Abstract
A curious hemodynamic phenomenon emerging as a consequence of the treatment of varicose veins can offer a reasonable explanation why varicose vein and reflux recurrences occur tenaciously irrespective of the applied therapeutic procedure. Saphenous reflux is the most important hemodynamic factor in varicose vein disease: it is responsible for the hemodynamic disturbance, ambulatory venous hypertension, clinical symptoms, and chronic venous insufficiency. Abolition of saphenous reflux eliminates the hemodynamic disturbance and restores physiological hemodynamic and pressure conditions, but at the same time it unavoidably evokes a pressure difference between the femoral vein and the incompetent superficial veins in the thigh during calf pump activity. The pressure difference increases flow and enhances fluid shear stress on the endothelium in pre-existing minor communicating channels between the femoral vein and the saphenous system in the thigh, which triggers release of biochemical agents nitride oxide and vascular endothelial growth factor; the consequence is enlargement (vascular remodeling) of the communicating channels, and ultimately reflux recurrence.
Hence, the abolition of saphenous reflux creates preconditions for the comeback of the previous pathological situation. This phenomenon—starting the same trouble while fixing the problem—has been called hemodynamic paradox; is explains why varicose vein and reflux recurrence can occur after any mode of therapy.
Keywords: varicose vein recurrence, venous hemodynamics, hemodynamic paradox
Varicose vein recurrence is a frequent event; it occurs in a wide range right up to 90%1,2,3,4 depending on the length of follow-up, the mode of therapy, and the method used to diagnose recurrence. The majority of recurrences is associated with further reflux in the groin. Spontaneous disease progression, inadequate surgery, and technical failure at the time of the original surgery have been blamed to be the main cause of recurrences, especially low ligation of the great saphenous vein (GSV) in the groin leaving behind incompetent saphenofemoral junction (SFJ) with saphenous stump and venous collaterals, as well as resigning to remove the GSV in the thigh.1,2,3,4,5,6,7,8 Meticulous dissection of the SFJ was considered in the past to be the sound protection from varicose vein and reflux recurrence. Nevertheless, groin recurrences occurred after correctly performed crossectomy and stripping as well, which was documented with duplex ultrasonography and phlebography.1,3,9,10,11,12,13,14 The reoccurrence of new venous channels emanating from the femoral vein in the groin and joining incompetent superficial vein in the thigh has been termed neovascularization; recurrences due to neovascularization were brought into direct relation with the surgical procedure.
Neovascularization
Recurrences after flawlessly performed crossectomy and stripping were reported in the range from 10.7 to 60%, occurring 2 to 34 years after surgery.3,9,11,15 Recurrences were more common if stripping was not added to crossectomy. After pure crossectomy, the saphenous remnant in the thigh remains patent and competent in most cases; recurrent reflux in incompetent GSV in the thigh 4 years after crossectomy was reported in 81.5% of cases.16
Recurrences depicted in duplex ultrasonography were described either as tortuous single-lumen channels or as a strand of tiny vessels.9,11 There are two possible mechanisms by which new reflux-carrying vessels develop in the groin, and they are as follows:
Vascular remodeling, that is, dilatation of pre-existing minor veins, apparent as single tortuous channels originating from the upper part of the femoral vein and connecting with incompetent superficial veins in the thigh; they are hemodynamically relevant.
Neoangiogenesis, newly formed vessels; they have the form of a strand or tangle consisting of several tiny vessels. They originate at the previous SFJ and connect with the saphenous vein or its branches. The hemodynamic significance of these strand-like formed channels is contentious.
Histological criteria and immunohistological findings can differentiate between neoangiogenesis and dilated preformed veins.1,2,17 Neoangiogenesis is characterized by incomplete wall structure, absence of nerves fibers, bizarre form of lumen, and multiple channel recurrence. Dilated preformed veins contain three-layered wall and intramural nerve fibers; they form single tortuous channels. The presence of the neural marker S100 protein in immunohistological findings indicates pre-existing dilated vessels, and its absence indicates new grown vessels.
