Abstract
Background:
CPAP adherence patterns are often established very early in the course of therapy. Our objective was to quantify patients' perception of CPAP therapy using a 6-item questionnaire administered in the morning following CPAP titration. We hypothesized that questionnaire responses would independently predict CPAP adherence during the first 30 days of therapy.
Methods:
We retrospectively reviewed the CPAP perception questionnaires of 403 CPAP-naïve adults who underwent in-laboratory titration and who had daily CPAP adherence data available for the first 30 days of therapy. Responses to the CPAP perception questionnaire were analyzed for their association with mean CPAP adherence and with changes in daily CPAP adherence over 30 days.
Results:
Patients were aged 52 ± 14 years, 53% were women, 54% were African American, the mean body mass index (BMI) was 36.3 ± 9.1 kg/m2, and most patients had moderate-severe OSA. Four of 6 items from the CPAP perception questionnaire— regarding difficulty tolerating CPAP, discomfort with CPAP pressure, likelihood of wearing CPAP, and perceived health benefit—were significantly correlated with mean 30-day CPAP adherence, and a composite score from these 4 questions was found to be internally consistent. Stepwise linear regression modeling demonstrated that 3 variables were significant and independent predictors of reduced mean CPAP adherence: worse score on the 4-item questionnaire, African American race, and non-sleep specialist ordering polysomnogram and CPAP therapy. Furthermore, a worse score on the 4-item CPAP perception questionnaire was consistently associated with decreased mean daily CPAP adherence over the first 30 days of therapy.
Conclusions:
In this pilot study, responses to a 4-item CPAP perception questionnaire administered to patients immediately following CPAP titration independently predicted mean CPAP adherence during the first 30 days. Further prospective validation of this questionnaire in different patient populations is warranted.
Commentary:
A commentary on this article appears in this issue on page 207.
Citation:
Balachandran JS; Yu X; Wroblewski K; Mokhlesi B. A brief survey of patients' first impression after CPAP titration predicts future CPAP adherence: a pilot study. J Clin Sleep Med 2013;9(3):199-205.
Keywords: Sleep apnea, CPAP adherence, compliance, questionnaire, patient perception
The prevalence of obstructive sleep apnea (OSA) has been well documented1 and is expected to increase as the prevalence of obesity increases.2 Untreated OSA is associated with not just increased cardiovascular3 and metabolic risks,4 but also with myriad comorbidities including decreased quality of life,5 depressed mood,6 decreased cognitive function,7 increased risk of motor vehicle and occupational accidents,8,9 and increased risk of pregnancy complications.10 Though continuous positive airway pressure (CPAP) therapy is highly efficacious11 and is associated with decreased cardiovascular morbidity and mortality12,13 and metabolic morbidity,14,15 treatment effectiveness depends largely on patient adherence, which is often suboptimal.16 Moreover, long-term patient adherence is typically established within the first week of CPAP therapy.17–19
Certain factors have already been associated with poor adherence to CPAP therapy: lack of sleep specialist consultation prior to polysomnogram (PSG),20,21 African American race,20,22 low socioeconomic status,23–25 reduced nasal airway caliber,26 and mask leak,27 to name a few. Social factors, such as living with another person,28 spousal involvement,29 and participation in educational support groups30 are associated with improved CPAP adherence. Other factors, including OSA severity, body mass index (BMI), and the presence of daytime sleepiness, have been studied, and there are conflicting data on their association with adherence to CPAP therapy.31,32
BRIEF SUMMARY
Current Knowledge/Study Rationale: CPAP therapy effectiveness for OSA depends on adherence to therapy. Since CPAP adherence patterns are often established early in treatment, and since interventions exist to improve adherence, there is value in developing simple methods to assess patient attitudes to therapy, ideally at the point of CPAP therapy initiation.
Study Impact: This study demonstrates that a brief assessment of patient perception on the morning after CPAP titration predicts 30-day CPAP adherence, and it extends our current understanding of early assessments of CPAP therapy by examining a female- and African American-predominant patient population. Prospective validation of our brief questionnaire in a larger, more varied population is warranted.
Not surprisingly, patient health belief models, perceptions of OSA risk, expectancies of CPAP therapy and therapy self-efficacy have been shown to be important early predictors of adherence.33,34 At present, most of the existing literature on evaluations of these beliefs and attitudes include lengthy questionnaires33–36 and serial assessments,37 which are useful in a research model but may not be practical in a clinical setting.
Several interventions have been shown to improve CPAP adherence, including cognitive behavioral therapy programs38 and bi-directional telecommunications programs.39–41 Being able to predict a patient's “risk” for poor CPAP adherence early, ideally at the point of CPAP therapy initiation, may be useful in targeting “high-risk” patients for these interventions.
Because patient attitudes are strong early predictors of CPAP adherence, and because targeted interventions exist to improve CPAP adherence, there is a value in developing ways to assess patient attitudes in a simple way. Lewis et al. demonstrated that a single question asked on the morning following CPAP titration predicted CPAP adherence at one month in a cohort of 70 patients in the United Kingdom.28 However, it remains unclear how applicable and generalizable their findings are in populations of different cultural and racial backgrounds, particularly in African Americans. Along these lines, our sleep laboratory had developed a 6-question quality-improvement tool to assess patients' perception of CPAP therapy on the morning following an in-laboratory CPAP titration. Our goal in developing this tool was to have a short questionnaire which could be completed by patients and which could aid in quality improvement in our sleep laboratory. After using this tool for several years, we designed a retrospective pilot study to quantify patients' perception of CPAP therapy based on the responses to the 6-item questionnaire. We hypothesized that responses to these questions would independently predict mean CPAP adherence during the first 30 days of therapy.
