Abstract
A pregnant woman, who had been suffering from hyperemesis gravidarum, presented with alteration of consciousness, ocular nystagmus and ataxia. Magnetic Resonance Imaging of the brain showed typical findings of Wernicke's encephalopathy and central pontine myelinolysis. The clinical features responded dramatically to thiamine supplementation.
Keywords: Central pontine myelinolysis, hyperemesis gravidarum, Wernicke's encephalopathy
Introduction
The combination of Wernicke's encephalopathy and central pontine myelinolysis in pregnancy with hyperemesis gravidarum is considered as a rare condition. We report the case of a pregnant woman with hyperemesis gravidarum who had classic clinical features and typical Magnetic resonance imaging (MRI) findings of Wernicke's encephalopathy, with additional features of central pontine myelinolysis (CPM) on the scan.
Case Report
A 21-year-old woman with 16 weeks pregnancy was admitted because of progressive difficulty in walking for 3 weeks. She had a weight loss of 12 kg after conceiving due to hyperemesis gravidarum. Due to hyperemesis, she could only eat sweet red jelly. Also, she had been drinking domestic whisky since she was 16 years of age. She had no alcohol dependent symptoms and signs, and she quitted alcohol immediately after knowing about her pregnancy. On admission, she was lethargic, and responded slowly to verbal commands.
Very prominent nystagmus was seen in the upbeat direction, and was prominent in all other directions. Limbs and truncal ataxia with ataxic gait were present. Mild proximal muscle weakness (grade 4/5) was noted. However, deep tendon reflexes were within the normal range. Thyroid function test was within the normal range, serum sodium was 135 mmol/L (normal range 135-145 mmol/L), potassium was 1.9 mmol/L (normal range 3.5-5.0 mmol/L), sodium bicarbonate was 31.5 mmol/L (normal range 21-32 mmol/L), phosphate was 3.2 mg/dL (normal range 2.5-4.9 mg/dL), and magnesium was 1.5 mg/dL (normal range 1.8-2.4 mg/dL). Magnetic resonance imaging (MRI) of the brain showed hypersignal intensity at the bilateral medial thalamus on diffusion weighted imaging (DWI), Fluid attenuated inversion recovery (FLAIR), and T2Weighted (T2W) series [Figure 1]. MRI of the brain also showed hypersignal intensity at central pons on the DWI, FLAIR, and T2W series [Figure 2]. Wernicke's encephalopathy with CPM was diagnosed. After three days of thiamine supplementation, her clinical features significantly improved. Hyperemesis gravidarum was managed by rehydration, corrected imbalance electrolytes (especially hypokalemia and hypomagnesemia), and antiemetic medications such as intravenous dimenhydranate. Last follow up at 2 months after discharge from the hospital demonstrated improvement in her conditions and normal findings, except for the presence ofmild vertical nystagmus. As she received antenatal care from another hospital, we did not have information about the pregnancy outcome.
Figure 1.
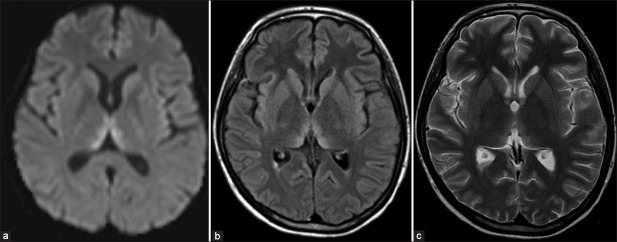
Magnetic resonance imaging of brain showed hypersignal intensity at bilateral medial thalamus on diffusion weighted imaging (a) Fluid attenuated inversion recovery (b) and T2Weighted (c) Series
Figure 2.
