Abstract
Objective
To estimate the risk of serious adverse reactions to benzathine penicillin in pregnant women for preventing congenital syphilis.
Methods
We searched for clinical trials or cohorts that assessed the incidence of serious adverse reactions to benzathine penicillin in pregnant women and the general population (indirect evidence). MEDLINE, EMBASE, Scopus and other databases were searched up to December 2012. The GRADE approach was used to assess quality of evidence. Absolute risks of each study were calculated along with their 95% confidence intervals (95% CI). We employed the DerSimonian and Laird random effects model in the meta-analyses.
Results
From 2,765 retrieved studies we included 13, representing 3,466,780 patients. The studies that included pregnant women were conducted to demonstrate the effectiveness of benzathine penicillin: no serious adverse reactions were reported among the 1,244 pregnant women included. In the general population, among 2,028,982 patients treated, 4 died from an adverse reaction. The pooled risk of death was virtually zero. Fifty-four cases of anaphylaxis were reported (pooled absolute risk = 0.002%; 95% CI: 0%–0.003% I2 = 12%). From that estimate, penicillin treatment would be expected to result in an incidence of 0 to 3 cases of anaphylaxis per 100,000 treated. Any adverse reactions were reported in 6,377 patients among 3,465,322 treated with penicillin (pooled absolute risk = 0.169%; 95% CI: 0.073%–0.265% I2 = 97%). The quality of evidence was very low.
Conclusion
Studies that assessed the risk of serious adverse events due to benzathine penicillin treatment in pregnant women were scarce, but no reports of adverse reactions were found. The incidence of severe adverse outcomes was very low in the general population. The risk of treating pregnant women with benzathine penicillin to prevent congenital syphilis appears very low and does not outweigh its benefits. Further research is needed to improve the quality of evidence.
Introduction
Over half of syphilis infections in pregnancy will result in congenital syphilis, which can manifest as early fetal loss, stillbirth, prematurity, low birth weight, neonatal death, or infection in the newborn [1]. Benzathine penicillin is the only effective treatment for preventing congenital syphilis [2], [3]. In contrast with other antimicrobials, the effectiveness of penicillin for syphilis and the sensitivity of Treponema pallidum to penicillin remains stable [4]. Since penicillin became available in 1943, the rates of congenital syphilis and deaths due to syphilis have dramatically decreased [4]. The use of penicillin in pregnant women with syphilis significantly reduces the risk of congenital syphilis, perinatal death, stillbirth and preterm delivery [5]–[9]. The global elimination of congenital syphilis is feasible and thus a major priority in public health [10].
Despite the widespread availability, low cost, and effectiveness of penicillin in controlling congenital syphilis, the worldwide incidence is still high [10], and the rates in some countries are increasing [11]–[15]. Annually more pregnancies are adversely affected by syphilis than by HIV infection [3]. Among the multiple causes of the inability to eliminate the mother-to-child transmission of syphilis are concerns about the safety of penicillin injections, mainly in resource-constrained settings and in patients with a history of penicillin allergy [4]. Anecdotal reports suggest that some rural or primary care health workers might not feel comfortable administering injectable penicillin.
In many settings, prior to penicillin benzathine administration, a subcutaneous or subdermal injection of benzathine penicillin is used as a screening method for an allergic reaction [16]. Hypersensitivity to penicillin, however, is often due to minor determinants and other metabolites of penicillin not contained in the parent molecule, which renders such tests limited in their ability to accurately predict whether patients will have an adverse reaction or not. Such testing might provide false positive or false negative results and thus misclassify patients [17]. A detailed clinical history accurately diagnoses hypersensitivity and helps in judging the clinical relevance of the symptoms, as some are not predictive or related to allergy [18]. Careful clinical examination should also be emphasized in patients with suspected penicillin allergy. It has been estimated that 90% of self-reported allergies are mislabeled, often because of confusion between adverse reactions and disease symptoms [19].
While speculations about penicillin hazards are frequent, systematic reviews about the incidence of serious adverse reactions in pregnancy are absent. Such evidence is likely to bring more objectivity to the clinical and policy decisions. Our aim was to review the risk of serious adverse reaction to benzathine penicillin in pregnant women with syphilis.
Methods
Protocol and Registration
The current review was registered on International Prospective Register of Systematic Reviews (PROSPERO), registration number: CRD42012002103.
Eligibility Criteria
We included randomized controlled trials (RCT) or cohort studies that assessed the incidence of serious adverse reactions to benzathine penicillin in pregnant women for preventing congenital syphilis. As indirect evidence, we also included studies that assessed the incidence of adverse reactions to benzathine penicillin in the general population. There were no restrictions for language, length of follow-up, publication date or status.
We used the following adverse reaction definition “an appreciably harmful or unpleasant reaction, resulting from an intervention related to the use of a medicinal product, which predicts hazard from future administration and warrants prevention or specific treatment, or alteration of the dosage regimen, or withdrawal of the product” [20], which includes drug allergy and allergic anaphylaxis [21]. Non-allergic adverse reactions reported by authors such as diarrhea, nausea, and vomiting were also included. We did not consider Jarisch-Herxheimer reaction as an adverse reaction, as its physiopathologic mechanism is related to a reaction to T. pallidum proteins rather than to penicillin [22].
We only included studies that fulfilled all inclusion criteria. If the study did not provide a clear definition of adverse reactions, we reviewed the primary data and assessed which studies contained data that could be categorized using our criteria. Once a study was accepted for inclusion, no patients were reassigned into or out of adverse reaction groups. Results were taken as a group from each study, as individual patient-level reporting was not available.
Information Sources and Search Strategy
We searched the following databases from inception up to January 2013: MEDLINE, EMBASE, Scopus, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Reactions Pharmacovigilance Insight (via OVID), Cochrane Central Register of Controlled Trials (CENTRAL), metaRegister of Current Clinical Trials (mRCT), Latin American and Caribbean Center on Health Sciences Information (LILACS) and Scientific Electronic Library Online (SciELO). References of relevant studies were also screened for eligibility. The search strategy for MEDLINE (via PubMed) is presented on Table S1. This strategy was adapted for searching on the other databases.
Study Selection
Two researchers independently reviewed the retrieved studies based on the analysis of the titles and abstracts (MCM and MCRS). Disagreements were resolved by authors’ consensus or by a third reviewer (TFG).