METHODS
Patients
We retrospectively evaluated the medical records of 1,126 consecutive, CPAP-naïve adults who were referred to the University of Chicago Sleep Laboratory for their first in-laboratory PSG because of clinical suspicion for OSA between July 2007 and June 2008, and who completed our 6-item questionnaire on the morning following their PSG. Exclusion criteria for these analyses included previous CPAP use, requirement for bilevel positive airway pressure or adaptive servoventilation, central sleep apnea, or lack of adherence data because of a lack of a wireless modem transmission device or faulty wireless modem transmission. The institutional review board of the University of Chicago approved the study, and ethical standards were observed during the investigation. Given the retrospective chart-review nature of the study, the need for informed consent was waived.
Baseline PSG and CPAP Titrations
Patients underwent either an in-laboratory full-night PSG followed by a full-night CPAP titration or a single split-night PSG. Split-night PSGs were performed on patients who had 2-3 h of baseline sleep with an apnea-hypopnea index (AHI) ≥ 30 events/h, if there were at least 3-4 h of titration time remaining. Patients diagnosed with OSA and referred for CPAP therapy had CPAP set up in their homes by a durable medical equipment (DME) provider. PSGs were scored according to the standards issued by the American Academy of Sleep Medicine.42 A hypopnea was scored if the magnitude of ventilation signal decreased by ≥ 50% of the baseline amplitude of the nasal pressure transducer for ≥ 10 sec associated with either an oxygen desaturation ≥ 3% as measured by finger pulse oximetry or a microarousal.
Covariates
On the night of the PSG, patients completed a routine questionnaire which included demographics, medical history, sleep history and self-reported habitual sleep duration, Epworth Sleepiness Scale (ESS),43 and the Center for Epidemiologic Studies Depression (CES-D) Scale.44 Self-reported race was categorized into African American and non-African American. Self-reported education level was categorized into “high school degree or less” and “more than high school degree.” Age, gender, and medical insurance type were obtained from the medical record. Medical insurance was categorized into Medicaid and non-Medicaid. We categorized patients into 2 groups based on the specialty of the physician ordering the PSG: non-sleep specialists or board-certified sleep-specialists.
CPAP Perception Questionnaire
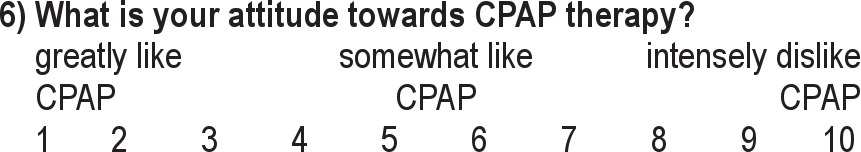
Upon awakening in the sleep laboratory, patients were asked by the sleep laboratory technicians to complete a 6-item questionnaire to quantify overall perception of their first experience with CPAP therapy after a night of titration (Appendix). The questionnaire was developed and implemented as part of a quality improvement initiative in our sleep laboratory to assess patient experiences during their CPAP titration PSGs. These questions were answered on a Likert-type visual analog scale ranging from 1 (no difficulty/no discomfort/positive attitude toward CPAP) to 10 (significant difficulty/significant discomfort/ negative attitude towards CPAP). The questions included: (1) How much difficulty did you have tolerating CPAP? (2) How uncomfortable was the mask? (3) How uncomfortable was the CPAP pressure? (4) What is the likelihood of you wearing the equipment at night almost every night? (5) How beneficial do you think CPAP is going to be for your health and sleep? (6) What is your attitude towards CPAP therapy?
CPAP Adherence
CPAP adherence was determined objectively via wireless modem technology that enabled remote daily downloading of data from the CPAP unit during the first 30 days of use. Only 2 DME providers performed CPAP set up in patients' homes. During the first 30 days of treatment, only the DME providers performed education on CPAP set up and any troubleshooting. The data obtained from each CPAP unit included hours of usage per night at the prescribed pressure, residual daily AHI, and average mask leak.
Statistical Analyses
Each of the 6 questions was subjected to bivariate analyses testing the correlation between question response and 30-day CPAP adherence (mean CPAP usage in minutes over the 30 days). Only questions that were significantly correlated to CPAP adherence were pooled. To validate the internal consistency of the questionnaire, we calculated Cronbach α.45 Factor analysis (principal component analysis) was performed to investigate the dimensionality of the scale.46 The sum of the pooled question responses was used in the analysis after the normality of the score distribution was assessed.
We performed a univariate analysis to evaluate associations between mean CPAP adherence during the first 30 days and important covariates such as the specialty of the physician ordering the PSG, age, gender, race, BMI, education level, insurance status, ESS score, CES-D score, AHI, and the CPAP perception score from the night of in-laboratory titration. We then performed a stepwise linear regression model to identify independent predictors of mean CPAP adherence during the first 30 days of therapy. We included the following variables in the stepwise regression model: specialty of the physician ordering the PSG, age, gender, race, BMI, OSA severity, education level, ESS, CES-D score, insurance status, and the CPAP perception score. The backward selection method was used, as the stepping method criteria variables with p-value ≤ 0.05 were kept in the model and variables with p-value > 0.10 were removed.
As a secondary analysis to evaluate changes in CPAP adherence over time and to confirm the findings of the primary analysis, random-effects regression was used with each patient contributing 30 days of data. Patients were categorized based on the CPAP perception score above or below the mean. Both linear (nightly CPAP usage in minutes) and logistic (nightly CPAP usage ≥ 4 h) models were fit. Lowess smooth curves were added to summary plots to aid in assessment of trends.
A p-value ≤ 0.05 was considered statistically significant. All analyses were performed using PASW Statistics (v.18.0, SPSS, Inc, Chicago IL) and Stata Version 12 (StataCorp., College Station, TX).
