Abstract
There is a relative dearth of fundamental anatomic information regarding the radial component of right and left coronary ostial location along the circumference of the aortic root. Recent literature has emphasized the importance of this anatomic component in the orientation of coronary buttons for the composite graft operation, especially as regards the use of porcine biological roots or design of novel mechanical or biological composite grafts. Problems in orientation of reattached buttons can lead to life-threatening ischemia. We assessed the radial location of native coronary arteries or coronary artery buttons by high-definition computed tomography scan in 100 patients (75 consecutive aneurysm patients undergoing aortic root replacement [ARR] and 25 control patients undergoing coronary artery bypass). We excluded six patients with unclear coronary anatomy and one with an anomalous origin. The center point of the aortic lumen was located, radii were drawn from there to each coronary ostium, and the angle was computed geometrically. The mean angle between the radii for the right and left coronary ostia was 122.9 degrees. The angle was similar for bicuspid and tri-leaflet aneurysm patients, 121.0 and 122.7 degrees, respectively. The angle was similar for aneurysm patients (121.6 degrees) and for controls (126.5 degrees). The angle showed very little variation among individuals for the overall group (standard deviation [SD] 13.1 degrees), for the aneurysm patients (SD 13.4 degrees), and for the controls (SD 12 degrees). This angle is different from that of the porcine roots (145 degrees) which are commonly used for ARR. The normal human angular separation between the right and left coronary ostia is 122.9 degrees for both aneurysm and control patients. This anatomic relationship is very different from that of porcine aortic roots. This anatomy needs to be borne in mind intraoperatively. This anatomic relationship can be used in the design of novel aortic root biological or composite grafts.
Keywords: aortic root replacement, coronary reimplantation, Medtronic FreeStyle, coronary angle
Aortic root replacement (ARR) has been recognized as the standard therapy for diseases of the aortic root since its introduction into clinical practice by Donald Ross in 1962.1,2,3,4,5 This procedure is most commonly performed to treat aortic root aneurysms and aortic dissections. The ARR procedure has been refined over the years and currently provides excellent long-term benefit with acceptable perioperative risk and excellent long-term freedom from morbidity and mortality.3,4,5 Experienced centers have reduced the mortality of this operation to 2 to 6%,3,4,5 essentially curing the patients of their potentially lethal aortic root pathology.
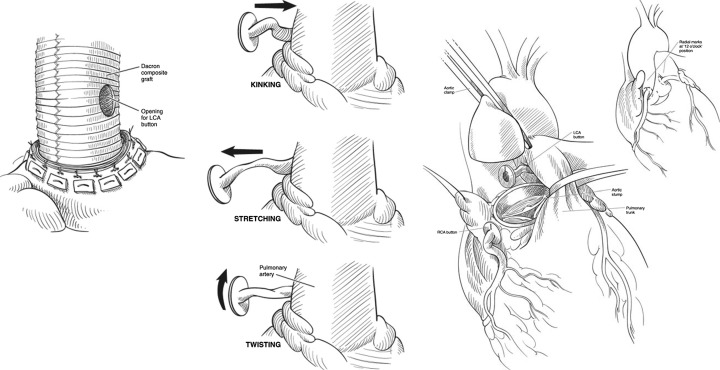
However, ARR procedures are more complex than standard aortic valve replacement (AVR). ARR has a significant learning curve and carries its own unique risks, including longer operative, cardiopulmonary bypass, and aortic cross-clamp times. The mobilization of coronary buttons is a delicate procedure that requires great care to produce adequate mobility without arterial perforation or sacrifice of important branches. The length, lie, and torsional orientation are crucial when the buttons are anastomosed to openings created in the side of the main graft. A potentially lethal problem while performing ARR is malpositioning of the coronary buttons—via tension, buckling, or torsion causing myocardial ischemia, ventricular arrhythmias, myocardial infarction, or pump failure (Fig. 1).6,7 Recent literature has emphasized the importance of the anatomic component in orientation of coronary buttons for the composite graft operation, especially as regards the use of porcine biological roots or design of novel mechanical or biological composite grafts.6,7 If unrecognized, myocardial ischemia due to technical problems with the coronary buttons will progress quickly to a lethal complication.6,7 Different centers have varying technical approaches to the process of orientation and reimplantation of coronary buttons. Specifically, different surgeons take different approaches to the orientation of the buttons vis-a-vis the native coronary ostia of porcine aortic roots (e.g., Medtronic Freesytle graft; Medtronic, Minneapolis, MN). Like Kincaid and colleagues, we also rotate the porcine root clockwise, putting the right button in place of the original left, and locating the left button in the original noncoronary sinus.6,7
Fig. 1.