Data Collection Process
We created a data extraction form to assemble previously defined relevant information from the studies: country, study design, dates of enrollment, population, penicillin regimen, sample size and adverse reactions. One author extracted the data (TFG) and another (MTS) confirmed the extracted information. We contacted studies’ corresponding authors to obtain any additional data not stated in the reports. We labeled the study as “confirmed multiple exposure” if all the patients of the study received more than one dose of penicillin.
Risk of Bias and Quality of Evidence Assessment
To assess the risk of bias in the randomized clinical trials, we considered the Cochrane Collaboration’s tool [23]. For observational studies we assessed: eligibility criteria, measurements of exposures and outcomes, control of confounding, and follow-up [24].
We used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to assess the quality of the evidence [25]. This method rates the quality of evidence as high, moderate, low or very low. We ranked the outcomes as critical, important or not important and then assessed study limitations (risk of bias), inconsistency, indirectness of evidence, imprecision, publication bias, and factors that could increase the quality of the evidence. The quality assessment was considered when interpreting the findings.
Data Analysis
The primary outcome measured was the incidence of serious adverse reactions in pregnant women due to treatment with benzathine penicillin for preventing congenital syphilis. As serious adverse reactions we considered anaphylaxis and death, but we did not summarize them as a composite outcome.
Absolute risks from individual studies were recalculated and presented along with 95% confidence intervals (95% CI) by the Mid-P test [26]. From the resulting confidence intervals, we did meta-analyses by random effects model using the method of DerSimonian and Laird [27]. As the incidence was small, we adjusted the values with exponential and natural logarithm function [28]. We did all the analysis on STATA (v. 10.1) statistical package. Chi2, I2 and Tau2 tests were calculated to estimate heterogeneity. We performed sensitivity analysis to identify the potential sources of heterogeneity across studies.
Results
Study Selection
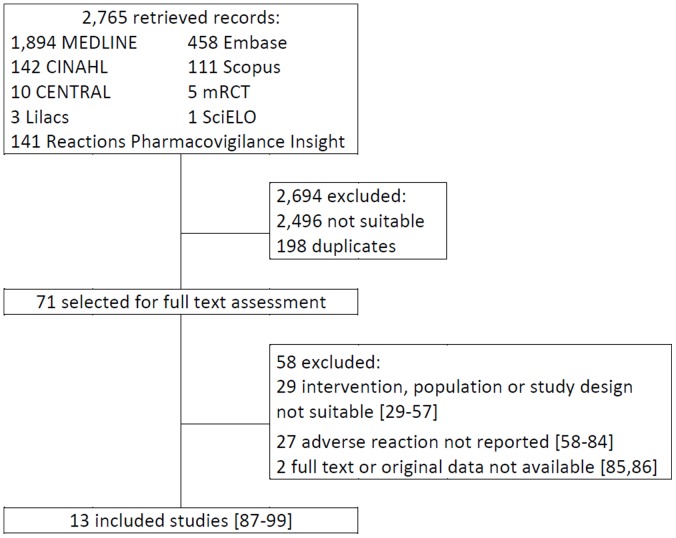
Our literature search identified 2,765 articles (Figure 1). After screening the titles and abstracts, 71 were selected for full text assessment [29]–[99], and 13 were included in the review (N = 3,466,780 patients) [87]–[99].
Figure 1. Results of search, selection and inclusion of studies in the review.
Study Characteristics
We could not identify any studies whose primary objective was to measure the incidence of adverse reactions in pregnant women with syphilis treated with benzathine penicillin. Studies that included pregnant women aimed to assess the effectiveness of benzathine penicillin for preventing congenital syphilis, and the incidence of adverse reactions was recorded as a secondary endpoint. All studies included in our review had a cohort design, either prospective or retrospective. The benzathine penicillin regimen varied from 1 to 4 doses of 1.2 million international units (MIU) and its use was compared to no treatment or erythromycin, or no comparison was done. Table 1 depicts the main characteristics of the included studies.
Table 1. Main characteristics of included studies.
| Study | Studydesign | Dates of enrolment | Country | Population(diagnosis method if available) | Benzathinepenicillin regimen | Control group |
| Shafer 1954 [87] | prospective cohort | 1950–1952 | USA | adults with sexually transmitted diseases | 1 or 2 doses of 2.4 MIU, IM* | no control group |
| Smith 1956 [88] | prospective cohort | 1946–1950 | USA | adults with syphilis or gonorrhea | 1, 2 or 3 doses of 2.4 MIU, IM | no control group |
| Willcox 1957 [89] | prospective cohort | 1946–1956 | USA | adults with syphilis or gonorrhea | 1 to 4 doses of 2.4 MIU, IM | no control group |
| Hsu 1958 [90] | prospective cohort | several years | USA | adults with rheumatic fever | 1.2 MIU, IM every fourweeks for several years | no control group |
| Phaosavasdi 1989 [91] | prospective cohort | 1984–1985 | Thailand | pregnant women with positive treponemal serological test (RPR, VDRL, TPHA) | 1, 2 or 3 doses of 2.4 MIU, IM | erythromycin 2 g dailyper 30 days, orally |
| International rheumatic fever group 1991 [92] | prospective cohort | 1988–1990 | 11 countries† | adults and children with rheumatic fever | 1.2 MIU, IM every 4weeks for three years | no control group |
| Jenniskens 1995 [93] | prospective cohort | 1992–1993 | Kenya | pregnant women with positivetreponemal serological test (RPR) | 2.4 MIU, IM | no treatment |
| Napoli 2000 [94] | prospective cohort | 1999–2000 | USA | adults with streptococcal pharyngitisprophylaxis | 1.2 MIU, IM | no control group |
| Apter 2004 [95] | prospective cohort | 1987–2001 | UK | adults and children who received penicillin prescription | 1 or 2 prescriptions of penicillin* | no control group |
| Watson-Jones 2005 [96] | retrospective cohort | 2000–2001 | Tanzania | pregnant women with positive treponemalserological test (RPR, TPHA, FTA-ABS) | 1 dose of 2.4 MIU, IM | no treatment |
| Bronzan 2007 [97] | prospective cohort | 2001–2002 | South Africa | pregnant women with primary, secondary,or early latent syphilis (RPR, TPHA) | 1, 2 or 3 doses of 2.4 MIU, IM | no treatment |
| Carles 2008 [98] | retrospective cohort | 1992–2004 | French Guiana | pregnant women with positive treponemalserological test (VDRL, TPHA) | 1, 2 or 3 doses of 2.4 MIU, IM | no treatment |
| Li 2012 [99] | retrospective cohort | 2001–2008 | China | adults with sexually transmitted diseases | 3 doses of 2.4 MIU, IM | erythromycin 2 g daily per14 days, orally ordoxycycline 200 mg orallyfor 15 days |
Notes:
It may have been included also patients treated with other types of penicillin.
