Abstract
Study Objectives:
(1) Present preliminary psychometrics for the Children's Report of Sleep Patterns (CRSP), a three-module measure of Sleep Patterns, Sleep Hygiene, and Sleep Disturbance; and (2) explore whether the CRSP provides information about a child's sleep above and beyond parental report.
Methods:
A multi-method, multi-reporter approach was used to validate the CRSP with 456 children aged 8-12 years (inclusive). Participants were recruited from pediatricians' offices, sleep clinics/laboratories, children's hospitals, schools, and the general population. Participants completed measures of sleep habits, sleep hygiene, anxiety, and sleepiness, with actigraphy and polysomnography used to provide objective measures of child sleep.
Results:
The CRSP demonstrated good reliability and validity. Differences in sleep hygiene and sleep disturbances were found for children presenting to a sleep clinic/laboratory (vs. community population); for younger children (vs. older children); and for children who slept less than 8 hours or had a sleep onset later than 22:00 on actigraphy. Further, significant associations were found between the CRSP and child-reported anxiety or sleepiness. Notably, approximately 40% of parents were not aware of child reported difficulties with sleep onset latency, night wakings, or poor sleep quality.
Conclusions:
The three modules of the CRSP can be used together or independently, providing a reliable and valid self-report measure of sleep patterns, sleep hygiene, and sleep disturbances for children ages 8-12 years. Children not only provide valid information about their sleep, but may provide information that would not be otherwise captured in both clinical and research settings if relying solely on parental report.
Citation:
Meltzer LJ; Avis KT; Biggs S; Reynolds AC; Crab-tree VM; Bevans KB. The Children's Report of Sleep Patterns (CRSP): a self-report measure of sleep for school-aged children. J Clin Sleep Med 2013;9(3):235-245.
Keywords: Children, sleep, sleep hygiene, sleep patterns, sleep disturbances, validation, measurement, self-report
Sleep is a highly complex physiological process that accounts for approximately 40% of a child's life by the age of 18 years.1 Obtaining sufficient sleep is important for multiple aspects of health and well-being in children. Disturbed or insufficient sleep has been associated with obesity2–5; poorer cognitive functioning, including learning, attention, and school performance6–9; difficulties with emotion regulation, including symptoms of depression and anxiety10–12; and disrupted family functioning.13 Thus, it is important to have measures that capture different aspects of children's sleep.
In 2003, the NIH's National Center for Sleep Disorders issued a research plan that called for development of new measures of pediatric sleep to advance clinical and outcomes research.14 Sleep is assessed in children with objective monitoring, sleep diaries, and questionnaires. While polysomnography is generally considered the gold standard for the assessment of sleep disordered breathing, it is limited by cost, availability, and the lack of data on the subjective experience of sleep quality. Similarly, although actigraphy can provide an estimate of sleep continuity for extended periods, it provides no information on subjective sleep quality or sleep hygiene, which requires direct input from children and parents. As of 2011, more than 180 patient-reported measures had been developed to assess pediatric sleep; while there are several adolescent self-report measures, very few measures have been validated for children ages 8-12 years.15
BRIEF SUMMARY
Current Knowledge/Study Rationale: Children as young as 8 years old can report on their own health, yet few self-report sleep measures exist for 8-12 year old children. The Children's Report of Sleep Patterns (CRSP) was developed to provide a multi-dimensional self-report questionnaire for school-aged children.
Study Impact: This study demonstrates that the CRSP is a valid and reliable self-report measure of sleep patterns, sleep hygiene, and sleep disturbances in school-aged children. This measure can provide complementary information to parental report in both clinical settings and research studies.
Children as young as 8 years of age can provide reliable, valid, and meaningful reports of health when developmentally appropriate assessment methods are applied.16 A recent Good Research Practices Task Force Report from the International Society of Pharmacoeconomics and Outcomes Research reported on the feasibility and reliability of self-reports in children 8 years and older.17 Specifically, they discussed how children in this age group have the cognitive capacity to understand health vocabulary and/or disease concepts,18 as shown with both cognitive interviews19 and when using Likert scales.20–22
While none of these studies looked at sleep constructs per se, several studies have found that child report can provide information that is useful and unique from parental report. Indeed, the inclusion of children's perspectives about sleep may provide insight in both clinical and research settings that may be missed if relying solely on parental report. One study found that in the absence of children's report, one-third of sleep problems may go unidentified.23 Despite the literature suggesting the value of child report, the need remains for a comprehensive self-report measure of children's sleep that provides an accompanying view to parental report.14,23,24 Because of the need for a well-validated self-report measure of sleep in children ages 8-12 years, we developed the Children's Report of Sleep Patterns (CRSP), a questionnaire that includes three modules (Sleep Patterns, Sleep Hygiene Index, Sleep Disturbances Scale) that can be used independently or in combination. Based on the existing literature, clinical experience, and interviews with pediatric sleep experts, these three modules were chosen due to their potential to identify sleep problems or insufficient sleep.
As children get older, sleep patterns change with later bedtimes and less parental involvement with the child's sleep routine.8,24–26 Although parents may have a good sense of the child's bedtime and wake time, they may not be aware of what happens once the child tries to fall asleep or during the night.23,24 For example, more than 60% of 5th graders in one study reported being awake at least several nights per week when parents thought they were asleep.27 As parents may not be aware of later bedtimes, difficulties falling asleep, or night wakings that can contribute to insufficient sleep, children's self-report of sleep patterns should be considered.
A limited number of published studies have examined sleep hygiene (e.g., caffeine, technology in the bedroom) in children and adolescents.28–31 However, to our knowledge, no studies have examined the self-reported sleep hygiene of typically developing healthy children. Since parents may be unaware of certain aspects of children's sleep hygiene (e.g., caffeine consumption during the day or technology usage in the bedroom), it is important to include sleep hygiene in a self-report measure for children as young as 8 years.
For sleep disturbances, such as sleep disordered breathing or partial arousal parasomnias, parental report is likely to be more accurate than child report, since the child may be unaware of snoring at night or sleepwalking on occasion. However, for disorders of initiating and maintaining sleep, sleep-wake transition, or sleep arousal, children's reports may provide complementary information.23,24,32 In addition, unless asked, children may not report discomfort that they experience at bedtime or during the night, and as such parents may be unaware of it. This discomfort could be symptomatic of restless legs syndrome or another underlying cause of sleep disruptions (e.g., pain). In one study, nearly one-third of children reported significant body pains during the night that the parents were not aware of.24 Thus, there is a need for a measure that asks children directly about symptoms of sleep disturbances.
This report provides preliminary psychometrics for the Children's Report of Sleep Patterns (CRSP), a multidimensional self-report measure for children that provides a complementary report for clinicians and researchers. This paper addresses two questions: (1) Is the CRSP a valid and reliable self-report measure of sleep for children? and (2) Does the inclusion of a child self-report measure such as the CRSP provide information about a child's sleep that enhances parental report and/or would not be captured by parental report alone?
METHODS
Participants
Six hundred seventy children were recruited from the following settings: (1) primary care pediatricians' offices, (2) an outpatient pediatric sleep clinic, (3) community flyers and advertisements, (4) two independent Australian schools, (5) two different pediatric sleep laboratories, and (6) outpatient clinics or inpatient units of a children's hospital for oncology patients (Table 1). Institutional review board approval was obtained for each individual site, and informed consent/assent was obtained from all participants.
Table 1.