RESULTS
Patient Demographics
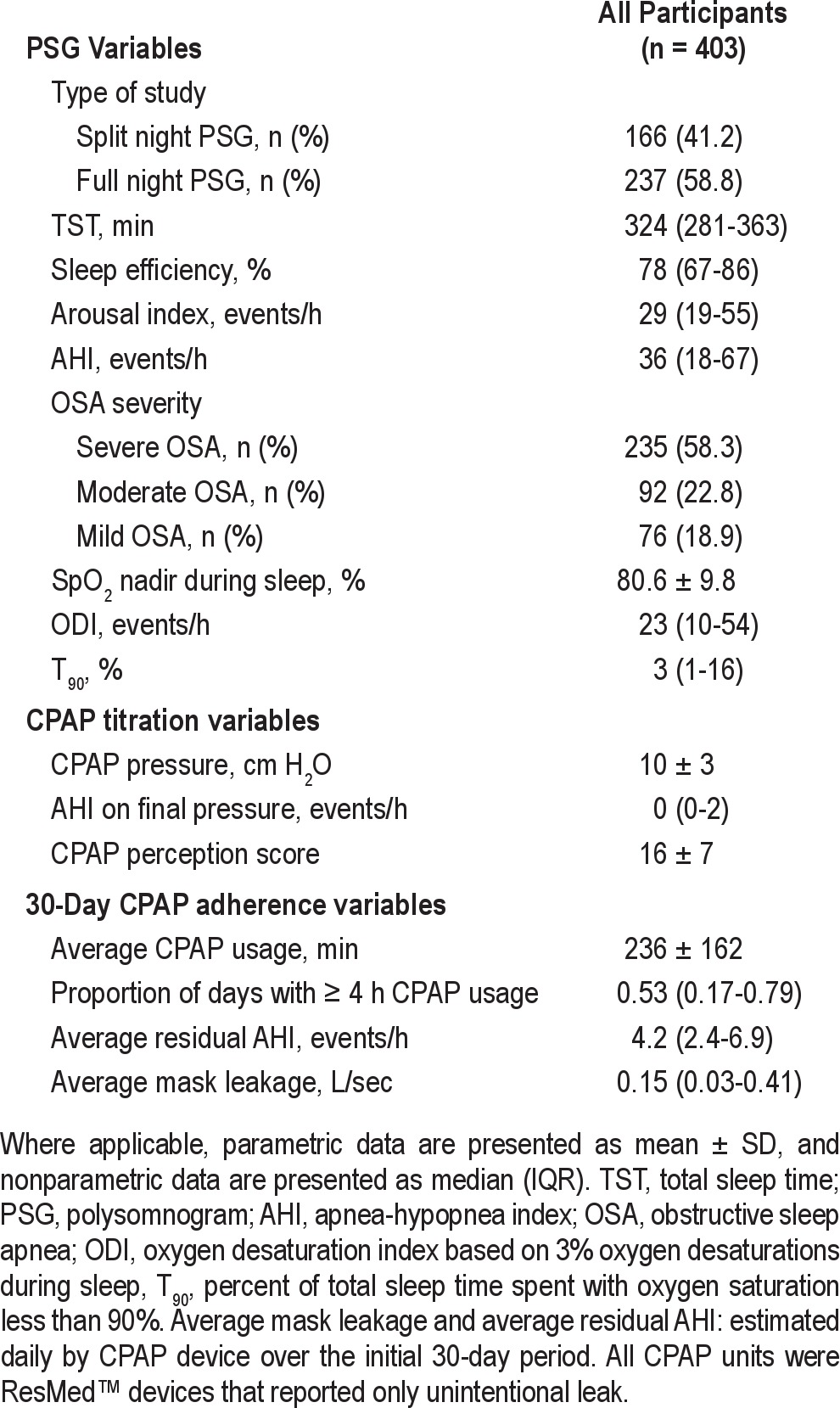
Of the 1,126 consecutive patients evaluated, 786 (70%) underwent CPAP titration. Data on CPAP adherence for the first 30 days were available for analysis in 403 of these patients (Figure 1). Demographic data are summarized in Table 1. The majority of the cohort was obese, African American, middle-aged, with “more than a high school degree” of education, and more than half were women. Medicaid was the only health insurance coverage in 21% of patients. Severe OSA (defined as AHI ≥ 30 events/h) was present in 58% of patients. Mean 30-day CPAP adherence was 236 ± 162 min per day (Table 2). Split-night PSG was performed in 41% of patients. Full-night PSG followed by full-night in-laboratory CPAP titration was performed in 59% of patients. There was no significant difference in mean 30-day CPAP adherence between patients undergoing split-night PSG vs. full-night PSG (p = 0.52). Due to a lack of a wireless modem transmission device or faulty wireless modem transmission, 383 patients were excluded from the final analysis because of lack of CPAP adherence data. These patients did not differ significantly with respect to any demographic category, sleep history, medical history, or PSG characteristic (data not shown).
Figure 1. Study flow diagram illustrating how the final cohort of patients was obtained.
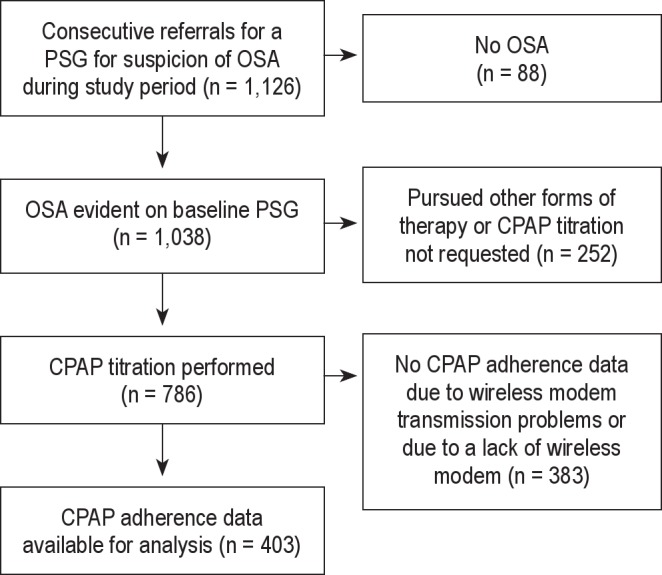
Table 1.
