Abstract
Purpose
This study aims to investigate direct and indirect pathways of family flexibility, social support, and family communication on health-related quality of life (HRQOL) for Chinese- and Korean-American breast cancer survivors (BCS).
Methods
A total of 157 Chinese (n = 86)- and Korean-American (n = 71) BCS were recruited from the California Cancer Surveillance Program and area hospitals in Los Angeles County. The present study was guided by the Resiliency Model of Family Stress, Adjustment, and Adaptation.
Results
Structural equation modeling demonstrated that (1) family communication was directly associated with HRQOL for both groups; (2) family flexibility was indirectly associated with HRQOL through family communication for Korean-Americans only; (3) social support mediated the relationship between family flexibility and family communication for Chinese-Americans only; and (4) acculturation was directly related to social support for both groups. Multigroup analysis demonstrated that the structural paths were equivalent between Chinese- and Korean-American BCS, although statistical differences in baseline parameters were noted.
Conclusions
Our findings suggest that family communication impacts HRQOL among Asian-American BCS. Our results show that while there are commonalities in family characteristics among Asian-Americans, specific ethnic variations also exist. Therefore, specific cultural and familial contexts should be assessed to better inform interventions to enhance family communication strategies and improve HRQOL.
Keywords: Asian-Americans, Breast cancer survivors, Family communication, Family functioning, Health-related quality of life
Introduction
Asian-Americans share an increasing representation among breast cancer survivors (BCS) due to their population growth and increasing breast cancer incidence and a 90.6 % survival rate [1, 2]. Yet, the term ‘Asian-Americans’ represents diverse groups with differential results on cancer-related quality of life [3, 4]. Thus, further research with larger samples of Asian-American subgroups is necessary to accurately document health-related quality of life (HRQOL) outcomes. This study specifically focused on examining family functioning and communication on HRQOL within Chinese- and Korean-American BCS as they are the largest and fastest growing Asian-American subpopulations in the United States [5]. Chinese- and Korean-Americans have emigrated from close geographical proximity and share several common aspects such as Confucian and collectivistic values [6]. At the same time, different cultures, languages, historical experiences, and immigration patterns exist between them [6]. For example, the Chinese group has a longer presence in the United States dating back to the 1800s, while the Korean group largely began in the 1960s [7]. Consequently, Korean-Americans are less likely than Chinese-Americans to be acculturated with limited social networks and as a result show higher expectations and demands within their own families [4, 8]. However, Chinese- and Korean-Americans who were born outside the United States are particularly understudied and may have greater cancer survivorship concerns. Therefore, this study focuses on the immigrant populations that we are defining as Chinese-American and Korean-American [9].
HRQOL is a major research interest in cancer survivorship studies. It is a concept that embraces the multidimensional aspects of health and can be used to assess the impact of cancer [10, 11]. The amount of HRQOL research has recently grown and is quite vast; however, there is a scarcity of information about Asian-Americans. Previous studies have found that Korean-American BCS expressed lower HRQOL than European-American BCS [12, 13] and even those of other Asian-American subgroups, including Chinese-Americans [3]. However, these studies included small numbers of Asian-Americans and relied largely on purposive or snowball sampling, thus limiting the generalizability for the findings [13, 14]. Furthermore, these studies lack evidence regarding specific factors associated with HRQOL outcomes among diverse Asian-American subgroups.
How individuals and their families cope with cancer experiences may influence HRQOL [15]. Specifically, family communication is an important component of the adaptive coping mechanisms for managing family tension among cancer survivors, including concepts such as listening, speaking, clarity, respect within the family, and decision making [16, 17]. Several studies have demonstrated that optimal communication (i.e., clarity, open emotional expression) and shared decision making during a traumatic event can improve HRQOL for BCS [18, 19]. Meanwhile, Morse and Fife [20] found that BCS who avoided conversations with their husbands about the impact of cancer demonstrated poorer adjustment than those who did engage in conversations. Generally, Asian culture emphasizes harmony or value of smooth interpersonal relationships in the family [21]. Thus, Chinese- and Korean-American women who maintain their traditional cultural viewpoints may feel uncomfortable expressing their emotional and physical distress during the survivorship period. Nevertheless, individuals who are more acculturated or bicultural may value more open and direct communication [22].
Patterns of family functioning (i.e., family flexibility) may influence communication within families facing a health crisis [23]. It is reported that families who are more flexible in modifying daily tasks effectively communicate to cope with stressors than do those families who are rigid [24]. Moreover, social support is regarded as one of the important family resources for coping, which can enhance a person’s ability to alleviate the impact of life stressors [25, 26]. Research on the mediating influence of social support has emphasized the role of social support in protecting against the effects of family functioning, and thereby contributing to a family’s coping process and adjustment [27]. However, there is no research on how family flexibility and social support are associated with family communication and HRQOL for Chinese- and Korean-American BCS.
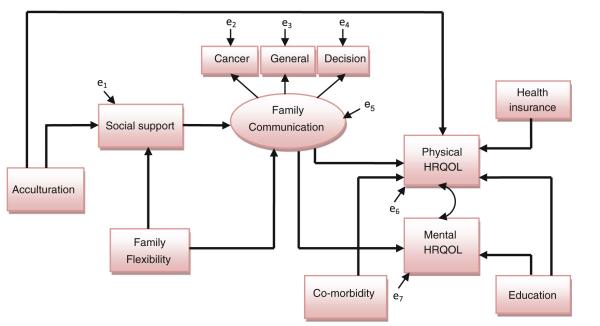
The present study was guided by the Resiliency Model of Family Stress, Adjustment, and Adaptation [28, 29]. The resilience model suggests that families will experience stress and hardship during crises, but through their own strengths and relationships in the community, they will adjust and adapt by giving meaning and purposes to their experience [30]. Specifically, strengths and capabilities or resiliency factors during the adaptation phase include family functioning, acquiring new or activating old social support resources at the individual, family, and community levels, and actively engaging in new coping and problem-solving strategies. This model also emphasizes the idea that family members engage in active coping efforts to balance family vulnerability with family capabilities and resources, considering the effects of culture on HRQOL (Fig. 1) [26]. Based on this Resilience Model, family communication, family flexibility, and social support factors were examined in this study. Given that cultural context can impact the relationships among variables in the study, the influence of acculturation in Chinese- and Korean-Americans was also considered.
