Abstract
Cerebral folate deficiency (CFD) syndrome is a neurodevelopmental disorder typically caused by folate receptor autoantibodies (FRAs) that interfere with folate transport across the blood–brain barrier. Autism spectrum disorders (ASDs) and improvements in ASD symptoms with leucovorin (folinic acid) treatment have been reported in some children with CFD. In children with ASD, the prevalence of FRAs and the response to leucovorin in FRA-positive children has not been systematically investigated. In this study, serum FRA concentrations were measured in 93 children with ASD and a high prevalence (75.3%) of FRAs was found. In 16 children, the concentration of blocking FRA significantly correlated with cerebrospinal fluid 5-methyltetrahydrofolate concentrations, which were below the normative mean in every case. Children with FRAs were treated with oral leucovorin calcium (2 mg kg−1 per day; maximum 50 mg per day). Treatment response was measured and compared with a wait-list control group. Compared with controls, significantly higher improvement ratings were observed in treated children over a mean period of 4 months in verbal communication, receptive and expressive language, attention and stereotypical behavior. Approximately one-third of treated children demonstrated moderate to much improvement. The incidence of adverse effects was low. This study suggests that FRAs may be important in ASD and that FRA-positive children with ASD may benefit from leucovorin calcium treatment. Given these results, empirical treatment with leucovorin calcium may be a reasonable and non-invasive approach in FRA-positive children with ASD. Additional studies of folate receptor autoimmunity and leucovorin calcium treatment in children with ASD are warranted.
Keywords: autism spectrum disorders, cerebral folate deficiency, folate receptor autoantibody, folinic acid, leucovorin calcium
Introduction
Cerebral folate deficiency (CFD) syndrome is a recently described neurometabolic disorder characterized by low concentrations of 5-methyltetrahydrofolate (5MTHF) in the cerebrospinal fluid (CSF), despite normal systemic folate levels. CFD is believed to be caused by the impaired transport of folates across the blood–brain barrier. The first reported cases of CFD manifested severe neurodevelopmental symptoms including spastic paraplegia, cerebellar ataxia, dyskinesia, seizures, acquired microcephaly and developmental regression, which occurred as early as 4 months of age.1, 2 Central visual disturbances (optic atrophy and blindness) and hearing loss occurred after age 3 and 6 years, respectively, in some cases.2
Since its original description, the phenotype of CFD has been expanded. Six studies have reported autism spectrum disorder (ASD) in a subset of children with CFD.2, 3, 4, 5, 6, 7 Most of these children with ASD were low functioning and had significant neurological abnormalities.4, 6 Although the biological mechanisms linking CFD to ASD are not known, deficits in folate within the central nervous system (CNS) could explain several findings documented in ASD. For example, deficits in folate one-carbon metabolism have been shown to promote methylation deficits and oxidative stress in some children with ASD,8, 9, 10 as well as alter DNA methylation in the brain of an animal model.11 Examination of some postmortem ASD brains has verified alterations in DNA methylation in the frontal cortex12 and increased oxidative stress in several cortical regions, including those associated with speech processing and emotional and social behavior.13 Ramaekers et al.14 suggested that expression of normally silenced genes could be caused by either alterations in the methyl CpG-binding protein 2 gene, as occurs in Rett's syndrome or alterations in DNA methylation resulting from CFD, thus explaining the similarity between the clinical symptoms of the original description of CFD and Rett's syndrome. Moreover, as chronic oxidative stress can result in mitochondrial dysfunction,15 the increased oxidative stress noted in postmortem ASD brain samples13 could account for the mitochondrial dysfunction observed in similar cortical regions in postmortem ASD brain samples.16 As folate is essential for production of purines and pyrimidines, the nucleotide precursors of RNA and DNA, low folate levels can result in abnormalities in cellular proliferation, as well as transcription and translation, and therefore contribute to DNA instability17 and chromosome breakage.18 Finally, animal models demonstrate that the folate receptor protein alpha (FRα) is important in the repair and regeneration of the CNS after injury.19
Methylfolate is transported across the blood–brain barrier by FRα, which has a high affinity for both folic acid and 5MTHF and is located on both sides of the epithelial surface of the choroid plexus.20 FRα is part of an ATP-dependent receptor-mediated system that transports folate derivatives across the blood–brain barrier through an endocytosis mechanism. FRα is essential for folate transport across the blood–brain barrier when extracellular folate concentrations are low.20 FRα is also located on thyroid cells,6 the microvillus plasma membrane of the placenta,21 as well as in the epithelium of the fallopian tubes, uterus and epididymis, acinar cells of the breast, submandibular salivary and bronchial glands and the alveolar lining including pneumocytes.22 Around 2005, autoantibodies were described that bind to the FRα, greatly impairing its function.6 FRα autoantibodies (FRAs) have been linked to CFD in cases with4 and without6 ASD and also in gestations with neural tube defects23 and subfertile women.24 In a 2007 case report, mitochondrial complex I deficiency was linked to CFD in a FRA-negative child,25 and in 2008, a wider array of mitochondrial diseases was associated with CFD.26
Folate can also be transported across cellular membranes using the folate receptor-β,27 the reduced folate carrier (RFC)28 and the proton-coupled folate transporter.29 Although folate receptor-β seems important in the placental transport of folate,27 the proton-coupled folate transporter is critical in folate transport in the gastrointestinal tract especially as impairment of this transporter function is responsible for hereditary folate malabsorption.29 The RFC is a transmembrane protein that is expressed in a wide range of tissues, including the placenta, kidney, intestine and both the basolateral and apical surfaces of the choroid plexus.30 Unlike the folate transport involving FRα, the RFC allows bidirectional transport of folate across the cellular membrane.30 The RFC is responsible for folate transport across the blood–brain barrier when extracellular folate concentrations are high20 and has a higher affinity for reduced forms of folate such as 5MTHF and folinic acid (leucovorin) as compared with folic acid.28 As leucovorin can enter the CNS through the RFC, it can normalize CSF 5MTHF levels in individuals with CFD.6 In some cases, clinical response is dramatic, especially if treatment is started early in life.1, 31 In children with concomitant ASD and CFD, treatment with oral leucovorin (0.5 to 2 mg kg−1 per day) has resulted in improvements ranging from partial improvements in communication, social interaction, attention and stereotypical behavior3, 5, 6, 7 to complete recovery of both neurological and ASD symptoms.4, 6
The aforementioned reports provide a compelling reason to study the FRA and CFD in more depth in children with ASD. However, a systematic study of FRA or CFD prevalence in children with ASD has not been performed. Unfortunately, the diagnosis of CFD requires a lumbar puncture (LP), a rather invasive procedure, to measure CSF 5MTHF levels. However, FRA concentrations can be measured using a blood test, thereby providing a minimally invasive method for identifying children who might be at increased risk for CFD. Starting in 2010, two of the authors (REF and DAR) offered FRA testing to patients evaluated in their clinics. Parents of children who were FRA positive were offered two treatment options for their children: either a diagnostic LP to measure the CSF 5MTHF level or an empirical treatment with oral leucovorin if they did not wish their child to undergo an invasive procedure. Response to oral leucovorin treatment in the child was rated by parents using a standardized scale. Surprisingly, FRA prevalence was very high in children with ASD, and the response to leucovorin in children was rated by parents as favorable on several cognitive dimensions.
Materials and methods
Two of the authors (REF and DAR) offered FRA testing as part of the workup for medical conditions associated with ASD. Approximately 1 ml serum was collected and sent to the laboratory of Dr Edward Quadros, PhD, at the State University of New York, Downstate (Brooklyn, NY, USA). The assay for both the blocking and the binding FRA concentrations has been described previously.6, 23 FRA concentrations were categorized as negative, low, medium or high (blocking autoantibody: negative <0.2, low 0.2–0.5, medium 0.5–1.0, high >1.0, expressed as pmol of folic acid blocked per ml of serum from binding to FRα binding autoantibody: negative <0.5, low 0.5–2, medium 2–10, high >10, expressed as pmol of IgG antibody per ml of serum).