Coronary reimplantation procedure and hypothetical mechanisms of myocardial ischemia. (Reproduced with permission Shahriari A, Eng M, Tranquili M, Elefteriades JA. Rescue coronary artery bypass grafting (CABG) after aortic composite graft replacement. J Cardiac Surg 2009;24:392–396.)
In this article, we report the anatomy of coronary orientation in 100 human patients, and patients with aortic root aneurysms and controls (coronary bypass patients). We use high-resolution computed tomography (CT) scans to determine the precise radial location of the coronary arteries, with an eye toward better anatomically arming the surgeon for these operations, especially as regards the use of porcine roots and the design and utilization of novel mechanical or biological aortic composite grafts.
Materials and Methods
Patients
This study was approved by the Yale Human Investigation Committee. We studied 75 consecutive aortic root aneurysm patients who underwent ARR between 2004 and 2011. We used the preoperative CT scans to determine the original position of their coronary arteries. We also studied 25 concurrent control patients (predominantly coronary artery bypass graft [CABG] patients, with two mitral valve replacements, two nonaneurysm AVR, two subtotal pericardectomy, and one tricuspid valve excision patient) with CT scan images.
Methods
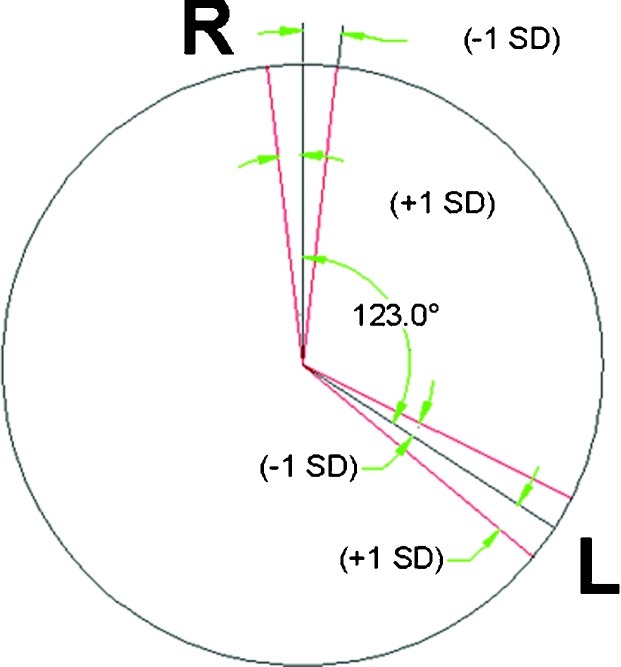
We assessed the radial location of coronary artery buttons by high-definition CT scan in 100 patients (75 consecutive aneurysm patients undergoing ARR and 25 control patients). Of these, six patients had a nondominant right coronary artery that was not readily identified and one had an anomalous coronary; these patients were excluded from analysis. We were able to construct radii from the center of the aorta to the radial positions of the coronary arteries (Fig. 2) (often by superimposing different but adjacent axial images, as the right coronary artery usually arises more caudally than the left). The center point of the aortic lumen was located, radii were drawn from that center point to each coronary ostium, and the angle was computed geometrically. For both patients and controls, we chose consecutive patients with suitable images operated between 2004 and 2011. The results were analyzed by Student t test and by simple arithmetic to identify the most common radial angular separation and to determine if there were differences between aneurysm patients and controls and if there were differences between bicuspid and tricuspid aortic valve patients.
Fig. 2.
High-definition computed tomography (CT) scan showing the position of left main and right coronary artery and our angular measurement methodology.