Fig. 1.
The conceptual model: The resiliency model of family adjustment and adaptation
The primary objective of this study was to test and compare an adapted conceptual model of HRQOL for Chinese- and Korean-American BCS. The authors hypothesized that (1) family communication would be directly associated with HRQOL; (2) family flexibility would be indirectly associated with HRQOL through family communication; (3) social support would mediate the relationship between family flexibility and communication; and (4) acculturation would be associated with family flexibility, social support, family communication, and HRQOL. These hypotheses were also tested to investigate differences between Chinese- and Korean-American BCS.
Methods
Sample
Participants were included if they (1) were within 1–5 years of breast cancer diagnosis (stages I–III); (2) had completed active treatment (surgery, radiation, and/or chemotherapy); (3) had not been diagnosed with another type of cancer; (4) did not have any other major disabling medical (e.g., stroke) or psychiatric conditions (e.g., schizophrenia); (5) self-identified as Chinese- or Korean-American; and (6) were able to speak Mandarin/Cantonese, Korean, and/or English.
Data collection procedures
Participants were drawn from the California Cancer Surveillance Program (CSP) and area hospitals in Los Angeles County from October 2009 to April 2011. To recruit study participants, investigators mailed invitation letters to BCS whose contact information was obtained from the CSP and local hospital registries. BCS who did not respond to the invitation letters received a telephone call from a research assistant 2 weeks after the mailing. If the potential participant was interested, then the research assistant conducted a screening over the phone to assess eligibility. Eligible participants were mailed a questionnaire and consent form and were asked to return them in an enclosed prepaid envelope within 3 weeks. If survivors had not returned the survey after the third follow-up phone call, they were considered nonrespondents. The recruitment procedure was approved by the Case Western Reserve University and the City of Hope Institutional Review Boards.
Instruments
Using a rigorous “forward–backward” translation procedure, the English versions of the questionnaires were translated and back-translated into Chinese and Korean by independent, bilingual translators. The panel of translators then compared the two English versions to ensure that they were equivalent. If they were not, corrections were made until equivalence was achieved. Revisions resulting from the pilot test were incorporated into the final questionnaires. In this study, the internal consistency of the scales ranged from 0.72 to 0.98 (Table 2). Preliminary analysis demonstrated that no major differences in demographic and medical characteristics as well as outcomes existed as a result of the language of administration.
Table 2.
Predictor and outcome variables for Chinese- and Korean-American breast cancer survivors
| Variables | Chinese (n = 86) |
Korean (n = 71) |
F | ||
|---|---|---|---|---|---|
| Mean (SD) | Cronbach’s α | Mean (SD) | Cronbach’s α | ||
| Physical HRQOL (SF-36 PCS) | 60.4 (23.0) | – | 63.6 (25.1) | – | 0.04 |
| Mental HRQOL (SF-36 MCS) | 63.5 (22.4) | – | 67.2 (23.5) | – | 0.27 |
| SF-36 subscales | |||||
| Physical functioning | 71.3 (25.2) | 0.87 | 61.8 (29.0) | 0.85 | 5.48* |
| Role-physical | 41.1 (40.3) | 0.83 | 58.9 (43.2) | 0.90 | 3.59 |
| Bodily pain | 70.7 (23.8) | 0.87 | 75.1 (24.8) | 0.89 | 0.35 |
| General health perception | 58.7 (23.0) | 0.81 | 58.6 (24.3) | 0.82 | 0.15 |
| Social functioning | 71.7 (24.7) | 0.81 | 75.5 (26.1) | 0.82 | 0.17 |
| Mental health | 69.2 (19.5) | 0.86 | 69.0 (19.8) | 0.85 | 0.02 |
| Role-emotional | 53.7 (43.1) | 0.81 | 70.0 (42.1) | 0.91 | 3.59 |
| Vitality | 58.5 (20.2) | 0.86 | 54.2 (20.6) | 0.81 | 2.05 |
| Family communication | |||||
| General communication | 3.7 (1.0) | 0.96 | 3.7 (1.0) | 0.96 | 0.08 |
| Cancer-related communication | 3.8 (1.2) | 0.95 | 4.2 (1.1) | 0.93 | 2.13 |
| Decisions with family | 3.8 (1.3) | 0.81 | 3.7 (1.2) | 0.72 | 0.01 |
| Family flexibility | 3.1 (0.8) | 0.92 | 2.9 (0.7) | 0.91 | 4.37* |
| Social support | 3.5 (1.0) | 0.97 | 3.2 (1.2) | 0.98 | 2.37 |
| The level of acculturation | 3.5 (1.0) | 0.96 | 3.0 (0.9) | 0.81 | 18.67*** |
Education, cancer stage, surgery-Axillary node dissection, and years since diagnosis have been controlled
SD standard deviation, HRQOL health-related quality of life, PCS physical component summary, MCS mental component summary
p<0.05;
p<0.001
Health-related quality of life
To assess HRQOL, the Medical Outcome Study (MOS) SF-36, which is an internally consistent and reliable self-report quality of life tool, was used [31]. This 36-item measure contains 8 multi-item subscales: (1) physical functioning, (2) physical role limitation, (3) bodily pain, (4) general health perception, (5) vitality, (6) social functioning, (7) emotional role limitation, and (8) mental health. These 8 scales provided the basis for calculating 2 summary scores, the Physical Component Summary (PCS) and the Mental Component Summary (MCS). Subscale scores were computed by summing across items in the same scale and then transforming raw scale scores to a range from 0 to 100. Higher scores on summary measures and all 8 subscales represent better HRQOL.