In all, 93 children with ASD who had FRA testing were included in this study. All children met the Diagnostic and Statistical Manual of Mental Disorders—Fourth Edition—Text Revision32 criteria for ASD and had previously been diagnosed by a developmental pediatrician, pediatric neurologist or clinical psychologist with ASD. Review of each child's medical record was obtained through an Institutional Review Board-approved protocol. Patient characteristics and history, including family history, were abstracted from the medical record. Patients with mitochondrial disease were diagnosed using standard criteria.33, 34 We also examined laboratory tests of autoimmunity, including other autoantibodies. As milk-free diets have been shown to reduce FRA titers5 and many children with ASD are treated empirically with diets that are milk-free (for example, gluten-free and casein-free diet), we asked families whether they had tried various diets commonly used to treat ASD and, if possible, to provide an evaluation of whether such interventions had an effect on their child's development. Similarly, we also asked parents whether their child was treated with intravenous immunoglobulin or steroids, two immunomodulatory treatments not uncommonly used to treat ASD, and, if possible, to provide an evaluation of whether such interventions had an effect on their child's development.
Cerebrospinal fluid was obtained through an LP under general sedation and fluoroscopy guidance for 16 children. CSF was collected with standardized reagent tubes, frozen at −80 °C and examined for 5MTHF and neurotransmitter metabolites (Medical Neurogenetics, Atlanta, GA, USA). In all cases, CSF demonstrated a normal number of white and red blood cells, protein, glucose and amino acids.
In all, 44 children (age mean=6 years 10 months; s.d.=2 years 8 months; range 2 years 11 months to 15 years 0 months) of the 70 FRA-positive (either blocking or binding autoantibody or both) children were treated with 2 mg kg−1 per day of leucovorin calcium tablets in two divided doses (maximum 50 mg daily). The dose was escalated over a 2-week period with half of the final dose administered during the first 2 weeks. After at least 1 month of treatment (mean treatment time was 4.0 months; s.d.=2.6 m) treatment response and adverse events (AEs) were assessed during a phone call or follow-up visit. No other significant changes in treatment were made during the follow-up period. Parents were asked to rate response to treatment using a modified Clinical Global Impression Scale—Improvement subscale. This scale gives an impression of changes compared with baseline.35 Parents were asked to rate changes in cognition and behavior on nine dimensions: verbal communication, receptive language, expressive language, non-verbal communication, stereotypical behavior, hyperactivity, mood, attention and aggression. Verbal communication was considered the primary outcome variable as communication was one of the significant improvements noted in previous reports with leucovorin treatment in children with ASD and CFD3, 5, 6, 7 and can be assessed more objectively (that is, number of words spoken and sentence complexity) than other cognitive and behavioral measures. Other ratings were considered secondary outcomes. Three children discontinued treatment within 2 weeks of starting treatment and one stopped treatment after 6 weeks because of an AE. The three children who stopped treatment within 2 weeks were not treated for a sufficient amount of time to judge any cognitive-behavior changes and, thus, response ratings were not performed on them.
The 26 FRA-positive children not treated were either awaiting FRA or LP results (wait group) from which a control group was derived.36 Parents of FRA-positive children in the wait group that had not made any treatment changes since the blood draw for the FRA were asked to rate changes in their child's behavior since the blood draw. These data were collected at the time when parents were notified of test results (nine children met this criteria; age mean=6 years 11 months, s.d.=2 years 8 months). The mean time between blood draw and rating was 3.1 m (s.d.=1.3 m) for controls, which was not significantly different than the time between starting leucovorin calcium and parental ratings in the treatment group (t=1.57, P>0.10).
For children who were positive for at least one FRA, parents were offered FRA testing for themselves and for the patient's siblings. In all, 27 parents and 6 siblings underwent FRA testing.
Statistical analysis
For statistical tests in which both variables were continuous (that is, age and autoantibody concentration), parametric statistics were used (that is, Pearson's r for correlations, t-test for group differences and generalized linear model for regression). Here, χ2 was used for tabular data. To determine whether parental ratings demonstrated greater improvement in the treatment group than in the control group, one-tailed Mann–Whitney U-nonparametric tests were used. The one-tailed test was used as we hypothesized that an improvement, not a decrement, in cognitive-behavioral function would occur with treatment. Parametric t-tests were also computed for comparison. Regression analysis was performed on the ratings that demonstrated differences between treatment groups to determine whether these ratings were related to age and/or FRA concentrations. Parental ratings were modeled as a multinomial distribution in the regression. Regression was performed using the procedure glimmix in SAS (Version 4.2, SAS Institute, Cary, NC, USA). In general, α was set at 0.05 for most statistical tests. For the tabular data, α was set at 0.01 to be conservative as multiple characteristics were compared. For comparisons between treatment and control groups, a power analysis was conducted on the primary outcome variable (that is, verbal communication) using G*Power 3 (Universität Kiel, Kiel, Germany).37 The optimal α for the one-tailed Mann–Whitney U-test was 0.05. This resulted in an 80% power. In comparison, an α of 0.01 would result in a power of only 55%.
Results
Subject characteristics
FRAs were analyzed in 84 male and 9 female children with ASD (mean age=7 years 3 months, s.d.=3 years 1 month; range=2 years 11 months–17 years 5 months). The sample was 82% non-Hispanic White, 12% Hispanic, 4% Asian and 2% African American. Table 1 lists additional characteristics.
Table 1. Patient characteristics.
| Autoantibody negative (n=23) | Autoantibody positive (n=70) | |
|---|---|---|
| Age | 8 years 4 months | 6 years 8 months* |
| Male % | 96 | 89 |
| Family history | ||
| Multiple mischarges | 20% | 7% |
| Neural tube defects | 0% | 1% |
| Prematurity | 15% | 3% |
| ADHD | 25% | 28% |
| ASD | 10% | 24% |
| Learning disabilities | 40% | 33% |
| Anemia | 20% | 6% |
| Autoimmune disease | 60% | 24%** |
| Neurological disorder | 30% | 40% |
| Psychiatric disorder | 35% | 46% |
| Spectrum diagnosis | ||
| PDD-NOS | 43% | 34% |
| Autistic disorder | 52% | 64% |
| Asperger | 4% | 1% |
| Developmental profile | ||
| Early delay | 57% | 64% |
| Regression | 57% | 49% |
| Stagnation | 22% | 9% |
| Late symptoms | 9% | 13% |
| Regression type | ||
| Abrupt | 62% | 65% |
| Very slow | 38% | 18% |
| Gradual | 0% | 17% |
| Medical diagnosis | ||
| Prematurity | 13% | 9% |
| Cerebral palsy | 0% | 0% |
| Sensory integration disorder | 22% | 20% |
| Hypothyroidism | 11% | 37% |
| ADHD | 22% | 17% |
| Mitochondrial disease | 43% | 31% |
| Genetic disorder | 0% | 4% |
| Growth disorders | ||
| Failure to thrive | 9% | 10% |
| Accelerated growth | 0% | 4% |
| Microcephaly | 0% | 1% |
| Macrocephaly | 9% | 4% |
| Neurological disorders | ||
| Epilepsy | 39% | 30% |
| Ataxia | 4% | 6% |
| Hypotonia | 30% | 41% |
| Hypertonia | 5% | 2% |
| Nystagmus | 9% | 1% |
| Hearing loss | 0% | 4% |
| Visual loss | 4% | 1% |
| Gastrointestinal disorders | ||
| Diarrhea | 35% | 41% |
| Constipation | 39% | 36% |
| Gastroesophageal reflux | 13% | 14% |
| Inflammation | 39% | 23% |
| Dysbiosis | 30% | 29% |
| Lymphoid nodular hyperplasia | 4% | 3% |
| Sleep disorders | ||
| Insomnia | 39% | 23% |
| Poor sleep maintenance | 43% | 41% |
| Apnea | 4% | 3% |
| Periodic leg movement during sleep | 0% | 3% |
| Diagnostic tests | ||
| Electroencephalogram | ||
| Normal | 53% | 75% |
| Epileptiform | 35% | 20% |
| Slowing | 12% | 5% |
| Abnormal magnetic resonance imaging | 27% | 13% |
| Response to treatments | ||
| GFCF diet (n=30) | 88% | 86% |
| Milk-free diet (n=25) | 80% | 85% |
| Specific carbohydrate diet (n=13) | 67% | 40% |
| IVIG (n=16) | 100% | 93% |
| Steroids (n=12) | 67% | 89% |
| B12 injections (n=31) | 75% | 83% |
Abbreviation: ADHD, attention deficit hyperactivity disorder; ASD, autism spectrum disorder; GFCF, gluten free casein free; IVIG, intravenous immunoglobulin; PDD-NOS, pervasive developmental disorder-not otherwise specified.
*P<0.05.