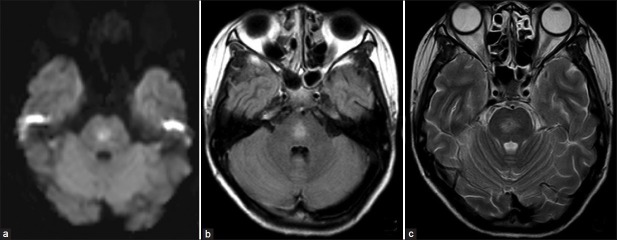
Magnetic resonance imaging of brain showed hypersignal intensity at central pons on diffusion weighted imaging (a) Fluid attenuated inversion recovery (b) and T2Weighted (c) Series
Discussion
Wernicke's encephalopathy is an acute, neuropsychiatric syndrome, characterized by nystagmus and/or ophthalmoplegia, mental status changes, and ataxic gait. It is an uncommon complication in hyperemesis gravidarum subsequent from the combination of poor nutritional status, frequent vomiting, and increased metabolic requirements of pregnancy.[1]
Deficiency of vitamin B1 is the main cause of this condition. Thiamine pyrophosphate, the biological active form of the vitamin, is an essential coenzyme in many biochemical pathways in the brain, including transketolase, alpha-ketoglutarate dehydrogenase, and pyruvate dehydrogenase.[2] Thiamine requirements depend on tissue metabolic rate. Depletion of thiamine initiates neuronal injury by inhibiting metabolism in brain regions with high metabolic requirements and high thiamine turnover.[3] Time to deplete the body's store of thiamine is about 3 weeks, and if the vitamin levels are not restored even after this period, impaired functioning of the enzymes requiring thiamine pyrophosphate occurs. Thiamine is absorbed in the duodenal part of the small intestine, and transported through the blood brain barrier by both passive and active mechanisms which allows for a rapid correction of the brain thiamine deficiency.[4] The daily requirement of thiamine varieswith the age and sex, 1.1 mg/day for females and an increased requirement of1.4-1.5 mg/day, particularly during pregnancy and lactation.[5]
If Wernicke's encephalopathy is suspected, treatment with thiamine, intravenously or intramuscularly, should be initiated immediately, and continued until a normal diet is resumed. Currently, there is no consensus about the optimal daily dose of thiamine treatment. Guidelines by the European Federation of Neurological Societies (EFNS) recommend that thiamine should be given 200 mg thrice daily via the intravenous route, before any carbohydrate, until there is no further improvement in signs and symptoms.[6] The Royal college of Physicians (London) developed comprehensive protocols for appropriate treatment, by using a high-potency vitamin B complex with minimum of thiamine 500 mg intravenously three times daily for 3 days; and, if clinical responded to treatment, continue daily thiamine 500 mg daily for 5 days or until clinical improvement ceases.[2] Many previous case reports of Wernicke's encephalopathy in hyperemesis gravidarum patients reported that thiamine 100 mg once daily is adequate to treat these patients.[5,7–9] In non-alcoholic patients, an intravenous dose of thiamine 100-200 mg once daily could be enough, whereas in alcoholic patients, still higher doses may be required.[10] Even though our patient had the history of drinking alcohol, she had quit it 4 months before the occurrence of Wernicke encephalopathy, and hence she was treated as a non-alcoholic patient by us. Her condition dramatically improved after administration of thiamine 100 mg intravenously once daily for five days.