Family communication
Three family communication scales were used to comprehensively create the latent factor of family communication including general communication, cancer-related communication, and shared decision making. First, the Family Adaptability and Cohesion Evaluation Scales (FACES IV)-Family Communication Scale was designed to investigate the functionality of communication within the family (referred to as general communication) [32]. Responses to this 10-item self-report questionnaire were given using a 5-point Likert scale. The general communication score was obtained by averaging 10 items with higher scores indicating better family communication. Second, the Family Avoidance of Communication About Cancer (FACC) Scale was used to assess the patient’s perception of the extent to which family avoids talking about the cancer experience (referred to as cancer-related communication) (5-item) [33]. Each item is measured on a 5-point Likert scale, and scores are calculated by averaging the items. Higher scores reflect better communication about the cancer. Third, we developed one question to assess the importance of family involvement in health decisions (3-item) (referred to as shared decision making). This study asked the following question: “How important is each of these groups/people to making the health decisions?” Respondents rated each item on (1) family (parents, siblings, and other relatives), (2) children, and (3) partner/spouse from 1 to 5, with higher scores indicating positive outcomes. A total score was obtained by averaging the 3 items.
Family flexibility
Family flexibility was adapted from the Family Adaptability and Cohesion Evaluation Scales-III (FACES-IIII), which is a 20-item standardized family functioning instrument [34]. The current study used 4 items in the FACES-III adaptability subscale (a family’s ability to cope as a flexible unit) to measure family flexibility, which is defined as the family’s ability to change its power structure, role relationships, and rules to respond to situational needs. The family flexibility score was obtained by averaging these 4 items. According to Olson [34], optimal family functioning exists in families who have moderate rather than extreme scores, suggesting that low scores on the adaptability scale indicate a rigid family and high scores indicate a chaotic family. Nevertheless, the current study showed a linear pattern without the extreme scores (skewness = 0.003), indicating that high scores on the family adaptability subscale reflected positive functioning in family flexibility.
Social support
Social support was assessed through the MOS Social Support Survey. A 19-item assessment of social support consists of 4 subscales: (1) emotional/informational (8-item), (2) tangible (4-item), (3) affectionate (3-item), and (4) positive social interaction (3-item) with one additional general item [35]. Items are rated on a five-point Likert scale ranging from 1 to 5, with higher scores indicating better social support. The social support score was computed by averaging all items.
Cultural characteristics
The Asian-American Multidimensional Acculturation Scale (AAMAS)–European-American section was used to assess the level of acculturation [36]. This scale consists of 15 items, including cultural identity and knowledge, language, and food consumption. Each item is measured on a 6-point Likert scale, with higher scores indicating more acculturation. Scores were obtained by averaging all items.
Demographic and medical characteristics
Demographic and medical information such as age, education, income, health insurance, employment status, marital status, living situation, country of birth, length of stay in the United States, cancer stage, years since diagnosis, and number of comorbidities were included to be considered as control variables. The number of comorbidities was obtained by summing the self-reported medical conditions from a list of 24 chronic medical conditions.
Data analyses
Exploratory data analyses were conducted to describe the demographic and medical characteristics. Correlation analyses assessed bivariate associations between variables. Univariate general linear model was also conducted to investigate differences in major variables by ethnicity, after controlling for covariates. Analyses were conducted using SPSS 20.0.
Structural equation modeling (SEM) was used to test the hypothesized conceptual model using AMOS 20.0. In our data, the number of missing values was less than 1 %; thus, missing data were addressed through full information maximum likelihood estimation to provide a less biased estimation [37]. As the first step, the confirmatory factor analysis (CFA) was conducted to determine the adequacy of a family communication construct consisting of general communication, cancer-related communication, and shared decision making to see whether these family communication variables shared a common latent origin.
In the second step, the relationships among variables were specified based on the conceptual model and the exploratory specification search procedure in AMOS [38]. Unit-weighted observed composites for indicators were used to reduce the number of parameter estimations for a complex structural model. The overall model was created by adding (1) the direct pathway of family communication on PCS and MCS; (2) the direct pathway of acculturation on family flexibility, social support, family communication, PCS, and MCS, (3) a mediated-path structural model of family communication between family flexibility and communication, and of social support between family flexibility and communication; (4) control variables influencing PCS and MCS; and (5) covariances between variables. Because we were interested in overall HRQOL for BCS, we included two outcome variables (PCS and MCS) in one combined model rather than examining outcomes separately.
The hypothesized model was evaluated using goodness of fit indices, including the chi-squared statistic or discrepancy function, the ratio of the discrepancy function to the degrees of freedom, the root mean square error of approximation (RMSEA; acceptable fit ≤ .08) [39], and the Comparative Fit Index (CFI; acceptable model fit ≥ .9) [40]. In SEM, a nonsignificant chi-square value is an indication that the hypothesized model has a good fit with the data [41]. Here, RMSEA has been selected because it is not affected by model complexity [42]. Model parameters were also considered to be statistically significant at the level of 0.05 [43].
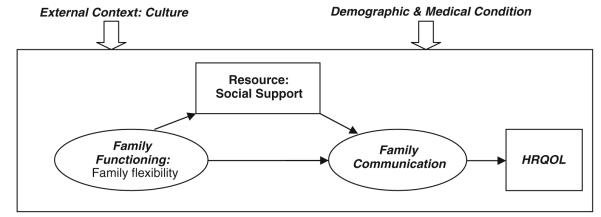
The hypothesized model was tested with the entire sample and for each ethnicity, separately, in order to identify the correct structural model to compare the two groups. The goodness of fit and model parameters were evaluated per the criteria specified above. To provide the best fitting model, we determined to exclude paths from the final model if p values are greater than 0.1, such that paths from acculturation to MCS (p = 0.423), and from acculturation to family communication (p = 0.609) were excluded. To adjust for covariates influencing outcomes, variables showing significant differences in PCS and MCS (i.e., health insurance, education, and number of comorbidities) were included as control variables. The modification indices in AMOS also suggested adding covariances (i.e., unstandardized correlations) between variables to significantly improve the fit of the model; thus, five covariances (i.e., acculturation and health insurance, social support and health insurance, social support and comorbidities, health insurance and education, and PCS and MCS) were added based on the theoretical justification for each relationship. The resulting final model was then used to test the differences between Chinese- and Korean-Americans (see Fig. 2).