**P<0.01.
Prevalence of FRAs
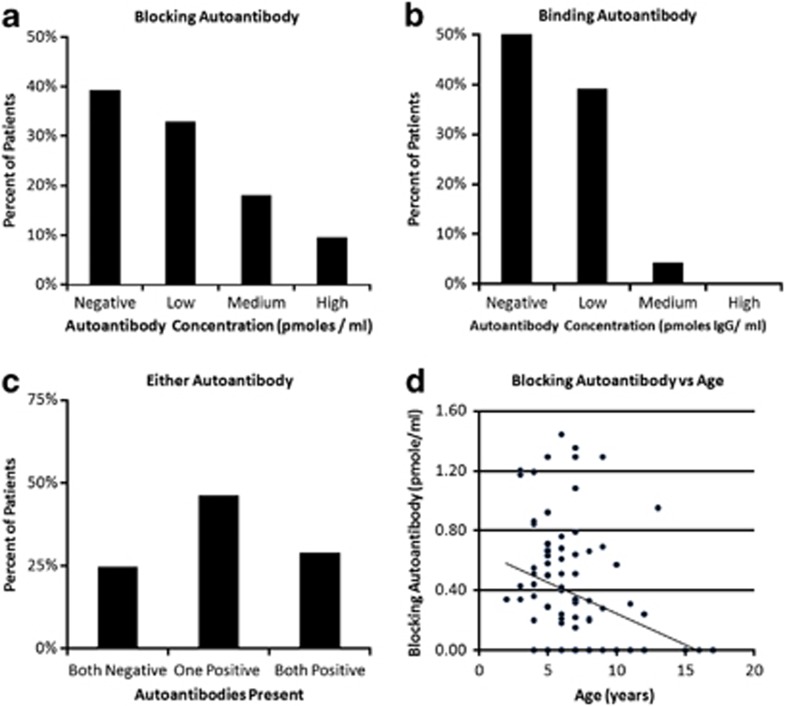
Overall, 56 of 93 (60%) children with ASD were positive for the blocking FRA and 41 of 93 (44%) were positive for the binding FRA. For children who were positive for the blocking FRA, a low, medium and high titer was found in 33%, 17% and 10% of the sample, respectively (Figure 1a). For children with the binding FRA, a low, medium and high titer was found in 40%, 4% and 0% of the sample, respectively (Figure 1b). Overall, 27 of 93 (29%) children were positive for both FRAs, 43 of 93 (46%) were positive for only one FRA and 70 of 93 (75.3%) were positive for at least one FRA (Figure 1c). Age was negatively correlated with the blocking (r=−0.32, P=0.003, see Figure 1d) but not with the binding (r=−0.12, P>0.10) FRA concentration.
Figure 1.
The prevalence of blocking and binding folate receptor autoantibodies in ASD. (a) The prevalence of children with ASD for negative, low, medium and high titers of the folate receptor-blocking autoantibody. (b) The prevalence of children with ASD for negative, low, medium and high titers of the folate receptor-binding autoantibody. (c) The prevalence of being negative for both the binding and the blocking autoantibodies, being positive for only the blocking or the binding autoantibody and being positive for both the binding and the blocking autoantibodies. (d) The blocking folate receptor autoantibody titer was found to significantly decrease with age. ASD, autism spectrum disorder.
Of the 27 parents who underwent FRA testing, 10 (37%) were found to be low positive for the blocking FRA, 2 (7%) were low positive for the binding FRA and none were positive for both FRA. Of the six siblings without ASD who underwent FRA testing, 1 (17%) was low positive for the blocking FRA, 1 (17%) was low positive for the binding FRA and none were positive for both FRA.
Characteristics of children with FRAs
One child had a metabolic disorder that was not a mitochondrial disease (CNS B6 deficiency) and three children demonstrated genetic abnormalities (deletions of 14q32.33, 15q13.1–3 and 8q; Table 1). Concurrent prescription medications are listed in Supplementary Table S1.
The characteristics of children who were FRA negative were compared with those of children positive for at least one FRA (Table 1). Children who were FRA negative were slightly, but significantly, older than those who were positive for at least one FRA (t-test=2.30, P=0.02). Significantly more children who were FRA negative had a family history of autoimmune disease compared with those with at least one FRA. Neither the distributions of autism spectrum diagnoses, type of regression and developmental profiles nor the specific medical diagnoses were significantly different across the groups. Although the incidence of hypothyroidism was higher in the FRA-positive group (37%) than in the FRA-negative group (11%), this difference was not statistically significant. FRA-positive and FRA-negative groups had a similar prevalence of gastrointestinal disorders. The percentage of children with normal, epileptiform or slow electroencephalograms was also not different across groups. Both groups had a similar response to various dietary and immunomodulatory treatments. There was no significant difference in any autoantibodies or markers of autoimmune disease between children who were FRA positive compared with FRA-negative children (Table 2). The one elevated erythrocyte sedimentation rate was minimal (12) and the two elevated antinuclear antibody titers were minimal (1:160), and a rheumatology consult on these children did not indicate that further evaluation for an autoimmune disorder was indicated.
Table 2. Autoimmune markers and other autoantibodies.
| Folate receptor autoantibody |
Negative |
Positive |
||
|---|---|---|---|---|
| Positive | Negative | Positive | Negative | |
| Autoantibodies to brain endothelial cells | 5 | 2 | 10 | 11 |
| Anti-Hu, anti-CV2, anti-Yo, anti-Ri, anti-CAR, anti-Ma, anti-Ta, anti-Zic4, voltage-gated calcium channels, P/Q-type and voltage-gated potassium channels, ganglionic nicotinic acetylcholine receptor, NR1 N-methyl D-aspartate receptor, glutamic acid decarboxylase | 0 | 2 | 0 | 7 |
| Thyroid autoantibodies | 1 | 0 | 1 | 4 |
| Anti-DNase-B and/or antistreptolysin O antibodies | 1 | 1 | 3 | 3 |
| Erythrocyte sedimentation rate | 0 | 0 | 1 | 5 |
| Antinuclear antibodies | 0 | 0 | 2 | 2 |
CSF studies
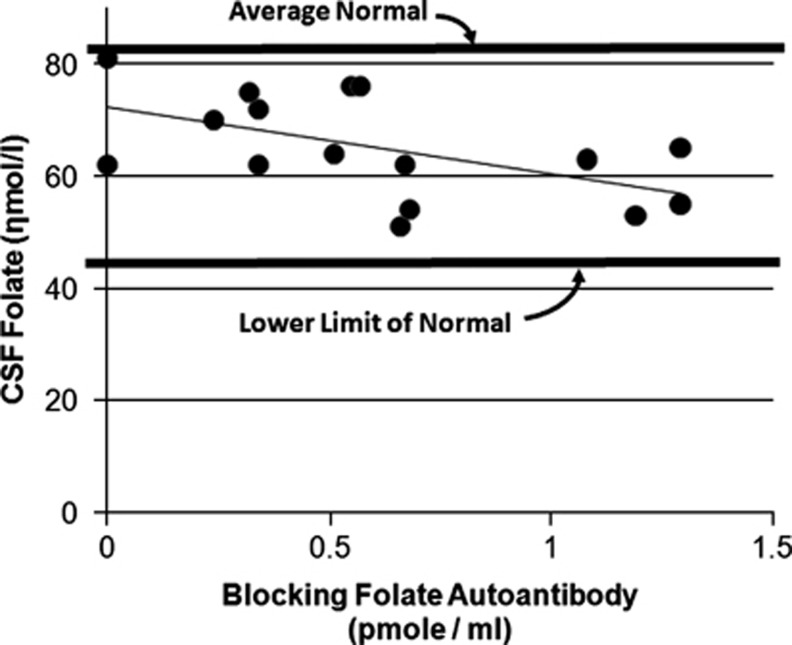
No significant difference in mean binding or blocking FRA titers or improvement ratings for any cognitive-behavioral subscale was observed between children who underwent an LP compared with those who did not. Regression analysis included variables of age and blocking and binding FRA concentrations. We included a curvilinear term for FRA concentrations in the regression.5 The regression analysis demonstrated a significant linear relationship between CSF 5MTHF and the blocking, but not the binding, FRA concentration (F(1,14)=5.78, P=0.03). The CSF 5MTHF concentration was predicted to be 72.3 nmol l−1 when no blocking FRA was present (that is, the Y-axis intercept) with an 11.9 nmol l−1 decrease in 5MTHF concentration for each 1 pmol ml−1 increase in blocking FRA (Figure 2). Notably, all 16 CSF 5MTHF values were below the normative mean CSF concentration. The probability of this occurring randomly (assuming a binomial distribution with half above and half below the mean) is 0.00001. There was no significant relationship between CSF 5MTHF or FRA concentrations and CSF neurotransmitter concentrations. Neurotransmitter concentrations were normal in all cases.
