. [DOI] [PubMed] [Google Scholar]
- 21.da Cunha Ferreira S, de Melo Tavares de Lima M A. Superior Canal Dehiscence Syndrome. Braz J Otorhinolaryngol. 2006;72:414–418. doi: 10.1016/S1808-8694(15)30978-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Minor L B, Cremer P D, Carey J P, Della Santina C C, Streubel S O, Weg N. Symptoms and signs in superior canal dehiscence syndrome. Ann N Y Acad Sci. 2001;942:259–273. doi: 10.1111/j.1749-6632.2001.tb03751.x. [DOI] [PubMed] [Google Scholar]
- 23.Minor L B. Superior canal dehiscence syndrome. Am J Otol. 2000;21:9–19. [PubMed] [Google Scholar]
- 24.Brantberg K, Bergenius J, Tribukait A. Vestibular-evoked myogenic potentials in patients with dehiscence of the superior semicircular canal. Acta Otolaryngol. 1999;119:633–640. doi: 10.1080/00016489950180559. [DOI] [PubMed] [Google Scholar]
- 25.Cremer P D, Minor L B, Carey J P, Della Santina C C. Eye movements in patients with superior canal dehiscence syndrome align with the abnormal canal. Neurology. 2000;55:1833–1841. doi: 10.1212/wnl.55.12.1833. [DOI] [PubMed] [Google Scholar]
- 26.Nadgir R N, Ozonoff A, Devaiah A K, Halderman A A, Sakai O. Superior semicircular canal dehiscence: congenital or acquired condition? AJNR Am J Neuroradiol. 2011;32:947–949. doi: 10.3174/ajnr.A2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sequeira S M, Whiting B R, Shimony J S, Vo K D, Hullar T E. Accuracy of computed tomography detection of superior canal dehiscence. Otol Neurotol. 2011;32:1500–1505. doi: 10.1097/MAO.0b013e318238280c. [DOI] [PubMed] [Google Scholar]
- 28.Belden C J, Weg N, Minor L B, Zinreich S J. CT evaluation of bone dehiscence of the superior semicircular canal as a cause of sound- and/or pressure-induced vertigo. Radiology. 2003;226:337–343. doi: 10.1148/radiol.2262010897. [DOI] [PubMed] [Google Scholar]
- 29.Williamson R A, Vrabec J T, Coker N J, Sandlin M. Coronal computed tomography prevalence of superior semicircular canal dehiscence. Otolaryngol Head Neck Surg. 2003;129:481–489. doi: 10.1016/S0194-59980301391-3. [DOI] [PubMed] [Google Scholar]
- 30.Piton J, Négrevergne M, Portmann D. [Dehiscence of the superior semicircular canal: approach and CT scan classifications] Rev Laryngol Otol Rhinol (Bord) 2008;129:17–26. [PubMed] [Google Scholar]
- 31.Chen E Y, Paladin A, Phillips G. et al. Semicircular canal dehiscence in the pediatric population. Int J Pediatr Otorhinolaryngol. 2009;73:321–327. doi: 10.1016/j.ijporl.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 32.Crovetto M, Whyte J, Rodriguez O M, Lecumberri I, Martinez C, Eléxpuru J. Anatomo-radiological study of the Superior Semicircular Canal Dehiscence Radiological considerations of Superior and Posterior Semicircular Canals. Eur J Radiol. 2010;76:167–172. doi: 10.1016/j.ejrad.2009.05.038. [DOI] [PubMed] [Google Scholar]
- 33.Calli C, Pinar E, Oncel S, Erdoğan N, Sadullahoğlu K. [Evaluation of superior semicircular canal dehiscence in patients with vertigo and tinnitus] Kulak Burun Bogaz Ihtis Derg. 2009;19:77–81. [PubMed] [Google Scholar]
- 34.Cloutier J F, Bélair M, Saliba I. Superior semicircular canal dehiscence: positive predictive value of high-resolution CT scanning. Eur Arch Otorhinolaryngol. 2008;265:1455–1460. doi: 10.1007/s00405-008-0672-2. [DOI] [PubMed] [Google Scholar]
- 35.Curtin H D. Superior semicircular canal dehiscence syndrome and multi-detector row CT. Radiology. 2003;226:312–314. doi: 10.1148/radiol.2262021327. [DOI] [PubMed] [Google Scholar]
- 36.Watson S R, Halmagyi G M, Colebatch J G. Vestibular hypersensitivity to sound (Tullio phenomenon): structural and functional assessment. Neurology. 2000;54:722–728. doi: 10.1212/wnl.54.3.722. [DOI] [PubMed] [Google Scholar]
- 37.Streubel S O, Cremer P D, Carey J P, Weg N, Minor L B. Vestibular-evoked myogenic potentials in the diagnosis of superior canal dehiscence syndrome. Acta Otolaryngol Suppl. 2001;545:41–49. doi: 10.1080/000164801750388090. [DOI] [PubMed] [Google Scholar]