Demographic information about study participants and inclusion in psychometric analyses
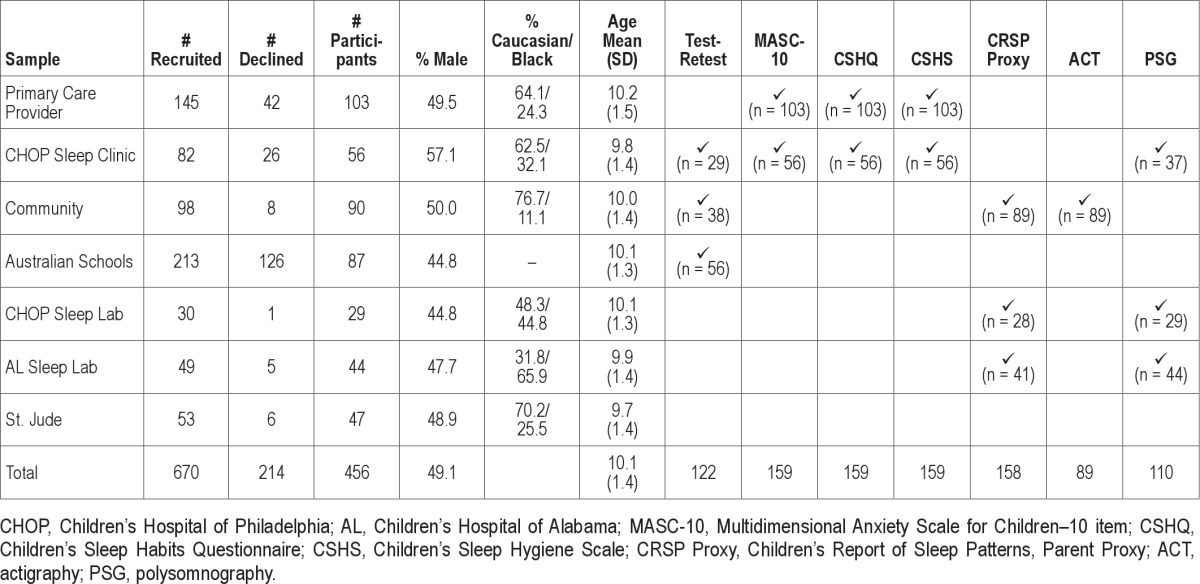
A total of 456 children completed the Children's Report of Sleep Patterns (CRSP), a 68% participation rate. Children who completed the CRSP were 49% male, had a mean age 10.1 (1.4) years (range 8-12 years inclusive, distributed across ages: 8 years = 16.7%, 9 years = 22.6%, 10 years = 21.3%, 11 years = 16.0%, 12 years = 23.5%), and were 62.6% White, 29.0% Black, 4.1% Hispanic, 1.6% Asian, and 2.8% Other. The most common reasons for not participating were not enough time or not interested. No significant difference between participants and non-participants was found for any demographic variable, including age distribution. Complete demographic information is seen in Table 1. Information about race was not collected for the Australian sample.
Measures
While all participants completed the CRSP, other measures were not uniformly collected across sites. Table 1 shows the different measures completed by each group of participants.
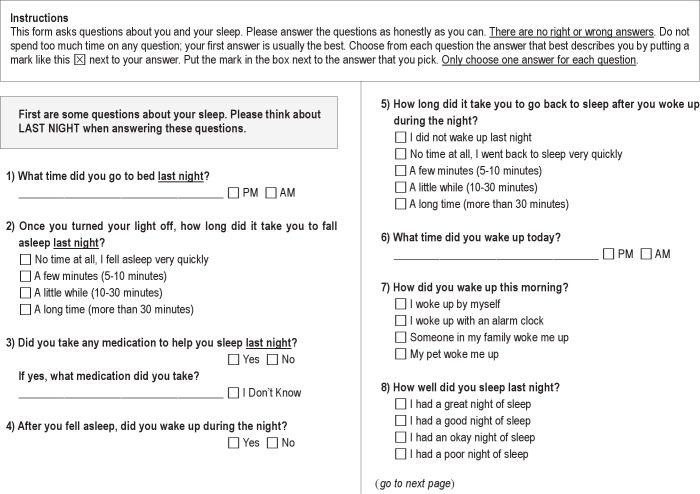
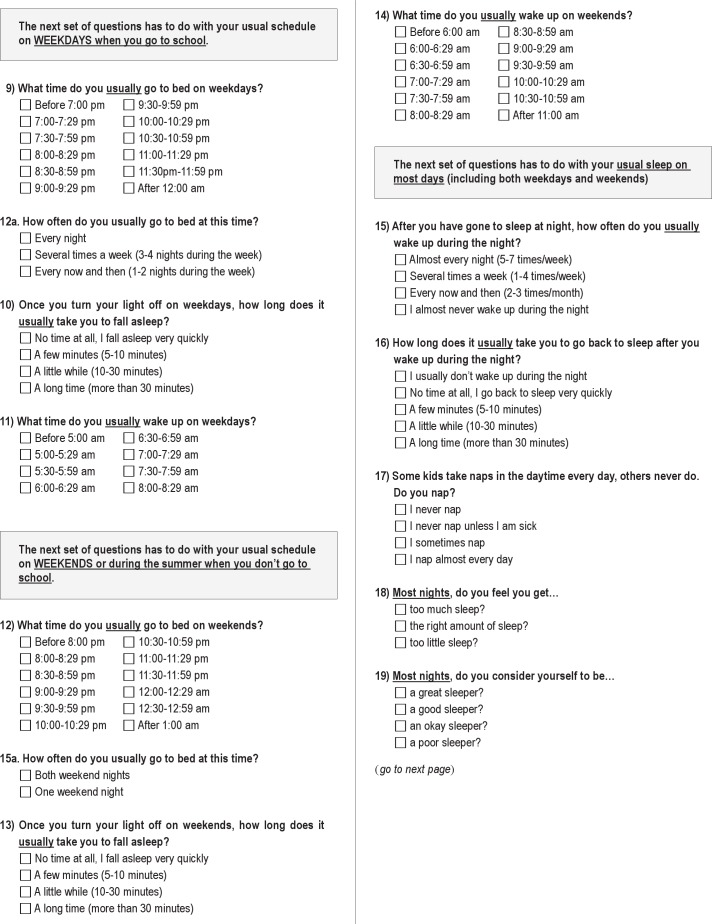
Children's Report of Sleep Patterns (CRSP)
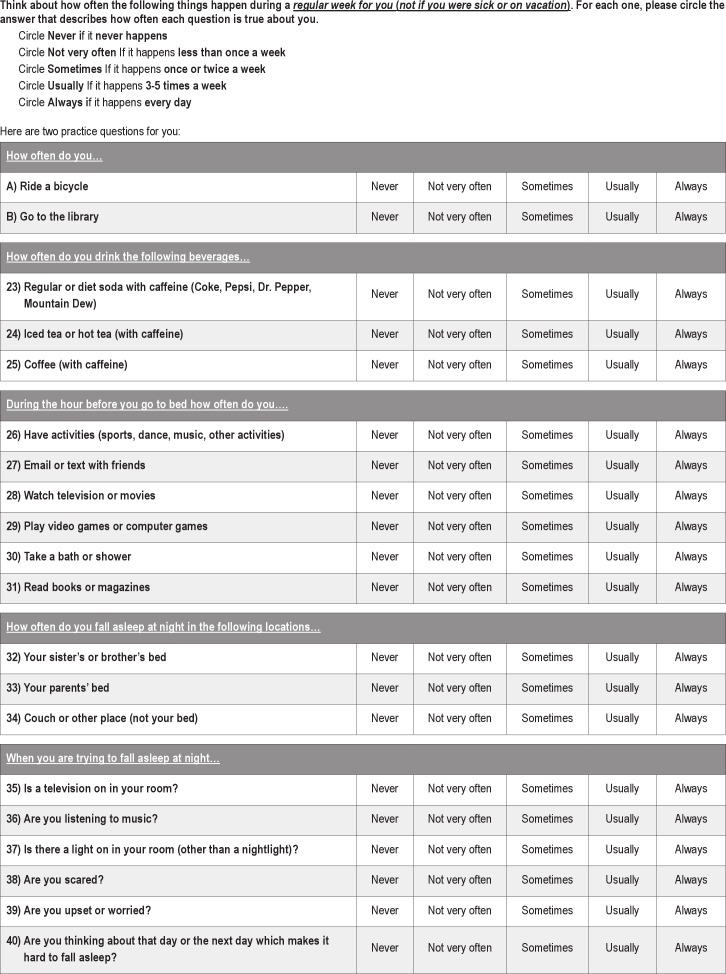
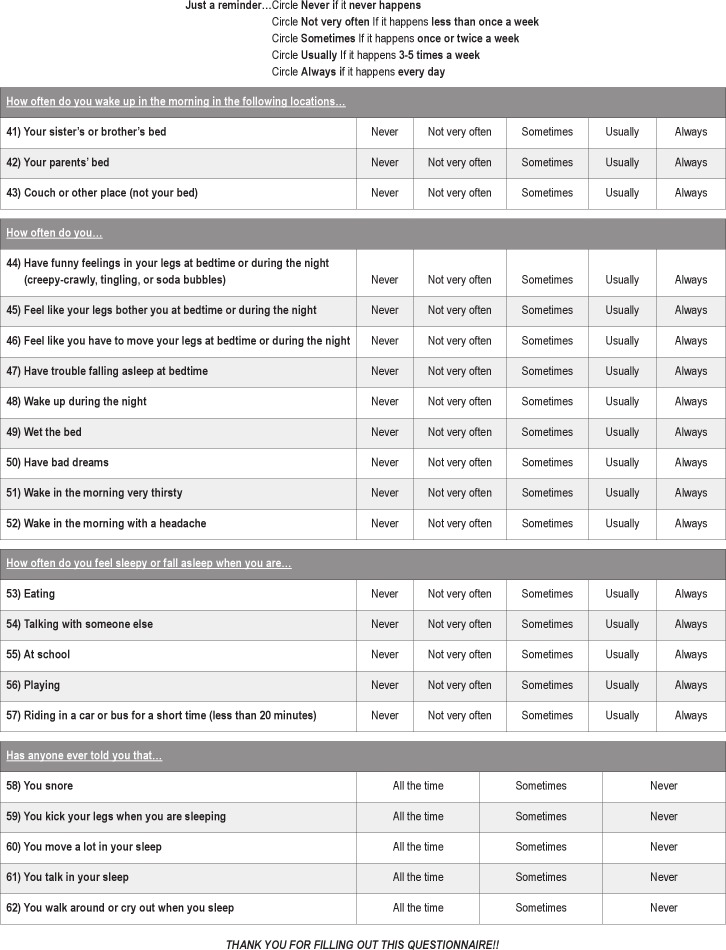
The Children's Report of Sleep Patterns (CRSP) is a 60-item questionnaire that has 3 modules: Sleep Patterns, Sleep Hygiene Index, and Sleep Disturbance Scale (Appendix). Sleep Patterns includes questions about bedtimes, wake times, sleep onset latency, night waking frequency and duration, naps, sleep schedule variability, and subjective sleep quality, with separate questions for last night, typical weekdays when the child is in school, typical weekends/holidays when the child is not in school, and overall sleep “most days.” The Sleep Hygiene Index included questions about caffeine use, activities in the hour before bed, sleep location (where child falls asleep and wakes up), and electronics used at the time of sleep onset. The Sleep Disturbance Scale had questions about bedtime fears/worries, restless legs syndrome symptoms, parasomnias, and insomnia. Additional indicator items were included for snoring, enuresis, and nightmares. Higher scores indicate poorer sleep hygiene or greater sleep disturbances.