Neovascularization has been blamed as the cause of recurrences after correctly performed surgery. Several methods were used to prevent neovascularization in the groin: suture of the foramen ovale, inverting suturing of the femoral vein after surgical resection of the SFJ, and insertion of various types of mechanical barriers using synthetic patches.10,12,18,19,20,21,22,23,24,25 These attempts either moderately reduced reflux recurrence at the groin in some studies or were ineffective in others, but in all they did not preclude development of recurrent reflux. Some authors expressed the opinion that recurrent reflux in varicose vein disease was unavoidable, no matter how careful and painstaking the primary procedure might be, and postulated that neovascularization might be the effect of altered venous hemodynamics triggered by unspecified hemodynamic factors.1,13
The Hemodynamic Paradox
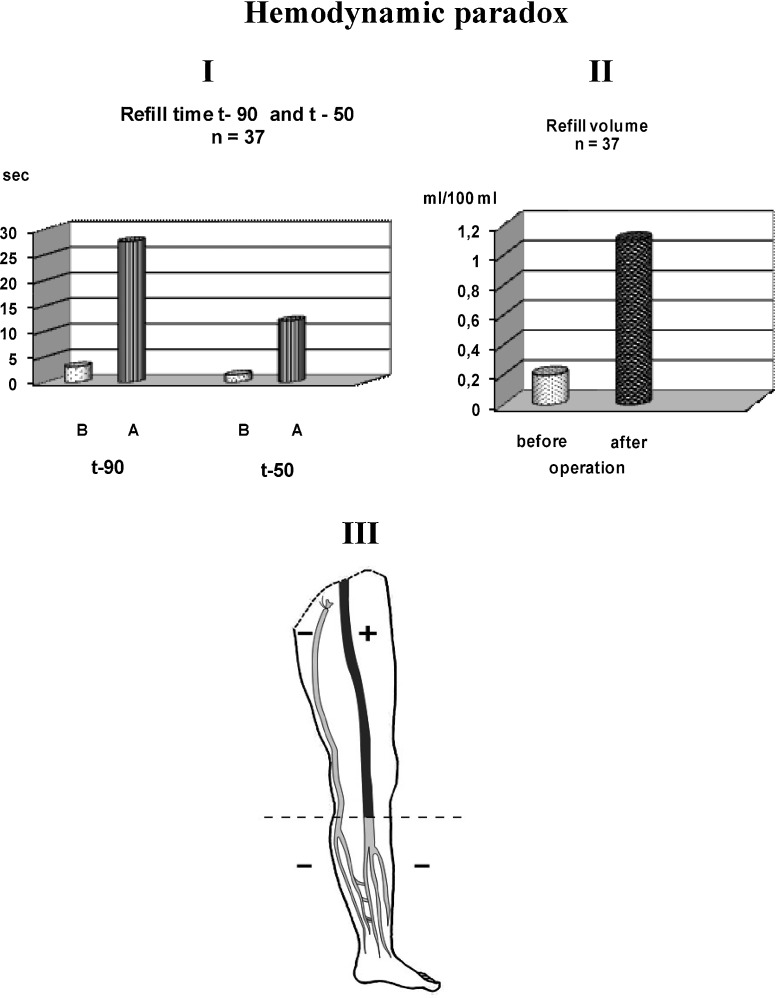
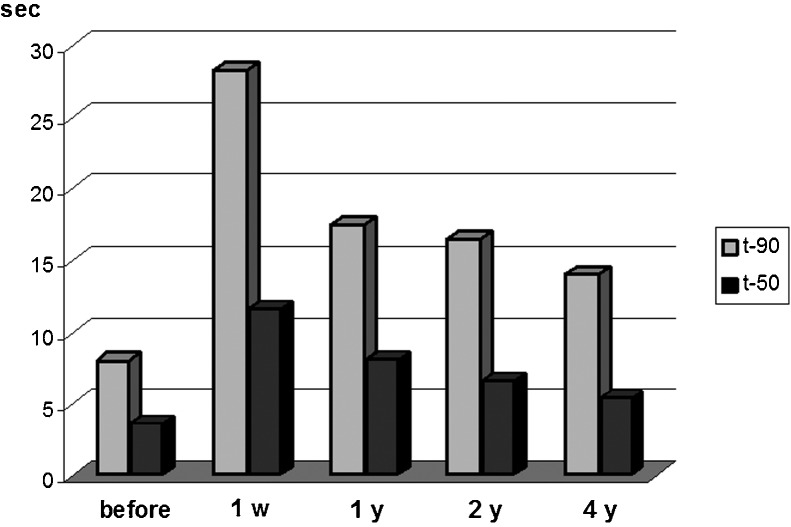
A curious hemodynamic phenomenon emerging as a consequence of treatment of varicose veins might offer a reasonable explanation why varicose vein and reflux recurrences occur tenaciously irrespective of the applied procedure. Saphenous reflux is the most important pathological phenomenon in varicose vein disease; it causes ambulatory venous hypertension and is responsible for the severity of hemodynamic disturbance, clinical symptoms, and appearance of chronic venous insufficiency. Abolition of saphenous reflux removes the hemodynamic pathology and restores physiological conditions even in patients afflicted with the severest form of chronic venous insufficiency, with varicose ulcers.26,27,28,29,30,31 Fig. 1 (I and II) sets an example of what had been proved a lot of times: surgical interruption of saphenous reflux in the groin removed the severest hemodynamic disturbance and restored physiological conditions immediately after surgery;26 consequently, the therapeutic goal was perfectly achieved. But curiously enough, abolition of saphenous reflux at the same time generates preconditions for the development of recurrent reflux and for progressive comeback of the previous pathological situation (Fig. 1, III). The excellent immediate result recorded 1 week after flawless elimination of saphenous reflux deteriorates progressively in the course of time due to the perturbing effect of recurrent reflux.16 Fig. 2 demonstrates this progressive deterioration of the hemodynamic situation during 4-year follow-up, evaluated by strain gauge plethysmography.16
Fig. 1.
