Abstract
Objective
Over the past 60 years, population control has become an increasingly urgent issue worldwide as a growing population strains already limited resources. The use of financial incentives to promote family planning is an innovative approach that has potential to make a contribution to efforts to better manage population growth. This report reviews eight studies that examined the effect of incentives on family planning.
Method
Published studies that tested the impact of incentives to promote some aspect of family planning and included an appropriate control or comparison condition were reviewed.
Results
Incentives have been used to promote attendance at contraceptive education sessions, adoption and continuation of contraceptive methods, sterilization, and to limit family size. All but one of the eight studies reviewed reported positive outcomes, but weaknesses in study design and execution limit the strength of the conclusions that can be drawn.
Conclusion
Review of this literature suggests that family planning behaviors, like other behaviors, are sensitive to incentives. Given the tremendous need for efficacious interventions in global efforts to manage population growth, further research on this topic using more rigorous experimental methods is warranted.
Keywords: Incentives, Family planning, Contraception
Introduction
In this report we review research on the use of financial incentives to promote family planning. The US Agency for International Development (USAID) defines family planning as activities that “enable couples to determine whether, when, and how often to have children” (USAID, 2011). Contraception is typically the primary component of family planning programs, but programs often include other medical, educational, and social activities. Family planning has profound health, economic, and social benefits for families and communities, including protecting the health of women by reducing high-risk pregnancies, protecting the health of children by allowing sufficient time between pregnancies, reducing abortions, supporting women’s rights and opportunities for education, employment, and full participation in society, and protecting the environment by stabilizing population growth. Decades of research have also shown that family planning is one of the most cost-effective health interventions in the developing world (USAID, 2011).
The family planning movement began in earnest in the 1950s, with the launching of national family planning programs in developing nations around the world. In pre-industrial, developing nations, large families were the norm. In mid-1950’s India, for example, women had an average of 6 children (Kulkarni and Rani, 1995). The high birth rate ensured that enough children would survive childhood to contribute to the economy of the household and to care for their parents as the parents aged. The high birth rate was also offset by a high death rate, the result of disease, drought, and other natural disasters, keeping overall population growth in check. However, development brought improvements in public health (e.g., sanitation), food production (e.g. crop rotation), and medicine (e.g., vaccines and antibiotics), which decreased both child and adult mortality and resulted in dramatic increases in the rate of population growth (Ashford and Noble, 1996). In India, for example, population growth had continued largely unabated for more than two decades despite long-standing concerns about the rate of population growth and efforts to curtail it by providing free or subsidized contraceptive supplies, services and education (Khan and Prasad, 1980). By the mid-1950’s, the national government began desperately searching for policies that could reduce the average family size and help reign in population growth. One of the novel strategies implemented was the use of monetary or other in-kind incentives delivered contingent on the adoption of family planning. The first use of these types of incentives, to our knowledge, took place in 1956 in Tamil Nadu, one of the more populous Indian states. The regional government began offering 30 Rupees (Rs.; ~US $7) to any man or woman who underwent sterilization. It was reported that the Tamil Nadu program averaged 3.42 sterilizations per thousand population while other Indian states averaged about 1.00, prompting many other Indian states to start similar programs (Elder and Estey, 1992).
Numerous financial incentive arrangements have subsequently been proposed (see review by Simon, 1976); however, relatively few have been instituted and even fewer have been evaluated empirically. Among those evaluated empirically, most were done in field settings using quasi-experimental designs common in family planning research and were conducted at the height of the family planning movement in the 1960’s, 70’s, and 80’s. While quasi-experimental designs have their limitations, many of the interventions tested were remarkably innovative for their time and the results overall provide preliminary evidence that family planning behaviors are sensitive to incentives. Thus, there is real potential for incentives to be part of the solution in continuing efforts to better manage global population growth. It is hoped that this review will reinvigorate the interest of the family planning literature in this approach and also that by including the topic in this broader supplemental issue on incentives and health, incentive experts will be encouraged to undertake empirical work on this extremely important topic.
Methods
The present review focused on studies where delivery of the financial incentive was explicitly contingent on the participant engaging in a family planning behavior. Bibliographic databases (EconLit, Family and Society Studies Worldwide, JSTOR, PsycINFO, PubMed, Social Sciences Full-text) were searched. Terms commonly used in the literature to refer to incentives (cash, incentives, money, payments, and voucher) were crossed with common family planning terms and phrases (birth spacing, contraception, family planning, pregnancy prevention, and sterilization) to search each database. If the title appeared relevant, the abstract was read. If the abstract appeared relevant, the full text was retrieved. Only original reports written in English were included in the review. Studies also had to include an appropriate control or comparison condition. Case reports, letters, editorials, and reviews were not included. Studies that exclusively incentivized patient recruiters or family planning service providers were not included (see review of this topic by Cleland and Robinson, 1992). One study in which one of the three conditions included an incentive for patient recruiters was included (Perkin, 1970). Incentive studies where the impact on family planning behaviors was indirect (e.g., pregnancy rates among girls receiving incentives contingent on school attendance (Baird et al., 2010) also were not included. The reference lists of retrieved articles were also searched to look for additional relevant citations.