- 38.Welgampola M S, Myrie O A, Minor L B, Carey J P. Vestibular-evoked myogenic potential thresholds normalize on plugging superior canal dehiscence. Neurology. 2008;70:464–472. doi: 10.1212/01.wnl.0000299084.76250.4a. [DOI] [PubMed] [Google Scholar]
- 39.Aw S T, Todd M J, Aw G E, Magnussen J S, Curthoys I S, Halmagyi G M. Click-evoked vestibulo-ocular reflex: stimulus-response properties in superior canal dehiscence. Neurology. 2006;66:1079–1087. doi: 10.1212/01.wnl.0000204445.81884.c7. [DOI] [PubMed] [Google Scholar]
- 40.Crane B T, Minor L B, Carey J P. Three-dimensional computed tomography of superior canal dehiscence syndrome. Otol Neurotol. 2008;29:699–705. doi: 10.1097/MAO.0b013e3181776726. [DOI] [PubMed] [Google Scholar]
- 41.Colebatch J G, Halmagyi G M, Skuse N F. Myogenic potentials generated by a click-evoked vestibulocollic reflex. J Neurol Neurosurg Psychiatry. 1994;57:190–197. doi: 10.1136/jnnp.57.2.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ferber-Viart C, Dubreuil C, Duclaux R. Vestibular evoked myogenic potentials in humans: a review. Acta Otolaryngol. 1999;119:6–15. doi: 10.1080/00016489950181864. [DOI] [PubMed] [Google Scholar]
- 43.Colebatch J G, Halmagyi G M. Vestibular evoked potentials in human neck muscles before and after unilateral vestibular deafferentation. Neurology. 1992;42:1635–1636. doi: 10.1212/wnl.42.8.1635. [DOI] [PubMed] [Google Scholar]
- 44.Ozeki H, Matsuzaki M, Murofushi T. Vestibular evoked myogenic potentials in patients with bilateral profound hearing loss. ORL J Otorhinolaryngol Relat Spec. 1999;61:80–83. doi: 10.1159/000027646. [DOI] [PubMed] [Google Scholar]
- 45.Murofushi T, Curthoys I S, Gilchrist D P. Response of guinea pig vestibular nucleus neurons to clicks. Exp Brain Res. 1996;111:149–152. doi: 10.1007/BF00229565. [DOI] [PubMed] [Google Scholar]
- 46.Didier A, Cazals Y. Acoustic responses recorded from the saccular bundle on the eighth nerve of the guinea pig. Hear Res. 1989;37:123–127. doi: 10.1016/0378-5955(89)90034-8. [DOI] [PubMed] [Google Scholar]
- 47.Murofushi T, Halmagyi G M, Yavor R A, Colebatch J G. Absent vestibular evoked myogenic potentials in vestibular neurolabyrinthitis. An indicator of inferior vestibular nerve involvement? Arch Otolaryngol Head Neck Surg. 1996;122:845–848. doi: 10.1001/archotol.1996.01890200035008. [DOI] [PubMed] [Google Scholar]
- 48.Gopen Q, Zhou G, Poe D, Kenna M, Jones D. Posterior semicircular canal dehiscence: first reported case series. Otol Neurotol. 2010;31:339–344. doi: 10.1097/MAO.0b013e3181be65a4. [DOI] [PubMed] [Google Scholar]
- 49.Mikulec A A, Poe D S. Operative management of a posterior semicircular canal dehiscence. Laryngoscope. 2006;116:375–378. doi: 10.1097/01.mlg.0000200358.93385.5c. [DOI] [PubMed] [Google Scholar]
- 50.Crane B T, Lin F R, Minor L B, Carey J P. Improvement in autophony symptoms after superior canal dehiscence repair. Otol Neurotol. 2010;31:140–146. doi: 10.1097/mao.0b013e3181bc39ab. [DOI] [PubMed] [Google Scholar]
- 51.Brantberg K, Bergenius J, Mendel L, Witt H, Tribukait A, Ygge J. Symptoms, findings and treatment in patients with dehiscence of the superior semicircular canal. Acta Otolaryngol. 2001;121:68–75. doi: 10.1080/000164801300006308. [DOI] [PubMed] [Google Scholar]
- 52.Hillman T A, Kertesz T R, Hadley K, Shelton C. Reversible peripheral vestibulopathy: the treatment of superior canal dehiscence. Otolaryngol Head Neck Surg. 2006;134:431–436. doi: 10.1016/j.otohns.2005.10.033. [DOI] [PubMed] [Google Scholar]
- 53.Pletcher S D, Oghalai J S, Reeck J B, Cheung S W. Management of superior canal dehiscence syndrome with extensive skull-base deficiency. ORL J Otorhinolaryngol Relat Spec. 2005;67:192–195. doi: 10.1159/000086663. [DOI] [PubMed] [Google Scholar]
- 54.Limb C J, Carey J P, Srireddy S, Minor L B. Auditory function in patients with surgically treated superior semicircular canal dehiscence. Otol Neurotol. 2006;27:969–980. doi: 10.1097/01.mao.0000235376.70492.8e. [DOI] [PubMed] [Google Scholar]