Demographic variables for the entire analytic cohort
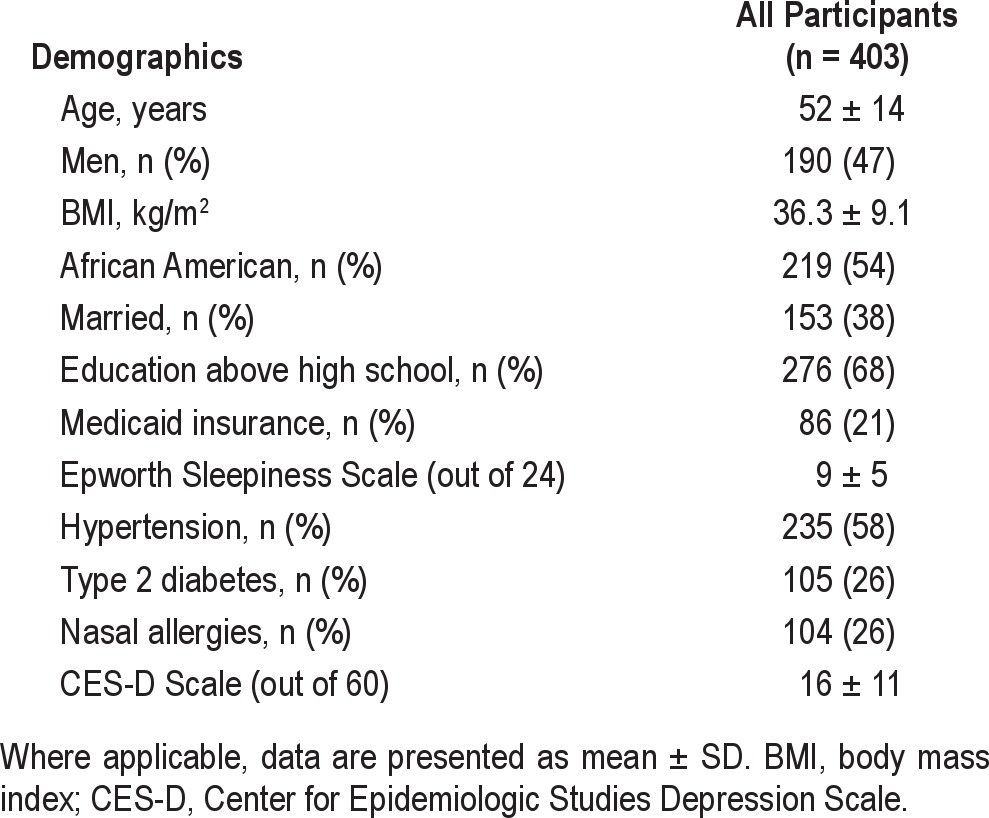
Table 2.
Polysomnographic, CPAP titration, and CPAP adherence data
Questionnaire Responses and Validation
In order to simplify the questionnaire and to identify the most important items, we tested the correlation between each individual question response and mean 30-day CPAP adherence. Only questions 1, 3, 4, and 5—regarding difficulty tolerating CPAP, discomfort with CPAP pressure, likelihood of wearing CPAP, and perceived health benefit—were significantly correlated with CPAP adherence (Pearson correlations and p values: Q1 = -0.122, p = 0.017; Q2 = -0.098, p = 0.057; Q3 = -0.143, p = 0.005; Q4 = -0.160, p = 0.002; Q5 = -0.122, p = 0.020; Q6 = -0.040, p = 0.444). Cronbach α for these 4 questions was 0.73, suggesting good internal consistency. Unidimensionality was confirmed with factor analysis with the first factor accounting for 55% of the total variance. Since each of the 4 question responses had a range of 1 to 10, the sum of responses to these 4 questions (referred to as the CPAP perception score) ranged from 4 to 40. A higher score represented more difficulty with and discomfort tolerating CPAP and a more negative attitude towards CPAP therapy. The mean CPAP perception score was 16 ± 7. The mean CPAP perception score among excluded patients was slightly higher (18 ± 8, p = 0.013). The CPAP perception scores were normally distributed.
Primary Analysis
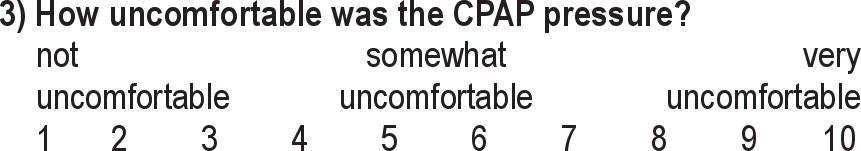
Stepwise linear regression analysis demonstrated that the CPAP perception score significantly predicted mean 30-day CPAP adherence, even after adjusting for specialty of the ordering physician and race (p = 0.007). Other variables considered were dropped from the model due to non-significance, including age, gender, BMI, education, OSA severity, ESS score, CES-D score, and insurance status (Table 3). The unstandardized beta-coefficient for this relationship was -3.3 minutes, suggesting that each point increase in the CPAP perception score was associated with an adjusted reduction in average nightly CPAP use of approximately 3 minutes. This means that all factors being equal, a patient with the maximum score of 40 (indicating the poorest CPAP perception) would be predicted to have approximately 108 minutes less nightly CPAP use than a patient with the minimum score of 4. In addition, in the stepwise linear regression model, only 2 other variables remained significant predictors of mean 30-day CPAP adherence: specialty of the ordering physician and race (Table 3).