The Sleep Hygiene Index and Sleep Disturbance Scale questions were asked in regards to a typical week. For most items the following Likert-type scale was used: “Never” (never happens), “Not very often” (less than once a week), “Sometimes” (once or twice a week), “Usually” (3-5 times a week), or “Always” (every day). For 5 sleep disturbance items that occur during sleep (snoring, kicking, restless sleep, sleep talking, sleepwalking/ terrors), children were asked if anyone told them that they engaged in these behaviors. Answer choices were: “All the time,” “Sometimes,” or “Never.”
Items were developed based on the existing literature and clinical experience of the investigators. Once developed, a group of 15 pediatric sleep experts (physicians, nurses, and psychologists) reviewed the items and were asked to place each item into one of the 3 modules (Sleep Patterns, Sleep Hygiene Index, Sleep Disturbance Scale), and then into the specific indices/scales (e.g., Caffeine Use, Restless Legs). All items had > 53% agreement across experts, with the majority (77%) of items achieving consensus rates of 87% or above.
Children's Report of Sleep Patterns–Parent Proxy
A parent proxy version of the CRSP was also administered to a subset of parents in both community and sleep laboratory populations (n = 158). This proxy version was used to measure convergent validity. No significant differences were found between children whose parents completed the CRSP Proxy and children whose parents did not complete the CRSP Proxy.
Children's Report of Sleep Patterns–Sleepiness Scale
The Children's Report of Sleep Patterns–Sleepiness Scale (CRSP-S) has 5 items that ask children to recall how often they felt sleepy or fell asleep in different situations (at school, during short car rides, while playing, while eating, and while talking).33 Higher scores indicate more sleepiness.
Multidimensional Anxiety Scale for Children–10 Item
The Multidimensional Anxiety Scale for Children–10 item (MASC-10) is a child self-report measure of anxiety.34 This well-validated measure has been used as a screening tool in both clinical and research settings.35 The 10 items are summed to provide a single score, which is then translated to a standard T-score. The MASC-10 was used as a measure of construct validity in a subset of 159 participants in pediatricians' offices or an outpatient sleep clinic.
Children's Sleep Habits Questionnaire (CSHQ)
The Children's Sleep Habits Questionnaire (CSHQ) is a 45-item parent-report measure of children's sleep.36 Parents are asked to recall sleep behaviors during a typical recent week. The CSHQ has demonstrated adequate reliability (coefficient α 0.68 to 0.78, test-retest 0.62 to 0.79) and validity, differentiating between children with and without sleep disorders.24,36 For the current study, subscale scores and the total Sleep Disturbances score were used to examine construct validity. For the CSHQ, higher scores indicate greater sleep disturbances. The CSHQ was completed by a subset of 159 parents in pediatricians' offices and an outpatient pediatric sleep clinic.
Children's Sleep Hygiene Scale
The Children's Sleep Hygiene Scale (CSHS) is a 22-item parent-report measure of children's sleep hygiene. This measure has demonstrated adequate reliability (coefficient α 0.60 to 0.86) in studies of children and adolescents.37 Subscale scores of the CSHS (physiological, cognitive, environmental, emotional, bedtime routines, sleep stability) were used to examine construct validity. For the CSHS, higher scores suggest better sleep hygiene. The CSHS was completed by a subset of 159 parents in the pediatricians' offices and outpatient pediatric sleep clinic.
Actigraphy
The Micro Motionlogger Sleep Watch (Ambulatory Monitoring Inc., Ardsley, NY) was worn by 90 children (recruited from the community through advertisements and peer-nominations) for one week on their nondominant wrist. Data were excluded for one participant due to a device failure (n = 1), resulting in usable actigraphy data for 89 children. Data were collected in 1-min epochs using the zero crossing mode and the Sadeh algorithm.38 Sleep onset time and sleep offset time were manually scored using the 3/5-minute rule (first min of 3 consecutive min of sleep for sleep onset, last minute of 5 consecutive min of sleep for sleep offset).39 Participants pressed an event marker to indicate the time they attempted to fall asleep at night and the time they woke in the morning. In addition, participants kept a concurrent daily sleep diary that was used to facilitate the scoring of sleep intervals and identify artifact. Measures derived for this study were sleep onset time, sleep offset time, and total sleep time (TST: minutes of sleep from sleep onset to sleep offset).
Polysomnography
Overnight polysomnography (PSG) was performed on 110 clinically referred children using either the Rembrandt polysomnography system (n = 61; Embla, Broomfield, CO) or the Sandman 9.2 PSG system (n = 49; Embla, Broomfield, CO). Recorded parameters included electroencephalography (F3-M2, F4-M1, C3-M2, C4-M1, O1-M2, O2-M1); left and right electrooculogram; submental electromyogram; bilateral tibial electromyogram; electrocardiogram; oronasal airflow with 3-pronged thermistor; nasal pressure with pressure transducer; rib cage and abdominal wall motion via respiratory impedance plethysmography; and end-tidal capnometry. Arterial oxygen saturation with pulse waveform was also recorded, as well as digital video and audio. Studies were scored based on American Academy of Sleep Medicine (AASM) pediatric criteria.40 The apnea-hypopnea index (AHI) was the primary variable of interest, with the AHI also providing severity of obstructive sleep apnea (no OSA: AHI < 1.5; mild OSA: AHI = 1.5-5, moderate/ severe OSA: AHI > 5).
Data Analyses
Composite scores were created for each of the 4 Sleep Hygiene indices and 4 Sleep Disturbances scales. Preliminary analyses were conducted to examine age differences across groups used for comparison (e.g., clinical vs. community, > or < 8 h of actigraphic recorded sleep). If significant differences were found, age was controlled for (ANCOVA) in those analyses.
Reliability and Validity of CRSP
Reliability
Cronbach α coefficients were used to measure internal consistency for the individual Sleep Disturbance scales. Because there were multiple indicators for each Sleep Hygiene index score that may not be related (e.g., a child who drinks soda may not also drink tea or coffee, but together these items indicate the frequency of caffeine use), we did not evaluate the internal consistency for sleep hygiene indices. Test-retest reliability (n = 123, mean days between administration = 19.2, range 7-28 days) was examined with Pearson correlation coefficients for indices/scales and Spearman rank order correlations for the individual items; paired t-tests were used to compare time 1 and time 2 sleep hygiene indices and sleep disturbances scales.