Fig. 2.
The hypothesized model of health-related quality of life for Chinese- and Korean-American breast cancer survivors. “Health insurance” is correlated with “acculturation,” “social support,” and “education”; “co-morbidity” is correlated with “social support”; health insurance was dummy coded (1 = public insurance; ref = private insurance); education was dummy coded (1 = <High school; ref = >High school); “e1–7” indicates the residual variance of each variable
Multigroup SEM was used to test for ethnic differences, whereby two final SEM, as shown in Fig. 2, were estimated and evaluated simultaneously. Initially, all parameters for Chinese- and Korean-Americans were unconstrained (i.e., the parameters are allowed to be different between ethnicity); this is the “baseline” model. Then, all factor loadings for the family communication latent factor were constrained to test for measurement invariance, in order to test whether or not family communication, as measured by the three subscales, was measuring the same construct for both Chinese- and Korean-Americans. Next, structural paths including measurement were constrained, testing for measurement and structural invariances, which would indicate whether or not the model was equivalent for Chinese- and Korean-Americans. Each constrained model was compared against the baseline model by computing a chi-square different test. Additionally, Sobel test was used for further verification of the mediation effects [44].
Results
Sample characteristics
Of the 619 BCS who were mailed invitation letters, 250 were accessible. Most did not respond to the letters or follow-up telephone call. Of all of the accessible persons, 157 BCS (86 Chinese- and 71 Korean-Americans) completed the final survey, achieving a final response rate of 62.8 % of the accessible sample. Those who participated in this study did not show any differences in available information (i.e., age, cancer stage, and years since diagnosis) compared with those who did not participate.
Chinese- and Korean-American BCS did not differ significantly on most demographic characteristics but education: Korean-Americans were more likely than Chinese-Americans to have higher levels of education. In the medical characteristics, cancer stage, surgery-axillary node dissection, and years since diagnosis showed significant differences between the two groups (Table 1). These differences were adjusted in the multivariate analysis. As illustrated in Table 2, HRQOL, family communication, and social support scores did not reveal significant differences between Chinese- and Korean-Americans, after adjusting for education, cancer stage, surgery-axillary node dissection, and years since diagnosis. However, the two groups differed significantly in family flexibility and acculturation after adjusting for covariates. Chinese-Americans were more likely than Korean-Americans to have flexibility in the family functioning and to be acculturated.
Table 1.
Demographic and medical characteristics of Chinese- and Korean-Americans
| Characteristics | Chinese (n = 86) |
Korean (n = 71) |
t |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Age | 55.2 (9.7) | 53.9 (9.7) | −0.19 |
| Length of stay in the United States |
23.5 (12.2) | 23.9 (9.9) | −0.48 |
| Years since diagnosis | 3.2 (1.8) | 3.9 (1.4) | −2.60* |
| Number of comorbidities | 3.8 (3.2) | 3.0 (3.4) | 1.48 |
|
| |||
| n (%) | n (%) | χ 2 | |
|
| |||
| Education | |||
| <High school | 16 (18.6) | 2 (2.8) | 10.05** |
| High school graduated | 11 (12.8) | 14 (19.7) | |
| >High school | 59 (68.6) | 55 (77.5) | |
| Household income | |||
| <25 K | 35 (40.7) | 22 (33.8) | 1.65 |
| 25 K–45 K | 13 (15.1) | 12 (18.5) | |
| 45 K–75 K | 14 (16.3) | 12 (18.5) | |
| >75 K | 18 (20.9) | 19 (29.2) | |
| Current employment status | |||
| Unemployed/homemaker | 57 (66.3) | 53 (74.6) | 1.30 |
| Employed | 29 (33.7) | 18 (25.4) | |
| Marital status | |||
| Married | 69 (80.2) | 56 (78.9) | 0.04 |
| Others | 17 (19.8) | 15 (21.1) | |
| Living situation | |||
| Alone | 10 (11.8) | 8 (11.3) | 0.01 |
| Partner | 62 (72.1) | 55 (77.5) | 0.59 |
| Children only | 48 (55.8) | 30 (42.3) | 2.86 |
| Partner and children | 33 (38.4) | 24 (33.8) | 0.35 |
| Others | 13 (15.1) | 8 (11.3) | 0.50 |
| Health insurance | |||
| Private | 38 (48.7) | 27 (45.0) | 1.17 |
| Public (Medicare/Medicaid) | 35 (44.9) | 26 (43.3) | |
| No insurance | 5 (6.4) | 7 (11.7) | |
| Primary language | |||
| Own language (Chinese/Korean) | 76 (88.4) | 66 (93.0) | 0.95 |
| English | 10 (11.6) | 5 (7.0) | |
| Country of birth | |||
| United States | 5 (5.8) | 1 (1.4) | 149.66*** |
| China/Taiwan | 74 (86.0) | 0 (0.0) | |
| Korea | 1 (1.2) | 70 (98.6) | |
| Other | 6 (7.0) | 0 (0.0) | |
| Cancer stage | |||
| 0 | 10 (11.6) | 1 (1.4) | 16.01** |
| I | 22 (25.6) | 34 (48.6) | |
| II | 45 (52.3) | 23 (32.9) | |
| III | 9 (10.5) | 12 (17.1) | |
|
| |||
| n (%) | n (%) | χ 2 | |
| Surgery (yes)a | |||
|
| |||
| Axillary node dissection | 39 (45.3) | 22 (31.0) | 3.38* |
| Lumpectomy | 45 (52.3) | 37 (52.1) | 0.00 |
| Mastectomy | 48 (55.8) | 35 (49.3) | 0.66 |
| Radiation (Yes) | 45 (55.6) | 41 (58.6) | 0.14 |
| Chemotherapy (yes) | 61 (72.6) | 44 (62.0) | 2.00 |
| Hormonal therapy (yes) | 58 (68.2) | 41 (58.6) | 1.55 |
SD standard deviation
p<0.05;
p<0.01;
p<0.001
Participants could select more than one response
Confirmatory factor analysis: family communication construct
CFA was performed to test the family communication construct across groups. The single-group analyses in both Chinese- and Korean-American BCS confirmed the adequacy of the family communication latent factor: Chinese: χ2(132) = 210.17, p = < 0.001, CFI = 0.94, RMSEA = 0.08; Korean: χ2(132) = 217.71, p = < 0.001, CFI = 0.93, RMSEA = 0.08. All indicators loaded on their respective factors at 0.36 or greater; all loadings were significant at a p < 0.01 level. Although the fit indices of this latent factor model were not high enough, we determined that this model is appropriate to reflect upon meaning of the family communication construct based on the theoretical justification.