Argentina, Chile, China, India, Jamaica, Korea, Kuwait, New Zealand, Taiwan, Thailand, Venezuela.
Abbreviations:
MIU: mega internacional units.
IM: intramuscular.
RPR: Rapid Plasma Reagin.
VDRL: Veneral Disease Research Laboratory.
TPHA: Treponema Pallidum Hemagglutination.
MHA-TP: microhemagglutination T. pallidum.
FTA-ABS: test or fluorescent treponemal antibody–absorption.
Quality of the Evidence
The quality of evidence of all outcomes was considered very low (Table 2). The quality was rated down from low, because of the observational design of the studies, to very low, due to limitations (mainly on the measurement of outcome, as the studies were not designed to report the incidence of adverse reactions in pregnant women), inconsistency (high heterogeneity), and indirectness (population different from pregnant woman with syphilis).
Table 2. Quality of evidence profile for the assessed outcomes, adapted from GRADE [25].
| Outcome (population) | Quality assessment | Quality | Importance | ||||
| N. studies | Limitation | Inconsistency | Indirectness | Imprecision | |||
| death (pregnant women) | five [91], [93], [96]–[98] | serious * | − | − | very low | Critical | |
| death (general population) | eight [87]–[90], [92], [94], [95], [99] | serious† | no important inconsistency | very serious§ | no important imprecision | very low | Critical |
| anaphylaxis (pregnant women) | five [91], [93], [96]–[98] | serious* | − | − | very low | Critical | |
| anaphylaxis(general population) | eight [87]–[90], [92], [94], [95], [99] | serious† | no important inconsistency | very serious§ | no important imprecision | very low | Critical |
| incidence of adverse reactions(pregnant women) | five [91], [93], [96]–[98] | serious* | − | − | very low | Important | |
| incidence of adverse reactions(general population) | eight [87]–[90], [92], [94], [95], [99] | serious† | very serious‡ | very serious§ | no important imprecision | very low | Important |
Notes:
All studies had observational design.
Publication bias could not be objectively assessed due to the small numbers of studies.
Imprecision could not be assessed since adequate meta-analysis calculation could not be performed.
RR: relative risk.
NE: Non-estimable.
−We could not access the item for this outcome.
Flawed measurement of outcome, as the study did not aimed to report the incidence of adverse reaction in pregnant women.
Some studies did not report the incidence of adverse reaction; the data was obtained with the authors.
Heterogeneous results across studies were observed.
Different population (patients were not pregnant women and did not have syphilis) and intervention. In one study [95] other types of penicillin, besides benzathine, may have been used.
Absolute Risk from Individual Studies and Pooled Results
Studies did not report any case of anaphylaxis or death in pregnant women treated with benzathine penicillin. The incidence of adverse reactions in this population is presented on Table 3. In total 1,244 women were assessed and only one case of skin rash was reported. As all studies had null events, a meta-analysis was not possible.
Table 3. Incidence of adverse reactions in pregnant women treated with benzathine penicillin for preventing congenital syphilis, 1954–2012.
| Study | Penicillin treatment group | No penicillin treatment group | ||
| No. of patients | Events | No. of patients | Events | |
| Phaosavasdi 1989 [91] | 191 | 1* | 6 | 0 |
| Jenniskens 1995 [93] | 751 | 0† | 109 | 0† |
| Watson-Jones 2005 [96] | 88 | 0† | 56 | 0† |
| Bronzan 2007 [97] | 141 | 0† | 31 | 0† |
| Carles 2008 [98] | 73 | 0† ‡ | 12 | 0† |
Notes:
Skin rash.
Data obtained from contact with corresponding author.
All patients received dexamethasone injection.
In studies whose primary objective was to evaluate the incidence of adverse reactions from benzathine penicillin treatment, no pregnant women were included. From 2,028,982 patients treated with benzathine penicillin, 4 died from an adverse reaction (Table 4). The absolute risk of individual studies ranged from 0% (95% CI: 0%–0.274%) to 3.125% (95% CI: 0.156%–14.460%) and the pooled risk of death was zero (I2 = 0%).
Table 4. Incidence of anaphylaxis or death in general population treated with benzathine penicillin: individual and pooled results, 1954–2012.
| Individual studies orpooled results | No. ofpatients | Death | Anaphylaxis | ||
| Events | Absolute risk (95% CI) | Events | Absolute risk % (95% CI) | ||
| Shafer 1954 [87] | 70,037 | 2 | 0.003 (0.001–0.009) | 0 | 0 (0–0.004) |
| Smith 1956 [88] | 7,109 | 0 | 0 (0–0.042) | 0 | 0 (0–0.042) |
| Willcox 1957 [89] | 895 | 0 | 0 (0–0.334) | 0 | 0 (0–0.334) |
| Hsu 1958 [90] | 32 | 1 | 3.125 (0.156–14.460) | 1 | 3.125 (0.156–14.460) |
| International rheumatic fevergroup 1991 [92] | 1,790 | 1 | 0.126 (0.006–0.623) | 4 | 0.223 (0.071–0.538) |
| Napoli 2000 [94] | 9,203 | 0 | 0 (0–0,032) | 2 | 0.022 (0.004–0.072) |
| Apter 2004 [95] | 2,017,957 | 0 | 0 (0–0,001) | 47* | 0.001 (0,002–0,003) |
| Li 2012 [99] | 1,094 | 0‡ | 0 (0–0.274) | 0‡ | 0 (0–0.274) |
| Pooled result | 2,108,117 | 4 | 0 (0–0); I2 = 0% | 54 | 0.002 (0–0.003); I2 = 12% |
Notes:
16 patients had anaphylaxis after the first prescription of penicillin and 32 had anaphylaxis after the second prescription of penicillin. One patient had anaphylaxis in both prescriptions. Total patients that experienced anaphylaxis in this study = 47.
There were reported 16 events of Jarisch-Herxheimer reaction, which were not considered adverse drug reaction in present review.