Table 3.
Stepwise linear regression model of mean CPAP adherence over the first 30 days of therapy
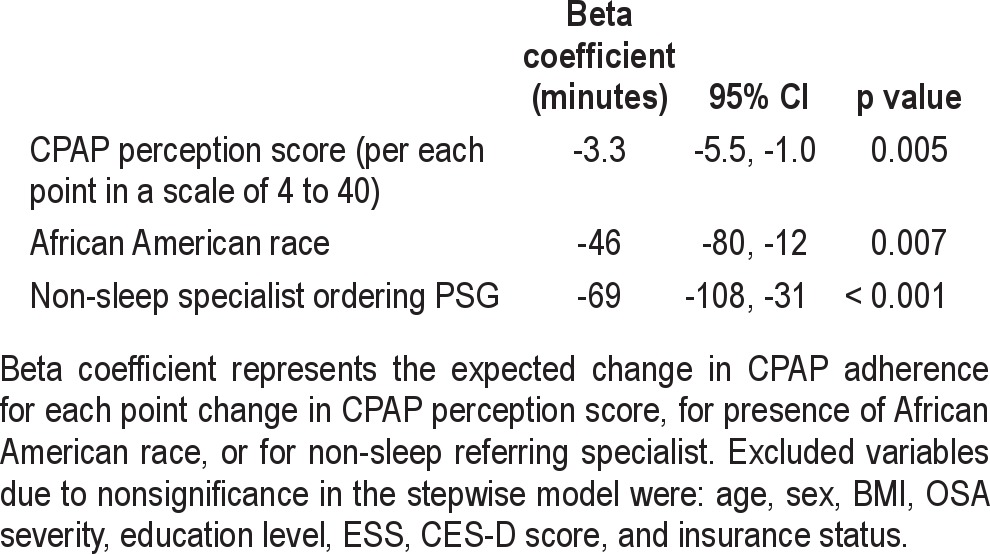
In our cohort, variables that were not predictive of CPAP adherence in the stepwise linear regression analysis were age, gender, BMI, OSA severity, ESS score, CES-D score, education level, and insurance status. Moreover, there was no significant interaction between race or physician specialty and the CPAP perception score. We fit additional stepwise regression models that also included self-reported habitual total sleep duration, type of PSG (split-night versus full-night), DME provider, and average leak as estimated by the CPAP devices; these did not have an impact on the 3 significant variables (CPAP perception score, race, and physician specialty; data not shown).
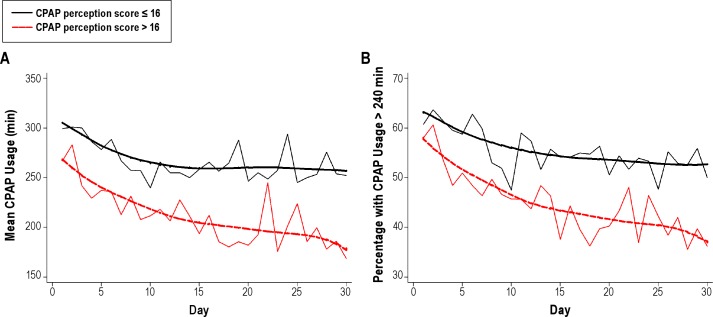
Secondary Analysis
We used the mean CPAP perception score to create 2 categories of patients: poor CPAP perception (scores > 16) and good CPAP perception (scores ≤ 16). Although there was a significant decrease in mean daily CPAP usage over time in both groups (p < 0.001), higher CPAP perception scores were associated with decreased mean daily usage (p = 0.001), and this relationship did not vary significantly over time (p = 0.40 for the time by CPAP perception score interaction) (Figure 2A). Similarly, there was a significant decrease over time in the percentage of patients using CPAP ≥ 4 hours each day (p < 0.001). Higher CPAP perception scores were associated with a decreased likelihood of patients using CPAP for ≥ 4 h each night (p < 0.001), and this relationship did not vary significantly over time (p = 0.15 for the time × CPAP perception score interaction) (Figure 2B).
Figure 2. CPAP perception score predicts nightly CPAP use and percentage of patients with ≥ 4 hours nightly CPAP use.
The mean CPAP perception score was used to create two categories of patients: poor CPAP perception (scores > 16) and good CPAP perception (scores ≤ 16). Higher scores on the CPAP perception score were associated with decreased nightly CPAP usage (A) p = 0.001. Similarly, higher scores on the CPAP perception score were associated with a decreased percentage of patients using CPAP ≥ 4 hours each night (B) p < 0.001. Lowess smooth curves were added to summary plots to aid in assessment of trends.
DISCUSSION
The main finding of our pilot study is that responses to a brief CPAP perception questionnaire administered to patients immediately following an in-laboratory CPAP titration predicts CPAP adherence during the first 30 days, even after adjusting for important covariates. This suggests that a brief, clinical evaluations of patient attitudes regarding CPAP therapy can have important predictive value.