Validity
Primary analyses including the full sample examined construct validity with group comparisons for the index/scale scores using ANOVA or ANCOVA (n = 456). Comparisons were made for group (clinical vs. community); age (8-10 years vs. 11-12 years); typical sleep quality (great/good vs. okay/ poor); and typical nap frequency (always/sometimes vs. never/ only when sick). Based on clinical experience, it was expected that more sleep disturbances would be reported in the clinical sample, that poorer sleep hygiene would be reported in older children, and that more sleep disturbances and poorer sleep hygiene would be reported in children with poor sleep quality or children who nap more frequently.
Convergent and divergent validity were further evaluated with Pearson correlation examining the association between the index/scale scores and both child-reported daytime sleepiness (n = 456) and child-reported anxiety (n = 159).
Secondary analyses to examine criterion validity were conducted with subsamples of the study population. For children who wore actigraphy (n = 89), one-way ANOVA or ANCOVA was used to examine differences in sleep hygiene and sleep disturbances between (1) children getting < and > 8 h of sleep (per actigraphy) and (2) children with a sleep onset time before and after 22:00 (per actigraphy, time determined by median split). Further, differences in actigraphic sleep onset time, sleep offset time, and TST were examined with one-way ANOVA for children who napped regularly (sometimes/always) versus infrequently (never/only when sick). For children who had overnight PSG (n = 110), one-way ANOVA was used to examine differences in sleep hygiene and sleep disturbances for children without OSA (AHI < 1.5), mild OSA (AHI 1.5-5), and moderate/severe OSA (AHI > 5); and Pearson correlation was used to examine the association between child reported sleep disturbances and AHI.
Parent-completed legacy measures (CSHQ and CSHS) were also used to examine validity. Pearson correlation was used to examine the association between child-reported sleep (CRSP) and parent-reported sleep patterns and sleep disturbances (CSHQ, n = 159), as well as the association between child-reported (CRSP) and parent-reported sleep hygiene (CSHS, n = 159). In addition, one-way ANCOVA was used to examine differences in sleep hygiene and sleep disturbances for children scoring above and below the clinical cutoff of 41 on the CSHQ.
Value Added of Child Self-Report of Sleep
The value of child report was examined 2 ways. First, using the question “Most nights do you consider yourself to be a _____ sleeper” (great/good, okay/poor), differences in parental report of sleep (CSHQ and CRSP) were examined. Second, Cohen κ was used to examine interrater reliability for sleep pattern variables (Child CRSP and parent proxy CRSP, n = 156; questions about “Last Night”: sleep onset latency [SOL], night waking frequency, and sleep quality; as well as questions about “Typical Night”: weekday bedtime, wake time, night waking frequency, and sleep quality). The mean, standard deviation, intraclass correlations, and effect size were used to examine parent-child agreement for the Sleep Hygiene Indices and the Sleep Disturbances Scales.
RESULTS
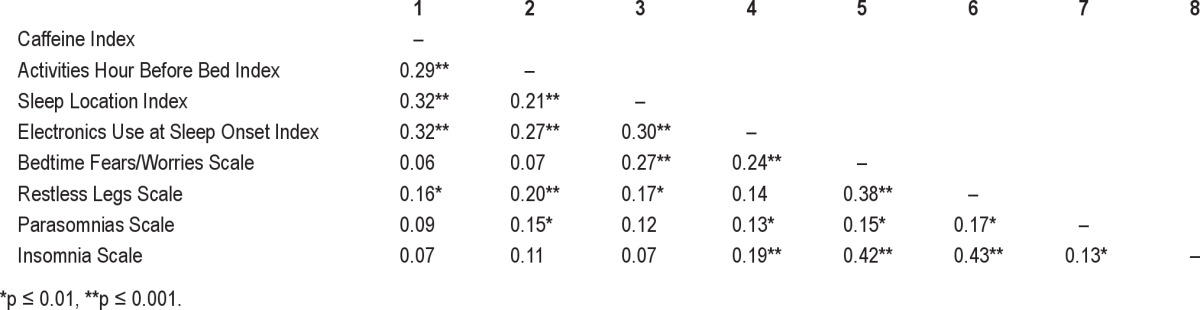
Means and standard deviations for individual items, Sleep Hygiene Indices, and Sleep Disturbance Scales can be found in Table 2; a correlation matrix for the indices/scales can be found in Table 3.
Table 2.
Descriptive statistics (mean, SD), internal consistency (coefficient α), correlations and paired t-tests for CRSP Sleep Hygiene Indices and Sleep Disturbances Scales for the full sample and test-retest sample
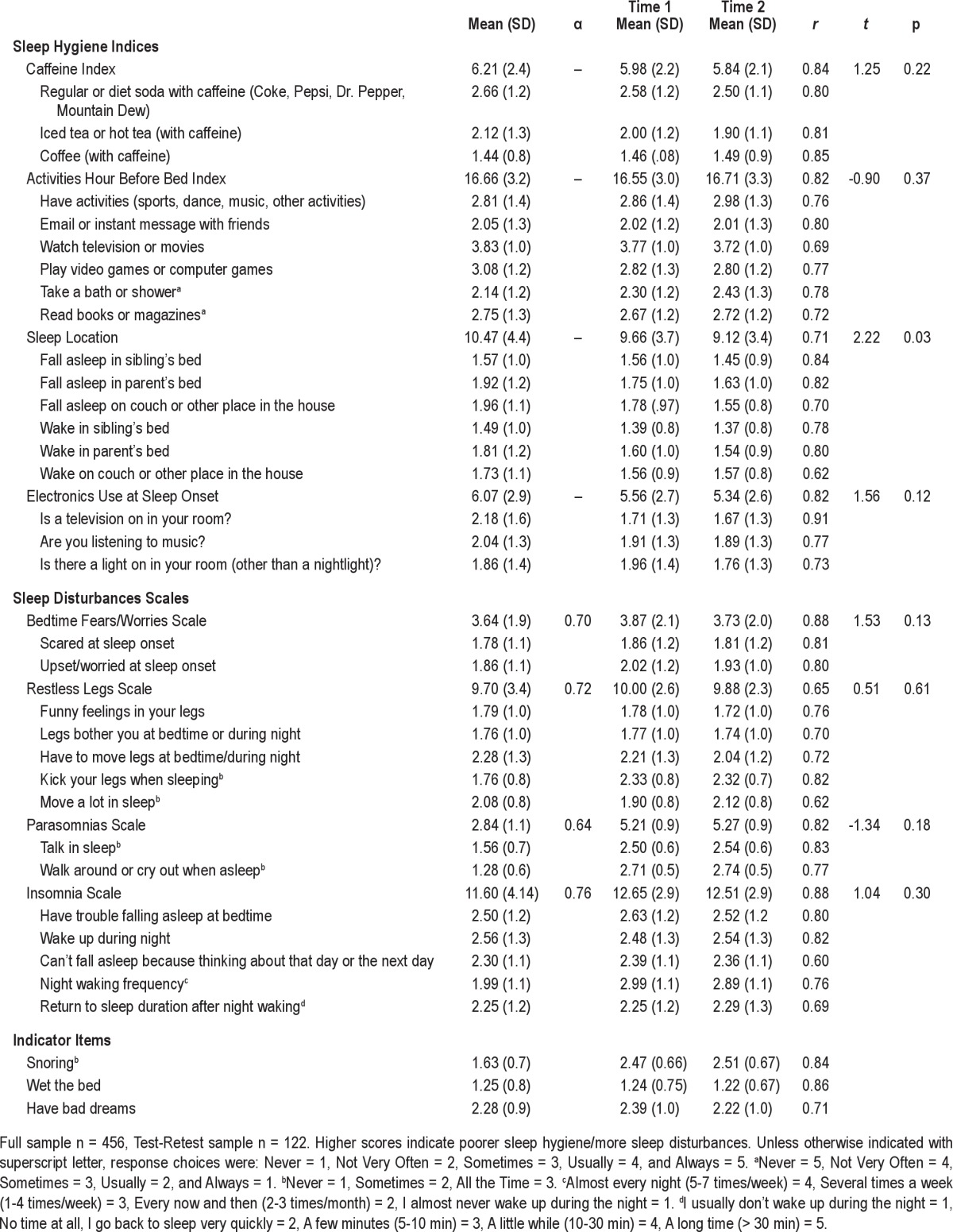
Table 3.