The studies retrieved through this search are presented below, organized in sections based on the family planning behavior targeted by the incentives: attendance at contraceptive education sessions; contraceptive use; sterilization; and limiting family size. In the description of each study, effort was made to provide some context for the value of the incentive used; in most cases, an estimate of monthly income is provided. Unless otherwise noted, all amounts are the value at the time of the study.
Results
Incentives targeting attendance at contraception education sessions
Stevens-Simon et al. (1997) conducted a randomized controlled trial of the Dollar-a-Day program, which attempted to reduce repeat teen pregnancies by incentivizing attendance at weekly peer support groups meetings. At these meetings, participants first talked informally about current concerns and future goals, which adult group leaders used as a starting point for more formal, didactic discussion about the advantages and disadvantages of various contraceptive methods and other topics. The study was funded with a combination of public and private monies. The majority of the 286 primiparous teenage girls from Denver, Colorado who participated in the trial were minorities (54%), had public health insurance (88%), and had dropped out of high school around the time of their first pregnancy (69%). Girls were randomized to 1 of 4 conditions: 1) a monetary incentive ($7) for attending the weekly peer-support group for 2 years; 2) access to a weekly peer-support group only; 3) the monetary incentive ($7) only; or 4) no intervention. The $28 available per month has about $45 in purchasing power in 2011 dollars. The results indicated that providing a monetary incentive did significantly increase participation in the peer-support group: only 9% of the group-only condition participated in group as compared to 58% of the group plus incentives condition. However, incentives did not impact pregnancy rates. Incidence of second pregnancies was 9% at 6 months, 20% at 12 months, 29% at 18 months, and 39% at 24 months after delivery of the first child and did not vary significantly by intervention condition.
This is the most rigorously conducted study in this literature to date and it provided strong evidence that the incentives increased the target behavior of attendance at weekly contraception education sessions. Unfortunately, increased attendance did not lead to decreases in repeat pregnancy rates as the authors had hoped. While contraceptive education in and of itself does not appear sufficient to substantially modify risky behaviors, it stands to reason that accurate knowledge about contraception is an important element of family planning. The present study provides a good model for interventions where the primary aim is to provide contraception education.
Incentives targeting contraception use
Three quasi-experimental studies tested interventions where incentives targeted initiation and/or continuation of contraception use. The first was conducted by the Planned Parenthood Association of Ghana, in Accra, Ghana, in West Africa in the late 1960’s (Perkin, 1970). At this time, field workers regularly distributed referral slips for the local family planning clinic to women in the community who expressed interest in adopting a family planning method, but few women followed through. A study was conducted using a quasi-reversal design to test the impact of offering incentives, in the form of tins of powdered milk, for adopting a family planning method. Perkin does not specify the methods offered, but they likely were condoms, birth control pills, IUDs, and sterilization (Mauldin, 1975). During weeks 1 and 3 of the 5-week study, field workers distributed referral slips as well as a coupon that could be redeemed at the clinic for 2 tins of powdered milk. At the time, the 2 tins of milk had a value of approximately US$1 and monthly average earnings in the area were estimated at US$20/month. During weeks 2 and 4, they distributed the referral slips alone. During week 5, field workers distributed referral slips plus the free milk coupon, but during this final week, there was also a contest for the field workers. Prizes of powdered milk were given out to the field workers who distributed the most referrals and who had the most referrals come into the clinic. The number of referred women who accepted family planning varied moderately as a function of the incentives being offered (Fig. 1). Without the incentive, acceptance was only about 10%, but adding the patient incentive increased acceptance 2-fold, while patient and referrer incentives increased acceptance more than 3-fold.
Fig. 1.
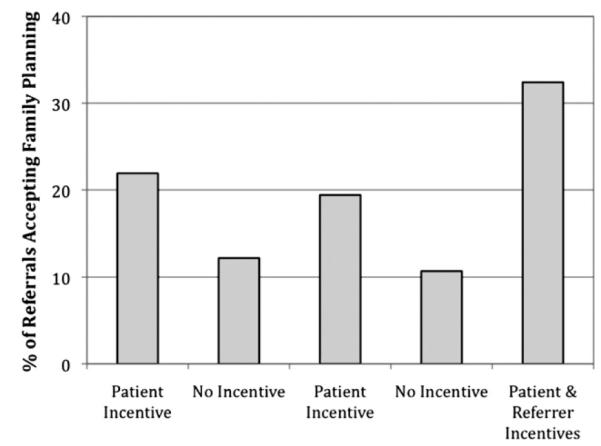
Percentage of referrals accepting family planning when participants were offered a referral slip plus a tinned milk incentive for attending a family planning session (weeks 1 & 3), a referral slip alone (weeks 2 & 4), or a referral slip, participant tinned milk incentive, and referrer tinned milk incentive (week 5). The study was conducted in Accra, Ghana, in West Africa in the late 1960’s. Graphed from data provided in the original manuscript (Perkin, 1970).