Figure 2.
The relationship between cerebrospinal fluid 5-methyltetrahydrofolate concentrations and blocking folate receptor autoantibody titers. Lower cerebrospinal fluid 5-methyltetrahydrofolate concentrations are associated with higher blocking folate receptor autoantibody titers.
Treatment with leucovorin
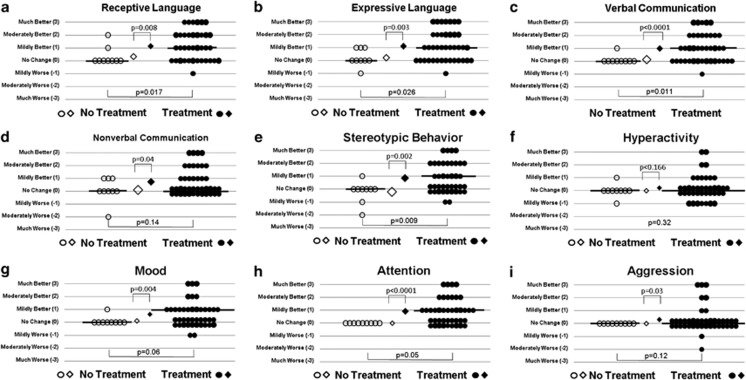
For each response measure, Figure 3 (a-i) depicts the individual ratings for both treated (filled circles) and control (unfilled circles) participants along with the medians (thick horizontal lines) and means (diamonds) for both groups. The P-value for the Mann–Whitney U-test are at the bottom of each graph, whereas P-value for the t-test are at the top of each graph. Significantly higher improvement ratings were found for treated compared with untreated children on ratings of verbal communication (primary outcome), receptive and expressive language, attention and stereotypical behavior. These significant differences were confirmed using the t-test. The Mann–Whitney U-test did not find significant differences between groups for the ratings of non-verbal communication, mood, hyperactivity or aggression, although the t-test did demonstrate significantly higher improvement ratings for treated compared with untreated children on ratings of non-verbal communication, mood and aggression. For cognitive-behavioral dimensions associated with statistically significant improvements related to treatment, approximately two-thirds of treated children demonstrated some improvement and approximately one-third of children demonstrated moderate or much improvement (Supplementary Table S2, Supplementary Material).
Figure 3.
Improvement ratings for nine cognitive-behavioral dimensions for children treated with leucovorin calcium compared with the no-treatment group (a-i). Improvement is rated on a 7-point scale ranging from much worse (−3) to much better (+3). For each cognitive-behavioral dimension, we provide the score for each child treated with leucovorin on the right of each graph (filled circles), and the score for each control child who did not undergo treatment (unfilled circles). The median for each group is given by a thick line, and the mean for each group is provided by diamonds. The P-value for the Mann–Whitney U-test is provided at the middle bottom of each graph and the P-value for the t-test is provided at the middle top of each graph.
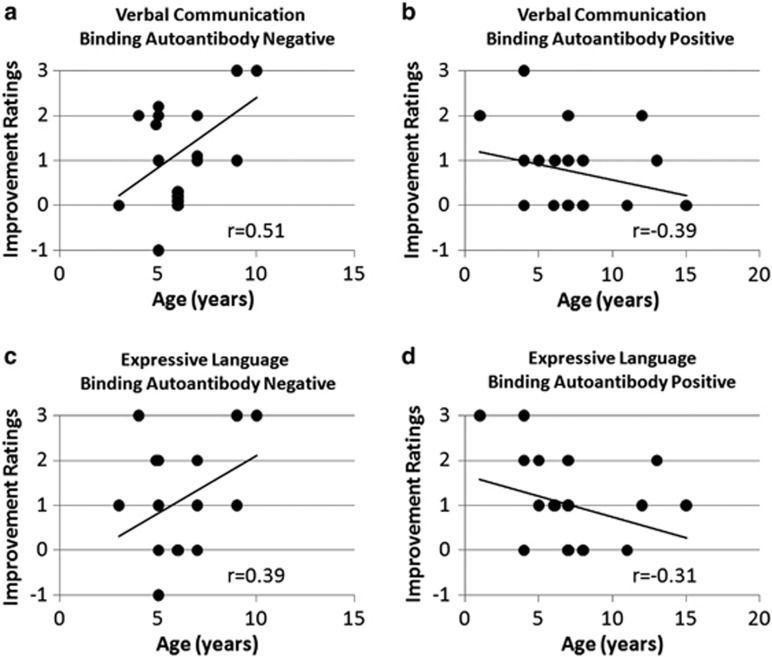
Linear regression demonstrated a significant relationship between age and improvement ratings for verbal communication and expressive language (F(1,31)=4.71, P=0.04 and F(1,31)=5.25, P=0.03, respectively) with this relationship moderated by the binding FRA concentration (binding: F(1,31)=4.92, P=0.03 and F(1,31)=6.06, P=0.02, respectively; age × binding: F(1,30)=7.21, P=0.01; F(1,31)=6.96, P=0.01, respectively). To examine the age effect in a straightforward manner, graphs of the relationship between age and ratings of improvement in verbal communication and expressive language are presented (see Figures 4a and c, respectively) for cases in which binding FRA was negative. These two graphs demonstrate that leucovorin calcium resulted in greater improvements in both verbal communication and expressive language in older children than in younger children. For children with a positive binding FRA, treatment with leucovorin calcium resulted in greater improvements in verbal communication and expressive language for children who were younger than for children who were older (see Figures 4b and d).
Figure 4.
The relationship between improvement ratings in verbal communication (a, b) and expressive language (c, d) and age for children with (b, d) and without (a, c) binding folate receptor autoantibody. (a, c) For children without the binding autoantibody, improvements in verbal communication and expressive language are higher for older children than for younger children. (b, d) For children with the binding autoantibody, improvements in verbal communication and expressive language are higher for younger children than for older children. Correlation coefficients are provided for the relationship between improvement and age for each graph; hence, the P-value for these correlations are not provided.
Adverse events were minimal for children treated for at least 1 month with leucovorin calcium (see Supplementary Table S3 and Supplementary Material). However, discontinuation of leucovorin was necessary in four children. After 6 weeks, insomnia and gastroesophageal reflux led to discontinuation of leucovorin calcium in one child. In addition, three boys, all of them concurrently taking risperidone, were not able to tolerate leucovorin calcium for even a short period of time. These boys developed worsening aggression (including self-injurious behavior in one) within 2 weeks of starting leucovorin calcium, resulting in immediate discontinuation, making worsening aggression the most common AE of leucovorin calcium treatment. Interestingly, aggressive behavior was the indication for risperidone, the medication that all three of these children had in common. Of the 40 children who tolerated the leucovorin calcium well, only one was concurrently receiving risperidone (see Supplementary Table S3 and Supplementary Material). Although some parents rated mood (5%), stereotypical behavior (5%) and hyperactivity (17%) as mildly worse on the Clinical Global Impression Scale in some children (Figure 3), they did not report these as AEs when specifically asked about AEs.
Discussion
This study is the first to examine FRA prevalence in children with ASD and to measure, in a controlled manner, the response to leucovorin calcium in FRA-positive children. We also reviewed the clinical characteristics of FRA-positive children and the correlation between FRA and CSF 5MTHF concentrations. Overall, this study demonstrates an unexpectedly high FRA prevalence and a favorable response to leucovorin calcium in FRA-positive children with ASD.
The prevalence of FRAs in ASD
Several studies have reported the presence of FRAs in children with ASD.2, 3, 4, 5, 6, 7 In these studies, children with ASD had both CFD and significant neurological abnormalities. In this case series, a high FRA prevalence was found in a group of children with ASD who did not have CFD or significant neurological abnormalities. The prevalence of blocking FRA (60%) was much higher than that reported in the control population of women, estimated to be 4–7.2% in Spain38, 39 and 9–13% in Ireland.23 To our knowledge, the prevalence of blocking FRA in the general US population has not been published, but has been estimated to be 10–15% by Dr Quadros' laboratory (unpublished data). The binding FRA prevalence of 44% in this case series is also higher than that reported in the general US population of 12%.23 Overall, our estimates suggest an elevated FRA prevalence in children with ASD; additional studies should be performed in ASD.