Hemodynamic paradox. Strain gauge plethysmographic parameters refill time t-90 and t-50 as well as refill volumes (I and II) evaluated in patients with a grave form of chronic venous insufficiency showed the severest hemodynamic disorder before surgery, and utter normalization of the hemodynamic situation 1 week after abolition of saphenous reflux. B, before; A, after operation. Curiously enough, at the same time preconditions for recurrent reflux and for progressive comeback of the previous pathological situation were generated (III). Pressure difference of 37.4 ± 6.4 mm Hg arising between the femoral vein and saphenous remnant during calf pump activity triggers biophysical and biochemical events that induce progressive enlargement of pre-existing minor communications between deep and superficial veins in the thigh; the process ultimately results in recurrent reflux. The sign + means higher pressure; the sign − means lower pressure. The dashed line shows the boundary of the ambulatory pressure gradient between thigh and lower leg veins occurring in healthy persons. For more details see text.
Fig. 2.
Progressive deterioration of the hemodynamic situation during 4-year follow-up after crossectomy evaluated by strain gauge plethysmographic parameters refill time t-90 and t-50. 1 w, 1 week after crossectomy; y, year(s).
In healthy persons, ambulatory pressure gradient arises during calf pump activity and separates thigh veins with a higher pressure from lower leg veins with a lower pressure,27 as shown in Fig. 3. Competent valves in deep lower leg veins as well as in the saphenous system preclude drainage of venous blood from the thigh into the lower leg, and ensure physiological decrease in venous pressure in the lower leg and foot during calf pump activity. In varicose vein patients, the saphenous remnant in the thigh remains patent and incompetent in most cases after interruption of saphenous reflux; it enables drainage of venous blood from the thigh into the deep lower leg veins during calf pump activity. This drainage of venous blood from superficial veins in the thigh into the deep lower leg veins is a characteristic pathological feature of varicose vein disease; as a consequence, ambulatory hypotension extends from deep lower leg veins into incompetent superficial veins in the thigh. Since the pressure in the femoral vein does not decrease during calf pump activity, a pressure gradient of 37.4 ± 6.4 mm Hg arises between the femoral vein and incompetent superficial veins in the thigh.27 The pressure difference enhances flow rate through pre-existing minor, as yet inactive communicating channels connecting deep and superficial veins in the thigh. The increased flow increases fluid shear stress on the endothelium, which activates biochemical agents nitride oxide and vascular endothelial growth factor28,29,30,31,32; these substances induce progressive enlargement of the tiny communicating channels (vascular remodeling), and ultimately bring about recurrent reflux. Formation of new venous communicating channels between deep and superficial veins in the upper part of the thigh after abolition of saphenous reflux has been documented in several articles, as cited above. The same process triggered by pressure difference, based on the same events, and forming collateral circulation apparently happens also in arterial occlusions, in venous thrombosis, and in congenital arteriovenous fistulas.
Fig. 3.