Correlation matrix for Sleep Hygiene Indices and Sleep Disturbances Scales
Reliability
As seen in Table 2, with the exception of the 2-item Parasomnia Scale (α = 0.64), the Cronbach α coefficients for the Sleep Disturbance scales were acceptable (α ≥ 0.70). Test-retest reliability in general was good for all subscales, with correlations > 0.80 for all indices/scales with the exception of the Restless Legs Scale (r = 0.65). Differences from time 1 to time 2 were found for the Sleep Location Index Score, with children sleeping in a location other than their own bed more often at time 1.
Construct Validity
Group Differences
Significant group differences were found (controlling for age), with children presenting to a sleep clinic, sleep laboratory, or pediatric oncology hospital reporting poorer sleep hygiene (sleeping somewhere other than their own bed, more electronics at sleep onset; Table 4) and more sleep disturbance (more symptoms of bedtime fears/worries, restless legs syndrome, parasomnias, and insomnia; Table 5). Further, children in the clinical sample reported snoring and enuresis more often than children in the community sample.
Table 4.
Means and standard deviations for the CRSP Sleep Hygiene Index ANOVA/ANCOVA analyses
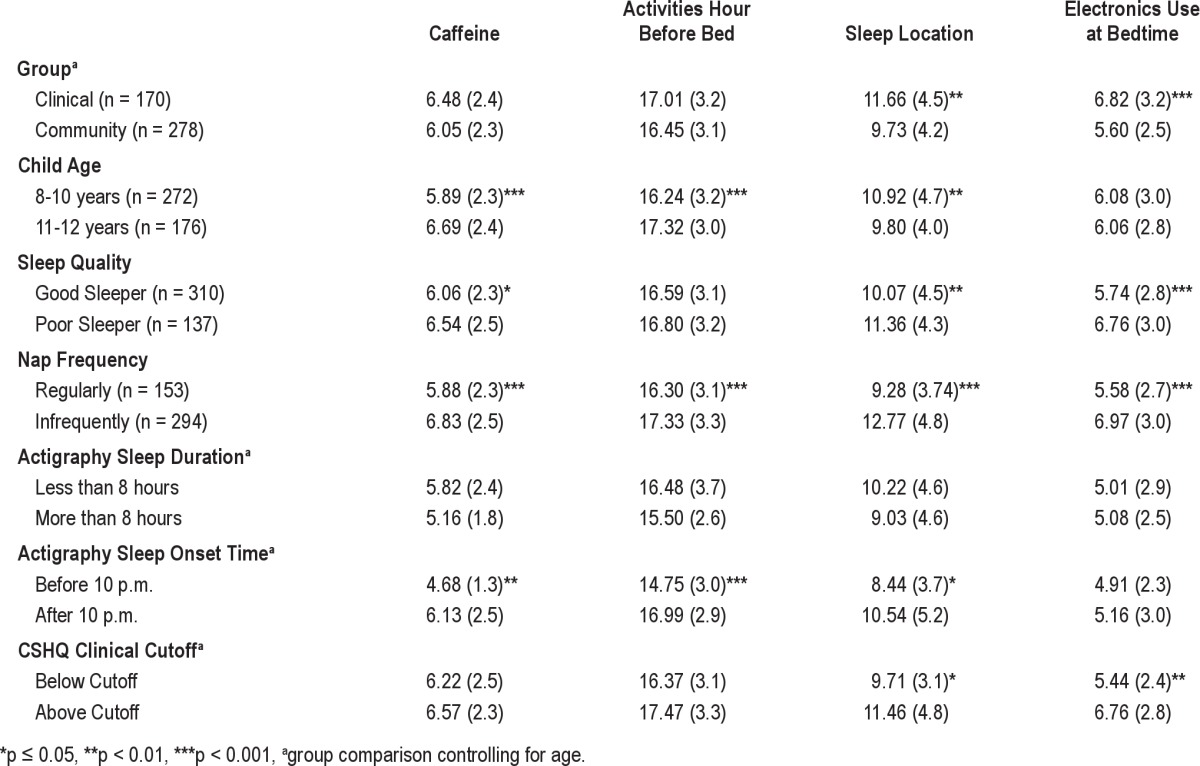
Table 5.
Means and standard deviations for the CRSP Sleep Disturbance Scale ANOVA/ANCOVA analyses
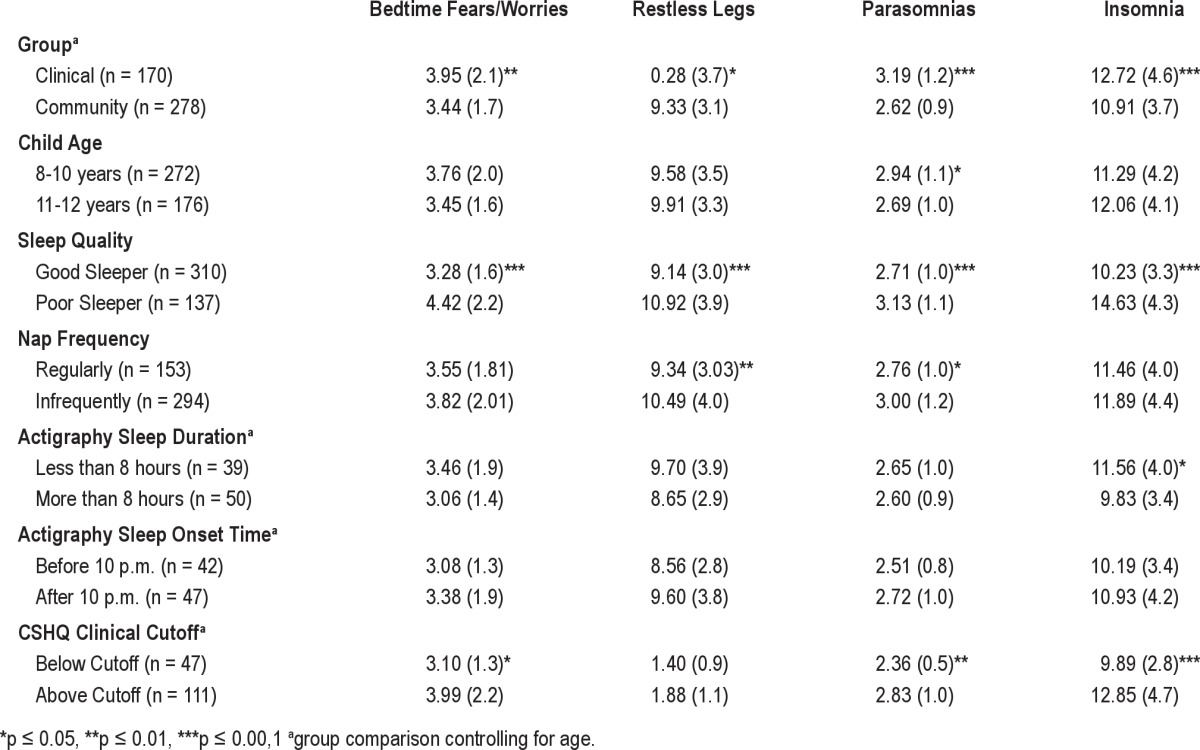
Differences between age groups were found for sleep hygiene (Table 4), with younger children reporting less caffeine use and engaging in fewer stimulating activities in the hour before bed than older children, but sleeping somewhere other than their own bed more often than older children.
Compared to children who classified themselves as good sleepers, children who classified themselves as poor sleepers reported both poorer sleep hygiene (sleeping somewhere other their own bed, more frequent use of electronics at sleep onset, Table 4) and more sleep disturbances (more bedtime fears/worries, and more symptoms of RLS, parasomnias, and insomnia, Table 5). Further, poor sleepers reported more frequent snoring, enuresis, and nightmares.
Finally, children who reported regular napping also reported poorer sleep hygiene, including more caffeine use, more stimulating activities in the hour before bed, sleeping somewhere other than their own bed, and more electronics use at sleep onset (Table 4).
Convergent and Divergent Validity
Child-Reported Sleepiness
Significant associations (p ≤ 0.002) were found between child-reported daytime sleepiness and all of the CRSP Sleep Hygiene Indices and Sleep Disturbances Scales. The strongest associations suggested that children who had greater daytime sleepiness also sleep somewhere other than their own bed (r = 0.33), use electronics more often at sleep onset (r = 0.27), and have more symptoms of RLS (r = 0.38).