Multigroup analyses of the hypothesized model across the two ethnic groups
The hypothesized model was created with two HRQOL outcome variables (PCS and MCS), two mediators (social support and family communication), one predictor (acculturation), and three covariates (health insurance, education, and number of comorbidities). When estimated with Chinese-American BCS only, the hypothesized model produced an excellent fit: χ2(36) = 44.36, p = 0.16, CFI = 0.96, RMSEA = 0.05. For Chinese-Americans, (1) family communication was significantly associated with both PCS (β = 0.350; p = 0.01) and MCS (β = 0.470; p = 0.003); (2) family flexibility was neither directly nor indirectly associated with HRQOL; (3) social support mediated the relationship between family flexibility and family communication (Sobel = 2.86; p < 0.01); and (4) acculturation was directly related to PCS (β = 0.124; p = 0.044) and social support (β = 0.266; p = 0.003) (Table 3). The model accounted for 27 % of the variance in PCS and 26 % in MCS for Chinese-Americans.
Table 3.
Factor loadings and path coefficients between variables
| Parameter | Standardized beta coefficients |
|||
|---|---|---|---|---|
| Baseline model |
Path coefficient–constrained model |
|||
| Chinese (n = 86) |
Korean (n = 71) |
Chinese (n = 86) |
Korean (n = 71) |
|
| Factor loadings | ||||
| General communication → Family communication | 0.824*** | 0.862*** | 0.838*** | 0.863*** |
| Cancer-related communication → Family communication | 0.381** | 0.330* | 0.329*** | 0.387*** |
| Decisions with family → Family communication | 0.443nt | 0.417nt | 0.417nt | 0.455nt |
| Direct relations | ||||
| Acculturation → Social support | 0.266** | 0.246* | 0.288*** | 0.219*** |
| Family flexibility → Social support | 0.452*** | 0.188 | 0.409*** | 0.280*** |
| Family flexibility → Family communication | 0.208 | 0.402** | 0.335*** | 0.267*** |
| Social support → Family communication | 0.669*** | 0.627** | 0.579*** | 0.674*** |
| Family communication → PCS | 0.350* | 0.509** | 0.399*** | 0.407*** |
| Family communication → MCS | 0.470** | 0.559** | 0.491*** | 0.529*** |
| Acculturation → PCS | 0.124* | 0.085 | 0.109* | 0.098* |
| Comorbidities → PCS | −0.170** | −0.105 | −0.156*** | −0.152*** |
| Health insurance → PCS | −0.157* | −0.001 | −0.102* | −0.098* |
| Education → PCS | −0.143 | −0.203* | −0.200* | −0.082* |
| Education → MCS | −0.193* | −0.237* | −0.240** | −0.104** |
The baseline model shows the unconstrained path coefficients for each of the two groups; the path coefficient–constrained model shows parameter values when the path coefficients are equivalent between Chinese- and Korean-Americans
PCS physical component summary, MCS mental component summary
p<0.05;
p<0.01;
p<0.001
When estimated with Korean-American BCS only, the model also yielded an excellent fit: χ2(36) = 31.45, p = 0.69, CFI = 0.99, RMSEA = 0.01. In the Korean-American BCS group, (1) family communication was significantly associated with PCS (β = 0.509; p = 0.005) and MCS (β = 0.559; p = 0.003); (2) family flexibility was indirectly associated with HRQOL through family communication; (3) although social support was directly associated with family communication (β = 0.627; p = 0.002), it did not mediate the relationship between family flexibility and family communication (Sobel = 1.55; p > 0.05); and (4) acculturation was directly related to social support (β = 0.246; p = 0.025) (Table 3). The model predicted 35 and 37 % of the variance in PCS and MCS for Korean-Americans.
Overall, the baseline model demonstrated an excellent fit for the entire sample, including Chinese- and Korean-American BCS: χ2(72) = 75.80, p = 0.36, CFI = 0.99, RMSEA = 0.02. The factor loading–constrained model also yielded an excellent fit: χ2(76) = 75.08, p = 0.41, CFI = 0.99, RMSEA = 0.01. The chi-square difference test did not find significant differences between these models (Δχ2(4) = 2.28, p = 0.68), suggesting that the baseline model demonstrated measurement invariance across ethnicity. The path coefficient–constrained model also showed an excellent fit: χ2(85) = 87.35, p = 0.41, CFI = 0.99, RMSEA = 0.01. The standardized path coefficients for the path coefficient–constrained model for both the groups are provided in the Table 3. Although statistical differences in baseline parameters were noted between the two groups, chi-squared tests did not find significant differences between the path coefficient– and factor loading–constrained models (Δχ2(9) = 9.27, p = 0.41); the structural paths are equivalent by ethnicity.
Discussion
The current study examined the influence of family functioning and communication on HRQOL for Chinese- and Korean-American BCS. The results demonstrated that (1) family communication was directly associated with HRQOL for both groups; (2) family flexibility was indirectly associated with HRQOL through family communication for Korean-Americans only; (3) social support mediated the relationship between family flexibility and family communication for Chinese-Americans only; (4) acculturation was directly related to social support for both groups; and (5) the structural paths were equivalent between Chinese- and Korean-American BCS, although differences in baseline parameters were noted. Thus, the study’s hypotheses were partially supported in this study.
