Abstract
An ectopic pancreas is defined as pancreatic tissue lacking vascular or anatomic communication with the normal body of the pancreas. It is rarely symptomatic as it is found incidentally at laparotomy most of the time. Despite advances in diagnostic modalities, it still remains a challenge to the clinician to differentiate it from a neoplasm. It is prudent to differentiate it from neoplastic etiologies, as simple surgical excision can potentially be curative. We discuss the presentation, diagnosis, and treatment of an interesting case of ectopic pancreas presenting as a gastric antral tumor.
Keywords: ectopic pancreas, heterotopic pancreas, gastric outlet obstruction, pancreatic heterotopia, classification of ectopic pancreas, gastric antral tumor, microscopy of ectopic pancreas
Case Report
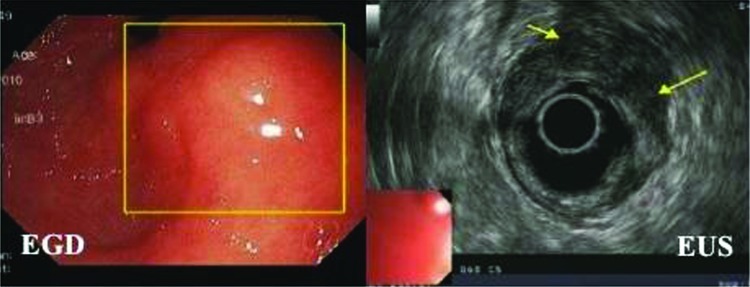
A 57-year-old nonsmoker, nonalcoholic man presented with a 2-year history of chronic abdominal pain and discomfort. Past medical history was relevant for an Helicobacter pylori duodenal ulcer (with persistent residual prepyloric gastric wall thickening on upper endoscopy), as well as a strong family history of gastric cancer. Physical examination on initial presentation revealed minimal tenderness in the epigastric region with no peritoneal signs. Vital signs were stable. Laboratory examination showed no biochemical abnormalities. Computed tomography scan of the abdomen and pelvis with oral and intravenous contrast showed an ill-defined mass at the gastric antrum causing gastric outlet obstruction (Fig. 1).
Fig. 1.
Contrast-enhanced computed tomography abdomen image demonstrating the mass (d), in relation to the gastric antrum (A) and pancreas (P). The green arrow is pointing to the gastric antral mass.
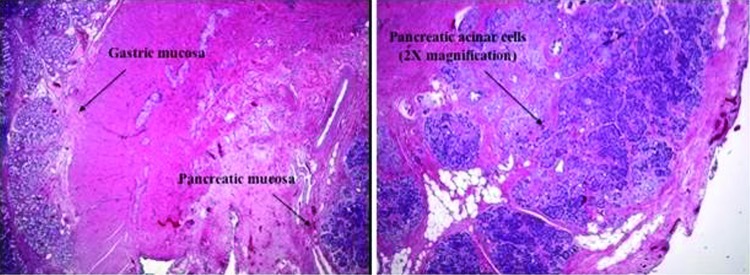
Esophagogastroduodenoscopy (EGD) and endoscopic ultrasound (EUS) examination revealed a 3 × 1 cm localized intramural wall mass in the prepyloric region (Fig. 2). Biopsy demonstrated no evidence of malignancy. The patient's family history of gastric malignancy, chronicity of his symptoms, and persistence of gastric wall thickening prompted a decision to proceed with an operative intervention to exclude a gastric neoplasm.
Fig. 2.
EGD image showing the antral mass (yellow box) and EUS demonstrating the hypoechoic mass measuring 3 × 1 cm (yellow arrows). EGD, esophagogastroduodenoscopy; EUS, endoscopic ultrasound.
On laparoscopy a distinct 3 × 2 × 1 cm mass was identified at the gastric antrum and was dissected off the duodenum. An antrectomy and antecolic gastrojejunostomy were performed with no complications. The patient had an uneventful postoperative course and was discharged home on postoperative day 5.
