Nocturia is defined as waking up one or more times at night to void,1 and is a common affliction among elderly.2,3 The prevalence of nocturia increases across age groups to more than 50% reporting 2 or more voids per night at age of 70.3 Higher prevalence of nocturia in this age group is multifactorial, and possible contributing causative factors include impaired bladder voiding, reduced bladder capacity, decreased vasopressin levels at night, increased comorbid conditions, and sleep disturbances.4
Nocturia has been associated with lower quality of life, cardiovascular disease, mortality, falls, and hip fractures.5,6 It has been suggested that decreased quality of life and some of the adverse health outcomes could be due to sleep disruption from nocturia.7 Several studies have looked at self reported sleep measures and suggest a causal association between nocturia and poor sleep after controlling for confounders such as diabetes mellitus, congestive heart failure, and diuretics.8 These studies used questionnaires or survey and report poor sleep quality, increased awakening, difficulty in falling back to sleep, decreased total hours of sleep, and daytime fatigue in subjects with nocturia.9–11 In these studies, sleep histories were not validated with objective measures such as wrist actigraphy or polysomnography (PSG).
In a study by Parthasarathy et al. of 6,342 Sleep Heart Health Study subjects who had PSG and filled questionnaires about sleep habits that was summarized over 1 month, nocturia was associated with less total sleep period, poor sleep efficiency, higher arousal index, and sleep disordered breathing (SDB). These objective sleep parameters were not adjusted for SDB and other factors.12 The primary aim of the study was to understand if the association between nocturia and cardiovascular disease was independent of SDB. Another study looked at objective sleep measure of sleep using PSG in 20 subjects with benign prostate hypertrophy. Nocturia was associated with increased daytime sleepiness but not with sleep efficiency or total sleep time. This was a small study, only 70% had nocturia, and more than half also had had sleep apnea.13
In this issue of the Journal, additional evidence is presented relating to the putative association between nocturia and sleep.14 Zeitter et al. studied association between nocturia and sleep via simultaneous assessment of both subjective and objective sleep measures in older subjects with insomnia. The mean age of males (n = 55) was 64.3 years and mean age of females (n = 92) was 62.5 years. All subjects maintained sleep logs for 2 weeks, and a subset (n = 60) wore an actigraph for a week. The mean RDI was 3.4, and only 2 subjects had SDB. Only 54.2% of nocturnal awakenings were associated with bathroom use. The number of trips to the bathroom was positively associated with wake time after sleep onset (WASO) (r = 0.24, linear regression; F6,409 = 5.66, p < 0.001 ANOVA), number (r = 0.23, linear regression; F6,409 = 5.03, p < 0.001 ANOVA), and length of wake bouts (r = 0.13, linear regression; F6,409 = 3.48, p < 0.01 ANOVA) measured using actigraph and negatively with feeling of restedness (r = -0.13, linear regression; F4,1093 = 4.27, p < 0.01 ANOVA) and sleep efficiency (r = -0.22, linear regression; F4,1768 = 24.5, p < 0.001 ANOVA) obtained from sleep diary. Furthermore, in subset of subjects (n = 19) who had 2 nights of bathroom use and 2 nights of no bathroom use, the bathroom use was associated with longer wake time, but there was no difference in total sleep time or sleep structure. The authors reported that nocturia in subjects with insomnia is associated with increased wake time and subjective feeling of decreased restedness.
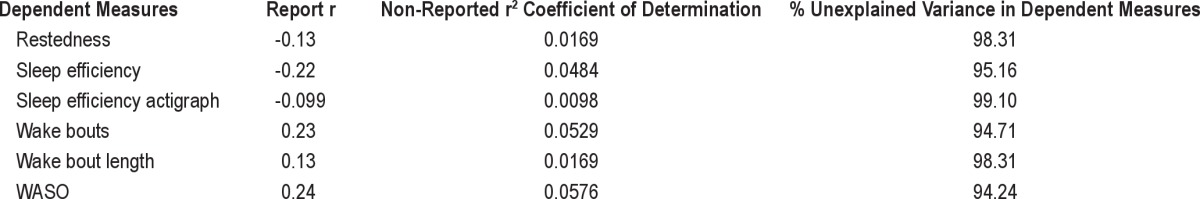
However, the study has several limitations. Even though the regression coefficients were statistically significant, as evident in the ANOVA F p-values, the residual error levels, that is, variance in the dependent variables, are extremely high. These as such indicate very weak precision in the models (Table 1). Also, the authors do not indicate whether or not the categorical groupings of the independent variable were indicator or dummy coded, since the groupings of trips were made into a categorical variable they need to be indicator coded (k-1).
Table 1.
Unexplained variance of dependent variables
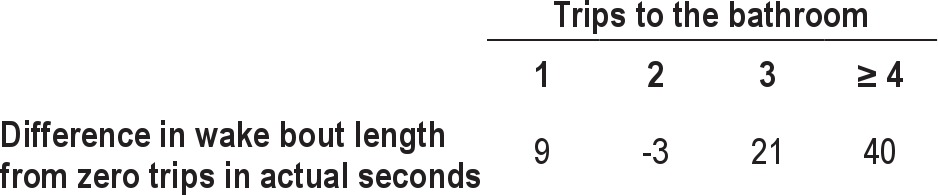
Regarding the magnitude of the effect, taking just one of the six measures, mean wake bout length, if we look at the difference from zero trips in actual seconds, we can see the data demonstrate a very tiny effect (Table 2). There was a 9 second difference in the wake bout length if there was 1 trip and -3 seconds if there were 2 trips.