The study findings supported the conceptual framework describing the pathways that articulate how family functioning and community influence HRQOL for Chinese- and Korean-American BCS. As suggested in the Resilience Model, the current study found that family communication is directly associated with HRQOL and family flexibility is indirectly related to HRQOL. Moreover, social support mediated the relationship between family flexibility and family communication. In particular, acculturation was included to consider cultural vulnerability of Chinese- and Korean-Americas and showed significant relationships with social support and HRQOL. Although the Resilience Model is frequently used in family and coping studies, this model was not previously tested and applied specifically to Asian subpopulations. Therefore, this study is valuable in that findings demonstrated whether the Resilience Model is applicable to Chinese- and Korean-American BCS; thus, this study increases our understanding of how family flexibility, social support, and family communication may influence HRQOL within the cultural context.
One of the key findings involved the creation of the family communication latent factor warrants further elaboration. Indeed, communication is a dynamic component of the system consisting of factors such as listening, speaking, clarity, respect, and shared decision making [45]. For cancer survivors specifically, how to communicate about cancer with their family beyond the general communication may be their urgent need because the mutual understanding of cancer can be helpful in improving both the survivor’s and family’s adjustment to cancer [46, 47]. Additionally, shared decision making was included as one component of the family communication latent factor based on the definition of family communication. Shared decision making within the family can be effective to obtain health information through quality communication and ultimately result in a better quality of cancer care and increased satisfaction for survivors [48]. Given that the latent factor of family communication yielded a good fit to our data, the study finding provides an answer about the comprehensive meaning of family communication for cancer survivors in Chinese and Korean cultures.
However, we need to further investigate whether the family communication latent factor can be applied to other Asian ethnic groups. Asian-Americans are a very diverse population. They range from the poorly educated to those with graduate degrees, from countries where English is the official language to those where Asian languages are mostly spoken, and from less acculturated to highly acculturated [49]. Hence, in Asian-American families, the meaning of family and cancer communication may be influenced by cultural contexts such as acculturation, intergenerational gaps, spoken language, and educational levels [50, 51]. Defining the family communication latent factor within Asian-Americans’ social and cultural contexts may be helpful to fully understand family communication patterns in Asian cultures.
Several studies report that Asian culture emphasizes harmony and tends to discourage discussing emotional problems in public and even within the family [21, 52], suggesting that family communication may have negative relationship with HRQOL in Asian culture. However, our findings showed that positive family communication can contribute to improving HRQOL, consistent with other studies for most White populations [33, 46, 53]. It implies that the ability of BCS to effectively communicate to manage general and cancer-related concerns and to share their decisions with family members can provide the strengths to improve HRQOL. Therefore, our finding can be translated within the survivorship community and psychosocial care to assist BCS in effective family communication practices and suggests that culturally appropriate family communication intervention may serve to improve HRQOL for Chinese- and Korean-American BCS. For example, when a family is functioning rigidly, the development and implementation of family communication intervention which is applied to the rigid family may be effective to improve family HRQOL.
The notable differences in the results between Chinese- and Korean-Americans were found in the relationship between family flexibility and family communication through social support. Chinese-Americans showed the mediating effect of social support (indirect relationship between family flexibility and communication), whereas Korean-Americans did not (their direct relationship). This result may be explained by cultural contexts in the Chinese- and Korean-American groups. As indicated in the introduction section, we assumed that Chinese-Americans are more likely than Korean-Americans to be acculturated and consequently, Korean-Americans may have higher expectations toward their own families due to limited social networks compared to Chinese-Americans. The current study demonstrated that Chinese-Americans were more likely than Korean-Americans to be acculturated, although the current study samples showed a similar length of stay in the United States. Furthermore, the level of acculturation may in part explain how family functioning is associated with family communication. Given that positive relationship between acculturation and social support exists in both groups, the mediating effect of social support in the relationship between family flexibility and communication for Chinese-Americans indicates that family functioning is particularly influenced by the availability of social support in the acculturated group. Hence, our finding suggests that understanding of the relationship among acculturation, family flexibility, social support, and family communication should be addressed within a cultural context.
The multigroup analysis did not find significant differences between unconstrained and constrained models, suggesting that the overall framework is equivalent across the two groups. Based on this finding, we can claim that the Resilience Model is applicable to Chinese- and Korean-American BCS. At the same time, however, we should not overlook that differences in the paths were noted between the two groups, as shown in the baseline model of Table 3. For example, the relationships between family flexibility and communication and between acculturation and PCS showed different patterns between the two groups. Therefore, this study provides important practical information on how to intervene on family flexibility, social support, family communication, and HRQOL with Chinese- and Korean-Americans. For example, an approach to extend social support resources may be effective in ultimately improving HRQOL for Chinese-Americans. For Korean-Americans, a family communication intervention with increased family flexibility may positively influence HRQOL. Hence, this study provides evidence supporting the importance of a disaggregated approach to Asian-American subgroups.
Several limitations of the study should be noted. First, because we relied on self-report measures, the findings may be influenced by recall bias. Second, the cross-sectional design does not adequately assess causality among variables. For example, unlike our proposed model, family communication may influence social support; thus, results should be interpreted with caution. Additionally, a longitudinal study will be necessary to fully understand these dynamic relationships. Third, this study included BCS only. Future studies should include family members to enhance our understanding of communication and coping within the family. Fourth, although we included some demographic and medical characteristics as control variables, we did not fully explore their impact on predictors and outcomes. Future study is required to develop and test a comprehensive model including individual, family, and medical characteristics with large sample size. Finally, our sample sizes were not large enough to detect a large effect size in this study; such that findings may not be generalized.
The findings of the current study further increase our knowledge of family flexibility, social support, family communication, and HRQOL in a cultural context. From a clinical perspective, this study suggests that the role of family communication on HRQOL may be a relatively important and positive area for adjustment in ethnic minorities. This study also highlights the importance of family flexibility within the BCS’s family. From a research perspective, the findings support the need for population-based, methodologically strong approaches to ethnic minority population research. Future efforts to achieve clinical and research goals may have benefits in reducing the burden of cancer among ethnic minority populations.
Acknowledgments
Funding for this research was supported by a grant from the NIH/NCI 1R03CA139941.