Fifty four patients of 2,028,982 treated with penicillin suffered anaphylaxis. Across studies, the absolute risk ranged from 0% (95% CI: 0%–0.004%) to 3.125% (95% CI: 0.156%–14.460%). Studies that included patients with multiple exposures to penicillin had a higher incidence of anaphylaxis [90], [92]. The pooled risk from the meta-analysis was 0.002% (95% CI: 0%–0.003%; I2 = 12%); from this estimate we can expect 0 to 3 cases of anaphylaxis per 100,000 treated patients.
For any adverse reaction 6,377 cases were observed among 3,465,322 treated patients (Table 5); no pregnant women were assessed. The absolute risk ranged from 0% (95% CI: 0%–0.274%) to 18.750% (95% CI: 7.968%–34.980%) among studies. The risk was higher in studies that included patients with confirmed multiple exposures to penicillin [90], [92], [95], [99], when compared with the ones in which the patients received only one dose of penicillin or multiple exposure to penicillin was not confirmed [87]–[89], [94], [95].
Table 5. Incidence of adverse reactions in general population treated with benzathine penicillin: individual and pooled results, 1954–2012.
| Individual studies orpooled results | No. ofpatients | Events | Absolute risk % (95% CI) | Type of adverse reaction(n of patients, if available) |
| Shafer 1954 [87] | 70,037 | 56* | 0.080 (0.061–0.103)* | only severe adverse events reported; type not available |
| Smith 1956 [88] | 7,109 | 18 | 0.253 (0.155–0.392) | urticaria, nausea and vomiting |
| Willcox 1957 [89] | 895 | 26† | 2.905 (1.947–4.168) | urticaria, urticaria, edema, asthma, rash, dyspnea, tetany, faintness, dizziness, diarrhea, urticaria, vomiting |
| Hsu 1958 [90] | 32 | 6 | 18.750 (7.968–34.980) | anaphylaxis (1), edema of lips, pruritic eruption (3), serum sickness (2) |
| International rheumatic fever group 1991 [92] | 1,790 | 57 | 3.184 (2.443–4.077) | pruritus or urticaria (33), macopapular rashes (11), arthralgia (8), anaphylaxis (4), wheeze (1) |
| Napoli 2000 [94] | 9,203 | 2* | 0.022 (0.004–0.072)* | anaphylaxis (2) |
| Apter 2004 [95] – one prescription of penicillin | 3,375,162 | 6,212 | 0.184 (0.179–0.189) | allergic-like event: adverse drug reaction, anaphylaxis, angioedema, erythema multiforme, toxic epidermal necrolysis, urticaria |
| Apter 2004 [95] – two prescriptions of penicillin within 60 days | 2,017,957‡ | 3,509‡ | 0.174 (0.168–0.180) | |
| Li 2012 [99] | 1094 | 0§ | 0 (0–0.274) | None|| |
| Pooled result¶ | 3,465,322 | 6,377 | 0.169 (0.073–0.265); I2 = 97% | − |
Notes:
Only severe adverse reaction was reported.
Probable cases.
These cases are included in the previous data (one penicillin prescription).
Data obtained from contact with corresponding author.
The study reported 16 events of Jarisch-Herxheimer reaction, but we did not consider them as adverse events.
For the polled result only the incidence of adverse reaction with one prescription of penicillin was considered for Apter 2004 [95] study.
The pooled risk for any adverse reaction was 0.169% (0.073%–0.265%; I2 = 97%). The statistical heterogeneity was very high. In the sensitivity analysis we investigated the effect of older studies, the level of country economic development where the studies were conducted, the stage of disease, and the dosing regimens. It is clear that studies were performed in different decades and settings, and this may be the main causes of the heterogeneity we found, but we could not identify the statistical sources of heterogeneity, nor could we derive more homogeneous results from the sensitivity analysis.
Discussion
Our findings show that the incidence of serious adverse reactions to benzathine penicillin in pregnant women was very low: no severe or fatal cases were reported. In the general population, a study population with a much larger sample size, the risk of serious adverse reactions was also small, and the pooled risk of death due to penicillin treatment was virtually zero. We rated the quality of the evidence as very low, resulting in a classification of the final evidence as inconclusive. Studies that assessed benzathine penicillin effectiveness in pregnant women did not plan the sample size to measure adverse reactions, therefore the statistical power to detect low frequency adverse reactions was suboptimal [100]. Further well-designed studies may change or confirm the findings [25].
Patients with multiple exposures to benzathine penicillin had a higher incidence of adverse reactions. That finding correlates with clinical data in which patients with more frequent exposure to penicillin have a higher chance of experiencing adverse reactions [101].
Most of the studies had no events of serious adverse reactions, which hampered the summarization of the risk. To conduct a meta-analysis, we tried different approaches, like replacing the zero events with 0.5 [102], and excluding the studies without events from the analysis. Such attempts overestimated the risk and we considered those results inadequate. The method of DerSimonian and Laird [27], calculated from confidence intervals of individual studies, was the best model to estimate the risk and was selected to estimate the pooled risk. Even using that method, in situations with very low rates like the risk of death in the general population, the pooled estimate resulted in “zero” risk. The risk does exist; studies reported four events in more than two million patients. But the meta-analysis – weighting the events by each study population – resulted in rounding the result to zero.
The included studies were performed in different decades, and disparate benzathine penicillin regimens and stages of disease were assessed. It is possible that the diagnosis of adverse reaction varied across studies, as well as the benzathine penicillin preparation and adjunct components, with greater variation in the older studies. A possible measurement bias may derive from study design, but this factor could not be investigated due to the low number of retrospective as compared with prospective studies. Such clinical and methodological diversity might explain the heterogeneity observed on the outcome of any adverse reaction and raises concerns about the external validity of the data [23], [28].
Given the widely documented effectiveness of benzathine penicillin in preventing adverse pregnancy outcomes in mothers with syphilis such as stillbirth, preterm delivery, perinatal death and congenital syphilis [5]–[9], limiting access to benzathine penicillin due to concerns about adverse penicillin reactions cannot be justified. However, in all settings in which benzathine penicillin is administered, it is critical that providers have adequate training and resources to provide sterile injections and management of anaphylaxis. A component of such training should include the routine assessment of a history of allergic reactions to antibiotics including penicillin. A history of penicillin allergy seems a good screening measure to predict the likelihood of a serious reaction. Those with a positive history of penicillin allergy might still benefit from targeted hypersensitivity testing to exclude a true allergy, if available [18].
