Abstract
Background:
Hyponatremia is the most common electrolyte abnormality seen in patients with aneurysmal SAH. Clinically significant hyponatremia (Serum Sodium <131 mEq/L) which needs treatment, has been redefined recently and there is a paucity of outcome studies based on this. This study aims to identify the mean Serum Sodium (S.Na+) level and its duration among inpatients with SAH and to identify the relationship between hyponatremia and the outcome status of patients undergoing surgery for SAH.
Materials and Methods:
This outcome study is undertaken in the department of neurosurgery, The Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, Kerala. Medical records of all patients with SAH from 1st January to 31st July 2010 were reviewed. Preoperative status was assessed using World Federation of Neurosurgical Societies (WFNS) grading system. Discharge status was calculated using the Glasgow outcome score scale.
Results:
Fifty nine patients were included in the study and 53 (89.8%) of them have undergone surgical treatment. Hyponatremia was observed in 22 of 59 patients (37%). The mean Sodium level of hyponatremic patients was 126.97 mEq/L for a median duration of two days. Glasgow outcome score was good in 89.8% of patients. We lost two patients, one of whom had hyponatremia and vasospasm.
Conclusion:
Hyponatremia is significantly associated with poor outcome in patients with SAH. Anticipate hyponatremia in patients with aneurysmal subarachnoid hemorrhage, timely detect and appropriately treat it to improve outcome. It is more common in patients who are more than 50 years old and whose aneurysm is in the anterior communicating artery. Our comprehensive monitoring ensured early detection and efficient surgical and nursing management reduced morbidity and mortality.
Keywords: Aneurysmal subarachnoid hemorrhage, hyponatremia, neurosurgical, outcome
Introduction
Clinically significant hyponatremia among neurosurgical patients, which needs treatment, has been redefined recently as a Serum Sodium of <131 mEq/L.[1] Hyponatremia after subarachnoid hemorrhage (SAH) has prevalence rates of approximately 30-55%.[2–4] Whether caused by syndrome of inappropriate antidiuretic hormone (SIADH) or cerebral salt waste syndrome (CSW), hyponatremia in patients with SAH has a clear association with increased morbidity including cerebrovascular spasm.[1,3] The complications associated with hyponatremia in neurosurgical patients viz. cerebral edema, seizures, or death may also arise from very slow or fast correction of hyponatremia.[1] Hyponatremia, even when mild, is associated with increased mortality.[5,6] When hyponatremia is treated promptly and appropriately, patients’ sodium levels return to normal without detrimental effects. Nurses at the bedside should neither miss diagnostic clues nor provide inappropriate care. This study is undertaken to identify the mean Serum Sodium (S.Na+) level and its duration among inpatients with SAH and to identify the relationship between hyponatremia and the outcome status of patients undergoing surgery for SAH.
Materials and Methods
This study was conducted by performing a retrospective review of medical records of patients with aneurysmal SAH, who were admitted to the neurosurgical intensive care unit (NSICU) of a tertiary level referral hospital, located in Thiruvananthapuram, Kerala, between 1st January and 31st July 2010. The medical records of these patients were reviewed with due permission from the departments concerned and the data were retrieved exclusively by the first author. Patients who were later diagnosed to have nonaneurysmal bleeding were excluded (three patients). Triple ‘H’ therapy (Hemodilutional, Hypertensive, and Hypovolemic therapy) and Nimodipine protocol is practiced in this department for patients admitted with aneurysmal SAH as follows.
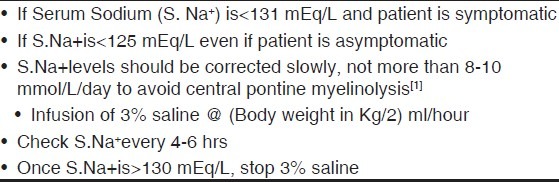
Nimodipine 60 mg (Tablet) is given Q4h from admission onwards and continued for 21 days. In some patients, Inj. Nimodipine 1-2 gm/hr intravenously is given on the day of surgery to a maximum of 30 gm. Sodium levels are routinely checked at 9 pm on the day of surgery, at 6am daily during postoperative period, every 4-6 hours if patient is getting intravenous saline (3%) and whenever there is polyurea or a change in mental status. Hence there is no chance that hyponatremia went unrecognized in any patients.