Child Reported Anxiety
Significant associations (p ≤ 0.007) were found between child reported anxiety (MASC-10) and the Sleep Location Index (r = 0.21), the Bedtime Fears/Worries Scale (r = 0.42), the Insomnia Scale (r = 0.24), and the Parasomnia scale (r = 0.22), suggesting that children who report more anxiety also report sleeping somewhere other than their own bed, more bedtime fears/worries, and more symptoms of insomnia and parasomnias. A significant association was also found between self-reported anxiety and nightmares (r = 0.35). As expected, other indices/scales were not correlated with anxiety.
Secondary Analyses
Actigraphy
Children with shorter sleep duration and a later bedtime were older than children with longer sleep duration and an earlier bedtime; thus age was controlled for in these analyses. Of the children who underwent actigraphy, those who slept < 8 h/night reported more symptoms of insomnia and more frequent snoring than children obtaining > 8 h of sleep per night (Table 5). Children with a sleep onset later than 22:00 reported more caffeine use, more stimulating activities in the hour before bed, sleeping more often somewhere other than their own bed, and more nightmares (Table 4).
Polysomnography
Children who had moderate/severe OSA (AHI > 5) reported more snoring than children without OSA (AHI = 0, F2,107 = 4.06, p = 0.02). No other differences on the CRSP were found between children with no, mild, or moderate/severe OSA. AHI was significantly correlated with the snoring item (r = 0.25, p = 0.01), but was not correlated with any of the Sleep Hygiene Indices or Sleep Disturbances Scales.
Parent-Reported Sleep Disturbances (CSHQ)
When parents reported poor sleep quality (above the clinical cutoff of 41 on CSHQ, controlling for child age) children reported sleeping somewhere other than their own bed and greater use of electronics at sleep onset; more symptoms of bedtime/ fears worries, parasomnias, and insomnia; and more frequent snoring and enuresis (Tables 4 and 5).
Significant associations (p ≤ 0.006) were found between the CSHQ and the CRSP for both the Sleep Hygiene Indices and Sleep Disturbances Scales. For the Sleep Hygiene Indices, children who reported sleeping somewhere other than their bed had parents who reported more bedtime resistance (r = 0.42) and more sleep anxiety (r = 0.29). Similarly, children who reported greater use of electronics to fall asleep had parents who reported more bedtime resistance (r = 0.23), greater sleep onset delay (r = 0.30), and more sleep anxiety (r = 0.28). Further, children who reported more worries at bedtime had parents who reported more bedtime resistance (r = 0.40), greater sleep onset delay (r = 0.24), and more sleep anxiety (r = 0.48).
For the Sleep Disturbances Scales, children who reported more parasomnias had parents who reported shorter sleep duration (r = 0.23) and more parasomnias (r = 0.41); children who reported more symptoms of insomnia had parents who reported shorter sleep duration (r = 0.32) and more night wakings (r = 0.41); children who reported more frequent snoring had parents who reported more sleep disordered breathing (r = 0.59); finally, children who reported more frequent nightmares had parents who reported shorter sleep duration (r = 0.31) and more night wakings (r = 0.22).
Parent-Reported Sleep Hygiene (CSHS)
Significant associations (p ≤ 0.001) were found between the CRSP Sleep Hygiene Indices (higher scores indicate poorer sleep hygiene) and the CSHS Scales (lower scores indicate poorer sleep hygiene). Specifically, associations were found between the CRSP Caffeine Index and the CSHS Physiological Scale (a measure of caffeine use, food and liquids consumed before bed, and rough play before bed, r = -0.25); the CRSP Activities in the Hour Before Bed Index and the CSHS Bedtime Routine Scale (a measure of having a calming bedtime routine, r = -0.39); the CRSP Sleep Location Index and the CSHS Sleep Stability Scale (a measure of consistency of sleep schedule and location of sleeping r = -0.36); the CRSP Sleep Electronics Index, and the CSHS Cognitive Scale (a measure of electronics use before bed and in bed, r = -0.37); and the CRSP Bedtime Fears/Worries Scale and the CSHS Emotional Scale (a measure of being upset or worried at bedtime, r = -0.41).
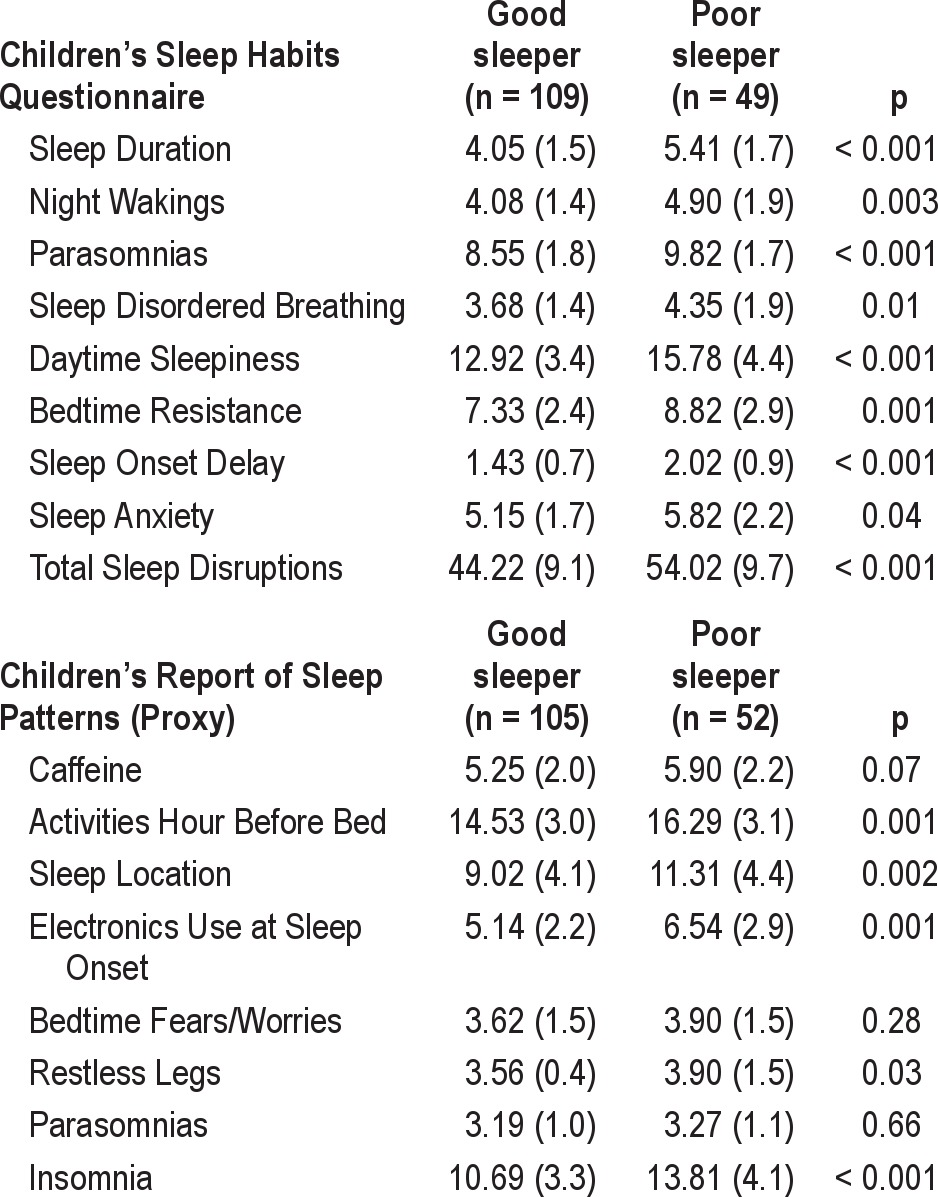
Value Added of Child Self-Report of Sleep Patterns
Differences in parent-reported sleep habits/sleep patterns (CSHQ and CRSP) were found between children who identified themselves as good versus poor sleepers (Table 6). This suggests that children who self-identify as okay/poor sleepers have parents who report more sleep disturbances in their children.
Table 6.
Comparison (means, SD, ANOVA p-values) for the Children's Sleep Habits Questionnaire and the CRSP Parent Proxy Report for children who self-report as great/ good sleepers versus okay/poor sleepers
Previous Night Agreement
For children who reported a long SOL the previous night, 38% of parents reported the child had a short SOL (κ = 0.33). For children who reported ≥ 1 night waking the previous night, 38% of parents reported no night wakings the previous night (κ = 0.40). For children reporting an okay/poor sleep quality the previous night, 42% of parents reported a good/great sleep quality the previous night (κ = 0.42).