Even though the risk of death and serious adverse reactions due to benzathine penicillin seem to be very low, research is needed to specifically determine and monitor the incidence of adverse reactions in pregnant women, including a more clear understanding of the rates of mild, moderate and severe adverse reactions. Large medical databases, for example, could provide a better estimate of the incidence of adverse reactions in the population [103], [104]. Furthermore, countries should consider actively monitoring the frequency of adverse events due to benzathine penicillin administration in pregnant women through pharmacovigilance systems [105].
It is also reasonable that researchers include the incidence and type of adverse reaction as one of the outcomes when designing prospective studies of benzathine penicillin use in pregnancy. In our literature search we found many studies that could have added more information to the present evidence base if the incidence and type of adverse reaction had been systematically recorded [58]–[61], [67]–[75], [80]–[82].
Conclusion
No case of serious adverse reactions to benzathine penicillin in pregnant women was reported and in the general population the incidence was very low. For clinical practice and public health policy our findings suggest that the risk of adverse reactions does not outweigh the benefits of benzathine penicillin use for maternal syphilis treatment and congenital syphilis prevention. Health authorities should eliminate any policy barriers to the administration of benzathine penicillin. Future studies about penicillin use should record the incidence and type of adverse reactions during pregnancy. Such research efforts are likely to strengthen the available evidence.
Supporting Information
Search strategy for MEDLINE (via PubMed).
(DOCX)
Acknowledgments
We would like to thank our collaborators from the University of Brasilia, Marcia Cristina de Sousa Reis and Mariana Correia Marques, for helping in the study-selection process.
Funding Statement
This research was partially funded by the Centro Latinoamericano de Perinatología/Salud de la Mujer y Reproductiva (CLAP/SMR), Pan-American Health Organization, World Health Organization. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO (2012) Investment case for eliminating mother-to-child transmission of syphilis: promoting better maternal and child health and stronger health systems. Geneva: World Health Organization.
- 2. Workowski KA, Berman S (2010) CDC (2010) Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep 59: 1–110. [PubMed] [Google Scholar]
- 3.WHO (2003) Guidelines for the management of sexually transmitted infections. Geneva: World Health Organization. [PubMed]
- 4. Douglas JM (2009) Penicillin treatment of syphilis: clearing away the shadow on the land. JAMA 301: 769–771. [DOI] [PubMed] [Google Scholar]
- 5. Wendel GD, Sheffield JS, Hollier LM, Hill JB, Ramsey PS, et al. (2002) Treatment of syphilis in pregnancy and prevention of congenital syphilis. Clin Infect Dis 35: S200–209. [DOI] [PubMed] [Google Scholar]
- 6. Menezes EV, Yakoob MY, Soomro T, Haws RA, Darmstadt GL, et al. (2009) Reducing stillbirths: prevention and management of medical disorders and infections during pregnancy. BMC Pregnancy Childbirth 9 Suppl 1 S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barros FC, Bhutta ZA, Batra M, Hansen TN, Victora CG, et al. (2010) Global report on preterm birth and stillbirth (3 of 7): evidence for effectiveness of interventions. BMC Pregnancy Childbirth 10 Suppl 1 S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hawkes S, Matin N, Broutet N, Low N (2011) Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect Dis 11: 684–691. [DOI] [PubMed] [Google Scholar]
- 9. Blencowe H, Cousens S, Kamb M, Berman S, Lawn JE (2011) Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health 11 Suppl 3 S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamb ML, Newman LM, Riley PL, Mark J, Hawkes SJ, et al.. (2010) A road map for the global elimination of congenital syphilis. Obstet Gynecol Int 2010. [DOI] [PMC free article] [PubMed]
- 11. Chen ZQ, Zhang GC, Gong XD, Lin C, Gao X, et al. (2007) Syphilis in China: results of a national surveillance programme. Lancet 369: 132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention CDC (2010) Congenital syphilis - United States, 2003–2008. MMWR Morb Mortal Wkly Rep 59: 413–417. [PubMed] [Google Scholar]
- 13. Reyna-Figueroa J, Esparza-Aguilar M, Hernández-Hernández LeC, Fernández-Canton S, Richardson-Lopez Collada VL (2011) Congenital syphilis, a reemergent disease in Mexico: its epidemiology during the last 2 decades. Sex Transm Dis 38: 798–801. [DOI] [PubMed] [Google Scholar]
- 14. Meyer Sauteur PM, Trück J, Bosshard PP, Tomaske M, Morán Cadenas F, et al. (2012) Congenital syphilis in Switzerland: gone, forgotten, on the return. Swiss Med Wkly 141: w13325. [DOI] [PubMed] [Google Scholar]
- 15. Tridapalli E, Capretti MG, Reggiani ML, Stronati M, Faldella G, et al. (2012) Congenital syphilis in Italy: a multicentre study. Arch Dis Child Fetal Neonatal Ed 97: F211–213. [DOI] [PubMed] [Google Scholar]
- 16. Warrington RJ, Simons FE, Ho HW, Gorski BA (1978) Diagnosis of penicillin allergy by skin testing: the Manitoba experience. Can Med Assoc J 118: 787–791. [PMC free article] [PubMed] [Google Scholar]
- 17. Sussman GL, Davis K, Kohler PF (1986) Penicillin allergy: a practical approach to management. CMAJ 134: 1353–1356. [PMC free article] [PubMed] [Google Scholar]
- 18. Lagacé-Wiens P, Rubinstein E (2012) Adverse reactions to β-lactam antimicrobials. Expert Opin Drug Saf 11: 381–399. [DOI] [PubMed] [Google Scholar]
- 19. Solensky R (2012) Allergy to β-lactam antibiotics. J Allergy Clin Immunol 130: 1442–1442.e1445. [DOI] [PubMed] [Google Scholar]
- 20. Edwards IR, Aronson JK (2000) Adverse drug reactions: definitions, diagnosis, and management. Lancet 356: 1255–1259. [DOI] [PubMed] [Google Scholar]
- 21. Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, et al. (2004) Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 113: 832–836. [DOI] [PubMed] [Google Scholar]
- 22. Pound MW, May DB (2005) Proposed mechanisms and preventative options of Jarisch-Herxheimer reactions. J Clin Pharm Ther 30: 291–295. [DOI] [PubMed] [Google Scholar]
- 23.Higgins J, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 ed: The Cochrane Collaboration.