Characteristics of children with ASD and FRAs
We found few clinical differences between children who were FRA positive compared with those who were FRA negative. Thus, it seems to be difficult, at this point, to distinguish children with ASD who are FRA positive from those who are FRA negative. A family history of autoimmune disorders was higher in children who were FRA negative compared with those who were FRA positive. This does not support the idea that disorders associated with the FRA, such as CFD, are autoimmune disorders. In fact, the lack of any association between FRA-positive children and other autoimmune markers or autoantibodies points away from the FRA being associated with classical autoimmune disease. Given that a case of juvenile rheumatoid arthritis was associated with CFD,40 it is clear that classical autoimmune disorders can result in FRA elevations, but our data suggest that this may not be common.
The blocking FRA concentration was found to decrease with increasing age. The reason for this finding is not clear. As a milk-free diet has been reported to reduce blocking FRA concentrations,5 it is possible that some children may have self-restricted their milk intake as they became older. However, as most of the children in this series, irrespective of age, were maintained on milk-free diets, this is unlikely. It is also possible that this finding is associated with the underlying pathophysiology that produces FRAs. As the onset of ASD is early in life (around toddler age) with improvement in some in early childhood, it is possible that the peak of the pathophysiology that causes ASD (and potentially causes the FRA elevations) could be most active early in life and decrease with age.
Serum FRAs and CSF 5MTHF concentrations
In this study, we found an inverse relationship between the blocking FRA and CSF 5MTHF concentrations, confirming previous findings.5 Given that the normative mean CFD 5MTHF concentration is 82±31 nmol l−1 (range: 44–181 nmol l−1)5, even the highest CSF 5MTHF concentration in this study (81 nmol l−1 in a child with no blocking FRA) was below the reported mean in normal children.
The estimated mean CSF 5MTHF with no blocking FRA (72.3 nmol l−1) was well below the mean concentration reported for normal controls. Given that the CSF 5MTHF was estimated to be below normal, even in children without blocking FRAs, it is possible that children with ASD, in general, might have a lower than normal CSF 5MTHF concentration. This would be consistent with many studies that have reported folate-related abnormalities in children with ASD.9, 10, 41, 42, 43 More importantly, children with ASD may be predisposed to abnormalities in the transport of folates across the blood–brain barrier, irrespective of the presence of FRAs, as one study reported RFC genetic variants associated with ASD9 and mitochondrial disorders, the most common metabolic disorder in ASD,33 also may result in compromised FRα function.26 Given that children with ASD already have abnormalities with folate metabolism, it is likely that FRAs act synergistically with other abnormalities to reduce CSF 5MTHF concentration.
Treatment with leucovorin
Treatment with leucovorin calcium in FRA-positive children with ASD was well tolerated and beneficial for cognitive-behavioral functions, including verbal communication, receptive and expressive language, attention and stereotypical behavior. Approximately two-thirds of the treated children were perceived as obtaining some benefit and about one-third had a moderate or much improvement in these cognitive-behavioral dimensions (Supplementary Table S2). The mean length of treatment was 4 months. As some studies have reported that 1–3 years of treatment with leucovorin calcium is required in children with CFD to obtain maximal improvements,4, 25 it is possible that a longer treatment period would have resulted in additional benefits.
The level of binding FRA and age seemed to affect the degree of improvement for verbal communication and expressive language. It has been suggested that younger children are relatively more responsive to leucovorin calcium than older children,2 but our data indicate that this might depend on the binding FRA concentration. For children negative for the binding FRA, younger children improved less than older children. However, these findings should be interpreted with caution as it is very possible that the follow-up period was not long enough to provide the necessary time for optimal improvement.
As FRA concentrations were not significantly different between children who did and did not undergo an LP, and all children who had an LP had a CSF 5MTHF concentration below the normative mean, it is likely that many FRA-positive children in this study also had a below-average CSF 5MTHF concentration. Some investigators have reported significant clinical improvements with leucovorin calcium treatment in children with low normal CSF 5MTHF concentrations.44 As the presence of even a low-blocking FRA concentration may be associated with a low CSF 5MTHF concentration, a low-blocking FRA titer may be clinically significant in some children with ASD, consistent with previous suggestions.5 The findings of this study suggest that empirical treatment with leucovorin calcium without performing an LP may be a reasonable and non-invasive approach in FRA-positive children with ASD.
Leucovorin calcium was generally well-tolerated. The most common AE was worsening aggressive behavior, which may have been associated with concurrent treatment with risperidone. Although it is not clear why this side effect occurred, the rapid development of behavioral changes in these children suggests that it may have been due to an increase in CNS dopamine secondary to increased 5MTHF or tetrahydrobiopterin in the CNS, which then may have reduced the dopamine receptor-blocking effect of risperidone.45 Another possible cause of these behavioral changes may have been due to an inhibition of mitochondrial function by risperidone.46, 47 Animal models of mitochondrial dysfunction report similar aggressive behavior.48, 49 However, for children who tolerated leucovorin calcium for at least 1 month, there was no indication of increased aggression. Thus, for children not concurrently receiving anti-psychotic medications and without aggressive behavior, empirical treatment of leucovorin calcium may be a reasonable course of treatment in FRA-positive children with ASD.
Given that the RFC provides a pathway for leucovorin calcium to enter the CNS in children who have reduced transport of folate across the blood–brain barrier due to the FRA, we assume that the effect of leucovorin calcium is through an increase in 5MTHF in the CNS. This is supported by studies demonstrating an increase in CNS 5MTHF concentrations after the use of leucovorin.2, 4 However, the RFC is an important folate carrier in other tissues such as the kidney and intestine. As gastrointestinal symptoms have been associated with more aberrant behavior in children with ASD,50 improvements in gastrointestinal function could result in improved behavior. Improvements in kidney function could provide better filtration of toxic metabolites associated with metabolic conditions that have been associated with ASD, thereby improving general physiology. In addition, leucovorin has also been demonstrated to improve markers of oxidative stress in children with ASD.51 Thus, improvements noted as a result of leucovorin calcium in some children could be the result of an effect of leucovorin calcium on non-CNS organs.
FRAs and ASD
The high prevalence of FRAs in this study is consistent with the literature that documents elevations in various autoantibodies in both children with ASD and mothers of children with ASD.52, 53 Although various autoantibodies have been reported in children with ASD, the clinical significance of many of these autoantibodies has not been fully documented, leaving open the possibility that some autoantibodies may be an epiphenomenon of immune dysfunction.53 In this study, we have demonstrated that the serum-blocking FRA concentration can modulate the CSF 5MTHF concentration and that leucovorin calcium treatment results in cognitive-behavioral improvements. Thus, FRAs should be added to the list of autoantibodies that may have clinical significance in the cognitive-behavioral features of ASD, such as autoantibodies to GABAergic54 and cerebellar55 neurons in children with ASD and antibodies to fetal brain proteins in mothers of children with ASD.56
It is likely that FRAs are not the only culprit in children with ASD, which result in depressed CSF 5MTHF levels, but rather FRAs may work synergistically with other susceptibility factors, including factors that can depress systemic and central 5MTHF levels,9, 41, 42, 43, 57 as well as factors that reduce the transport of folates across the blood–brain barrier.9, 26, 33 For example, methylenetetrahydrofolate reductase gene variants reported in some children with ASD41 can be associated with the decreased production of 5MTHF. Interestingly, certain methylenetetrahydrofolate reductase genotypes have been reported to be associated with certain autistic behavior, including unusual body movements, hyperactivity and self-injurious behaviors.58 Furthermore, a genetic variant in the dihydrofolate reductase enzyme, which is involved in the process of producing 5MTHF43 and genetic variants in the RFC9 have been reported in some children with ASD and could contribute to impaired folate transport into the CNS. Finally, mitochondrial dysfunction, which has been associated with ASD,33 can contribute to reduced transport of folate across the blood–brain barrier. Gastrointestinal problems reported in some children with ASD could compound this problem. For example, abnormal levels of certain gut bacteria reported in some children with ASD, including Clostridia species,59, 60 can produce enteric short-chain fatty acids61 that have been shown to contribute to autistic-like behavior in animal models.62 These fatty acids can deplete carnitine stores and lead to secondary mitochondrial dysfunction.63 Thus, it is very possible that children who possess one or more of these susceptibility factors could be at increased risk for depressed CSF 5MTHF concentrations if FRAs develop during childhood. As FRα is essential for folate transport into the CNS when extracellular folate concentrations are low,20 blocking of the FRα by FRA may be especially detrimental under conditions of low extracellular folate availability.