Hyponatremia and management
Hyponatremia is classically defined as a Serum Sodium concentration level of less than 135 mEq/L (<135 mmole/L, SI). However; clinically significant hyponatremia (i.e., Serum Sodium <131 mEq/L OR <131 mmole/L1) requires further investigation and treatment. The latter clinical definition is used to detect hyponatremia in the present study. Hyponatremia following subarachnoid hemorrhage occurs due to the inappropriate secretion of antidiuretic hormone (SIADH). However; it is also associated with certain dehydration states.[7] Fluid restriction to correct hyponatremia appears to be potentially dangerous in patients with aneurysmal subarachnoid hemorrhage, especially in the latter category.[8] Accordingly, the management modality followed in our setting is given in Tables 1 and 2.
Table 1.
Management of hyponatremia.is it SIADH or CSW?
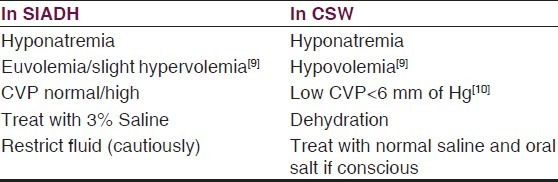
Table 2.
Treatment of hyponatremia using 3% saline
Data were collected using a proforma developed by the investigator that included demographic variables, preexisting hypertension, diagnostic investigations done, results and treatment given, occurrence of hyponatremia, its duration and management, delay in reaching the hospital from onset of symptoms, delay in surgery from day of admission, duration of ICU stay and hospital stay, days on mechanical ventilator, and complications developed. Pre operative status was assessed using the World Federation of Neurosurgical Societies (WFNS) grade. Discharge status was calculated using the Glasgow outcome scale (GOS) as good outcome (5 = full recovery, 4 = moderate disability independent but has neurological or intellectual impairment), or poor outcome (3 = severely disabled, conscious but totally dependent, 2 = vegetative survival, and 1 = dead). When S.Na+ was determined more than once a day, daily mean values were used for analysis.
Chi-square tests or Fisher's exact tests were done to assess statistical significance of the difference in percentages. Spearman's rank correlation was used to assess the strength of association between the preoperative WFNS grade and the Glasgow outcome score. Multivariate analysis was attempted by a multiple logistic regression model with discharge status as the outcome; and the independent predictor variables were hyponatremia, age and duration of ICU stay. P value of 0.05 or less was the criterion used to conclude statistical significance. All statistical analyses were done using SPSS Statistics for Windows 17.0 (Chicago, Illinois).
Results
The medical records of 62 patients who were admitted to the NSICU with a diagnosis of Aneurysmal SAH, during the study period were reviewed. Three patients who were later diagnosed with arteriovenous malformation were excluded. The age of the sample (n = 59) ranged from 28 to 76 years (mean, 50.5 years). There were almost equal number of males (n = 30) and females (n = 29). Preexisting hypertension was present in 23 (39%) of them. Thirty four patients (57.6%) had undergone a CT angiogram (CTA), which was the most common diagnostic investigation performed for these patients. CTA and/or digital subtraction carotid angiogram (DSA) were performed in another 19 (32.2%), and magnetic resonance imaging (MRI) was done in six (10.2%) patients. DSA was positive in 57 patients and negative in the remaining two. The locations of the aneurysms of the 57 patients were as follows : Anterior communicating artery (n = 21), middle cerebral artery (n = 9), internal carotid artery communicating/ophthalmic segment (n = 14), posterior communicating artery (n = 9) and multiple aneurysms (n = 4).