Table 2.
Difference in wake bout length in seconds
The subjects with insomnia were recruited in the study, what is unclear is if insomnia per se prompts more trips to the bathroom. With age, insomnia is the most common sleep complaint, and adults tend to experience more awakenings and difficulty in maintaining sleep.15
In conclusion, the relation between nocturia and its causal effect on sleep parameters needs to be further elucidated. Further, prospective studies controlling for major confounders need to be conducted to better clarify this relationship. Future studies should consider polysomnogram to capture awakening and associated voids, bladder monitoring to study if sleep disturbances per se cause awakening and hence nocturia, or vice versa by looking at the effect of bladder manipulation on sleep. This would help to tailor the treatment according to patient and possibly improve sleep and related consequences.
DISCLOSURE STATEMENT
The author has indicated no financial conflicts of interest.
CITATION
Budhiraja P. Nocturia and disturbed sleep: where do we stand? J Clin Sleep Med 2013;9(3):263-264.
References
- 1.van Kerrebroeck P, Abrams P, Chaikin D, et al. The standardisation of terminology in nocturia: Report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:179–83. doi: 10.1002/nau.10053. [DOI] [PubMed] [Google Scholar]
- 2.Fitzgerald MP, Litman HJ, Link CL, McKinlay JB BACH Survey Investigators. The association of nocturia with cardiac disease, diabetes, body mass index, age and diuretic use: results from the BACH survey. J Urol. 2007;177:1385–9. doi: 10.1016/j.juro.2006.11.057. [DOI] [PubMed] [Google Scholar]
- 3.Burgio KL, Johnson TM, 2nd, Goode PS, et al. Prevalence and correlates of nocturia in community-dwelling older adults. J Am Geriatr Soc. 2010;58:861–6. doi: 10.1111/j.1532-5415.2010.02822.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bosch JL, Weiss JP. The prevalence and causes of nocturia. J Urol. 2013;189(1 Suppl):S86–92. doi: 10.1016/j.juro.2012.11.033. [DOI] [PubMed] [Google Scholar]
- 5.Donovan JL. Measuring the impact of nocturia on quality of life. BJU Int. 1999;84(Suppl 1):21–5. doi: 10.1046/j.1464-410x.84.s1.2.x. [DOI] [PubMed] [Google Scholar]
- 6.Asplund R. Mortality in the elderly in relation to nocturnal micturition. BJU Int. 1999;84:297–301. doi: 10.1046/j.1464-410x.1999.00157.x. [DOI] [PubMed] [Google Scholar]
- 7.van Dijk L, Kooij DG, Schellevis FG, Kaptein AA, Boon TA, Wooning M. Nocturia: impact on quality of life in a Dutch adult population. BJU Int. 2004;93:1001–4. doi: 10.1111/j.1464-410X.2004.04769.x. [DOI] [PubMed] [Google Scholar]
- 8.Rembratt A, Norgaard JP, Andersson KE. Nocturia and associated morbidity in a community-dwelling elderly population. BJU Int. 2003;92:726–30. doi: 10.1046/j.1464-410x.2003.04467.x. [DOI] [PubMed] [Google Scholar]
- 9.Asplund R, Aberg H. Health of the elderly with regard to sleep and nocturnal micturition. Scand J Prim Health Care. 1992;10:98–104. doi: 10.3109/02813439209014044. [DOI] [PubMed] [Google Scholar]
- 10.Yu HJ, Chen FY, Huang PC, Chen TH, Chie WC, Liu CY. Impact of nocturia on symptom-specific quality of life among community-dwelling adults aged 40 years and older. Urology. 2006;67:713–8. doi: 10.1016/j.urology.2005.10.054. [DOI] [PubMed] [Google Scholar]
- 11.Bliwise DL, Foley DJ, Vitiello MV, Ansari FP, Ancoli-Israel S, Walsh JK. Nocturia and disturbed sleep in the elderly. Sleep Med. 2009;10:540–8. doi: 10.1016/j.sleep.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parthasarathy S, Fitzgerald M, Goodwin JL, Unruh M, Guerra S, Quan SF. Nocturia, sleep-disordered breathing, and cardiovascular morbidity in a community-based cohort. PLoS One. 2012;7:e30969. doi: 10.1371/journal.pone.0030969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bal K, Ayik S, Issi Y, Bolukbasi A, Akhan G. Sleep analysis of patients with nocturia and benign prostatic obstruction. Urology. 2012;80:383–8. doi: 10.1016/j.urology.2011.12.067. [DOI] [PubMed] [Google Scholar]
- 14.Zeitzer JM, Bliwise DL, Hernandez B, Friedman L, Yesavage JA. Nocturia compounds nocturnal wakefulness in older individuals with insomnia. J Clin Sleep Med. 2013;9:259–262. doi: 10.5664/jcsm.2492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stepnowsky CJ, Jr, Ancoli-Israel S. Sleep and its disorders in seniors. Sleep Med Clin. 2008;3:281–93. doi: 10.1016/j.jsmc.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