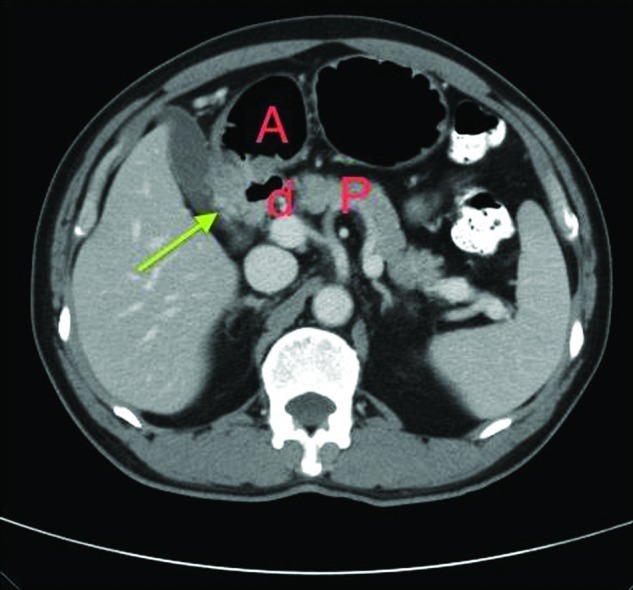
Histopathology of the mass showed pancreatic heterotopia with ducts and acini in the antral wall of the stomach (Fig. 3).
Fig. 3.
Microscopic appearance of pancreatic islet cells, acinar cells, and ducts in the ectopic pancreas.
Discussion
Ectopic pancreas is also referred to as pancreatic heterotopia, heterotopic pancreas, and accessory or aberrant pancreas.1 It is defined as pancreatic tissues lacking vascular or anatomic communication with the normal body of the pancreas, yet possessing histological features of pancreatic acinar formation, duct development, and islets of Langerhans with independent blood supply and ductal system.2,3,4 Ectopic pancreas is a relatively rare entity with an incidence of 0.2% at laparotomy5,6 and 0.5 to 13.7% on autopsies.7
Multiple theories have been implicated on the embryological origin of this rare condition. One of them implicates the persistence of a duodenal evagination involved in the normal development of the pancreas. This remnant can migrate with the developing gastrointestinal tract accounting for its various locations.8 Another theory suggests pancreatic metaplasia of the endodermal tissue in the gastric mucosa.8
Ectopic pancreata can be found in various anatomical sites such as the stomach, duodenum, jejunum, gallbladder, esophagus, common bile duct, spleen, mesentery, mediastinum, and fallopian tubes. The stomach is the most common location (25 to 38%),8 with pancreatic rests most frequently found in the submucosa (75% of cases) but sporadically also in the muscularis propria and serosa.9
Based on Heinrich's 1909 classification and the subsequent Gasper-Fuentes modification in 1973, there are four types of pancreatic heterotopia, and they are as follows10:
Type I—typical pancreatic tissue with acini, ducts, and islet cells similar to the normal pancreas.
Type II (canalicular variety)—pancreatic ducts only.
Type III (exocrine pancreas)—acinar tissue only.
Type IV (endocrine pancreas)—islet cells only.
The patient in our case report was a type I, with all components of the organ.
Although ectopic pancreata are usually an incidental finding, they can present with nonspecific symptoms such as abdominal pain, abdominal fullness, nausea, vomiting, anorexia, weight loss, anemia, and melena.11 Abdominal pain is the most common symptomatic presentation, and can be explained by the inflammation and irritation of surrounding tissues secondary to the secretion of pancreatic enzymes and hormones.12 Pain can also be explained as a result of hemorrhage in the lesion due to mucosal erosion and ulcer formation, especially when it occurs in the small intestine.13 Patients can also present with symptoms of gastric outlet obstruction as in our patient with larger lesions at the gastric antrum, especially those greater than 1.5 cm in size.14 Published literature reports have described rare instances of malignant degeneration in the ectopic pancreatic tissue.15
Radiological studies such as barium swallows can sometimes assist in the diagnosis by showing nonspecific fold thickening with rounded filling defects and a typical central indentation.16 Contrast-enhanced computed tomography can sometimes demonstrate nondiagnostic findings such as exophytic bowel wall lesions or mural wall thickening, as seen in our case.17
EGD findings include the possibility of a submucosal nodule with an umbilicated appearance.18 Most of the time, however, it is indistinguishable from other neoplastic processes such as gastrointestinal stromal tumors, gastrointestinal autonomic nerve tumors, carcinoid tumors, lymphomas,19 and gastric cancers.