The mean delay in reaching this institute from onset of symptoms was 26.5 days with a range of zero days to one year and a median of eight days. The preoperative neurologic grade of SAH according to the WFNS classification scheme was grade I for 44 patients, grade II for seven patients, grade III for four patients and grade IV for four patients. Fifty-three patients underwent surgery, mostly clipping of aneurysm. The mean delay in surgery from day of admission was 2.8 days with a range of one to 12 days, and a median of two days. Twenty two of the 53 patients (41.5%) had undergone surgery, the very next day of admission. Fifty patients underwent clipping of aneurysm, one patient was treated with wrapping of aneurysm whereas two others had undergone superficial temporal artery to middle cerebral artery bypass (STA-MCA bypass). Of the remaining six patients, two patients got discharged since DSA was negative for aneurysm, two patients were referred to our Imaging Sciences and Interventional Radiology department for coiling, one patient's surgery was deferred due to severe vasospasm, and one patient who had multiple aneurysm died due to rebleeding. Standard care now for SAH is endovascular coiling first, based on the International Subarachnoid Aneurysm Trial (ISAT) results.[11] However, due to reasons of cost, neurosurgical clipping is the practice followed in this institute.
Hyponatremia was observed in 22 of the 59 (37%) patients. The mean S.Na+ level was 126.97 mEq/L, with a range of 115-131 mEq/L. The duration of hyponatremia ranged from one to nine days with a median of two days. Fourteen patients (63.6%) were treated with 3% hypertonic saline and the remaining 8 (36.4%) were treated with 0.9% normal saline and extra table salt (sodium chloride) in diet. Hyponatremia was seen more in patients with anterior communicating artery aneurysm, 11 of 21 (52.4%) followed by three of nine (33.3%) each in case of middle cerebral artery aneurysm as well as posterior communicating artery aneurysm. Hyponatremia was comparatively less among patients with internal carotid artery aneurysm and multiple aneurysms, five out of 18 (27.7%).
The mean duration of ICU stay was 6.9 days with a range of one to 18 days, and median six days. The mean duration of hospital stay was 11.4 days with a range of one to 28 days and the median was ten days. Eight patients required mechanical ventilation with a mean duration of 2.9 days with a range of one to seven days. All of them had good outcomes at discharge : Two had full recovery and six had moderate disability at the time of discharge.
The surgical outcome of all patients at the time of discharge was assessed according to Glasgow Outcome Scale as having a good outcome (full recovery in 40 patients, moderate disability in 13 patients), or poor outcome (severe disability in four patients (hyponatremic), death in two patients). Among the six patients with poor outcome, five had hyponatremia. The association between hyponatremia and poor outcome was statistically significant (P = 0.023) [Table 3]. The GOS is moderately correlated with the preoperative WFNS grade (r = 0.41, P = 0.001). The cause of death was rebleeding (normal S.Na+) in one patient and aortoiliac dissection in another patient (hyponatremic).
Table 3.
Association between hyponatremia and Glasgow outcome scale
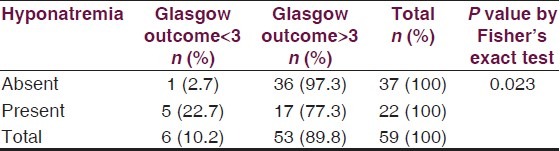
Selected demographic variables and baseline characteristics were compared between the groups with and without hyponatremia. There was no difference in occurrence of hyponatremia between males and females (P = 0.288), presence or absence of hypertension (P = 0.582), location of aneurysm in the Anterior communicating artery or elsewhere (P = 0.158), early surgery within two days or later (P = 1.00), or preoperative WFNS grade <II or more (P = 0.537). However; old age (>50 years) was significantly associated with hyponatremia (P = 0.003). Though hyponatremia was not associated with longer duration (>median 10 days) of hospital stay (P = 0.06), it was significantly associated with a longer duration (>median 6 days) of ICU stay (P = 0.014). Moreover, the association between poor outcome and hyponatremia, adjusted for age and ICU stay (the significant variables) was found to be significant (Odds Ratio (OR) 14.78, 95% Confidence interval 1.12, 195.12, P = 0.041). The vey wide confidence interval is mainly due to small sample size.