In addition, the timing of the development of FRA may be a crucial factor in the phenotypic expression of reduced CNS folate. As the FRA does have non-zero prevalence in non-ASD adult populations23, 38, 39 and is found in some siblings and parents of FRA-positive children with ASD, the mere presence of FRAs does not necessarily cause ASD. Indeed, it is likely that FRAs appear during a period of rapid development, when folate is critically required for brain growth. As human FRAs cross-react with folate receptors in human, bovine and goat milk,5 it is very possible that exposure to any of these milk products, as occurs during the first year of life, could trigger FRA production. Chronic elevations in FRA could result in a progressive depression in CNS folate over time. Thus, symptoms of reduced CNS folate may only develop over a prolonged period of FRA elevations and reduced CNS folate.5 This would be a true example of a genetic susceptibility interacting with an environmental trigger. Unfortunately, we did not have the opportunity to measure FRA concentrations during the development of ASD symptoms in these children, but it is possible that FRA concentrations were higher during that time period. Clearly, a longitudinal study would be helpful to determine whether there is a critical window in which FRAs are most detrimental to brain development.
Interestingly, these novel findings along with the high prevalence of FR autoantibodies may help to integrate some apparently disparate findings described in some children with ASD. For example, folate deficiency in the CNS can lead to ASD in some children.4 Deficits in folate one-carbon metabolism have been shown to promote methylation deficits and oxidative stress in some children with ASD.8, 9, 10 This in turn could be associated with oxidative stress in the ASD brain.13, 64 Moreover, chronic oxidative stress can contribute to mitochondrial dysfunction,15 which has also been reported in the brains of some children with ASD.16 Abnormal populations of gut bacteria could contribute to increased production of enteric short-chain fatty acids, which could enhance the adverse effects of CNS folate deficiency and deplete carnitine levels, which has been described in some children with ASD.65 Furthermore, dietary cow's milk exposure may increase the production of these autoantibodies and help explain why some children with ASD improve on a milk-free diet.66 These findings point to metabolic-, environmental- and gastrointestinal-related factors in ASD, which may help explain ASD behaviors and brain changes, and serve as a rationale for additional experimentation and study in these areas.
CFD: a disorder on a continuum?
To our knowledge, this is the first study to report the prevalence of FRAs in a sample of children with ASD who did not possess significant neurological abnormalities. The findings of this study suggest that CFD may exist on a continuum, with less severely affected children developing ASD, and more significantly affected children (that is, those with the lowest CSF 5MTHF levels) possessing more severe neurological abnormalities including classical CFD syndrome. Additional studies examining children with ASD and children with CFD are required to explore this possibility.
Study limitations
This case series had several notable limitations, including a high male-to-female ratio (9:1), as compared with the more typical ratio for children with ASD of 4.5:167 or CFD of 2.5–3:1.2, 4, 5 In addition, both clinics included in this report primarily serve children with ASD who have persistent cognitive-behavioral deficits. This suggests that the samples may be subject to referral bias. Future studies are required to address whether a general ASD population also has an elevated FRA prevalence. Even if the presence of FRA is limited to a smaller subset of the ASD population than reported here, the significant response to leucovorin calcium in some children suggests that this in an important abnormality found in the ASD population that requires further study.
This study was not a clinical trial and neither the physicians nor the parents were blinded to treatment. In additional, our controls were not given a placebo; hence, the magnitude of the placebo effect was not taken into account, and we used a subjective parental report rather than objective assessment measures. Double-blind, placebo-controlled studies are required to confirm and expand upon the findings of this case series.
Conclusions
Several studies have reported the presence of FRAs in children with ASD who had significant neurological abnormalities.2, 3, 4, 5, 6, 7 In this study, an unexpectedly high prevalence (75.3%) of FRAs was found in 93 children with ASD without significant neurological abnormalities. In 16 children, the blocking FRA concentration was correlated with the CSF 5MTHF concentration, which was below the normative mean in each case. FRA-positive children who were treated with leucovorin calcium demonstrated significant improvements in verbal communication, receptive and expressive language, attention and stereotypical behavior compared with controls. The findings of this study suggest that empirical treatment with leucovorin calcium without performing an LP may be a reasonable and non-invasive approach in FRA-positive children with ASD. This study also supports further investigations of folate receptor autoimmunity and leucovorin calcium treatment in ASD. Although there is an animal model of hereditary folate malabsorption,68 there is no animal model of CFD or the clinical effects of FRAs at the current time. Such a model would be very helpful is validating the clinical significance of the FRA findings and leucovorin treatment. However, at this time, from the current evidence, it appears that FRA testing can lead to treatment that may improve the lives of children with ASD. As FRAs appears to be highly prevalent in children with ASD, we recommend that FRA testing should be considered in all patients with ASD.
Acknowledgments
We thank Michelle R Christie and Jamie Chu for their technical assistance. This study was supported, in part, by funding from the Autism Research Institute and the Jane Botsford Johnson Foundation.
Daniel Rossignol has two children with ASD and is a practicing primary care physician who treats ASD children with standard and integrative treatments. In the past, Dr Frye has provided expert opinion for child neurology cases for both the plaintiff and defendant, including cases with children suffering from mitochondrial disorders. All proceeds from such work are provided to the Department of Pediatrics at the University of Texas with some of these funds supporting Dr Frye's research. Drs Quadros and Sequeira are inventors on a US patent no. 7846672, issued to the Research Foundation of the State University of New York. Dr James has no conflict of interest to declare.
Footnotes
Supplementary Information accompanies the paper on the Molecular Psychiatry website (http://www.nature.com/mp)
Supplementary Material
References
- Ramaekers VT, Hausler M, Opladen T, Heimann G, Blau N. Psychomotor retardation, spastic paraplegia, cerebellar ataxia and dyskinesia associated with low 5-methyltetrahydrofolate in cerebrospinal fluid: a novel neurometabolic condition responding to folinic acid substitution. Neuropediatrics. 2002;33:301–308. doi: 10.1055/s-2002-37082. [DOI] [PubMed] [Google Scholar]
- Ramaekers VT, Blau N. Cerebral folate deficiency. Dev Med Child Neurol. 2004;46:843–851. doi: 10.1017/s0012162204001471. [DOI] [PubMed] [Google Scholar]
- Moretti P, Peters SU, Del Gaudio D, Sahoo T, Hyland K, Bottiglieri T, et al. Brief report: autistic symptoms, developmental regression, mental retardation, epilepsy, and dyskinesias in CNS folate deficiency. J Autism Dev Disord. 2008;38:1170–1177. doi: 10.1007/s10803-007-0492-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaekers VT, Blau N, Sequeira JM, Nassogne MC, Quadros EV. Folate receptor autoimmunity and cerebral folate deficiency in low-functioning autism with neurological deficits. Neuropediatrics. 2007;38:276–281. doi: 10.1055/s-2008-1065354. [DOI] [PubMed] [Google Scholar]