In a second study, incentives were used to promote continuation of a reversible contraceptive method following method adoption. The study was conducted in two matched clusters of villages (Clusters A & B) in Ammanpettai in the Indian state of Tamil Nadu in 1987–88 (Stevens and Stevens, 1992). The clusters were matched on socioeconomic variables and were equidistant from the study clinic. Thirty-nine percent of women in these villages had no formal education; those that did averaged just 6 years. More than 90% of women were manual laborers in agriculture and the average monthly income was 243 Rs./month. To be eligible for the Ammanpettai study, women had to be <35 years old, married, and capable of having children. If women had children, the age of the youngest had to fall in the range between 6 months and 5 years. In the Cluster A villages, women were invited to a clinic for free maternal/child health services, contraceptive education, and supplies of reversible contraceptive methods. Cluster B villages were offered the same services as Cluster A, but the women were also offered 20 Rs. at the 1st visit and at subsequent monthly visits (for a total of 6 months) if they continued their contraceptive method and were not pregnant. There were also two Control villages that had no contact with the study. Results indicated that enrollment was dramatically different in the two village clusters, with more than 1000 women coming to the Cluster B clinics within the first few days and only 14 women coming to the Cluster A clinics during the same period. Population-based rates of contraception use before the intervention and >1 year after the end of the intervention also differed and are shown in Fig. 2. Within clusters, contraception rates increased more than 3-fold in Cluster A villages, but the increase was even more dramatic in Cluster B villages, with a more than 8-fold increase in the rate of contraception use compared to baseline rates in each cluster. Between clusters, compared to Control villages, contraception rates at follow-up were 2-fold higher in Cluster A villages and 5-fold higher in Cluster B villages. These results suggest that increasing access to contraceptives by providing them free of charge does moderately increase their use, but that providing incentives contingent on their use results in even better outcomes.
Fig. 2.
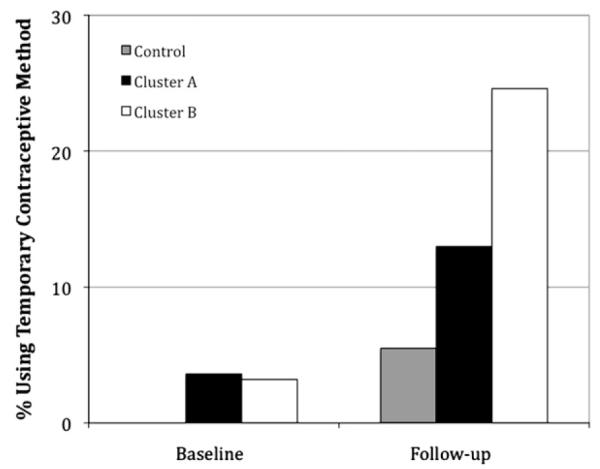
Population-based rates of temporary contraceptive method use in no-contact Control villages (gray bars), villages where women were invited to receive free family planning services only (Cluster A; black bars), and villages where women were invited to receive free family planning services and offered monetary incentives (20 Rupees) at an initial visit and subsequent monthly visits for accepting and continuing to use contraception (Cluster B; white bars) at baseline and at follow-up >1 year after incentives were discontinued. The study was conducted in Ammanpettai in the Indian state of Tamil Nadu in 1987–88. Note. No baseline data on the contraceptive use of no-contact Control villages was available. Graphed from data provided in the original manuscript (Stevens and Stevens, 1992).
A third study in nine villages in northeast Thailand examined whether financial incentives can be used to influence contraceptive practice at the individual and community levels (Weeden et al., 1986). The Population Crisis Committee, an international nongovernmental organization (NGO), funded the project and it was carried out by the Population and Community Development Association, a Thai NGO. In each of the six experimental villages, a community loan fund was made available to villagers for income-generating activities, mostly agricultural projects. At the time of the project, monthly average earnings in the area were estimated at US$40/month. Villagers who practiced family planning (reversible methods or sterilization) were able to obtain larger loans than those who did not, with the typical loan ranging between US$80 and $200. The loan fund also increased in value as the contraceptive prevalence rate increased, although if prevalence declined, no money was withdrawn. The contraceptive prevalence rate was surveyed in three control villages at the beginning and end of the two-year program and these control villages were matched to experimental villages on baseline contraceptive prevalence and method mix, population size, access to family planning services, economic need, and the amount of interest demonstrated by village leaders in the project. Results indicate that contraceptive prevalence increased in loan fund villages as compared to control villages over this two-year period (29% vs. 6%, respectively). In parallel, the pregnancy rate in loan fund villages decreased moderately by 6% while the rate increased 1% in control villages.
All three of these studies of incentives targeting initiation and/or continuation of contraceptives reported moderate outcomes that favored the incentive condition. Nevertheless, limitations in the design and execution of each study temper the conclusions that can be drawn. The Perkin (1970) report does not define the target behavior of “accepting family planning,” leaving it unclear exactly what the incentive was contingent on and how noteworthy the results are. Increasing acceptance of longer-term methods such as IUDs or sterilization would be more remarkable than acceptance of methods like condoms and birth control pills, which are frequently used incorrectly and are easily discontinued. On a related note, neither the Stevens and Stevens (1992) nor Weeden et al. (1986) report indicates how the target behaviors (i.e., contraceptive use and not being pregnant) were verified. If the investigators relied on self-report, the outcomes may be biased due to demand characteristics. Additional weaknesses of all three the studies are the quasi-experimental designs and the absence of statistical analyses.