Results
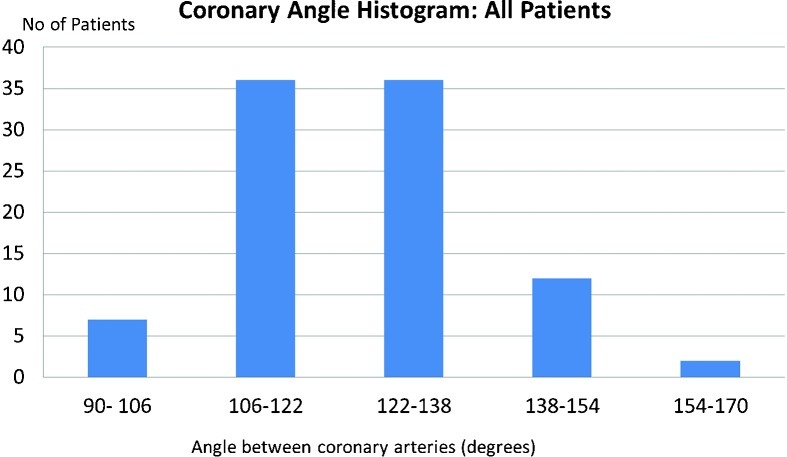
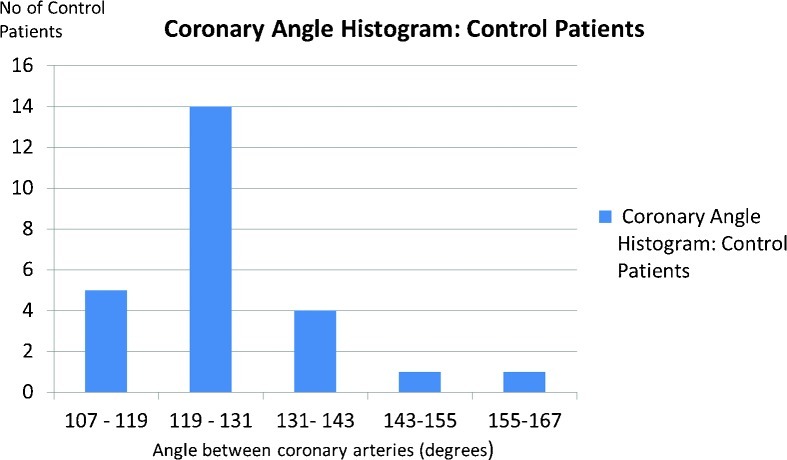
The mean angular separation between the radii for the right and left coronaries was 122.9 degrees with little variation for the overall group of patients. The angle was similar for aneurysm patients (121.6 degrees) and for controls (126.5 degrees) (nonsignificant p value). The angle showed very little variation among individuals for the overall group (standard deviation [SD] 13.1 degrees), for the aneurysm patients (SD 13.4 degrees), and for the controls (SD 12 degrees)(Figs. 3,4,5,6,7).
Fig. 3.
Theradial separation of right and left coronary artery is ~ 123 degrees. The positions of the right and left coronaries fall mostly between the red lines (± one SD).
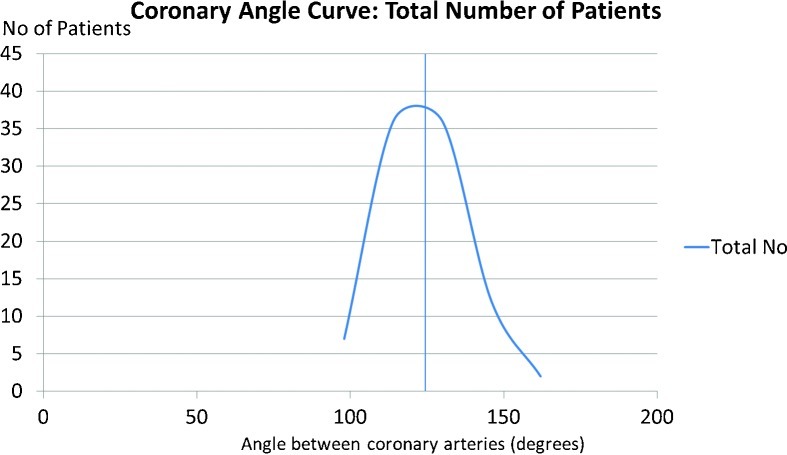
Fig. 4.
Frequency of distribution of coronary angle for the total number of patients excluding those with unclear angiography.
Fig. 5.
Frequency of distribution of coronary angle for control subjects.
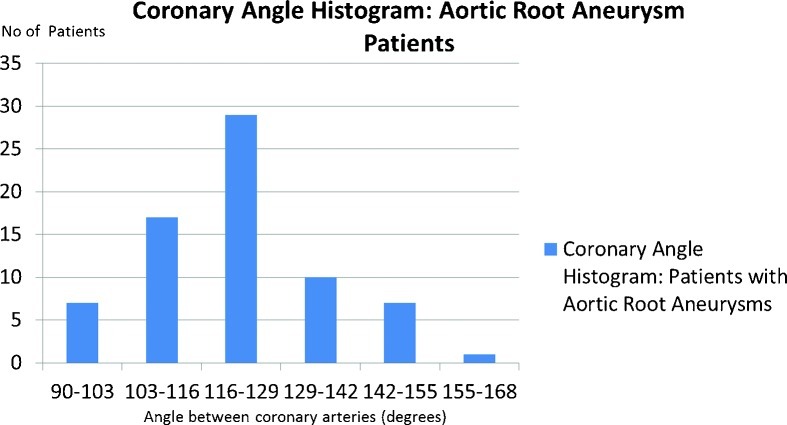
Fig. 6.