Typical Sleep Patterns Agreement
Similar results were found for typical sleep patterns. Of children who reported a typical weekday bedtime later than 21:00, only 12% of parents reported a typical weekday bedtime before 21:00 (κ = 0.69). When children reported a typical weekday wake time before 07:00, only 17% of their parents reported a typical weekday wake time after 07:00 (κ = 0.49). For children who reported having ≥ 1 night waking per week, 42% of parents reported that the child had night wakings less than once a week (κ = 0.42). Finally, of children who reported a typical sleep quality of okay/poor, 39% of their parents reported the child had a typical sleep quality of good/great (κ = 0.43). All variables were also examined by age category, with no differences found in the results.
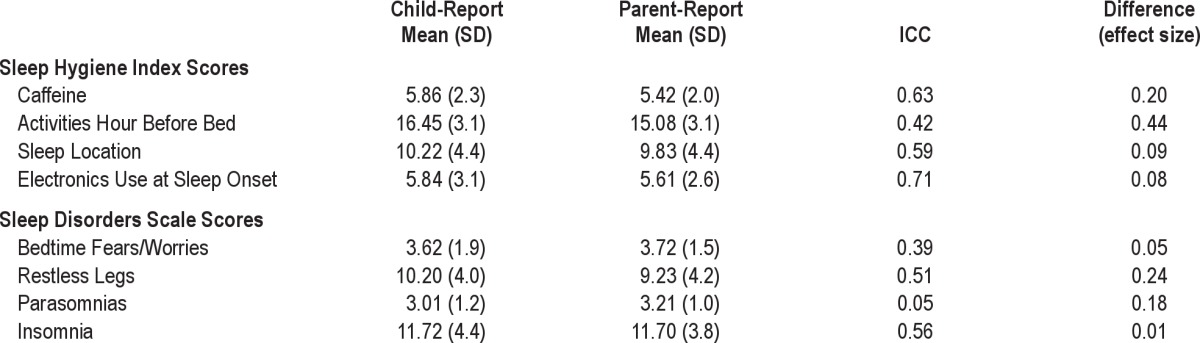
CRSP Sleep Hygiene Indices and Sleep Disturbances Scales
Moderate agreement between parent and child report (ICC > 0.50) was found for caffeine use, sleep location, and electronics use at sleep onset; as well as symptoms of both RLS and insomnia (Table 7). Fair agreement (ICC < 0.50) was found for stimulating activities in the hour before bed, bedtime fears/ worries, and parasomnias.
Table 7.
Comparison (mean, SD, ICC, effect size) of child-report and parent-report for CRSP Sleep Hygiene Indices and Sleep Disturbances Scales (n = 107)
DISCUSSION
In this paper we have presented the preliminary psychometrics of the Children's Report of Sleep Patterns (CRSP), a self-report measure for children ages 8-12 years that includes three modules: Sleep Patterns, Sleep Hygiene Index, and Sleep Disturbances Scale. The CRSP demonstrated good reliability and validity, and provides support for children 8 years and older reporting information about their own sleep. Further, our findings suggest that children may provide information about sleep patterns and disturbances that may not be captured if relying solely on parental report. The strengths of this study include the use of a multi-modal (objective and subjective measures) and multi-reporter (child and parent) approach for the validation of the CRSP.
The reliability of the CRSP was demonstrated through good internal consistency for three of the four sleep disturbance scales. The exception to this was the Parasomnias Scale, which included only two items, both of which focused on what happens while the child is asleep. Test-retest reliability showed that the CRSP items, indices, and scales were relatively stable over time. The only scale that differed from time 1 to time 2 was the Sleep Location Scale, a result that may be due to greater dayto-day variability in where the child falls asleep and wakes up.
The group differences found on the CRSP highlight the validity of this measure. As would be expected, children seen in a sleep clinic, sleep laboratory, or children's hospital had more sleep disturbances, including bedtime fears/worries, parasomnias, insomnia, snoring, and enuresis. The higher scores on the Sleep Location Index and Electronics Use at Sleep Onset Index support the fact that behavioral sleep issues (e.g., children “migrating” to the parents bed during the night, poor sleep hygiene) are commonly seen in pediatric sleep clinics.41
National surveys have shown that caffeine use and technology in the bedroom both increase with age.25,42 Thus, it was not surprising that we found that older children reported more caffeine use and more stimulating activities in the hour before bed. With earlier school start times, it is possible that older children use more caffeine to help them stay awake and alert in the evening, which allows them to engage in more alerting activities before bed (e.g., playing video games, watching television). Consequently, older children may be obtaining less sleep which perpetuates the cycle of evening caffeine use and stimulation.
Children who were self-reported poor sleepers consistently reported more sleep disturbances, demonstrating that children are not only aware of factors that disturb their sleep (e.g., bedtime worries, difficulties initiating/maintaining sleep), but also potential underlying sleep disruptors (e.g., RLS, snoring). In terms of sleep hygiene, children who reported regular napping also reported poorer sleep hygiene, including more caffeine use, and engaging in stimulating activities in the hour before bed. Notably, children who napped regularly also reported increased symptoms of underlying sleep disruptors. Asking children about napping frequency in a clinical setting could provide valuable information about potential poor sleep hygiene and/or underlying sleep disruptors.
A key strength of the present study was inclusion of objective measures to quantify sleep duration and compare with subjective reports in the CRSP. Actigraphy provided an objective measure to demonstrate the validity of the CRSP, highlighting that children provide important information about sleep disturbances, particularly insomnia and snoring. Although not statistically significant, children who slept less than 8 hours also reported more symptoms of RLS, suggesting that their sleep may have been disturbed by their discomfort. Child report of RLS symptoms was greater than parental report, suggesting children may not be reporting their discomfort to their parents. As such, children who are at least 8 years old should be directly asked about any discomfort at bedtime or during the night.
Both the well-established CSHQ and the parent proxy CRSP showed that children are able to provide information about their own sleep habits and sleep disturbances. Children scoring above the clinical cutoff for the CSHQ reported poorer sleep hygiene and more sleep disturbances. Further, children self-identified as poor sleepers had parents who also reported more sleep disturbances on the CSHQ and poorer sleep hygiene on the parent proxy CRSP.
The value that a children's report of sleep patterns provides for a clinical interview or research study was best highlighted with the examination of parent-child agreement for sleep patterns. As would be expected, there was high agreement between parents and children for typical weekday bedtimes and wake times. Although parents become less involved with the bedtime routine as children get older, the awareness of bedtimes and wake times is likely greater in children than adolescents, with teenagers often going to sleep later than their parents. What was notable, however, was that in this study approximately 40% of parents were not aware that their child had difficulties falling asleep, night wakings, or poor sleep quality either the previous night or on a typical night. Although sleep quality is based on a subjective report, self-reported sleep quality is an important treatment outcome, especially for children with insomnia. As such, this result has important clinical implications.
Parents and children had poor agreement on report of parasomnias, with parents reporting more parasomnia symptoms than children. As expected, a behavior that occurs during sleep is better reported by the parent as an outside observer than by the child. This provides evidence for the importance of obtaining both parent and child report of sleep disorders.
Study limitations should be noted. First and foremost, while the full sample was robust in size and diversity, not all participants completed each of the different measures. In addition, some of the subsamples may have lacked variability (e.g., children who wore actigraphy were primarily healthy, good sleepers), while other samples may have been biased (e.g., children recruited from schools or primary care practices may have had undiagnosed sleep disorders), resulting in muted differences between groups. Further, while a diverse sample would suggest generalizability, race/ethnicity data were not collected from the Australian sample, and no additional SES data were obtained. Finally, although we did not find any differences in terms of completion rates or any reported difficulties for younger children in completing this measure, it is possible that the CRSP may be challenging for younger children to complete. Thus we would recommend that adult supervision be available if needed, including someone to read the questions aloud, when younger children complete the CRSP.