Endoscopic-guided fine needle aspiration is usually superficial and nondiagnostic as these tumors are covered with normal gastric mucosa. However, a positive biopsy can be diagnostic.20 The recent advent of EUS has improved the sensitivity of diagnosis for these lesions by 80 to 100%.21,22 Kim et al23 reported that EUS features of ectopic pancreata that differentiate them from mesenchymal tumors include the following: larger longest/shortest diameter ratio, antral location, mural growth pattern, third (submucosal) layer disruption, irregular margins, and intermediate echogenicity. However, none of these findings individually or collectively are diagnostic of ectopic pancreata, as they can be seen with any neoplastic lesion of the bowel wall and still require operative resection to confirm the diagnosis.
At pathology, the gross appearance of an ectopic pancreas includes the presence of a characteristic central ductal orifice.24 Histopathological examination reveals pancreatic acini, ducts, islets of Langerhans, and intervening connective tissue.
The preoperative diagnosis of an ectopic pancreas is still challenging despite advanced diagnostic tools, and the frequent inability to differentiate it from neoplastic lesions warrants surgical excision. Despite keen clinical acumen and technological advances in diagnostic tools, the final diagnosis of ectopic pancreas in our case was made after excision on histopathology, hence explaining the “diagnostic dilemma.”
In conclusion, although ectopic pancreas is a rare entity, clinicians should consider this as an important differential diagnosis of extramucosal gastric lesions as a simple excision can be potentially curative.
References
- 1.Kim J Y, Lee J M, Kim K W. et al. Ectopic pancreas: CT findings with emphasis on differentiation from small gastrointestinal stromal tumor and leiomyoma. Radiology. 2009;252(1):92–100. doi: 10.1148/radiol.2521081441. [DOI] [PubMed] [Google Scholar]
- 2.Cullen J J, Weydert C, Hinkhouse M M. et al. The role of manganese superoxide dismutase in the growth of pancreatic adenocarcinoma. Cancer Res. 2003;63(6):1297–1303. [PubMed] [Google Scholar]
- 3.Ozcan C, Celik A, Güçlü C, Balik E. A rare cause of gastric outlet obstruction in the newborn: pyloric ectopic pancreas. J Pediatr Surg. 2002;37(1):119–120. doi: 10.1053/jpsu.2002.29443. [DOI] [PubMed] [Google Scholar]
- 4.Hsu S D, Chan D C, Hsieh H F, Chen T W, Yu J C, Chou S J. Ectopic pancreas presenting as ampulla of Vater tumor. Am J Surg. 2008;195(4):498–500. doi: 10.1016/j.amjsurg.2007.01.043. [DOI] [PubMed] [Google Scholar]
- 5.Laurent T, Fournier D, Doenz F, Karaaslan T, Wassmer F A. Complex lesion of the gastric wall: an unusual presentation of ectopic pancreas. J Clin Ultrasound. 1995;23(7):438–441. doi: 10.1002/jcu.1870230709. [DOI] [PubMed] [Google Scholar]
- 6.Ura H, Denno R, Hirata K, Saeki A, Hirata K, Natori H. Carcinoma arising from ectopic pancreas in the stomach: endosonographic detection of malignant change. J Clin Ultrasound. 1998;26(5):265–268. doi: 10.1002/(sici)1097-0096(199806)26:5<265::aid-jcu7>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 7.Mulholland K C, Wallace W D, Epanomeritakis E, Hall S R. Pseudocyst formation in gastric ectopic pancreas. JOP. 2004;5(6):498–501. [PubMed] [Google Scholar]