- 24. Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, et al. (2011) GRADE guidelines: 4. Rating the quality of evidence–study limitations (risk of bias). J Clin Epidemiol 64: 407–415. [DOI] [PubMed] [Google Scholar]
- 25. Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, et al. (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64: 401–406. [DOI] [PubMed] [Google Scholar]
- 26. Berry G (1995) Mid-P confidence intervals: a brief review. The Statistician 44: 417–423. [Google Scholar]
- 27.Deeks JJ, Altman DG, Bradburn MJ (2001) Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M SG, Altman DG, editor. Systematic Reviews in Health Care: Meta-analysis in context. 2nd ed. London: BMJ Publishing Group.
- 28.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2009) Introduction to meta-analysis. Chichester: Wiley.
- 29. Willcox RR (1958) Penicillin reactions: analysis of a WHO questionnaire. Bull World Health Organ 18: 457–460. [PMC free article] [PubMed] [Google Scholar]
- 30. Willcox RR (1964) Influence of penicillin allergic reactions on veneral disease control programmes. Br J Vener Dis 40: 200–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Morton RS (1957) Side-effects of penicillin treatment. Br J Vener Dis 33: 176–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sciple GW, Knox JM, Montgomery CH (1959) Incidence of penicillin reactions after an antihistaminic simultaneously administered parenterally. N Engl J Med 261: 1123–1125. [DOI] [PubMed] [Google Scholar]
- 33. Bowell P, Mayne K, Puckett A, Entwistle C, Selkon J (1989) Serological screening tests for syphilis in pregnancy: results of a five year study (1983–87) in the Oxford region. J Clin Pathol 42: 1281–1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ricci JM, Fojaco RM, O’Sullivan MJ (1989) Congenital syphilis: the University of Miami/Jackson Memorial Medical Center experience, 1986–1988. Obstet Gynecol. United States. 687–693. [PubMed]
- 35. King PA, Duthie SJ, Ma HK (1990) Sexually transmitted diseases amongst pregnant Vietnamese refugees in Hong Kong. Genitourin Med 66: 257–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Donders GG, Desmyter J, De Wet DH, Van Assche FA (1993) The association of gonorrhoea and syphilis with premature birth and low birthweight. Genitourin Med 69: 98–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rutgers S (1993) Syphilis in pregnancy: a medical audit in a rural district. Cent Afr J Med 39: 248–253. [PubMed] [Google Scholar]
- 38.McFarlin BL, Bottoms SF (1995) Maternal syphilis in Michigan: the challenge to prevent congenital syphilis. Midwifery. Scotland. 55–60. [DOI] [PubMed]
- 39. Blank S, McDonnell DD, Rubin SR, Neal JJ, Brome MW, et al. (1997) New approaches to syphilis control. Finding opportunities for syphilis treatment and congenital syphilis prevention in a women’s correctional setting. Sex Transm Dis 24: 218–226. [DOI] [PubMed] [Google Scholar]
- 40. Cameron ST, Thong KJ, Young H, Liston WA (1997) Routine antenatal screening for syphilis in Lothian: a study of the results 1988 to 1994. Br J Obstet Gynaecol 104: 734–737. [DOI] [PubMed] [Google Scholar]
- 41. Nathan L, Bohman VR, Sanchez PJ, Leos NK, Twickler DM, et al. (1997) In utero infection with Treponema pallidum in early pregnancy. Prenat Diagn 17: 119–123. [DOI] [PubMed] [Google Scholar]
- 42. Lee MJ, Hallmark RJ, Frenkel LM, Del Priore G (1998) Maternal syphilis and vertical perinatal transmission of human immunodeficiency virus type-1 infection. Int J Gynaecol Obstet 63: 247–252. [DOI] [PubMed] [Google Scholar]
- 43. Hurtig AK, Nicoll A, Carne C, Lissauer T, Connor N, et al. (1998) Syphilis in pregnant women and their children in the United Kingdom: results from national clinician reporting surveys 1994–7. BMJ 317: 1617–1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Swain GR, Kowalewski SJ, Schubot DB (1998) Reducing the incidence of congenital syphilis in Milwaukee: a public/private partnership. Am J Public Health 88: 1101–1102. [PubMed] [Google Scholar]
- 45. Fitzgerald DW, Behets FMT, Lucet C, Roberfroid D (1998) Prevalence, burden, and control of syphilis in Haiti’s rural artibonite region. International Journal of Infectious Diseases 2: 127–131. [DOI] [PubMed] [Google Scholar]
- 46.Blank S, Sternberg M, Neylans LL, Rubin SR, Weisfuse IB, et al.. (1999) Incident syphilis among women with multiple admissions to jail in New York City. J Infect Dis. United States. 1159–1163. [DOI] [PubMed]
- 47. Wabwire-Mangen F, Gray RH, Mmiro FA, Ndugwa C, Abramowsky C, et al. (1999) Placental membrane inflammation and risks of maternal-to-child transmission of HIV-1 in Uganda. J Acquir Immune Defic Syndr 22: 379–385. [DOI] [PubMed] [Google Scholar]
- 48. Heikkinen T, Laine K, Neuvonen PJ, Ekblad U (2000) The transplacental transfer of the macrolide antibiotics erythromycin, roxithromycin and azithromycin. BJOG 107: 770–775. [DOI] [PubMed] [Google Scholar]
- 49. Bique Osman N, Challis K, Folgosa E, Cotiro M, Bergström S (2000) An intervention study to reduce adverse pregnancy outcomes as a result of syphilis in Mozambique. Sex Transm Infect 76: 203–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ramsey PS (2000) Pharmacokinetics of azithromycin in the term gravida. Infect Dis Obstet Gynecol 8: 203. [Google Scholar]
- 51.Sheffield JS, Sanchez PJ, Morris G, Maberry M, Zeray F, et al.. (2002) Congenital syphilis after maternal treatment for syphilis during pregnancy. Am J Obstet Gynecol. United States. 569–573. [DOI] [PubMed]
- 52. Ramsey PS, Vaules MB, Vasdev GM, Andrews WW, Ramin KD (2003) Maternal and transplacental pharmacokinetics of azithromycin. Am J Obstet Gynecol 188: 714–718. [DOI] [PubMed] [Google Scholar]