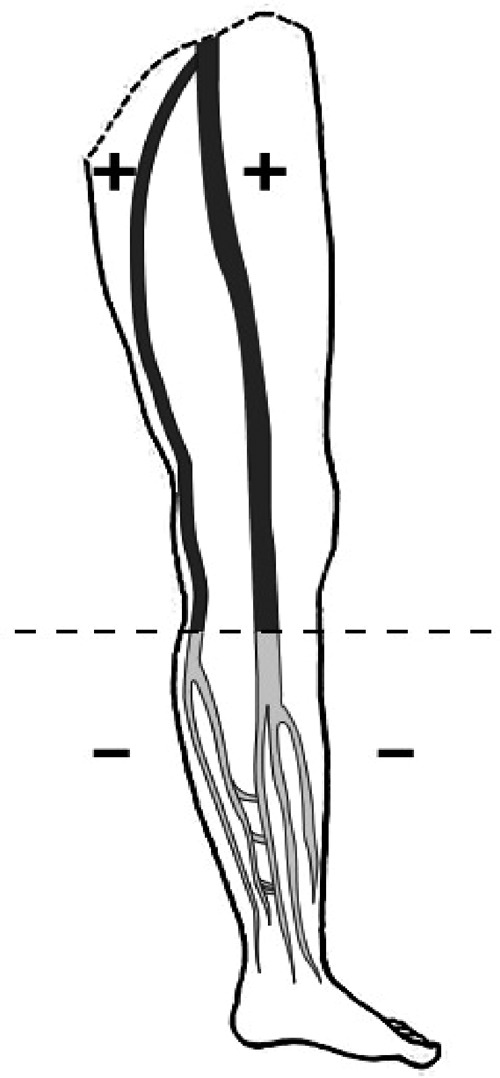
Ambulatory pressure gradient arising during calf pump activity in healthy persons with a higher pressure in the thigh veins and a lower pressure in the lower leg veins. The sign + means higher pressure; the sign − means lower pressure. The dashed line shows the boundary of the ambulatory pressure gradient.
From this point of view, abolition of saphenous reflux should be considered as a very effective, nevertheless just a palliative therapeutic measure, because the propensity for reflux recurrence progressively attenuates and ultimately thwarts the excellent immediate therapeutic result.16 Although the pressure gradient between the femoral vein and incompetent veins in the thigh in varicose vein patients triggers biophysical and biochemical events that induce the recurrence process, other unspecified circumstances involved in the recurrence process determine which type of recurrence, as concerns amount and timing of recurrence will take place.
Neovascularization or vascular remodeling does not come about in persons with healthy veins. As set out, competent valves in healthy persons preclude drainage of venous blood from the thigh veins into the lower leg veins. That results in development of ambulatory pressure gradient during calf pump activity with a higher pressure in thigh veins and a lower pressure in lower leg veins (Fig. 3). Hence, no pressure difference occurs between the femoral vein and superficial veins in the thigh in healthy persons, the process of neovascularization cannot be set off. Vascular remodeling after harvesting GSV for bypass graft does not take place. The surgical intervention per se is not involved in the development of recurrent reflux.
Only a procedure which would preclude drainage of blood from superficial thigh veins into the lower leg, that means which would reinstall conditions distinctive of healthy persons would be capable to heal varicose vein disease. Because we are not able to convert incompetent superficial venous network into a competent one, we cannot assure definitive cure while treating varicose vein disease, and we have to realize that recurrent reflux tends to occur regardless of the therapeutic strategy adopted.
Summary
Recurrent reflux is an obstinate problem embarrassing treatment of varicose vein disease; it occurs also after correctly performed procedures. Neovascularization in the groin has been claimed as the probable cause of such recurrences. Nevertheless, attempts to preclude neovascularization and reflux recurrence in the groin by inserting mechanical barriers over the ligated SFJ failed. A hemodynamic factor–pressure difference arising after abolition of saphenous reflux between the femoral vein and the incompetent saphenous system in the thigh during calf pump activity triggers biophysical and biochemical events that entail enlargement of tiny communicating channels between the femoral vein and the saphenous system, and evokes reflux recurrence. Hence, a hemodynamic paradox develops: abolition of saphenous reflux removes the hemodynamic disturbance and restores physiological conditions, but at the same time it generates precondition for the comeback of the previous pathological situation.
The hemodynamic paradox comes about only in varicose vein disease; in healthy persons, ambulatory pressure gradient separates thigh veins with higher pressure from lower leg veins with lower pressure. Competent saphenous system precludes drainage of venous blood from the thigh into the lower leg. Consequently, no pressure difference between the femoral vein and the saphenous system in the thigh can be generated, no trigger for neovascularization occurs, vascular remodeling does not take place after harvesting of GSV for bypass grafts in patients with healthy veins.