Prior studies have demonstrated that long-term CPAP adherence patterns are often established within the first week of therapy.18,19,36 Moreover, measures of the experience with and benefit perceived from CPAP therapy after just the first night of CPAP titration have been shown to be important factors in determining long-term adherence.28,47 Therefore, assessing this initial night of therapy would be helpful in determining which patients are “at risk,” particularly since effective interventions such as education and support programs exist for increasing CPAP adherence.38–41
Tools for assessing patient perceptions and beliefs about therapy already exist and are very useful for developing a multidimensional understanding of factors related to CPAP adherence.19,33,35 However, most of these assessments are lengthy and may not be practical in a busy clinical setting. Notably, Lewis et al. demonstrated that even a single question on the morning following CPAP titration may predict adherence.28 In this study, the patients were asked a closed-ended simple question: “Have you encountered any problems during this first night of CPAP?'' with two possible responses: “yes” or “no.” Their study, however, included only 70 patients with significant underrepresentation of women (n = 4) and ethnic minorities. In contrast, our pilot study included significant numbers of African Americans and women and demonstrated that a four-question assessment provides a brief and simple method of assessing CPAP therapy perception and significantly predicts mean 30-day CPAP adherence. It is important to note that there are significant similarities between the single closed-ended question asked by Lewis et al. and two of the questions included in our CPAP perception questionnaire that were answered on a Likert scale: “How much difficulty did you have tolerating CPAP?” and “How uncomfortable was the CPAP pressure?” Therefore, our results confirm the findings of Lewis et al., that reporting problems after the first night of CPAP use is an important predictor of poor CPAP adherence.
We initially evaluated responses to six brief questions; of those, two questions—“How uncomfortable was the mask?” and “What is your attitude towards CPAP therapy?”—were not significantly predictive of CPAP adherence. The lack of association between the second question—“How uncomfortable was the mask?”—and CPAP adherence was observed despite the fact that the range of responses to this question was broad. Reasons for this remain unclear, but could be related to subsequent intervention and adjustment of mask fit by DME providers during the first 30 days of therapy. The lack of predictive value with the sixth question—“What is your attitude towards CPAP therapy?”—could be related to patients' unwillingness to voice a negative attitude towards potential therapy. Alternatively, the question may have simply been too vague.
Our group has previously reported that African American race and a non-sleep specialist ordering the PSG and home CPAP therapy were also predictive of decreased CPAP adherence, even after adjusting for relevant covariates.20 Lower CPAP adherence in African Americans has been reported by other groups as well.18,22,48, 49 Whether this finding is related to other factors not captured by education level or insurance status, such as socioeconomic status, health literacy, or health beliefs surrounding CPAP therapy, requires further study. Although it is plausible that CPAP adherence is lower in African Americans because of shorter habitual sleep duration, the impact of race on CPAP adherence remained unchanged when we introduced self-reported habitual sleep duration into the model.
Regarding our finding that a consultation with a sleep specialist prior to undergoing a diagnostic PSG was predictive of increased 30-day CPAP use, it is possible that contact with a sleep specialist may have led to improved patient education, better awareness about OSA and its implications, and emphasis on the importance of CPAP therapy. Other investigators have reported that patients managed by accredited sleep centers have a reduced risk of discontinuing CPAP therapy.21 In spite of this, response patterns to the fifth question—“How beneficial do you think CPAP is going to be for your health and sleep?”—were not different when comparing patients referred by sleep specialists to those referred by non-sleep specialists. This question may not have been sufficient to capture the impact of sleep specialist consultation on patients' CPAP perception.
Our study had several limitations. First, a number of patients were excluded from our analysis due to a lack of objective CPAP adherence data. In all of these cases, the adherence data were missing due to either lack of or malfunction of wireless modem devices. Although there were no significant differences in baseline characteristics of included and excluded patients (suggesting a lack of systematic bias), the mean CPAP perception score was higher in the excluded cohort (18 ± 8 vs. 16 ± 7, p = 0.013). The clinical significance of this difference remains unclear given that the CPAP perception questionnaire has a scale of 4 to 40. Second, ours was a single-center study which limits the generalizability of our findings. Importantly, however, our study did include a substantial proportion of African Americans and women, two patient populations frequently under-studied with respect to CPAP therapy adherence. The retrospective nature of our study may also limit the conclusions that can be drawn about the reported associations. Our findings will therefore need to be validated prospectively in different patient populations.
It should be noted that our questionnaire was developed out of a longstanding quality-improvement initiative to assess patient perception of CPAP therapy after CPAP titration, a practice that is employed in many sleep laboratories. Our findings demonstrate the clinical utility and predictive power of a practical and simple questionnaire for post-CPAP titration assessment of patients' perceptions.
In summary, our pilot study demonstrates that 30-day CPAP adherence can be predicted by a brief assessment of patients' experiences and beliefs performed on the morning after an in-laboratory CPAP-titration. Those patients with scores suggesting an increased risk of non-adherence can then be targeted for interventions designed to improve adherence. Prospective validation of our questionnaire in a larger, more varied population is warranted. In addition, it would be intriguing to assess the utility of this questionnaire in predicting adherence when administered not just on the morning following CPAP titration but also on outpatient follow-up.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Support for this study was provided in part by NIH Grant HD057796.
APPENDIX
Sleep Disorders Center CPAP Questionnaire
Please answer the following questions so we can better understand how you feel about CPAP. Please circle a number from 1 to 10 to indicate your choice for each question.
- 1) How much difficulty did you have tolerating CPAP?
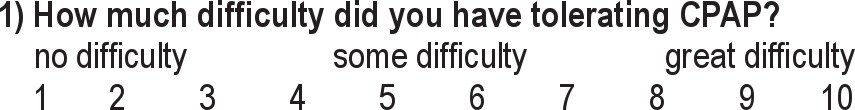
- 2) How uncomfortable was the mask?
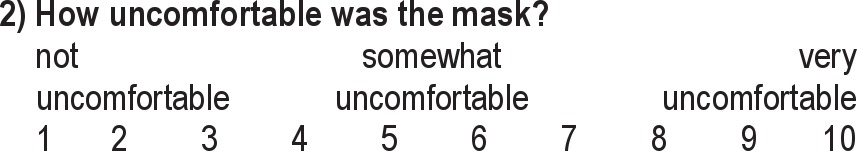
- 3) How uncomfortable was the CPAP pressure?