Discussion
Hyponatremia is frequently observed during the acute phase after aneurysmal SAH. The incidence of hyponatremia (<131 mEq/L) observed in the present series (37%) lies within the reported prevalence rate of hyponatremia (<135 mEq/L) after subarachnoid hemorrhage.[2–4] However, Kao et al., reported a higher incidence (59.2%)of hyponatremia (135 mEq/L) and lower incidence (15.2%) of moderate to severe hyponatremia (<130 mEq/L) than the present study.[12] Majority of the patients (63.6%) were treated with 3% saline since they had SIADH as the cause of hyponatremia. SIADH was found to be the most frequent cause of severe hyponatremia among patients with aneurysmal SAH in earlier studies.[12,13] Hyponatremia was associated with an increased duration of hospital stay in earlier studies.[12,13] However, such association was not found in the present study, though hyponatremia was significantly associated with a longer duration of ICU stay.
Among hyponatremic patients, 22.7% had poor outcome, as per GOS, either severe disability or death. No patients were in vegetative state. This rate is less than the reported poor outcome (32%) among hyponatremic patients with aneurysmal subarachnoid hemorrhage.[4] In the present study, hyponatremia was significantly associated with poor outcome at discharge even after adjusting for age and ICU stay (the significant variables). Those patients with aneurysmal SAH who developed hyponatremia were 14.78 times more likely to develop poor outcome. Qureshi et al., in a prospective study of patients with SAH demonstrated poor outcome at three months in hypernatremic patients (odds ratio, 2.7;95% confidence interval, 1.2-6.1). However, hyponatremia (S.Na + <135 mEq/L) was not associated with poor outcomes at three months.[4,14] Wijdicks et al., reported significant and fatal cerebral infarction among hyponatremic patients with aneurysmal subarachnoid hemorrhage, which might cause poor outcome.[8] In patients with SAH, hyponatremia was associated with a significantly greater risk of developing cerebrovascular spasm (CVS).[3] Advanced age, smoking, hyponatremia, rebleeding, and cerebral vasospasm were independent risk factors causing death of patients with subarachnoid hemorrhage.[6] Even mild hyponatremia (130-134 mEq/L) was independently associated with a higher risk of in-hospital and long-term mortality in patients admitted for orthopedic surgical procedures.[5] These morbidities or mortality were not studied in the present study. However, we had two deaths, in which one had hyponatremia and the other had rebleeding; both were independent risk factors causing death of patients with subarachnoid hemorrhage.[6]
The correlation between preoperative WFNS grade and postoperative GOS score was moderate and about 0.4, but statistically significant. The lower the WFNS grade the better the GOS and vice versa underscoring the importance of early hospitalization and early surgery.
The limitation of our study is that it is a retrospective study at a single institute. Being a tertiary level referral institute, many patients have reached the institute many days/months after the initial symptoms. However, all the patients were managed systematically as per protocol contributing to the good outcome.