- 53. Gichangi P, Renterghem LV, Karanja J, Bwayo J, Kiragu D, et al. (2004) Congenital syphilis in a Nairobi maternity hospital. East Afr Med J 81: 589–593. [PubMed] [Google Scholar]
- 54. Salakhov E, Tikhonova L, Southwick K, Shakarishvili A, Ryan C, et al. (2004) Congenital syphilis in Russia: the value of counting epidemiologic cases and clinical cases. Sex Transm Dis 31: 127–132. [DOI] [PubMed] [Google Scholar]
- 55. Yakubovsky A, Sokolovsky E, Miller WC, Sparling PF, Ryder RW, et al. (2006) Syphilis management in St. Petersburg, Russia: 1995–2001. Sexually Transmitted Diseases 33: 244–249. [DOI] [PubMed] [Google Scholar]
- 56. O’Connor M, Kleinman S, Goff M (2008) Syphilis in pregnancy. J Midwifery Womens Health 53: e17–21. [DOI] [PubMed] [Google Scholar]
- 57. Sia VM, Romero C, Sia DC, Pou J, Rajegowda BK (2011) Epidemiology of congenital syphilis in a South Bronx population: a follow-up study. J Perinat Med 39: 71–75. [DOI] [PubMed] [Google Scholar]
- 58. Ingraham NR (1950) The value of penicillin alone in the prevention and treatment of congenital syphilis. Acta Derm Venereol Suppl (Stockh) 31: 60–87. [PubMed] [Google Scholar]
- 59. Wammock V (1950) Penicillin therapy of the syphilitic pregnant woman: its practical application to a large urban obstetrical service. American Journal of Obstetrics & Gynecology 59: 806–817. [Google Scholar]
- 60. Guinness LF, Sibandze S, McGrath E, Cornelis AL (1988) Influence of antenatal screening on perinatal mortality caused by syphilis in Swaziland. Genitourin Med 64: 294–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Hira SK, Bhat GJ, Chikamata DM, Nkowane B, Tembo G, et al. (1990) Syphilis intervention in pregnancy: Zambian demonstration project. Genitourinary Medicine 66: 159–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Shafer JK, Smith CA (1954) Treatment of early infectious syphilis with N,N’-dibenzylethylenediamine dipenicillin G; a second report. Bull World Health Organ 10: 619–626. [PMC free article] [PubMed] [Google Scholar]
- 63.Willcox RR (1955) The treatment of primary and Secondary syphilis. Postgrad Med J 31: 548–551, 557. [DOI] [PMC free article] [PubMed]
- 64. Willcox RR (1954) A WHO study of treatment schedules for early syphilis in use throughout the world. Bull World Health Organ 10: 579–617. [PMC free article] [PubMed] [Google Scholar]
- 65. Rotchford K, Lombard C, Zuma K, Wilkinson D (2000) Impact on perinatal mortality of missed opportunities to treat maternal syphilis in rural South Africa: Baseline results from a clinic randomized controlled trial. Tropical Medicine and International Health 5: 800–804. [DOI] [PubMed] [Google Scholar]
- 66. Lumbiganon P, Piaggio G, Villar J, Pinol A, Bakketeig L, et al. (2002) The epidemiology of syphilis in pregnancy. Int J STD AIDS 13: 486–494. [DOI] [PubMed] [Google Scholar]
- 67. Donders GG, Desmyter J, Hooft P, Dewet GH (1997) Apparent failure of one injection of benzathine penicillin G for syphilis during pregnancy in human immunodeficiency virus-seronegative African women. Sex Transm Dis 24: 94–101. [DOI] [PubMed] [Google Scholar]
- 68. Wilkinson D, Sach M, Connolly C (1997) Epidemiology of syphilis in pregnancy in rural South Africa: opportunities for control. Trop Med Int Health 2: 57–62. [DOI] [PubMed] [Google Scholar]
- 69.Alexander JM, Sheffield JS, Sanchez PJ, Mayfield J, Wendel GD Jr (1999) Efficacy of treatment for syphilis in pregnancy. Obstet Gynecol. United States. 5–8. [DOI] [PubMed]
- 70. Temmerman M, Gichangi P, Fonck K, Apers L, Claeys P, et al. (2000) Effect of a syphilis control programme on pregnancy outcome in Nairobi, Kenya. Sex Transm Infect 76: 117–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Watson-Jones D, Gumodoka B, Weiss H, Changalucha J, Todd J, et al.. (2002) Syphilis in pregnancy in Tanzania. II. The effectiveness of antenatal syphilis screening and single-dose benzathine penicillin treatment for the prevention of adverse pregnancy outcomes. J Infect Dis. United States. 948–957. [DOI] [PubMed]
- 72.Myer L, Abdool Karim SS, Lombard C, Wilkinson D (2004) Treatment of maternal syphilis in rural South Africa: effect of multiple doses of benzathine penicillin on pregnancy loss. Trop Med Int Health. England. 1216–1221. [DOI] [PubMed]
- 73.Mullick S, Beksinksa M, Msomi S (2005) Treatment for syphilis in antenatal care: compliance with the three dose standard treatment regimen. Sex Transm Infect. England. 220–222. [DOI] [PMC free article] [PubMed]
- 74. Cheng JQ, Zhou H, Hong FC, Zhang D, Zhang YJ, et al. (2007) Syphilis screening and intervention in 500 000 pregnant women in Shenzhen, the People’s Republic of China. Sexually Transmitted Infections 83: 347–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Terris-Prestholt F, Watson-Jones D, Mugeye K, Kumaranayake L, Ndeki L, et al. (2003) Is antenatal syphilis screening still cost effective in sub-Saharan Africa. Sex Transm Infect 79: 375–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Tikhonova L, Salakhov E, Southwick K, Shakarishvili A, Ryan C, et al. (2003) Congenital syphilis in the Russian Federation: magnitude, determinants, and consequences. Sex Transm Infect 79: 106–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Sangtawesin V, Lertsutthiwong W, Kanjanapattanakul W, Khorana M, Horpaopan S (2005) Outcome of maternal syphilis at Rajavithi Hospital on offsprings. J Med Assoc Thai 88: 1519–1525. [PubMed] [Google Scholar]
- 78. McClean H, Daniels D, Carne C, Bunting P, Miller R (2006) UK National Audit of Early Syphilis Management. Case notes audit: diagnosis and treatment. Int J STD AIDS 17: 334–339. [DOI] [PubMed] [Google Scholar]