- 4) What is the likelihood of you wearing the equipment at night almost every night?
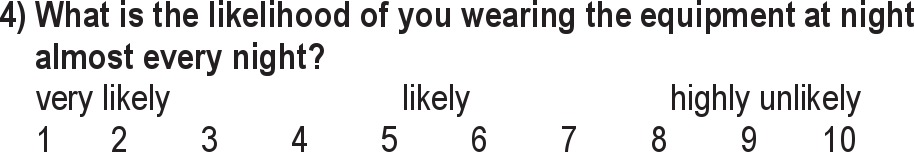
- 5) How beneficial do you think CPAP is going to be for your health and sleep?
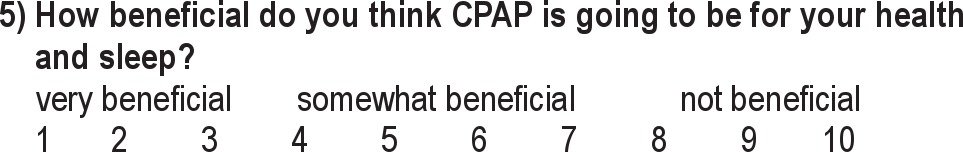
- 6) What is your attitude towards CPAP therapy?
References
- 1.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 2.Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284:3015–21. doi: 10.1001/jama.284.23.3015. [DOI] [PubMed] [Google Scholar]
- 3.Kohli P, Balachandran JS, Malhotra A. Obstructive sleep apnea and the risk for cardiovascular disease. Curr Atheroscler Rep. 2011;13:138–46. doi: 10.1007/s11883-011-0161-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lurie A. Metabolic disorders associated with obstructive sleep apnea in adults. Adv Cardiol. 2011;46:67–138. doi: 10.1159/000325106. [DOI] [PubMed] [Google Scholar]
- 5.Baldwin CM, Griffith KA, Nieto FJ, O'Connor GT, Walsleben JA, Redline S. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep. 2001;24:96–105. doi: 10.1093/sleep/24.1.96. [DOI] [PubMed] [Google Scholar]
- 6.Schröder CM, O'Hara R. Depression and obstructive sleep apnea (OSA) Ann Gen Psychiatry. 2005;4:13. doi: 10.1186/1744-859X-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HC, Young T, Matthews CG, Weber SM, Woodward AR, Palta M. Sleep-disordered breathing and neuropsychological deficits. A population-based study. Am J Respir Crit Care Med. 1997;156:1813–9. doi: 10.1164/ajrccm.156.6.9610026. [DOI] [PubMed] [Google Scholar]
- 8.Masa JF, Rubio M, Findley LJ. Habitually sleepy drivers have a high frequency of automobile crashes associated with respiratory disorders during sleep. Am J Respir Crit Care Med. 2000;162:1407–12. doi: 10.1164/ajrccm.162.4.9907019. [DOI] [PubMed] [Google Scholar]
- 9.Lindberg E, Carter N, Gislason T, Janson C. Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med. 2001;164:2031–5. doi: 10.1164/ajrccm.164.11.2102028. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y-H, Kang J-H, Lin C-C, Wang I-T, Keller JJ, Lin H-C. Obstructive sleep apnea and the risk of adverse pregnancy outcomes. Am J Obstet Gynecol. 2012;206:136.e1–5. doi: 10.1016/j.ajog.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;1:862–5. doi: 10.1016/s0140-6736(81)92140-1. [DOI] [PubMed] [Google Scholar]
- 12.Campos-Rodriguez F, Martinez-Garcia MA, de la Cruz-Moron I, Almeida-Gonzalez C, Catalan-Serra P, Montserrat JM. Cardiovascular mortality in women with obstructive sleep apnea with or without continuous positive airway pressure treatment: a cohort study. Ann Intern Med. 2012;156:115–22. doi: 10.7326/0003-4819-156-2-201201170-00006. [DOI] [PubMed] [Google Scholar]
- 13.Marin JM, Carrizo SJ, Vicente E, Agusti AGN. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 14.Sharma SK, Agrawal S, Damodaran D, et al. CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med. 2011;365:2277–86. doi: 10.1056/NEJMoa1103944. [DOI] [PubMed] [Google Scholar]
- 15.Weinstock TG, Wang X, Rueschman M, et al. A controlled trial of CPAP therapy on metabolic control in individuals with impaired glucose tolerance and sleep apnea. Sleep. 2012;35:617–25. doi: 10.5665/sleep.1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147:887–95. doi: 10.1164/ajrccm/147.4.887. [DOI] [PubMed] [Google Scholar]
- 17.Weaver TE, Kribbs NB, Pack AI, et al. Night-to-night variability in CPAP use over the first three months of treatment. Sleep. 1997;20:278–83. doi: 10.1093/sleep/20.4.278. [DOI] [PubMed] [Google Scholar]
- 18.Budhiraja R, Parthasarathy S, Drake CL, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep. 2007;30:320–4. [PubMed] [Google Scholar]
- 19.Aloia MS, Arnedt JT, Stanchina M, Millman RP. How early in treatment is PAP adherence established? Revisiting night-to-night variability. Behav Sleep Med. 2007;5:229–40. doi: 10.1080/15402000701264005. [DOI] [PubMed] [Google Scholar]
- 20.Pamidi S, Knutson KL, Ghods F, Mokhlesi B. The impact of sleep consultation prior to a diagnostic polysomnogram on continuous positive airway pressure adherence. Chest. 2012;141:51–7. doi: 10.1378/chest.11-0709. [DOI] [PubMed] [Google Scholar]
- 21.Parthasarathy S, Haynes PL, Budhiraja R, Habib MP, Quan SF. A national survey of the effect of sleep medicine specialists and American Academy of Sleep Medicine Accreditation on management of obstructive sleep apnea. J Clin Sleep Med. 2006;2:133–42. [PubMed] [Google Scholar]