Despite these limitations, the CRSP is a valid and reliable measure that can provide additional and important information (beyond parental report) to clinicians and researchers. Although the CRSP was not designed to be a diagnostic clinical tool, we believe this measure has utility in a clinical setting. Many pediatric sleep providers rely solely on parent-completed questionnaires about their child's sleep. As shown by the current results, this may lead to an incomplete or misinformed assessment of the child's sleep. The inclusion of the CRSP may provide additional information to a clinical provider, as well as be utilized as a pre-post treatment measure. In research studies, the CRSP can provide complementary information to parental report, as well as identify sleep patterns or sleep disturbances that parents may not be aware of such as delayed sleep onset latency and multiple night wakings.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the children and families who participated in this study. In addition, we thank Kelly Ann Davis, Colleen Walsh, Julie Ormsby, and Nancy West, for their assistance with data collection and data entry. This study was funded in part by MH077662.
SUPPLEMENTAL MATERIAL
Appendix—Children's Report of Sleep Patterns (CRSP)
References
- 1.Mindell JA, Owens JA. A clinical guide to pediatric sleep: diagnosis and management of sleep problems. 2nd ed. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2010. [Google Scholar]
- 2.Gupta NK, Mueller WH, Chan W, Meininger JC. Is obesity associated with poor sleep quality in adolescents? Am J Hum Biol. 2002;14:762–8. doi: 10.1002/ajhb.10093. [DOI] [PubMed] [Google Scholar]
- 3.Hart CN, Cairns A, Jelalian E. Sleep and obesity in children and adolescents. Pediatr Clin North Am. 2011;58:715–733. doi: 10.1016/j.pcl.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nixon GM, Thompson JM, Han DY, et al. Short sleep duration in middle childhood: risk factors and consequences. Sleep. 2008;31:71–8. doi: 10.1093/sleep/31.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wing YK, Li SX, Li AM, Zhang J, Kong AP. The effect of weekend and holiday sleep compensation on childhood overweight and obesity. Pediatrics. 2009;124:e994–e1000. doi: 10.1542/peds.2008-3602. [DOI] [PubMed] [Google Scholar]
- 6.Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am. 2011;58:649–65. doi: 10.1016/j.pcl.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paavonen EJ, Raikkonen K, Pesonen AK, et al. Sleep quality and cognitive performance in 8-year-old children. Sleep Med. 2010;11:386–92. doi: 10.1016/j.sleep.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: What a difference an hour makes. Child Dev. 2003;74:444–55. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- 9.Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bogels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med Rev. 2010;14:179–89. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Chorney DB, Detweiler MF, Morris TL, Kuhn BR. The interplay of sleep disturbance, anxiety, and depression in children. J Pediatr Psychol. 2008;33:339–48. doi: 10.1093/jpepsy/jsm105. [DOI] [PubMed] [Google Scholar]
- 11.Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev. 2012;16:129–36. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Gregory AM, Rijsdijk FV, Dahl RE, McGuffin P, Eley TC. Associations between sleep problems, anxiety, and depression in twins at 8 years of age. Pediatrics. 2006;118:1124–32. doi: 10.1542/peds.2005-3118. [DOI] [PubMed] [Google Scholar]
- 13.Meltzer LJ, Montgomery-Downs HE. Sleep in the family. Pediatr Clin North Am. 2011;58:765–74. doi: 10.1016/j.pcl.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NHLBI. Bethesda, MD: National Institutes of Health; 2003. National Sleep Disorders Research Plan. Report No 03-5209. [Google Scholar]
- 15.Spruyt K, Gozal D. Pediatric sleep questionnaires as diagnostic or epidemiological tools: A review of currently available instruments. Sleep Med Rev. 2011;15:19–32. doi: 10.1016/j.smrv.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Riley AW. Evidence that school-age children can self-report on their health. Ambul Pediatr. 2004;4:371–6. doi: 10.1367/A03-178R.1. [DOI] [PubMed] [Google Scholar]
- 17.Matza LS, Patrick D, Riley AW, et al. Developing and implementing PRO instruments for assessment of children and adolescents. Report. http://www.ispor.org/meetings/WashingtonDC0512/releasedpresentations/Pediatric-PRO-Task-Force-EM-TUES-Georgetown.pdf. [Google Scholar]
- 18.Bevans KB, Riley AW, Moon J, Forrest CB. Conceptual and methodological advances in child-reported outcomes measurement. Expert Rev Pharmacoecon Outcomes Res. 2010;10:385–96. doi: 10.1586/erp.10.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Irwin DE, Varni JW, Yeatts K, DeWalt DA. Cognitive interviewing methodology in the development of a pediatric item bank: a patient reported outcomes measurement information system (PROMIS) study. Health Qual Life Outcomes. 2009;7:3. doi: 10.1186/1477-7525-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riley AW, Forrest CB, Rebok GW, et al. The Child Report Form of the CHIP-Child Edition: reliability and validity. Med Care. 2004;42:221–31. doi: 10.1097/01.mlr.0000114910.46921.73. [DOI] [PubMed] [Google Scholar]
- 21.Ronen GM, Streiner DL, Rosenbaum P. Health-related quality of life in children with epilepsy: development and validation of self-report and parent proxy measures. Epilepsia. 2003;44:598–612. doi: 10.1046/j.1528-1157.2003.46302.x. [DOI] [PubMed] [Google Scholar]
- 22.Rebok G, Riley A, Forrest C, et al. Elementary school-aged children's reports of their health: a cognitive interviewing study. Qual Life Res. 2001;10:59–70. doi: 10.1023/a:1016693417166. [DOI] [PubMed] [Google Scholar]
- 23.Paavonen EJ, Aronen ET, Moilanen I, et al. Sleep problems of school-aged children: A complementary view. Acta Paediatr. 2000;89:223–228. doi: 10.1080/080352500750028870. [DOI] [PubMed] [Google Scholar]
- 24.Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000;21:27–36. doi: 10.1097/00004703-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 25.National Sleep Foundation. Sleep in America Poll. Retrieved May 11, 2007 from http://www.sleepfoundation.org/2004.
- 26.Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Dev Psychol. 2000;36:291–301. doi: 10.1037//0012-1649.36.3.291. [DOI] [PubMed] [Google Scholar]
- 27.Amschler DH, McKenzie JF. Elementary students' sleep habits and teacher observations of sleep-related problems. J Sch Health. 2005;75:50–6. doi: 10.1111/j.1746-1561.2005.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 28.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009;10:771–9. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 29.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115:257–265. doi: 10.1542/peds.2004-0815H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Calamaro C, Thornton B, Ratcliffe S. Adolescents living the 24/7 lifestyle: Effects of caffeine and technology. Pediatrics. 2009;123:e1005–10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 31.Van der Heijden KB, Smits MG, Gunning WB. Sleep hygiene and actigraphically evaluated sleep characteristics in children with ADHD and chronic sleep onset insomnia. J Sleep Res. 2006;15:55–62. doi: 10.1111/j.1365-2869.2006.00491.x. [DOI] [PubMed] [Google Scholar]
- 32.Owens JA, Maxim R, Nobile C, McGuinn M, Msall M. Parental and self-report of sleep in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med. 2000;154:549–55. doi: 10.1001/archpedi.154.6.549. [DOI] [PubMed] [Google Scholar]
- 33.Meltzer LJ, Biggs S, Reynolds A, Avis KT, Crabtree VM, Bevans KB. The Children's Report of Sleep Patterns - Sleepiness Scale: A self-report measure for school-aged children. Sleep Med. 2012;13:385–9. doi: 10.1016/j.sleep.2011.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.March JS. Multidimensional Anxiety Scale for Children (MASC) Technical Manual. Toronto: MHS Inc.; 1997. [Google Scholar]
- 35.March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. J Am Acad Child Psychiatry. 1997;36:554–65. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- 36.Owens JA, Spirito A, McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–51. [PubMed] [Google Scholar]
- 37.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson A, Harsh J. Sleep hygiene and sleep quality in Italian and American adolescents. Ann NY Acad Sci. 2004;1021:352–4. doi: 10.1196/annals.1308.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: An empirical test of methodological issues. Sleep. 1994;17:201–7. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- 39.Meltzer LJ, Westin AM. A comparison of actigraphy scoring rules used in pediatric research. Sleep Med. 2011;12:793–6. doi: 10.1016/j.sleep.2011.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Iber C, Ancoli-Israel S, Chesson AL, Jr., Quan SF for the American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 41.Meltzer LJ, Moore M, Mindell JA. The need for interdisciplinary pediatric sleep clinics. Behav Sleep Med. 2008;6:268–82. doi: 10.1080/15402000802371395. [DOI] [PubMed] [Google Scholar]
- 42.National Sleep Foundation. Sleep in America Poll. Retrieved March 31, 2006 from http://www.sleepfoundation.org/2006.