Incentives targeting sterilization
Two observational studies examined the influence of incentives on sterilization rates. The first analyzed sterilization rates of workers from four factories (two in East India, two in West India) run by Tata Industries, an Indian conglomerate, to those of workers from four matched factories not part of the Tata conglomerate (Khan and Prasad, 1980). It was Tata Industries policy at the time to provide monetary incentives averaging 188 (Rs. for undergoing sterilization, while non-Tata factories offered an average of 31 Rs. The average education level of the factory workers ranged between 6 and 9 years and monthly earnings ranged from Rs. 300 to 500. To be eligible for sterilization, workers had to be married, have two or more living children, and be covered by their company’s benefits plan. Cumulative sterilization rates were first compared statistically in 1969, about 2 years after initiation of the Tata incentive program. Results indicate that rates were significantly higher among Tata workers compared to non-Tata workers in both the East and the West (East: 17.9% vs. 11.8%; West: 24.6% vs. 18.5%; ps<0.05). Cumulative sterilization rates were compared statistically again in 1976, by which time many non-Tata factories and other agencies in East India were offering large incentives for sterilization. The rate of sterilization was no longer different in the East (34.4% vs. 32.2%), but remained significantly higher in the West (41.7% vs. 35.1%, p<0.05). Overall, the study suggested modest increases in sterilization with larger incentive values.
The second study analyzed monthly average sterilization rates in Sri Lanka in response to changes in the magnitude of the incentive provided by the federal government to citizens undergoing sterilization from 1968 to 1985 (Thapa et al., 1987). These authors report in another study that the magnitude of the incentive was changed when the government perceived the need to expand the availability and accessibility of family planning services (de Silva et al., 1988). Sterilization acceptors had to meet age requirements (<49 years for men and <44 years for women), be married and have the informed consent of their spouse, and have at least two living children. At the time, households with a monthly income of <1000 Rs. were considered poor. The results are shown in Fig. 3 and demonstrate that monthly average sterilization rates varied according to the magnitude of the incentive offered. Implementation of a 100 Rs. incentive resulted in a nearly 3-fold increase in sterilization rates over no incentive levels, while implementation of a 500 Rs. incentive resulted in a 12-fold increase. Subsequent implementation of 200 and 300 Rs. incentives generated approximately the same rate of sterilization as 100 Rs., while a return to the 500 Rs. incentive resulted in a 4.5-fold increase compared to no incentive levels. Overall, these results provide a largely orderly illustration of the impact of incentive magnitude, with larger magnitudes generally resulting in a larger response. Less orderly are the seemingly blunted responses to the 200 and 300 Rs. incentive values and the dramatically different responses to the two offerings of 500 Rs. It is possible that the 200 and 300 Rs. values seemed comparatively small in contrast to the 500 Rs. incentive that preceded them. Similarly, the response during the initial 500 Rs. period may have been inflated due to the contrast with the preceding reward of only 100 Rs. In addition, the initial 500 Rs. incentive was only offered for 4 months, while the second was offered for 31 months. Thus, the lower average registered during the second 500 Rs. offer may be a more accurate representation of the performance of that incentive amount over an extended period of time. Nevertheless, the results suggest a generally orderly impact of incentive magnitude on sterilization rates.
Fig. 3.
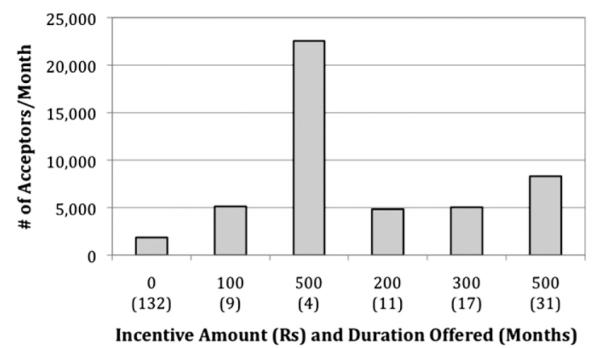
Average number of sterilizations per month when participants were offered no incentives or monetary incentives of varying magnitudes for undergoing sterilization. The y-axis indicates the order and magnitude of the monetary incentives offered, as well as the number of months each incentive was offered. The study was conducted in Sri Lanka from 1968 to 1985. Graphed from data provided in the original manuscript (Thapa et al., 1987).