References
- 1.El Wajeh Y, Giannoukas A D, Gulliford C J, Suvarna S K, Chan P. Saphenofemoral venous channels associated with recurrent veins are not neovascular. Eur J Vasc Endovasc Surg. 2004;28(6):590–594. doi: 10.1016/j.ejvs.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Geier B, Stücker M, Hummel T. et al. Residual stumps associated with inguinal varicose vein recurrences: a multicenter study. Eur J Vasc Endovasc Surg. 2008;36(2):207–210. doi: 10.1016/j.ejvs.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Jones L, Braithwaite B D, Selwyn D, Cooke S, Earnshaw J J. Neovascularisation is the principal cause of varicose vein recurrence: results of a randomised trial of stripping the long saphenous vein. Eur J Vasc Endovasc Surg. 1996;12(4):442–445. doi: 10.1016/s1078-5884(96)80011-6. [DOI] [PubMed] [Google Scholar]
- 4.Winterborn R J, Foy C, Earnshaw J J. Causes of varicose vein recurrence: late results of a randomized controlled trial of stripping the long saphenous vein. J Vasc Surg. 2004;40(4):634–639. doi: 10.1016/j.jvs.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Dwerryhouse S, Davies B, Harradine K, Earnshaw J J. Stripping the long saphenous vein reduces the rate of reoperation for recurrent varicose veins: five-year results of a randomized trial. J Vasc Surg. 1999;29(4):589–592. doi: 10.1016/s0741-5214(99)70302-2. [DOI] [PubMed] [Google Scholar]
- 6.Egan B Donnelly M Bresnihan M Tierney S Feeley M Neovascularization: an “innocent bystander” in recurrent varicose veins J Vasc Surg 20064461279–1284., discussion 1284 [DOI] [PubMed] [Google Scholar]
- 7.Joshi D, Sinclair A, Tsui J, Sarin S. Incomplete removal of great saphenous vein is the most common cause for recurrent varicose veins. Angiology. 2011;62(2):198–201. doi: 10.1177/0003319710375090. [DOI] [PubMed] [Google Scholar]
- 8.Sarin S, Scurr J H, Coleridge Smith P D. Stripping of the long saphenous vein in the treatment of primary varicose veins. Br J Surg. 1994;81(10):1455–1458. doi: 10.1002/bjs.1800811017. [DOI] [PubMed] [Google Scholar]
- 9.Frings N, Nelle A, Tran V TP, Glowacki P. Unavoidable recurrence and neoreflux after correctly performed ligation of the saphenofemoral junction: neovascularization? (German) Phlebologie. 2003;32:96–100. [Google Scholar]
- 10.Frings N, Nelle A, Tran P, Fischer R, Krug W. Reduction of neoreflux after correctly performed ligation of the saphenofemoral junction. A randomized study. Eur J Vasc Endovasc Surg. 2004;28(3):246–252. doi: 10.1016/j.ejvs.2004.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Fischer R, Linde N, Duff C, Jeanneret C, Chandler J G, Seeber P. Late recurrent saphenofemoral junction reflux after ligation and stripping of the greater saphenous vein. J Vasc Surg. 2001;34(2):236–240. doi: 10.1067/mva.2001.115802. [DOI] [PubMed] [Google Scholar]
- 12.Glass G M. Prevention of sapheno-femoral and sapheno-popliteal recurrence of varicose veins by forming a partition to contain neovascularization. Phlebology. 1998;13:3–9. [Google Scholar]
- 13.Turton E P, Scott D J, Richards S P. et al. Duplex-derived evidence of reflux after varicose vein surgery: neoreflux or neovascularisation? Eur J Vasc Endovasc Surg. 1999;17(3):230–233. doi: 10.1053/ejvs.1998.0719. [DOI] [PubMed] [Google Scholar]
- 14.Rij A M van, Jones G T, Hill G B, Jiang P. Neovascularization and recurrent varicose veins: more histologic and ultrasound evidence. J Vasc Surg. 2004;40(2):296–302. doi: 10.1016/j.jvs.2004.04.031. [DOI] [PubMed] [Google Scholar]
- 15.Allegra C, Antignani P L, Carlizza A. Recurrent varicose veins following surgical treatment: our experience with five years follow-up. Eur J Vasc Endovasc Surg. 2007;33(6):751–756. doi: 10.1016/j.ejvs.2006.12.020. [DOI] [PubMed] [Google Scholar]
- 16.Recek C. Saphenofemoral junction ligation supplemented by postoperative sclerotherapy: a review of long-term clinical and hemodynamic results. Vasc Endovascular Surg. 2004;38(6):533–540. doi: 10.1177/153857440403800607. [DOI] [PubMed] [Google Scholar]