- 8.Chandan V S, Wang W. Pancreatic heterotopia in the gastric antrum. Arch Pathol Lab Med. 2004;128(1):111–112. doi: 10.5858/2004-128-111-PHITGA. [DOI] [PubMed] [Google Scholar]
- 9.Owen D A. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. The stomach. In: Sternberg's Diagnostic Surgical Pathology. 4th ed; pp. 1436–1437. [Google Scholar]
- 10.Gaspar Fuentes A, Campos Tarrech J M, Fernández Burgui J L. et al. [Pancreatic ectopias] Rev Esp Enferm Apar Dig. 1973;39(3):255–268. [PubMed] [Google Scholar]
- 11.Matsumoto Y, Kawai Y, Kimura K. Aberrant pancreas causing pyloric obstruction. Surgery. 1974;76(5):827–829. [PubMed] [Google Scholar]
- 12.Ormarsson O T, Gudmundsdottir I, Mårvik R. Diagnosis and treatment of gastric heterotopic pancreas. World J Surg. 2006;30(9):1682–1689. doi: 10.1007/s00268-005-0669-6. [DOI] [PubMed] [Google Scholar]
- 13.Armstrong C P, King P M, Dixon J M, Macleod I B. The clinical significance of heterotopic pancreas in the gastrointestinal tract. Br J Surg. 1981;68(6):384–387. doi: 10.1002/bjs.1800680606. [DOI] [PubMed] [Google Scholar]
- 14.Hsia C Y, Wu C W, Lui W Y. Heterotopic pancreas: a difficult diagnosis. J Clin Gastroenterol. 1999;28(2):144–147. doi: 10.1097/00004836-199903000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Eisenberger C F, Gocht A, Knoefel W T. et al. Heterotopic pancreas—clinical presentation and pathology with review of the literature. Hepatogastroenterology. 2004;51(57):854–858. [PubMed] [Google Scholar]
- 16.Nicolau A, Bruneton J N, Balu C, Aubanel D, Roux P. [Radiologic study of aberrant pancreas of gastroduodenal topography. Apropos of 11 cases] J Radiol. 1983;64(5):319–324. [PubMed] [Google Scholar]
- 17.Shanbhogue A K, Fasih N, Surabhi V R, Doherty G P, Shanbhogue D K, Sethi S K. A clinical and radiologic review of uncommon types and causes of pancreatitis. Radiographics. 2009;29(4):1003–1026. doi: 10.1148/rg.294085748. [DOI] [PubMed] [Google Scholar]
- 18.Sakorafas G H, Sarr M G. Ectopic gastric submucosal pancreatic tissue. JOP. J Pancreas. 2003;4:214–215. [PubMed] [Google Scholar]
- 19.Riyaz A, Cohen H. Ectopic pancreas presenting as a submucosal gastric antral tumor that was cystic on EUS. Gastrointest Endosc. 2001;53(6):675–677. doi: 10.1067/mge.2001.113270. [DOI] [PubMed] [Google Scholar]
- 20.Osanai M, Miyokawa N, Tamaki T, Yonekawa M, Kawamura A, Sawada N. Adenocarcinoma arising in gastric heterotopic pancreas: clinicopathological and immunohistochemical study with genetic analysis of a case. Pathol Int. 2001;51(7):549–554. doi: 10.1046/j.1440-1827.2001.01240.x. [DOI] [PubMed] [Google Scholar]
- 21.Thoeni R F, Gedgaudas R K. Ectopic pancreas: usual and unusual features. Gastrointest Radiol. 1980;5(1):37–42. doi: 10.1007/BF01888597. [DOI] [PubMed] [Google Scholar]
- 22.Chak A, Canto M I, Rösch T. et al. Endosonographic differentiation of benign and malignant stromal cell tumors. Gastrointest Endosc. 1997;45(6):468–473. doi: 10.1016/s0016-5107(97)70175-5. [DOI] [PubMed] [Google Scholar]
- 23.Kim J H, Lim J S, Lee Y C. et al. Endosonographic features of gastric ectopic pancreases distinguishable from mesenchymal tumors. J Gastroenterol Hepatol. 2008;23(8 Pt 2):e301–e307. doi: 10.1111/j.1440-1746.2008.05351.x. [DOI] [PubMed] [Google Scholar]
- 24.Sebastian M W. Philadelphia: WB Saunders Company; 1997. The stomach and duodenum; p. 872. [Google Scholar]