Frequency of distribution of coronary angle for patients with aortic root aneurysm.
Fig. 7.
Frequency distribution of coronary angle for the total number of patients excluding those with unclear anatomy. Black line depicts the mean angle (123.4 degrees).
The median angle was 121, and 113 degrees was the single most frequent value obtained. Similarity of angle values was evident even for bicuspid and tricuspid valves. We used our intraoperative valve morphology data to identify 22 patients with bicuspid valves and 39 patients known to have tricuspid valves, and angle means were 121.0 and 122.7 degrees, respectively (nonsignificant p value).
Conclusion
Since its introduction in 1962 by Bentall and De Bono1 and Ross,2 ARR has undergone significant evolution and is now an established treatment for diseases of the aortic valve and the aortic root. Root replacement has proven to be a very safe procedure with mortality averaging around 3% in recent published series.3,4,5,7
A considerable share of the published morbidity and mortality for these operations involves the risks and complications inherent to reimplantation of the coronary ostia. In our series, 2.2% of the patients needed rescue CABG for postoperative coronary insufficiency.7 Although, fortunately, this did not translate into mortality in our cohort, not recognizing this complication would have led to surgical mortality.7
This investigation indicates that radial separation of the right and left coronary arteries in humans (absent major anatomic anomalies) is ~ 123 degrees. This varies very little from individual to individual. This anatomic relationship is also preserved in the presence of an aortic root aneurysm; that is, as the aorta enlarges, the radial separation of the right and left coronary arteries maintains it original relationship.
The anatomic relationship between the right and left coronary arteries differs from that of porcine aortic roots. We were able to calculate from Medtronic photographs an angle of 145 degrees for the porcine roots; very different from the human angle we have shown here. This anatomy needs to be borne in mind intraoperatively, when using porcine roots, to avoid the risk of coronary insufficiency, which has been reported by Kincaid and colleagues in the root replacement setting.6
New valve conduits regularly come in the market, which are designed to facilitate coronary button implantation. Design of novel aortic root, biological or composite, grafts needs to respect the radial coronary anatomy. We hope that the findings from this anatomic study can inform the design of novel conduits and eliminate or minimize misalignment and subsequent coronary tension or torsion.
References
- 1.Bentall H, De Bono A. A technique for complete replacement of the ascending aorta. Thorax. 1968;23(4):338–339. doi: 10.1136/thx.23.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ross D N. Homograft replacement of the aortic valve. Lancet. 1962;2(7254):487. doi: 10.1016/s0140-6736(62)90345-8. [DOI] [PubMed] [Google Scholar]
- 3.Lima B Hughes G C Lemaire A Jaggers J Glower D D Wolfe W G Short-term and intermediate-term outcomes of aortic root replacement with St. Jude mechanical conduits and aortic allografts Ann Thorac Surg 2006822579–585., discussion 585 [DOI] [PubMed] [Google Scholar]
- 4.Hatzaras I, Koullias G J, Tranquilli M, Achneck H, Elefteriades J A. Mid-term thromboembolic and bleeding complications are minimal after composite graft replacement of the aortic root. Int J Angiol. 2005;14:118–122. [Google Scholar]
- 5.Westaby S, Katsumata T, Vaccari G. Aortic root replacement with coronary button re-implantation: low risk and predictable outcome. Eur J Cardiothorac Surg. 2000;17(3):259–265. doi: 10.1016/s1010-7940(00)00347-x. [DOI] [PubMed] [Google Scholar]
- 6.Kincaid E H Cordell A R Hammon J W Adair S M Kon N D Coronary insufficiency after stentless aortic root replacement: risk factors and solutions Ann Thorac Surg 2007833964–968., discussion 968 [DOI] [PubMed] [Google Scholar]
- 7.Shahriari A, Eng M, Tranquilli M, Elefteriades J A. Rescue coronary artery bypass grafting (CABG) after aortic composite graft replacement. J Card Surg. 2009;24(4):392–396. doi: 10.1111/j.1540-8191.2008.00762.x. [DOI] [PubMed] [Google Scholar]