Recognizing the controversial nature of incentives contingent on sterilization, the authors of both of these studies conducted follow-up interviews with a subset of the study population. In both studies, incentives were not found to be a significant factor in this decision to undergo sterilization. Granted, these analyses were based on retrospective responses that may have been subject to rationalization. In addition, it must be noted that other surveyors have reported that a high percentage of men stated that the incentive was their “sole motivating factor” for undergoing vasectomy (Srinivasan & Kachirayan, 1968 as cited in Rogers, 1971), that men who had not met all the requirements were sterilized and paid the incentive anyway (Repetto, 1968), and that a concerning percentage of patients regretted their decision (Hapugalle et al., 1989). In addition to documentation of abuses and mismanagement in some of these incentive programs, more recent advances in other areas of science have added to our understanding of decision-making processes that readily apply to the decision to undergo sterilization. For example, there is now strong empirical evidence from the field of behavioral economics that demonstrates that people place disproportionate weight on more immediate gains and losses at the expense of longer-term outcomes (Bickel and Marsch, 2001; Loewenstein et al., 2007). Further, this bias is stronger in disadvantaged populations (Green et al., 1996; Jaroni et al., 2004), who not coincidentally are more likely to experience contraceptive failure, discontinue contraception, and have an unintended pregnancy, along with other adverse reproductive outcomes (Finer and Henshaw, 2006; Hammerslough, 1984; Trussell and Vaughn, 1999). This bias towards more immediate gains could result in people overvaluing the relatively immediate option (the incentive payment for undergoing sterilization) while substantially underestimating the longer-term consequences of that decision (permanent sterility). As a result, it is very unlikely that it would be ethical to provide incentives contingent on sterilization in today’s world.
Incentives to limit family size
Two quasi-experimental studies examined long-term incentive interventions designed to limit family size. The first was conducted on multiple tea estates in South India (Ridker, 1980). Husbands and wives were employed and lived on the same estate and tended to spend most of their lives on the same estate, which was responsible for health care costs (including those related to maternity/child health) as well as pensions. The No-Birth Bonus Scheme (NBBS), as the intervention was known, was evaluated from 1971 to 1978. On the three NBBS estates, women received 5 Rs. per month for every month they were not pregnant, which was deposited into an account that earned 5% annual interest. If a woman became pregnant, payments into the account ceased for 12 months. In addition, deductions were taken from the account for all births after the second child. These deductions varied based on the number and spacing of children born to the woman and ranged from 50 Rs. to the entire balance of the account. Only live births and living children were counted; no deductions were made in the case of a miscarriage and if one of the first two children in a family died, no deduction was made for the third birth. The account could not be drawn on until the end of a woman’s childbearing years, roughly the same age as retirement. Booklets with spaces to record deposits, deductions, and a running total were updated and passed out every few months so that women and their families could follow their progress. The tea estates provided the incentive payments, presumably repurposing money that would have otherwise been used to pay for standard maternity and child-care benefits. For comparison, women working on the six control estates received standard maternity and child-care benefits. Sociodemographic characteristics and the availability of family planning services were comparable across estates. Eighty-two percent of eligible women on the NBBS estates enrolled in the intervention. They had very little education, averaging just 1 year of formal schooling. At the start of the evaluation, monthly average earnings in the area were estimated at 100 Rs./month; by 1975, monthly average earnings were estimated at >200 Rs./month. Fig. 4 shows the birthrate outcomes. Population-based birthrates on the NBBS estates decreased from 40.5 to 21.9 (per 1000) whereas on the control estates birthrates decreased from 39.2 to just 34.1. These results demonstrate the moderately successful use of a longer-term, more complex incentive schedule that was composed primarily of positive reinforcement (incentives for avoiding pregnancy) along with judicious use of occasional negative punishment (temporary suspension of payments during pregnancy, deductions from account for higher-order births).
Fig. 4.
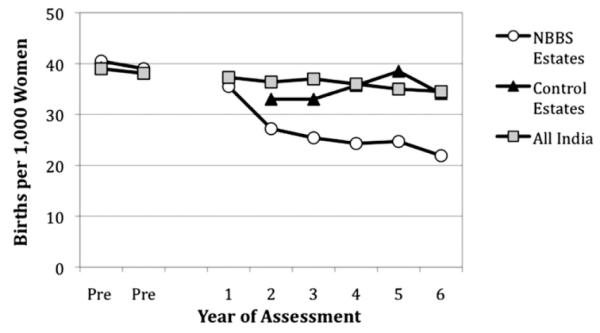
Population-based birth rates per year among women living on No-Birth Bonus Scheme Estates (NBBS; white circles), Control Estates (gray triangles), and in all of India (black squares) during two years prior to the implementation of NBBS (“Pre”) and over the years NBBS incentives were offered to women for avoiding pregnancy (years 1–6). The study was conducted on multiple tea estates in South India from 1971 to 1978. Note. Values for Control Estates were not available for the first year of assessment. Graphed from data provided in the original manuscript (Ridker, 1980).
A second study in rural Taiwan in the 1970’s developed and tested a similar incentive intervention aimed at limiting family size (Sun and Cernada, 1985–6). The Huatan Educational Savings Plan, as the intervention was known, appears to have been financed with foreign funds and carried out by the Taiwan Provincial Institute of Family Planning. To enroll, couples had to be married, have ≤3 children, and the mother had to be <30 years old. Subsequently, money was deposited into an interest-earning educational savings account each year that the couple maintained their family size of ≤3 children. Larger incentives were deposited into accounts of families with ≤2 children vs. 3 children and deposit amounts escalated over time (e.g., $5 in years 1 & 2, $10 in years 3 & 4, $15 in years 5 & 6, etc.) as long as families maintained their smaller family size. A onetime withdrawal of funds was then expected to occur 10–14 years after enrollment to pay for higher education fees. Sixty-seven percent of eligible couples enrolled. The overwhelming majority had a primary school education or less, but expected their children, especially sons, to complete college. About half of participating families had an average monthly household income of <US$25 while the other half had an average monthly household income of >US$100 (Finnigan and Sun, 1972). Results indicated that fertility rates in Huatan over the decade that the plan was in place declined 30% whereas in a similar, control township, the decline was only 20%, suggesting a modest positive impact of the intervention.