- 22.Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34:1653–8. doi: 10.5665/sleep.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Platt AB, Field SH, Asch DA, et al. Neighborhood of residence is associated with daily adherence to CPAP therapy. Sleep. 2009;32:799–806. doi: 10.1093/sleep/32.6.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bakker JP, O'Keeffe KM, Neill AM, Campbell AJ. Ethnic disparities in CPAP adherence in New Zealand: effects of socioeconomic status, health literacy and self-efficacy. Sleep. 2011;34:1595–603. doi: 10.5665/sleep.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32:545–52. doi: 10.1093/sleep/32.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li H-Y, Engleman H, Hsu C-Y, et al. Acoustic reflection for nasal airway measurement in patients with obstructive sleep apnea-hypopnea syndrome. Sleep. 2005;28:1554–9. doi: 10.1093/sleep/28.12.1554. [DOI] [PubMed] [Google Scholar]
- 27.Valentin A, Subramanian S, Quan SF, Berry RB, Parthasarathy S. Air leak is associated with poor adherence to autoPAP therapy. Sleep. 2011;34:801–6. doi: 10.5665/SLEEP.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lewis KE, Seale L, Bartle IE, Watkins AJ, Ebden P. Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep. 2004;27:134–8. doi: 10.1093/sleep/27.1.134. [DOI] [PubMed] [Google Scholar]
- 29.Baron KG, Gunn HE, Czajkowski LA, Smith TW, Jones CR. Spousal Involvement in CPAP: does pressure help? J Clin Sleep Med. 2012;8:147–53. doi: 10.5664/jcsm.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Russo-Magno P, O'Brien A, Panciera T, Rounds S. Compliance with CPAP therapy in older men with obstructive sleep apnea. J Am Geriatr Soc. 2001;49:1205–11. doi: 10.1046/j.1532-5415.2001.49238.x. [DOI] [PubMed] [Google Scholar]
- 31.Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15:343–56. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245–58. [PMC free article] [PubMed] [Google Scholar]
- 33.Weaver TE, Maislin G, Dinges DF, et al. Self-efficacy in sleep apnea: instrument development and patient perceptions of obstructive sleep apnea risk, treatment benefit, and volition to use continuous positive airway pressure. Sleep. 2003;26:727–32. doi: 10.1093/sleep/26.6.727. [DOI] [PubMed] [Google Scholar]
- 34.Olsen S, Smith S, Oei T, Douglas J. Health belief model predicts adherence to CPAP before experience with CPAP. Eur Respir J. 2008;32:710–7. doi: 10.1183/09031936.00127507. [DOI] [PubMed] [Google Scholar]
- 35.Moran AM, Everhart DE, Davis CE, Wuensch KL, Lee DO, Demaree HA. Personality correlates of adherence with continuous positive airway pressure (CPAP) Sleep Breath. 2011;15:687–94. doi: 10.1007/s11325-010-0422-8. [DOI] [PubMed] [Google Scholar]
- 36.Stepnowsky CJ, Jr, Marler MR, Ancoli-Israel S. Determinants of nasal CPAP compliance. Sleep Med. 2002;3:239–47. doi: 10.1016/s1389-9457(01)00162-9. [DOI] [PubMed] [Google Scholar]
- 37.Aloia MS, Arnedt JT, Stepnowsky C, Hecht J, Borrelli B. Predicting treatment adherence in obstructive sleep apnea using principles of behavior change. J Clin Sleep Med. 2005;1:346–53. [PubMed] [Google Scholar]
- 38.Richards D, Bartlett DJ, Wong K, Malouff J, Grunstein RR. Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep. 2007;30:635–40. doi: 10.1093/sleep/30.5.635. [DOI] [PubMed] [Google Scholar]
- 39.Smith CE, Dauz ER, Clements F, et al. Telehealth services to improve nonadherence: A placebo-controlled study. Telemed J E Health. 2006;12:289–96. doi: 10.1089/tmj.2006.12.289. [DOI] [PubMed] [Google Scholar]
- 40.Sparrow D, Aloia M, Demolles DA, Gottlieb DJ. A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomised controlled trial. Thorax. 2010;65:1061–6. doi: 10.1136/thx.2009.133215. [DOI] [PubMed] [Google Scholar]
- 41.Fox N, Hirsch-Allen AJ, Goodfellow E, et al. The impact of a telemedicine monitoring system on positive airway pressure adherence in patients with obstructive sleep apnea: a randomized controlled trial. Sleep. 2012;35:477–81. doi: 10.5665/sleep.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iber C, Ancoli-Israel S, Chesson A, Quan S. The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 43.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 44.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 45.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 46.Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994. [Google Scholar]
- 47.Drake CL, Day R, Hudgel D, et al. Sleep during titration predicts continuous positive airway pressure compliance. Sleep. 2003;26:308–11. doi: 10.1093/sleep/26.3.308. [DOI] [PubMed] [Google Scholar]
- 48.Means MK, Ulmer CS, Edinger JD. Ethnic differences in continuous positive airway pressure (CPAP) adherence in veterans with and without psychiatric disorders. Behav Sleep Med. 2010;8:260–73. doi: 10.1080/15402002.2010.509255. [DOI] [PubMed] [Google Scholar]
- 49.Joo MJ, Herdegen JJ. Sleep apnea in an urban public hospital: assessment of severity and treatment adherence. J Clin Sleep Med. 2007;3:285–8. [PMC free article] [PubMed] [Google Scholar]