Signs and symptoms associated with thiamine deficiency lack sensitivity and specificity, and hence thiamine deficiency is frequently underdiagnosed by physicians.[10] Wernicke 's encephalopathy is an uncommon complication in hyperemesis gravidarum. Any pregnant women who suffers from hyperemesis should receive thiamine supplements, and if her mental states, alters, or any other ocular signs or ataxia develop, Wernicke's encephalopathy should be considered. This warrants immediate treatment by thiamine. Total thiamine in blood sample should be measured before its administration, and MRI brain should be taken to support the diagnosis of Wernicke's encephalopathy.[6]
MRI brain showed hypersignal intensity signal in T2-weighted, DWI nd FLAIR at central of pons. These findings were compatible with central pontine myelinolysis (CPM), which is. a demyelinating disorder, symmetrically involving the central portion of the pons. Typical pathology of CPM is characterized by loss of oligodendrocytes and myelin: however, the neurons and axons remain preserved.[11] CPM almost always occurs in patients with chronic medical conditions, particularly alcoholic abuse and malnutrition. Coexistence of Wernicke's encephalopathy and CPM has been reported in some specific conditions.[12] Furthermore, Wernicke's encephalopathy with CPM in hyperemesis gravidarum has been reported in the literature.[7,8,13] There is also a case in which the pontine lesion was seen in the imaging; however, there were no clinical signs or symptoms of pontine involvement.[7] Therefore, CPM can emerge without any clinical evidence, as seen in our case. Malnutrition may be caused both CPM and Wernicke's encephalopathy in such cases.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Netravathi M, Sinha S, Taly AB, Bindu PS, Bharath RD. Hyperemesis gravidarum induced Wernicke's encephalopathy: Serial clinical, electrophysiological and MR imaging observations. J Neurol Sci. 2009;284:214–6. doi: 10.1016/j.jns.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Sechi G, Serra A. Wernicke's encephalopathy: New clinical settings and recent advances in diagnosis and management. Lancet Neurol. 2007;6:442–55. doi: 10.1016/S1474-4422(07)70104-7. [DOI] [PubMed] [Google Scholar]
- 3.Martin PR, Singleton CK, Hiller-Sturmhofel S. The role of thiamine deficiency in alcoholic brain disease. Alcohol Res Health. 2003;27:134–42. [PMC free article] [PubMed] [Google Scholar]
- 4.Brody T. Nutritional Biochemistry. 2nd ed. San Diego: Academic Press; 1999. Vitamins; pp. 491–692. [Google Scholar]
- 5.Chiossi G, Neri I, Cavazzuti M, Basso G, Facchinetti F. Hyperemesis gravidarum complicated by Wernicke encephalopathy: Background, case report, and review of the literature. Obstet Gynecol Surv. 2006;61:255–68. doi: 10.1097/01.ogx.0000206336.08794.65. [DOI] [PubMed] [Google Scholar]
- 6.Galvin R, Brathen G, Ivashynka A, Hillbom M, Tanasescu R, Leone MA. EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol. 2010;17:1408–18. doi: 10.1111/j.1468-1331.2010.03153.x. [DOI] [PubMed] [Google Scholar]
- 7.Zara G, Codemo V, Palmieri A, Schiff S, Cagnin A, Citton V, et al. Neurological complications in hyperemesis gravidarum. Neurol Sci. 2012;33:133–5. doi: 10.1007/s10072-011-0660-y. [DOI] [PubMed] [Google Scholar]
- 8.Bergin PS, Harvey P. Wernicke's encephalopathy and central pontine myelinolysis associated with hyperemesis gravidarum. BMJ. 1992;305:517–8. doi: 10.1136/bmj.305.6852.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson RK, Kuncl RW, Corse AM. Wernicke's encephalopathy: Beyond alcoholism. Nat Clin Pract Neurol. 2006;2:54–8. doi: 10.1038/ncpneuro0094. quiz 8. [DOI] [PubMed] [Google Scholar]
- 10.Manzanares W, Hardy G. Thiamine supplementation in the critically ill. Curr Opin Clin Nutr Metab Care. 2011;14:610–7. doi: 10.1097/MCO.0b013e32834b8911. [DOI] [PubMed] [Google Scholar]
- 11.Norenberg MD. Central pontine myelinolysis: Historical and mechanistic considerations. Metab Brain Dis. 2010;25:97–106. doi: 10.1007/s11011-010-9175-0. [DOI] [PubMed] [Google Scholar]
- 12.Thompson PD, Gledhill RF, Quinn NP, Rossor MN, Stanley P, Coomes EN. Neurological complications associated with parenteral treatment: Central pontine myelinolysis and Wernicke's encephalopathy. Br Med J (Clin Res Ed) 1986;292:684–5. doi: 10.1136/bmj.292.6521.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Falcone N, Compagnoni A, Meschini C, Perrone C, Nappo A. Central pontine myelinolysis induced by hypophosphatemia following Wernicke's encephalopathy. Neurol Sci. 2004;24:407–10. doi: 10.1007/s10072-003-0197-9. [DOI] [PubMed] [Google Scholar]