Both studies of these long-term interventions (Ridker=6 years; Sun & Cernada=10 years) to limit family size reported outcomes that favored the incentive condition. The positive results in both studies are somewhat surprising given the long delay imposed before participants could access their earnings, estimated at between 10 and 15 years, as delay has been shown to be a significant moderator of the effect size in other incentive interventions (Lussier et al., 2006). As with prior studies, quasi-experimental designs and the absence of statistical analyses also limit conclusions. The complexity and duration of the incentive schedules in these studies also call attention to the need for additional monitoring and management in interventions such as these. Indeed, Ridker reported that NBBS administrators on the tea estates were too busy with other tasks to update and distribute the booklets on a regular basis after the first year of the program and that interviews conducted four years after the NBBS was instituted indicated that many women enrolled in the intervention did not fully understand how the contingencies operated. While these initial results suggest further study of similar interventions is warranted, these studies also point to potential problems that future researchers should take care to address.
Discussion
In this report we reviewed research on the use of financial incentives to promote family planning. Outcomes favoring the incentive condition were reported in all but one of the reports included in the review and there are suggestions that family planning behaviors, like other behaviors, are sensitive to incentives, as the patterns of results across studies are consistent with results observed in studies of incentives to promote other types of behavior change. For example, the study by Thapa et al. (1987) examining different magnitudes of incentives to promote sterilization observed generally orderly effects of magnitude, consistent with well-established evidence that that the magnitude of the incentive is a significant moderator of the effect size of incentive interventions (e.g., Lussier et al., 2006). Similarly, the structure of the incentive schedules utilized by Ridker (1980) and Sun and Cernada (1985–6), which included escalating incentive values and deductions from earnings when the behavioral target was missed, parallel incentive schedules that have been successfully used to promote abstinence from substance of abuse (Higgins and Silverman, 2008; Lussier et al., 2006). Overall, the literature on incentives to promote family planning behaviors provides preliminary evidence that these behaviors respond to incentives in orderly and predictable ways that parallel positive results observed in studies of incentives to promote other types of behavior change.
Nevertheless, the existing research has substantive limitations. First, the majority of the studies had quasi-experimental designs. We limited the review to studies with control or comparison groups, each of which was matched to the experimental group on factors thought to influence outcomes, but without random assignment, there is greater chance that confounding variables are responsible for the differences observed. Second, family planning behaviors targeted by incentives have varied widely, from attending weekly contraception education sessions to limiting family size. Studies targeting use of reversible methods likely relied on self-report of the use of methods like birth control pills and condoms, a significant source of potential bias. Third, few studies were analyzed statistically and the differences observed were often modest in size. Thus, drawing firm conclusions from the existing research literature on the efficacy of incentives to promote family planning behaviors is difficult at this time.
Sterilization has also been a target of incentives. As noted earlier, elucidation of the “present bias,” where the prospect of short-term gains may result in individuals acting contrary to their long-term interests, make incentives contingent on sterilization ethically untenable. However, the opposite problem, that individuals may be deterred by the short-term costs of actions that would bring them long-term benefits, must likewise be considered in a comprehensive ethical analysis of interventions in family planning. In this situation, as Chomitz and Birdsall (1990) aptly state, “it is their inaction rather than their action that induces regret (pg. 317).” Indeed, in family planning, it is likely that individuals discount the delayed reinforcement gained by adopting family planning (e.g., postponing pregnancy until adulthood; spacing pregnancies sufficiently; avoiding unintended pregnancy) so significantly that it is not sufficient to sustain the more proximal behavioral costs/efforts necessary to do so. For example, initiating and continuing use of the more effective prescription contraceptives requires a number of steps that may be cumbersome such as finding a provider you feel comfortable with, getting to the appointment, answering embarrassing questions about sexual behavior, undergoing uncomfortable procedures, paying for the costly prescription, remembering to use the method consistently and correctly, and managing side effects. But these are small costs relative to the often grave consequences that can result from not engaging in family planning. For example, pregnancy before adulthood increases the risk of persistent disadvantage across the lifespan (Breen, 2004; Graham, 2007). Inadequate spacing between pregnancies leaves mothers and infants at greater risk of adverse perinatal outcomes, such as preterm birth, as well as longer-term health and social consequences, such as poorer school performance (Conde-Agudelo et al., 2006; Hayes et al., 2006). Unintended pregnancy has been independently associated with adverse consequences including increased risk of pregnancy complications, depression and poorer psychological wellbeing, domestic violence, school dropout and lost career opportunities (Brown and Eisenberg, 1995; Logan et al., 2007). From this perspective, systematically providing reinforcement in the form of financial incentives contingent on engaging in family planning has tremendous potential as both an efficacious and ethical intervention that bridges the temporal gap between initiating contraception, for example, and collecting the naturalistic but delayed rewards for doing so.