- 17.Nyamekye I, Shephard N A, Davies B, Heather B P, Earnshaw J J. Clinicopathological evidence that neovascularisation is a cause of recurrent varicose veins. Eur J Vasc Endovasc Surg. 1998;15(5):412–415. doi: 10.1016/s1078-5884(98)80202-5. [DOI] [PubMed] [Google Scholar]
- 18.Heim D, Negri M, Schlegel U, De Maeseneer M. Resecting the great saphenous stump with endothelial inversion decreases neither neovascularization nor thigh varicosity recurrence. J Vasc Surg. 2008;47(5):1028–1032. doi: 10.1016/j.jvs.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 19.Winterborn R J, Foy C, Heather B P, Earnshaw J J. Randomized trial of flush saphenofemoral ligation for primary great saphenous varicose veins. Eur J Vasc Endovasc Surg. 2008;36:477–484. doi: 10.1016/j.ejvs.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 20.Sheppard M. A procedure for the prevention of recurrent saphenofemoral incompetence. Aust N Z J Surg. 1978;48(3):322–326. doi: 10.1111/j.1445-2197.1978.tb05240.x. [DOI] [PubMed] [Google Scholar]
- 21.Gibbs P J, Foy D M, Darke S G. Reoperation for recurrent saphenofemoral incompetence: a prospective randomised trial using a reflected flap of pectineous fascia. Eur J Vasc Endovasc Surg. 1999;18(6):494–498. doi: 10.1053/ejvs.1999.0906. [DOI] [PubMed] [Google Scholar]
- 22.De Maeseneer M G, Philipsen T E, Vandenbroeck C P. et al. Closure of the cribriform fascia: an efficient anatomical barrier against postoperative neovascularisation at the saphenofemoral junction? A prospective study. Eur J Vasc Endovasc Surg. 2007;34(3):361–366. doi: 10.1016/j.ejvs.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 23.Earnshaw J J, Davies B, Harradine K, Heather B P. Preliminary results of PTFE patch saphenoplasty to prevent neovascularization leading to recurrent varicose veins. Phlebology. 1998;13:10–13. [Google Scholar]
- 24.Bhatti T S, Whitman B, Harradine K, Cooke S G, Heather B P, Earnshaw J J. Causes of re-recurrence after polytetrafluorethylene patch saphenoplasty for recurrent varicose veins. Br J Surg. 2000;87(10):1356–1360. doi: 10.1046/j.1365-2168.2000.01602.x. [DOI] [PubMed] [Google Scholar]
- 25.Winterborn R J, Earnshaw J J. Randomized trial of polytetrafluorethylene patch insertion for recurrent great saphenous varicose veins. Eur J Vasc Endovasc Surg. 2007;34:367–373. doi: 10.1016/j.ejvs.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 26.Recek C. Saphenous reflux as the cause of venous hemodynamic disturbance in primary varicose veins and chronic venous insufficiency (German) Acta Chir Austriaca. 1998;30(2):76–77. [Google Scholar]
- 27.Recek C, Pojer H. Ambulatory pressure gradient in the veins of the lower extremity. Vasa. 2000;29(3):187–190. doi: 10.1024/0301-1526.29.3.187. [DOI] [PubMed] [Google Scholar]
- 28.Schaper W. Collateral circulation: past and present. Basic Res Cardiol. 2009;104(1):5–21. doi: 10.1007/s00395-008-0760-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pipp F, Boehm S, Cai W J. et al. Elevated fluid shear stress enhances postocclusive collateral artery growth and gene expression in the pig hind limb. Arterioscler Thromb Vasc Biol. 2004;24(9):1664–1668. doi: 10.1161/01.ATV.0000138028.14390.e4. [DOI] [PubMed] [Google Scholar]
- 30.Schaper W, Scholz D. Factors regulating arteriogenesis. Arterioscler Thromb Vasc Biol. 2003;23(7):1143–1151. doi: 10.1161/01.ATV.0000069625.11230.96. [DOI] [PubMed] [Google Scholar]
- 31.Resnick N, Gimbrone M A. Hemodynamic forces are complex regulators of endothelial gene expression. FASEB J. 1995;9(10):874–882. doi: 10.1096/fasebj.9.10.7615157. [DOI] [PubMed] [Google Scholar]
- 32.Schierling W, Troidl K, Troidl C, Schmitz-Rixen T, Schaper W, Eitenmüller I K. The role of angiogenic growth factors in arteriogenesis. J Vasc Res. 2009;46(4):365–374. doi: 10.1159/000189797. [DOI] [PubMed] [Google Scholar]