Abbreviations
- BCS
Breast cancer survivors
- CFI
Comparative Fit Index
- FACES
Family Adaptability and Cohesion Evaluation Scales
- HRQOL
Health-related quality of life
- MCS
Mental component summary
- PCS
Physical component summary
- RMSEA
Root mean square error of approximation
- SEM
Structural equation modeling
- SF-36
The RAND 36-item health survey
Contributor Information
Jung-won Lim, Mandel School of Applied Social Sciences, Case Western Reserve University, 10900 Euclid Avenue, Cleveland, OH 44106, USA.
Kimlin T. Ashing-Giwa, Department of Population Sciences, Center of Community Alliance for Research and Education (CCARE), City of Hope National Medical Center, 1500 East Duarte Road, Duarte, CA 91010, USA kashing@coh.org
References
- 1.American Cancer Society . Cancer facts and figures 2006. American Cancer Society; Atlanta: 2006. [Google Scholar]
- 2.Clegg LX, Li FP, Hankey BF, Chu K, Edwards BK. Cancer survival among U.S. whites and minorities: A SEER program population-based study. Archives of Internal Medicine. 2002;162:1985–1993. doi: 10.1001/archinte.162.17.1985. [DOI] [PubMed] [Google Scholar]
- 3.Kim J, Ashing-Giwa K, Kagawa-Singer M, Tejero JS. Breast cancer among Asian Americans: Is acculturation related to health-related quality of life? Oncology Nursing Forum. 2006;33(6):E90–E99. doi: 10.1188/06.ONF.E90-E99. [DOI] [PubMed] [Google Scholar]
- 4.Ashing-Giwa KT, Padilla G, Tejero J, Kagawa-Singer M. Understanding the breast cancer experience of Asian American women. Psycho-Oncology. 2003;12(1):38–58. doi: 10.1002/pon.632. [DOI] [PubMed] [Google Scholar]
- 5.Barnes JS, Bennett CE. The Asian population: 2000. Census 2000 brief. 2002.
- 6.Srinivasan S, Guillermo T. Toward improved health: disaggregating Asian American and Native Hawaiian/Pacific Islander data. American Journal of Public Health. 2000;90(11):1731–1734. doi: 10.2105/ajph.90.11.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mui AC, Shibusawa T. Asian American elders in the twenty-first century: Key indicators of well-being. Columbia University Press; New York: 2008. [Google Scholar]
- 8.Lim J, Yi J, Zebrack B. Acculturation, social support, and quality of life for Korean immigrant breast and gynecological cancer survivors. Ethnicity & Health. 2008;13(5):1–18. doi: 10.1080/13557850802009488. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Census Bureau 2010 American Community Survey. 2011 Available at http://www.census.gov/
- 10.Cella DF, Tulsky DS. Quality of life in cancer: Definition, purpose, and method of measurement. Cancer Investigation. 1993;11(3):327–336. doi: 10.3109/07357909309024860. [DOI] [PubMed] [Google Scholar]
- 11.Ware JE. Conceptualizing disease impact and treatment outcomes. Cancer. 1984;53(10 Suppl):2316–2326. doi: 10.1002/cncr.1984.53.s10.2316. [DOI] [PubMed] [Google Scholar]
- 12.Ashing-Giwa KT, Tejero JS, Kim J, Padilla GV, Hellemann G. Examining predictive models of HRQOL in a population-based, multiethnic sample of women with breast carcinoma. Quality of Life Research. 2007;16(3):413–428. doi: 10.1007/s11136-006-9138-4. [DOI] [PubMed] [Google Scholar]
- 13.Lim J, Zebrack B. Different pathways in social support and quality of life between Korean American and Korean breast and gynecological cancer survivors. Quality of Life Research. 2008;17:679–689. doi: 10.1007/s11136-008-9343-4. [DOI] [PubMed] [Google Scholar]
- 14.Ashing-Giwa KT, Padilla GV, Tejero JS, Kim J. Breast cancer survivorship in a multiethnic sample: Challenges in recruitment and measurement. Cancer. 2004;101(3):450–465. doi: 10.1002/cncr.20370. [DOI] [PubMed] [Google Scholar]
- 15.Northouse L, Walker J, Schafenacker A. A familybased program of care for women with recurrent breast cancer and their family members. Oncology Nursing Forum. 2002;29:1411–1419. doi: 10.1188/02.ONF.1411-1419. [DOI] [PubMed] [Google Scholar]
- 16.Olson DH. Circumplex model of marital and family systems. Journal of Family Therapy. 2000;22:144–167. [Google Scholar]
- 17.Hilton BA, Koop PM. Family communication pattern in coping with early breast cancer. Western Journal of Nursing Research. 1994;16(4):366–391. doi: 10.1177/019394599401600403. [DOI] [PubMed] [Google Scholar]
- 18.Cordova MJ, Cunningham LL, Carlson CR, Andry-kowski MA. Social constraints, cognitive processing, and adjustment to breast cancer. Journal of Consulting and Clinical Psychology. 2001;69:706–711. [PubMed] [Google Scholar]
- 19.Black K, Lobo M. A conceptual review of family resilience factors. Journal of Family Nursing. 2008;14:33–55. doi: 10.1177/1074840707312237. [DOI] [PubMed] [Google Scholar]
- 20.Morse SR, Fife B. Coping with a partners’ cancer: Adjustment at four stages of the illness trajectory. Oncology Nursing Forum. 1998;25:751–760. [PubMed] [Google Scholar]
- 21.McCollaum B, Lester D. Locus of control, depression and suicidality in Korean workers. Psychological Reports. 1997;80:1282. doi: 10.2466/pr0.1997.80.3c.1282. [DOI] [PubMed] [Google Scholar]
- 22.Flores E, Tschann JM, VanOss Marin B, Pantoja P. Marital conflict and acculturation among Mexican American husbands and wives. Cultural Diversity & Ethnic Minority Psychology. 2004;10:39–52. doi: 10.1037/1099-9809.10.1.39. [DOI] [PubMed] [Google Scholar]
- 23.Figley CR. Treating stress in families. Brunner/Mazel; New York: 1989. [Google Scholar]
- 24.Radina ME, Armer JM. Surviving breast cancer and living with lymphedema: Resiliency among women in context of their families. Journal of Family Nursing. 2004;10(4):485–505. [Google Scholar]