While strong conclusions regarding the efficacy of incentive interventions to promote family planning behaviors cannot be drawn at this time, the existing literature suggests that further research is warranted. General suggestions that would advance this literature include the use of more rigorous study designs and the conduct of statistical analyses. More specific to incentive interventions, much has been learned about the key components of effective incentive interventions that could be readily adapted for interventions that target family planning behaviors (see Higgins et al., 2011). Key principles include objectively verifying that the target response has occurred, minimizing delay in delivering consequences following verification, and using a consequence of sufficient magnitude or intensity to function as an effective reinforcer. Regarding objective verification of the target behavior, potential problems encountered in past studies with having to rely on self-report of contraceptive use and/or pregnancy may be more easily dealt with given modern methods of contraception and pregnancy testing. For example, a number of the more effective contraceptive methods such as depot injections, IUDS, and implants, require administration or insertion/removal by a health care professional, thus making their use more readily verifiable. In addition, simple but sensitive urine dip strip tests can detect pregnancy earlier and less expensively than in the past. Regarding minimization of delay, it appears that most of the studies included in the review delivered the incentive in a timely manner. The significant delay in the availability of incentive earnings in the Ridker and Sun & Cernada studies was intentional on their part – the interventions were designed to provide participants something akin to a modern 401 K or 529 plan. In future studies, efforts such as those described by Ridker to keep the contingencies and the incentives collected salient by distributing account statements on a regular basis could help counteract the delay. Regarding the magnitude of the incentive, while larger magnitudes are typically more efficacious, as Thapa et al.’s results suggest, care must be taken with this class of behaviors that the magnitude does not become coercive. Much more research is needed to determine optimal incentive values, schedules, and targets, but the extant literature suggests family planning behaviors will be sensitive.
Overall, the existing literature on incentives to promote family planning behaviors provides preliminary evidence that these behaviors are sensitive to incentives and that future research in this area is warranted, especially given urgent, ongoing need to better manage population growth worldwide. It is hoped that by reviewing this literature, the interest of the family planning literature in this approach will be reinvigorated. In addition, it is hoped that including this review in this broader supplemental issue on incentives and health will introduce this topic to incentives experts and inspire them to undertake empirical work in this critical area.
Acknowledgments
Preparation of this manuscript was supported by research grants R34 DA030534 and T32 DA07242 from the National Institute on Drug Abuse. The study sponsor had no involvement in the preparation of the manuscript.
Footnotes
Conflict of Interest The authors declare there is no conflict of interest.
References
- Ashford LS, Noble JA. Population policy: consensus and challenges. Consequences. 1996;2:25–36. [Google Scholar]
- Baird S, Chirwa E, McIntosh C, Özler B. The short-term impacts of a schooling conditional cash transfer program on the sexual behavior of young women. Health Econ. 2010;19:55–68. doi: 10.1002/hec.1569. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA. Toward a behavioral economic understanding of drug dependence: delay discounting processes. Addiction. 2001;96:73–86. doi: 10.1046/j.1360-0443.2001.961736.x. [DOI] [PubMed] [Google Scholar]
- Breen R, editor. Social Mobility in Europe. Oxford University Press; Oxford: 2004. [Google Scholar]
- Brown SS, Eisenberg L, editors. The Best Intentions: Unintended Pregnancy and the Well-Being of Children and Families. National Academy Press; Washington, DC: 1995. [PubMed] [Google Scholar]
- Chomitz KM, Birdsall N. Incentives for Small Families: Concepts and Issues. Proceedings of the World Bank Annual Conference on Development Economics. 1990:309–349. [Google Scholar]
- Cleland J, Robinson W. The use of payments and benefits to influence reproductive behaviour. In: Phillips JF, Ross JA, editors. Family Planning Programmes and Fertility. Clarendon Press; Oxford: 1992. pp. 159–177. [Google Scholar]
- Conde-Agudelo A, Rosas-Bermudez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006;295:1809–1823. doi: 10.1001/jama.295.15.1809. [DOI] [PubMed] [Google Scholar]
- de Silva V, Thapa S, Wilkens LR, Farr MG, Jayasinghe K, McMahan JE. Compensatory payments and vasectomy acceptance in urban Sri Lanka. J. Biosoc. Sci. 1988;20:143–156. doi: 10.1017/s0021932000017387. [DOI] [PubMed] [Google Scholar]
- Elder JP, Estey JD. Behavior change strategies for family planning. Soc. Sci. Med. 1992;35:1065–1076. doi: 10.1016/0277-9536(92)90246-m. [DOI] [PubMed] [Google Scholar]
- Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect. Sex Reprod. Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- Finnigan OD, Sun TH. Planning, starting, and operating an educational incentives project. Stud. Fam. Plann. 1972;3:1–7. [PubMed] [Google Scholar]
- Graham H. Unequal Lives: Health and Socioeconomic Inequalities. Open University Press; Maidenhead: 2007. [Google Scholar]
- Green L, Meyerson J, Lichtman D, Rosen D, Fry A. Temporal discounting in choice between delayed rewards: the role of age and income. Psychol. Aging. 1996;11:79–84. doi: 10.1037//0882-7974.11.1.79. [DOI] [PubMed] [Google Scholar]
- Hammerslough CR. Characteristics of women who stop using contraceptives. Fam. Plann. Perspect. 1984;16:14–18. [PubMed] [Google Scholar]
- Hapugalle D, Janowitz B, Weir S, Covington DL, Wilkens L, Aluvihare C. Sterilization regret in Sri Lanka: a retrospective study. Int. Fam. Plann. Perspect. 1989;15:22–28. [Google Scholar]
- Hayes H, Luchok K, Martin AB, McKeown RE, Evans A. Short birth intervals and the risk of school unreadiness among a Medicaid population in South Carolina. Child Care Health Dev. 2006;32:423–430. doi: 10.1111/j.1365-2214.2006.00624.x. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Silverman K. Contingency management. In: Galanter M, Kleber HD, editors. Substance Abuse Treatment. American Psychiatric Publishing, Inc.; Arlington, VA: 2008. pp. 387–399. [Google Scholar]
- Higgins ST, Silverman K, Washio Y. Contingency Management. In: Galanter M, Kleber HD, editors. Psychotherapy for the Treatment of Substance Abuse. 6th ed American Psychiatric Publishing, Inc.; Washington, D.C.: 2011. pp. 193–218. [Google Scholar]
- Jaroni JL, Wright SM, Lerman C, Epstein LH. Relationship between education and delay discounting in smokers. Addict. Behav. 2004;29:1171–1175. doi: 10.1016/j.addbeh.2004.03.014. [DOI] [PubMed] [Google Scholar]
- Khan ME, Prasad CVS. Fertility control in India: a critical evaluation of the role of incentives in promoting sterilization among industrial workers. Manohar Publishers; New Delhi, India: 1980. [Google Scholar]
- Kulkarni PM, Rani S. Recent fertility declines in China & India: a comparative view. Asia Pac. Popul. J. 1995;10:53–74. [PubMed] [Google Scholar]
- Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298:2415–2417. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- Logan C, Holcombe E, Manlove J, Ryan S. The Consequences of Unintended Childbearing: A White Paper. The National Campaign to Prevent Teen and Unplanned Pregnancy and Child Trends, Inc.; [accessed 18 December 2011]. 2007. Available at: http://www.thenationalcampaign.org/resources/pdf/consequences.pdf. (Archived by WebCite® at http://www.webcitation.org/6426Y0OjA) [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Mauldin WP. Assessment of national family planning programs in developing countries. Stud. Fam. Plann. 1975;6:30–36. [PubMed] [Google Scholar]
- Perkin GW. Nonmonetary commodity incentives in family planning programs: a preliminary trial. Stud. Fam. Plann. 1970;1:12–15. [PubMed] [Google Scholar]
- Repetto R. A case study of the Madras vasectomy program. Stud. Fam. Plann. 1968;31:8–16. [Google Scholar]
- Ridker RG. The No-Birth Bonus Scheme: the use of savings accounts for family planning in south India. Popul. Dev. Rev. 1980;6:31–46. [Google Scholar]
- Rogers EM. Incentives in the diffusion of family planning innovations. Stud. Fam. Plann. 1971;2:241–248. [PubMed] [Google Scholar]
- Simon JL. Income, wealth, and their distribution as policy tools in fertility control. In: Ridker RG, editor. Population and Development: The Search for Selective Interventions. Johns Hopkins University Press; Baltimore: 1976. pp. 36–76. [Google Scholar]
- Srinivasan K, Kachirayan M. Vasectomy follow-up study: findings and implications. Bulletin of the Gandhigram Institute of Rural Health and Family Planning. 1968;3:12–32. [Google Scholar]
- Stevens JR, Stevens CM. Introductory small cash incentives to promote child spacing in India. Stud. Fam. Plann. 1992;23:171–186. [PubMed] [Google Scholar]
- Stevens-Simon C, Dolgan JI, Kelly L, Singer D. The effect of monetary incentives and peer support groups on repeat adolescent pregnancies: a randomized trial of the Dollar-a-Day program. J. Am. Med. Assoc. 1997;277:977–982. [PubMed] [Google Scholar]
- Sun TH, Cernada GP. Beyond family planning: Incentives in Taiwan. Int. Q. Community Health Educ. 1985–6;6:241–251. doi: 10.2190/VWBE-QHGB-M1WX-MM1F. [DOI] [PubMed] [Google Scholar]
- Thapa S, Abeywickrema D, Wilkens LR. Effects of compensatory payments on vasectomy acceptance in urban Sri Lanka: a comparison of two economic groups. Stud. Fam. Plann. 1987;18:352–360. [Google Scholar]
- Trussell J, Vaughn B. Contraceptive failure, method-related discontinuation and resumption of use: results from the 1995 National Survey of Family Growth. Fam. Plann. Perspect. 1999;31:64–72. [PubMed] [Google Scholar]
- USAID Family Planning. 2011 http://www.usaid.gov/our_work/global_health/pop/
- Weeden D, Bennett A, Lauro D, Viravaidya M. An incentive program to increase contraceptive prevalence in rural Thailand. Int. Fam. Plan. Perspect. 1986;12:11–16. [Google Scholar]