- 79. Garcia SG, Tinajeros F, Revollo R, Yam EA, Richmond K, et al. (2007) Demonstrating public health at work: a demonstration project of congenital syphilis prevention efforts in Bolivia. Sex Transm Dis 34: S37–41. [DOI] [PubMed] [Google Scholar]
- 80. Potter D, Goldenberg RL, Chao A, Sinkala M, Degroot A, et al. (2008) Do targeted HIV programs improve overall care for pregnant women?: Antenatal syphilis management in Zambia before and after implementation of prevention of mother-to-child HIV transmission programs. J Acquir Immune Defic Syndr 47: 79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Munkhuu B, Liabsuetrakul T, Chongsuvivatwong V, McNeil E, Janchiv R (2009) One-stop service for antenatal syphilis screening and prevention of congenital syphilis in Ulaanbaatar, Mongolia: a cluster randomized trial. Sex Transm Dis 36: 714–720. [DOI] [PubMed] [Google Scholar]
- 82. Hong FC, Liu JB, Feng TJ, Liu XL, Pan P, et al. (2010) Congenital syphilis: an economic evaluation of a prevention program in China. Sex Transm Dis 37: 26–31. [DOI] [PubMed] [Google Scholar]
- 83. Zhu L, Qin M, Du L, Xie RH, Wong T, et al. (2010) Maternal and congenital syphilis in Shanghai, China, 2002 to 2006. International Journal of Infectious Diseases 14: e45–e48. [DOI] [PubMed] [Google Scholar]
- 84. Caddy SC, Lee BE, Sutherland K, Robinson JL, Plitt SS, et al. (2011) Pregnancy and neonatal outcomes of women with reactive syphilis serology in Alberta, 2002 to 2006. J Obstet Gynaecol Can 33: 453–459. [DOI] [PubMed] [Google Scholar]
- 85. Brown WJ (1960) An evaluation of the incidence of reactions to penicillin. Br J Vener Dis 36: 30–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Gjessing HC (1960) [Penicillin consumption in Norway. Venereal disease-penicillin consumption-complications]. Tidsskr Nor Laegeforen 80: 977–980. [PubMed] [Google Scholar]
- 87. Shafer J (1954) Are people allergic to penicillin? The Journal of Social Hygiene 40: 69–71. [Google Scholar]
- 88. Smith CA, Kamp M, Olansky S, Price EV (1956) Benzathine penicillin G in the: treatment of syphilis. Bull World Health Organ 15: 1087–1096. [PMC free article] [PubMed] [Google Scholar]
- 89. Willcox RR, Fryers GR (1957) Sensitivity to repository penicillins. Br J Vener Dis 33: 209–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Hsu I (1958) Untoward reactions to benzathine penicillin G in a study of rheumatic-fever prophylaxis in adults. N Engl J Med 259: 581–583. [DOI] [PubMed] [Google Scholar]
- 91. Phaosavasdi S, Snidvongs W, Thasanapradit P, Ungthavorn P, Bhongsvej S, et al. (1989) Effectiveness of benzathine penicillin regimen in the treatment of syphilis in pregnancy. J Med Assoc Thai 72: 101–108. [PubMed] [Google Scholar]
- 92. International Rheumatic Fever Study Group (1991) Allergic reactions to long-term benzathine penicillin prophylaxis for rheumatic fever. The Lancet 337: 1308–1310. [PubMed] [Google Scholar]
- 93. Jenniskens F, Obwaka E, Kirisuah S, Moses S, Yusufali FM, et al. (1995) Syphilis control in pregnancy: decentralization of screening facilities to primary care level, a demonstration project in Nairobi, Kenya. Int J Gynaecol Obstet 48 Suppl: S121–128 [DOI] [PubMed] [Google Scholar]
- 94. Napoli D, Neeno T (2000) Anaphylaxis to Benzathine Penicillin G. Pediatric Asthma, Allergy & Immunology. 14: 329–332. [Google Scholar]
- 95. Apter AJ, Kinman JL, Bilker WB, Herlim M, Margolis DJ, et al. (2004) Represcription of penicillin after allergic-like events. J Allergy Clin Immunol 113: 764–770. [DOI] [PubMed] [Google Scholar]
- 96. Watson-Jones D, Oliff M, Terris-Prestholt F, Changalucha J, Gumodoka B, et al. (2005) Antenatal syphilis screening in sub-Saharan Africa: Lessons learned from Tanzania. Tropical Medicine and International Health 10: 934–943. [DOI] [PubMed] [Google Scholar]
- 97. Bronzan RN, Mwesigwa-Kayongo DC, Narkunas D, Schmid GP, Neilsen GA, et al. (2007) Onsite rapid antenatal syphilis screening with an immunochromatographic strip improves case detection and treatment in rural South African clinics. Sexually Transmitted Diseases 34: S55–S60. [DOI] [PubMed] [Google Scholar]
- 98.Carles G, Lochet S, Youssef M, El Guindi W, Helou G, et al.. (2008) [Syphilis and pregnancy]. J Gynecol Obstet Biol Reprod (Paris). France. 353–357. [DOI] [PubMed]
- 99.Li J, Wang LN, Zheng HY (2012) Jarisch-Herxheimer reaction among syphilis patients in China. J Eur Acad Dermatol Venereol. [DOI] [PubMed]
- 100.Liu XS (2011) Implications of statistical power for confidence intervals. Br J Math Stat Psychol. [DOI] [PubMed]
- 101. Macy E, Ho NJ (2012) Multiple drug intolerance syndrome: prevalence, clinical characteristics, and management. Ann Allergy Asthma Immunol 108: 88–93. [DOI] [PubMed] [Google Scholar]
- 102. Friedrich JO, Adhikari NK, Beyene J (2007) Inclusion of zero total event trials in meta-analyses maintains analytic consistency and incorporates all available data. BMC Med Res Methodol 7: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Perlis RH, Iosifescu DV, Castro VM, Murphy SN, Gainer VS, et al. (2012) Using electronic medical records to enable large-scale studies in psychiatry: treatment resistant depression as a model. Psychol Med 42: 41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Aickin M (2011) Patient-centered research from electronic medical records. Perm J 15: 89–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Miguel A, Azevedo LF, Lopes F, Freitas A, Pereira AC (2012) Methodologies for the detection of adverse drug reactions: comparison of hospital databases, chart review and spontaneous reporting. Pharmacoepidemiol Drug Saf. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy for MEDLINE (via PubMed).
(DOCX)