- 25.Choenarom C, Williams RA, Hagerty BM. The role of sense of belonging and social support on stress and depression in individuals with depression. Archieves of Psychiatric Nursing. 2005;19(1):18–29. doi: 10.1016/j.apnu.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 26.McCubbin M, McCubbin HI. Families coping with illness: The resiliency model of family stress, adjustment, and adaptation. University of Wisconsin-Madison; Madison, WI: 1993. [Google Scholar]
- 27.McCubbin HI, McCubbin MA. Research utilization in social work practice of family treatment. In: Grasso AJ, Epstein I, editors. Research utilization in the social sciences: Innovations for practice and administration. Haworth; New York, NY: 1992. [Google Scholar]
- 28.McCubbin MA, McCubbin HI. Families coping with illness: The Resiliency Model of Family Stress, Adjustment, and Adaptation. In: Danielson C, Hamel-Bissell B, Winstead-Fry, editors. Families, health, and illness. Mosby; New York, NY: 1993. pp. 21–63. [Google Scholar]
- 29.McCubbin MA, McCubbin HI. Resiliency in families: A conceptual model of family adjustment and adaptation in response to stress and crises. In: McCubbin HI, Thompson AI, McCubbin MA, editors. Family assessment: Resiliency, coping and adaptation: Inventories for research and practice. University of Wisconsin; Madison, WI: 1996. pp. 1–64. [Google Scholar]
- 30.McCubbin M, Balling K, Possin P, Frierdich S, Bryne B. Family resiliency in childhood cancer. Family Relations. 2002;51:103–111. [Google Scholar]
- 31.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: Manual and interpretation guide. Health Institute, New England Medical Center; Boston: 1993. [Google Scholar]
- 32.Olson DH, Gorall DM, Tiesel JW. FACES IV package. Life Innovations; Minneapolis, MN: 2004. [Google Scholar]
- 33.Mallinger JB, Griggs JJ, Shields CG. Family communication and mental health after breast cancer. European Journal of Cancer. 2006;15:355–361. doi: 10.1111/j.1365-2354.2006.00666.x. [DOI] [PubMed] [Google Scholar]
- 34.Olson DH. Circumplex model VII: Validation studies and FACES III. Family Process. 1986;25(3):337–351. doi: 10.1111/j.1545-5300.1986.00337.x. [DOI] [PubMed] [Google Scholar]
- 35.Sherbourne CD, Stewart AL. The MOS social support survey. Social Science and Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 36.Chung RH, Kim BK, Abreu JM. Asian American multidimensional acculturation scale: Development, factor analysis, reliability, and validity. Cultural Diversity and Ethnic Minority Psychology. 2004;10(1):66–80. doi: 10.1037/1099-9809.10.1.66. [DOI] [PubMed] [Google Scholar]
- 37.Enders C, Bandalos D. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8(3):430–457. [Google Scholar]
- 38.Schumacker RE. Conducting specification searches with Amos. Structural Equation Modeling. 2006;13(1):118–129. [Google Scholar]
- 39.Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 40.Bentler PM. Comparative fix indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 41.Kline R. Principles and practice of structural equation modeling. Guilford Press; New York: 1998. [Google Scholar]
- 42.Wu AD, Li Z, Zumbo BD. Decoding the meaning of factorial invariance and updating the practice of multi-group confirmatory factor analysis: A demonstration with TIMSS data. Practice Assessment, Research & Evaluation. 2007;12(3):1–26. [Google Scholar]
- 43.Bentler PM. On tests and indices for evaluating structural models. Personality and Individual Differences. 2007;42:825–829. [Google Scholar]
- 44.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociological methodology. Jossey-Bass; San Francisco: 1982. pp. 290–312. [Google Scholar]
- 45.Hultquist AK. Psychological type and family functioning exploring the interface between the self and the system. Journal of Systemic Therapies. 2002;21(2):90–108. [Google Scholar]
- 46.Zhang AY, Siminoff LA. Silence and cancer: Why do families and patients fail to communicate? Health Communication. 2003;15(4):415–429. doi: 10.1207/S15327027HC1504_03. [DOI] [PubMed] [Google Scholar]
- 47.Kilpatrick MG, Kristjanson LJ, Tataryn DJ, Fraser VH. Information needs of husbands of women with breast cancer. Oncology Nursing Forum. 1998;25:1595–1601. [PubMed] [Google Scholar]
- 48.Edwards A, Elwyn G. Shared decision-making in health care: Achieving evidence-based patient choice. Oxford University Press; New York: 2009. [Google Scholar]
- 49.Leu J, Walton E, Takeuchi D. Contextualizing acculturation: Gender, family, and community reception influences on Asian immigrant mental health. American Journal of Community Psychology. 2011;48:168–180. doi: 10.1007/s10464-010-9360-7. [DOI] [PubMed] [Google Scholar]
- 50.Kim M, Park IJK. Testing the moderating effect of parent-adolescent communication on the acculturation gap-distress relation in Korean American families. Journal of Youth Adolescence. 2011;40:1661–1673. doi: 10.1007/s10964-011-9648-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hwang W. Acculturative family distancing: theory, research, and clinical practice. Psychotherapy: Theory, Research, and Practice. 2006;43(4):397–409. doi: 10.1037/0033-3204.43.4.397. [DOI] [PubMed] [Google Scholar]
- 52.Ritsner M, Ponizovsky A, Kurs R, Modai I. Somatization in an immigrant population in Israel: A community survey of prevalence, risk factors, and help-seeking behavior. American Journal of Psychiatry. 2000;157(3):385–392. doi: 10.1176/appi.ajp.157.3.385. [DOI] [PubMed] [Google Scholar]
- 53.Bodenmann G. Dyadic coping and its significant for marital functioning. In: Revenson T, Kayser K, Bodenmann G, editors. Couples coping with stress: Emerging perspectives on dyadic coping. American Psychological Association; Washington, DC: 2005. pp. 33–50. [Google Scholar]