- Ramaekers VT, Sequeira JM, Blau N, Quadros EV. A milk-free diet downregulates folate receptor autoimmunity in cerebral folate deficiency syndrome. Dev Med Child Neurol. 2008;50:346–352. doi: 10.1111/j.1469-8749.2008.02053.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaekers VT, Rothenberg SP, Sequeira JM, Opladen T, Blau N, Quadros EV, et al. Autoantibodies to folate receptors in the cerebral folate deficiency syndrome. N Engl J Med. 2005;352:1985–1991. doi: 10.1056/NEJMoa043160. [DOI] [PubMed] [Google Scholar]
- Moretti P, Sahoo T, Hyland K, Bottiglieri T, Peters S, del Gaudio D, et al. Cerebral folate deficiency with developmental delay, autism, and response to folinic acid. Neurology. 2005;64:1088–1090. doi: 10.1212/01.WNL.0000154641.08211.B7. [DOI] [PubMed] [Google Scholar]
- James SJ, Cutler P, Melnyk S, Jernigan S, Janak L, Gaylor DW, et al. Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. Am J Clin Nutr. 2004;80:1611–1617. doi: 10.1093/ajcn/80.6.1611. [DOI] [PubMed] [Google Scholar]
- James SJ, Melnyk S, Jernigan S, Cleves MA, Halsted CH, Wong DH, et al. Metabolic endophenotype and related genotypes are associated with oxidative stress in children with autism. Am J Med Genet B Neuropsychiatr Genet. 2006;141:947–956. doi: 10.1002/ajmg.b.30366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnyk S, Fuchs GJ, Schulz E, Lopez M, Kahler SG, Fussell JJ, et al. Metabolic imbalance associated with methylation dysregulation and oxidative damage in children with autism. J Autism Dev Disord. published online 26 April 2011. [DOI] [PMC free article] [PubMed]
- Pogribny IP, Karpf AR, James SR, Melnyk S, Han T, Tryndyak VP. Epigenetic alterations in the brains of Fisher 344 rats induced by long-term administration of folate/methyl-deficient diet. Brain Res. 2008;1237:25–34. doi: 10.1016/j.brainres.2008.07.077. [DOI] [PubMed] [Google Scholar]
- Nagarajan RP, Hogart AR, Gwye Y, Martin MR, LaSalle JM. Reduced MeCP2 expression is frequent in autism frontal cortex and correlates with aberrant MECP2 promoter methylation. Epigenetics. 2006;1:e1–11. doi: 10.4161/epi.1.4.3514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajdel-Sulkowska EM, Xu M, McGinnis W, Koibuchi N. Brain region-specific changes in oxidative stress and neurotrophin levels in autism spectrum disorders (ASD) Cerebellum. 2010;10:43–48. doi: 10.1007/s12311-010-0223-4. [DOI] [PubMed] [Google Scholar]
- Ramaekers VT, Hansen SI, Holm J, Opladen T, Senderek J, Hausler M, et al. Reduced folate transport to the CNS in female Rett patients. Neurology. 2003;61:506–515. doi: 10.1212/01.wnl.0000078939.64774.1b. [DOI] [PubMed] [Google Scholar]
- Chauhan A, Chauhan V. Oxidative stress in autism. Pathophysiology. 2006;13:171–181. doi: 10.1016/j.pathophys.2006.05.007. [DOI] [PubMed] [Google Scholar]
- Chauhan A, Gu F, Essa MM, Wegiel J, Kaur K, Ted Brown W, et al. Brain region-specific deficit in mitochondrial electron transport chain complexes in children with autism. J Neurochem. 2011;117:209–220. doi: 10.1111/j.1471-4159.2011.07189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duthie SJ, Hawdon A. DNA instability (strand breakage, uracil misincorporation, and defective repair) is increased by folic acid depletion in human lymphocytes in vitro. FASEB J. 1998;12:1491–1497. [PubMed] [Google Scholar]
- Crott JW, Mashiyama ST, Ames BN, Fenech M. The effect of folic acid deficiency and MTHFR C677T polymorphism on chromosome damage in human lymphocytes in vitro. Cancer Epidemiol Biomarkers Prev. 2001;10:1089–1096. [PubMed] [Google Scholar]
- Iskandar BJ, Rizk E, Meier B, Hariharan N, Bottiglieri T, Finnell RH, et al. Folate regulation of axonal regeneration in the rodent central nervous system through DNA methylation. J Clin Invest. 2010;120:1603–1616. doi: 10.1172/JCI40000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wollack JB, Makori B, Ahlawat S, Koneru R, Picinich SC, Smith A, et al. Characterization of folate uptake by choroid plexus epithelial cells in a rat primary culture model. J Neurochem. 2008;104:1494–1503. doi: 10.1111/j.1471-4159.2007.05095.x. [DOI] [PubMed] [Google Scholar]
- Solanky N, Requena Jimenez A, D'Souza SW, Sibley CP, Glazier JD. Expression of folate transporters in human placenta and implications for homocysteine metabolism. Placenta. 2010;31:134–143. doi: 10.1016/j.placenta.2009.11.017. [DOI] [PubMed] [Google Scholar]
- Weitman SD, Weinberg AG, Coney LR, Zurawski VR, Jennings DS, Kamen BA. Cellular localization of the folate receptor: potential role in drug toxicity and folate homeostasis. Cancer Res. 1992;52:6708–6711. [PubMed] [Google Scholar]
- Molloy AM, Quadros EV, Sequeira JM, Troendle JF, Scott JM, Kirke PN, et al. Lack of association between folate-receptor autoantibodies and neural-tube defects. N Engl J Med. 2009;361:152–160. doi: 10.1056/NEJMoa0803783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrocal-Zaragoza MI, Fernandez-Ballart JD, Murphy MM, Cavalle-Busquets P, Sequeira JM, Quadros EV. Association between blocking folate receptor autoantibodies and subfertility. Fertil Steril. 2009;91 (4 Suppl:1518–1521. doi: 10.1016/j.fertnstert.2008.08.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaekers VT, Weis J, Sequeira JM, Quadros EV, Blau N. Mitochondrial complex I encephalomyopathy and cerebral 5-methyltetrahydrofolate deficiency. Neuropediatrics. 2007;38:184–187. doi: 10.1055/s-2007-991150. [DOI] [PubMed] [Google Scholar]
- Garcia-Cazorla A, Quadros EV, Nascimento A, Garcia-Silva MT, Briones P, Montoya J, et al. Mitochondrial diseases associated with cerebral folate deficiency. Neurology. 2008;70:1360–1362. doi: 10.1212/01.wnl.0000309223.98616.e4. [DOI] [PubMed] [Google Scholar]
- O'Byrne MR, Au KS, Morrison AC, Lin JI, Fletcher JM, Ostermaier KK, et al. Association of folate receptor (FOLR1, FOLR2, FOLR3) and reduced folate carrier (SLC19A1) genes with meningomyelocele. Birth Defects Res. 2010;88:689–694. doi: 10.1002/bdra.20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matherly LH, Hou Z, Deng Y. Human reduced folate carrier: translation of basic biology to cancer etiology and therapy. Cancer Metastasis Rev. 2007;26:111–128. doi: 10.1007/s10555-007-9046-2. [DOI] [PubMed] [Google Scholar]
- Yuasa H, Inoue K, Hayashi Y. Molecular and functional characteristics of proton-coupled folate transporter. J Pharma Sci. 2009;98:1608–1616. doi: 10.1002/jps.21515. [DOI] [PubMed] [Google Scholar]
- Hou Z, Matherly LH. Oligomeric structure of the human reduced folate carrier: identification of homo-oligomers and dominant-negative effects on carrier expression and function. J Biol Chem. 2009;284:3285–3293. doi: 10.1074/jbc.M807206200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen FJ, Blau N. Cerebral folate deficiency: life-changing supplementation with folinic acid. Mol Genet Metab. 2005;84:371–373. doi: 10.1016/j.ymgme.2004.12.001. [DOI] [PubMed] [Google Scholar]
- APA Diagnostic and Statistical Manual of Mental Disorders4th ednAmerican Psychiatric Association: Washington, DC; 1994 [Google Scholar]
- Rossignol DA, Frye RE. Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Mol Psychiatry. [DOI] [PMC free article] [PubMed]
- Frye RE, Rossignol DA. Mitochondrial dysfunction can connect the diverse medical symptoms associated with autism spectrum disorders. Pediatric Res. 2011;69 (5 Pt 2:41R–47R. doi: 10.1203/PDR.0b013e318212f16b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy W. ECDEU Assessment Manual for Psychopharmacology - Revised (DHEW Publ No ADM 76-338). Rockville, MD, U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs. 1976. pp. 218–222.
- Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB.Designing Clinical Research3rd ednLippincott Williams & Wilkins: Philadephia; 2006 [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis for the social, behavioral, and biomedical sciences. Behavior Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Berrocal-Zaragoza MI, Fernandez-Ballart JD, Murphy MM, Cavalle-Busquets P, Sequeira JM, Quadros EV. Association between blocking folate receptor autoantibodies and subfertility. Fertil Steril. 2009;91:1518–1521. doi: 10.1016/j.fertnstert.2008.08.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrocal-Zaragoza MI, Murphy MM, Ceruelo S, Quadros EV, Sequeira JM, Fernandez-Ballart JD. High milk consumers have an increased risk of folate receptor blocking autoantibody production but this does not affect folate status in Spanish men and women. J Nutr. 2009;139:1037–1041. doi: 10.3945/jn.108.102475. [DOI] [PubMed] [Google Scholar]
- Koenig MK, Perez M, Rothenberg S, Butler IJ. Juvenile onset central nervous system folate deficiency and rheumatoid arthritis. J Child Neurol. 2008;23:106–107. doi: 10.1177/0883073807307986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad NS, Jain JM, Chintakindi KP, Singh RP, Naik U, Akella RR. Aberrations in folate metabolic pathway and altered susceptibility to autism. Psychiatr Genet. 2009;19:171–176. doi: 10.1097/YPG.0b013e32832cebd2. [DOI] [PubMed] [Google Scholar]
- Boris M, Goldblatt A, Galanko J, James SJ. Association of MTHFR gene variants with autism. J Am Physicians Surgeons. 2004;9:106–108. [Google Scholar]
- Adams M, Lucock M, Stuart J, Fardell S, Baker K, Ng X. Preliminary evidence for involvement of the folate gene polymorphism 19bp deletion-DHFR in occurrence of autism. Neurosci Lett. 2007;422:24–29. doi: 10.1016/j.neulet.2007.05.025. [DOI] [PubMed] [Google Scholar]
- Hyland K, Shoffner J, Heales SJ. Cerebral folate deficiency. J Inherit Metab Dis. 2010;33:563–570. doi: 10.1007/s10545-010-9159-6. [DOI] [PubMed] [Google Scholar]
- Miller AL. The methylation, neurotransmitter, and antioxidant connections between folate and depression. Altern Med Rev. 2008;13:216–226. [PubMed] [Google Scholar]
- Neustadt J, Pieczenik SR. Medication-induced mitochondrial damage and disease. Mol Nutr Food Res. 2008;52:780–788. doi: 10.1002/mnfr.200700075. [DOI] [PubMed] [Google Scholar]
- Ahn MS, Sims KB, Frazier JA. Risperidone-induced psychosis and depression in a child with a mitochondrial disorder. J Child Adolesc Psychopharmacol. 2005;15:520–525. doi: 10.1089/cap.2005.15.520. [DOI] [PubMed] [Google Scholar]
- Thomas RH, Foley KA, Mepham JR, Tichenoff LJ, Possmayer F, MacFabe DF. Altered brain phospholipid and acylcarnitine profiles in propionic acid infused rodents: further development of a potential model of autism spectrum disorders. J Neurochem. 2010;113:515–529. doi: 10.1111/j.1471-4159.2010.06614.x. [DOI] [PubMed] [Google Scholar]
- MacFabe DF, Cain DP, Rodriguez-Capote K, Franklin AE, Hoffman JE, Boon F, et al. Neurobiological effects of intraventricular propionic acid in rats: possible role of short chain fatty acids on the pathogenesis and characteristics of autism spectrum disorders. Behav Brain Res. 2007;176:149–169. doi: 10.1016/j.bbr.2006.07.025. [DOI] [PubMed] [Google Scholar]
- Nikolov RN, Bearss KE, Lettinga J, Erickson C, Rodowski M, Aman MG, et al. Gastrointestinal symptoms in a sample of children with pervasive developmental disorders. J Autism Dev Disord. 2009;39:405–413. doi: 10.1007/s10803-008-0637-8. [DOI] [PubMed] [Google Scholar]
- James SJ, Melnyk S, Fuchs G, Reid T, Jernigan S, Pavliv O, et al. Efficacy of methylcobalamin and folinic acid treatment on glutathione redox status in children with autism. Am J Clin Nutr. 2009;89:425–430. doi: 10.3945/ajcn.2008.26615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croen LA, Braunschweig D, Haapanen L, Yoshida CK, Fireman B, Grether JK, et al. Maternal mid-pregnancy autoantibodies to fetal brain protein: the early markers for autism study. Biol Psychiatry. 2008;64:583–588. doi: 10.1016/j.biopsych.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills S, Cabanlit M, Bennett J, Ashwood P, Amaral D, Van de Water J. Autoantibodies in autism spectrum disorders (ASD) Ann NY Acad Sci. 2007;1107:79–91. doi: 10.1196/annals.1381.009. [DOI] [PubMed] [Google Scholar]
- Wills S, Rossi CC, Bennett J, Cerdeno VM, Ashwood P, Amaral DG, et al. Further characterization of autoantibodies to GABAergic neurons in the central nervous system produced by a subset of children with autism. Mol Autism. 2011;2:5. doi: 10.1186/2040-2392-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills S, Cabanlit M, Bennett J, Ashwood P, Amaral DG, Van de Water J. Detection of autoantibodies to neural cells of the cerebellum in the plasma of subjects with autism spectrum disorders. Brain Behav Immun. 2009;23:64–74. doi: 10.1016/j.bbi.2008.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braunschweig D, Ashwood P, Krakowiak P, Hertz-Picciotto I, Hansen R, Croen LA, et al. Autism: maternally derived antibodies specific for fetal brain proteins. Neurotoxicology. 2008;29:226–231. doi: 10.1016/j.neuro.2007.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James SJ, Melnyk S, Jernigan S, Hubanks A, Rose S, Gaylor DW. Abnormal transmethylation/transsulfuration metabolism and DNA hypomethylation among parents of children with autism. J Autism Dev Disord. 2008;38:1966–1975. doi: 10.1007/s10803-008-0591-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goin-Kochel RP, Porter AE, Peters SU, Shinawi M, Sahoo T, Beaudet AL. The MTHFR 677C-->T polymorphism and behaviors in children with autism: exploratory genotype-phenotype correlations. Autism Res. 2009;2:98–108. doi: 10.1002/aur.70. [DOI] [PubMed] [Google Scholar]
- Finegold SM, Molitoris D, Song Y, Liu C, Vaisanen ML, Bolte E, et al. Gastrointestinal microflora studies in late-onset autism. Clin Infect Dis. 2002;35 (Suppl 1:S6–S16. doi: 10.1086/341914. [DOI] [PubMed] [Google Scholar]
- Finegold SM. State of the art; microbiology in health and disease intestinal bacterial flora in autism. Anaerobe. [DOI] [PubMed]
- Williams BL, Hornig M, Buie T, Bauman ML, Cho Paik M, Wick I, et al. Impaired carbohydrate digestion and transport and mucosal dysbiosis in the intestines of children with autism and gastrointestinal disturbances. PLoS One. 2011;6:e24585. doi: 10.1371/journal.pone.0024585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacFabe DF, Thomas RH, Foley KA, Mepham JR, Tichenoff LJ, Possmayer F. Altered brain phospholipid and acylcarnitine profiles in propionic acid infused rodents: further development of a potential model of autism spectrum disorders. J Neurochem. 2010;113:515–529. doi: 10.1111/j.1471-4159.2010.06614.x. [DOI] [PubMed] [Google Scholar]
- MacFabe DF, Rodríguez-Capote K, Hoffman JE, Franklin AE, Mohammad-Asef Y, Taylor AR, et al. A novel rodent model of autism: intraventricular infusions of propionic acid increase locomotor activity and induce neuroinflammation and oxidative stress in discrete regions of adult rat brain. Am J Biochem Biotech. 2008;4:146–166. [Google Scholar]
- Sajdel-Sulkowska EM, Xu M, Koibuchi N. Increase in cerebellar neurotrophin-3 and oxidative stress markers in autism. Cerebellum. 2009;8:366–372. doi: 10.1007/s12311-009-0105-9. [DOI] [PubMed] [Google Scholar]
- Filipek PA, Juranek J, Nguyen MT, Cummings C, Gargus JJ. Relative carnitine deficiency in autism. J Autism Dev Disord. 2004;34:615–623. doi: 10.1007/s10803-004-5283-1. [DOI] [PubMed] [Google Scholar]
- Whiteley P, Haracopos D, Knivsberg AM, Reichelt KL, Parlar S, Jacobsen J, et al. The ScanBrit randomised, controlled, single-blind study of a gluten- and casein-free dietary intervention for children with autism spectrum disorders. Nutr Neurosci. 2010;13:87–100. doi: 10.1179/147683010X12611460763922. [DOI] [PubMed] [Google Scholar]
- Rice C. Prevalence of autism spectrum disorders –autism and developmental disabilities monitoring network, United States, 2006. MMWR Surveill Summ. 2009;58:1–20. [PubMed] [Google Scholar]
- Salojin KV, Cabrera RM, Sun W, Chang WC, Lin C, Duncan L, et al. A mouse model of hereditary folate malabsorption: deletion of the PCFT gene leads to systemic folate deficiency. Blood. 2011;117:4895–4904. doi: 10.1182/blood-2010-04-279653. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.