Conclusion
Hyponatremia occurs in more than one third of patients with aneurysmal SAH and is associated with poor outcome. Though a treatable condition, it increases the morbidity in these patients. While treating these patients, differentiating between SIADH and CSW is essential. Aetiology and treatment for hyponatremia varies in the presence of hypervolemia/Euvolemia or hypovolemia. The neurosurgical team should be able to anticipate hyponatremia in aneurysmal SAH especially in patients who are more than 50 years old, and provide effective treatment for this reversible, but potentially dangerous condition.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Rahman M, Friedman WA. Hyponatremia in neurosurgical patients: Clinical guidelines development. Neurosurg. 2009;65:925–35. doi: 10.1227/01.NEU.0000358954.62182.B3. [DOI] [PubMed] [Google Scholar]
- 2.Sherlock M, O’Sullivan E, Agha A, Behan LA, Rawluk D, Brennan P, et al. The incidence and pathophysiology of hyponatraemia after subarachnoid hemorrhage. Clin Endocrinol. 2006;64:250–4. doi: 10.1111/j.1365-2265.2006.02432.x. [DOI] [PubMed] [Google Scholar]
- 3.Chandy D, Sy R, Aronow WS, Lee WN, Maguire G, Murali R. Hyponatremia and cerebrovascular spasm in aneurysmal subarachnoid hemorrhage. Neurol India. 2006;54:273–5. doi: 10.4103/0028-3886.27151. [DOI] [PubMed] [Google Scholar]
- 4.Qureshi AI, Suri MF, Sung GY, Straw RN, Yahia AM, Saad M, et al. Prognostic significance of hypernatremia and hyponatremia among patients with aneurysmal subarachnoid hemorrhage. Neurosurgery. 2002;50:749–55. doi: 10.1097/00006123-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Waikar SS, Mount DB, Curhan GC. Mortality after Hospitalization with Mild, Moderate, and Severe Hyponatremia. Am J Med. 2009;122:857–65. doi: 10.1016/j.amjmed.2009.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu G, Zhu F, Wang Y, He G, Hu J, Wang X, et al. A historic cohort study on the survival rate and the correlated risk factors regarding 174 patients with subarachnoid hemorrhage. Neurosurg Quart. 2010;20:136–41. [PubMed] [Google Scholar]
- 7.Kurokawa Y, Uede T, Ishiguro M, Honda O, Honmou O, Kato T, et al. Pathogenesis of hyponatremia following subarachnoid hemorrhage due to ruptured cerebral aneurysm. Surg Neurol. 1996;46:500–7. doi: 10.1016/s0090-3019(96)00034-1. [DOI] [PubMed] [Google Scholar]
- 8.Wijdicks EF, Vermeulen M, Hijdra A, van Gijn J. Hyponatremia and cerebral infarction in patients with ruptured intracranial aneurysms: Is fluid restriction harmful? Ann Neurol. 1985;17:137–40. doi: 10.1002/ana.410170206. [DOI] [PubMed] [Google Scholar]
- 9.Palmer BF. Hyponatraemia in a neurosurgical patient : Syndrome of inappropriate antidiuretic hormone secretion versus cerebral salt wasting. Nephrol Dial Transplant. 2000;15:262–8. doi: 10.1093/ndt/15.2.262. [DOI] [PubMed] [Google Scholar]
- 10.Damaraju SC, Rajshekhar V, Chandy MJ. Validation study of a central venous pressure-based protocol for the management of neurosurgical patients with hyponatremia and natriuresis. Neurosurgery. 1997;40:312–6. doi: 10.1097/00006123-199702000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms : Arandomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366:809–17. doi: 10.1016/S0140-6736(05)67214-5. [DOI] [PubMed] [Google Scholar]
- 12.Kao L, Al-Lawati Z, Vavao J, Steinberg GK, Katznelson L. Prevalence and clinical demographics of cerebral salt wasting in patients with aneurysmal subarachnoid hemorrhage. Pituitary. 2009;12:347–51. doi: 10.1007/s11102-009-0188-9. [DOI] [PubMed] [Google Scholar]
- 13.Benvenga S. What is the pathogenesis of hyponatremia after subarachnoid hemorrhage? Nat Clin Pract Endocrinol Metab. 2006;2:608–9. doi: 10.1038/ncpendmet0302. [DOI] [PubMed] [Google Scholar]
- 14.Zheng B, Qiu Y, Jin H, Wang L, Chen X, Shi C, et al. A predictive value of hyponatremia for poor outcome and cerebral infarction in high-grade aneurysmal subarachnoid hemorrhage patients. J Neurol Neurosurg Psychiatry. 2011;82:213–7. doi: 10.1136/jnnp.2009.180349. [DOI] [PubMed] [Google Scholar]


