Abstract
Understanding the cellular and molecular mechanisms involved in the development and progression of pulmonary hypertension (PH) remains imperative if we are to successfully improve the quality of life and life span of patients with the disease. A whole plethora of mechanisms are associated with the development and progression of PH. Such complexity makes it difficult to isolate one particular pathway to target clinically. Changes in intracellular free calcium concentration, the most common intracellular second messenger, can have significant impact in defining the pathogenic mechanisms leading to its development and persistence. Signaling pathways leading to the elevation of [Ca2+]cyt contribute to pulmonary vasoconstriction, excessive proliferation of smooth muscle cells and ultimately pulmonary vascular remodeling. This current review serves to summarize the some of the most recent advances in the regulation of calcium during pulmonary hypertension.
Keywords: CaSR, NFAT, ORAI, STIM, TRP
INTRODUCTION
Calcium signaling impacts almost every aspect of cellular existence. It is the most common second messenger and, as such, regulation of calcium homeostasis within cells can have pertinent effects on cellular function. Pulmonary Hypertension (PH) is just one disease where changes in intracellular free calcium concentration ([Ca2+]cyt) can have significant impact in defining the pathogenic mechanisms leading to its development and persistence.
PH is a rare but severe and fatal lung disease, affecting predominantly women, which is caused by a plethora of mechanisms. The latest WHO clinical classification of PH groups manifestations of disease with similarities in the pathophysiologic mechanisms, clinical presentation, and therapeutic approaches together [1]. The pulmonary artery under normal conditions is maintained as a low resistance low pressure system which enables it to receive the entire cardiac output (CO) at one time. Mean pulmonary artery pressure (mPAP) is normally maintained at 16 mmHg. PH is characterized by an increase in mPAP to ≥25 mmHg at rest. Such an elevation of mPAP is typically due to increased pulmonary vascular resistance (PVR) as determined by the equation PVR×CO=mPAP. When blood flow through the pulmonary artery becomes restricted the right side of the heart compensates by pumping more forcefully, when this is sustained the right hand side of the heart becomes increasingly muscular and right ventricular hypertrophy ensues, the prognosis is poor. One of the hallmarks of PH contributing to the increase in PVR is a severe obstructive vasculopathy where the intima, media and adventitia are significantly thickened and more distal vessels become increasingly muscular. Characteristic vascular lesions, such as plexiform lesions and neointimal proliferation, also lead to obstruction of the pulmonary arteries [2]. Vasoconstriction of the arteries or occlusion due to in situ thrombosis is other examples contributing to the increase PVR in PH.
There has been a whole plethora of mechanisms associated with the development and progression of PH. Such complexity makes it difficult to isolate one particular pathway to target clinically. One commonality amongst these deregulated signaling pathways is the elevation of [Ca2+]cyt contributing to pulmonary vasoconstriction and excessive proliferation of smooth muscle cells and ultimately pulmonary vascular remodeling. The topic of calcium regulation in PH has been widely studied and there are a number of comprehensive reviews which I direct readers to [3-5]. Current therapeutic approaches, for example prostacyclin derivatives, endothelin-receptor antagonists, and phosphodiesterase type 5 inhibitors, have been unable to substantially decrease the morbidity and mortality due to PH. New mechanisms and novel therapeutic targets in PH are still at the forefront of research into PH and the current review serves to summarize the some of the most recent advances in the regulation of calcium during pulmonary hypertension.
VOLTAGE-DEPENDENT CALCIUM CHANNELS
Spanning the cell membrane are assortments of channels each allowing the specific transport of ions in or out of the cells. Voltage dependent Ca2+ channels (VDCC) are four domains, 6 transmembrane spanning proteins which have been functionally classified by their activation voltages. Low voltage-gated T-type channels (LVA) and high voltage-gated dihydropyridine-sensitive L-type channels (HVA) have both been identified with electrophysiological data supporting a functional role in the pulmonary artery, reviewed in Firth et al. [6]. The channels comprise of pore forming α subunits and additional regulatory subunits (β, α2δ and γ). Despite the detection of six α1 subunits at the transcriptional level functional evidence suggests that channels are either encoded by the α1c-subunit (L-type VDCC) or the α1G-subunit (T-type VDCC). L-type calcium channels are widely accepted as the source for depolarization dependent Ca2+ influx in pulmonary arterial smooth muscle cell (PASMC). The activity of these channels is largely controlled by membrane potential and voltage-gated potassium channels (Kv channels) are proposed to be the major regulators of resting membrane potential in PASMC. Inhibition of Kv channel expression and function is described in PASMC exposed to chronic hypoxia (CH) and those isolated from patients with idiopathic pulmonary arterial hypertension (IPAH); this change in Kv current is sufficient to depolarize the membrane and activate L-type VDCC Ca2+ influx [7-11].
T-type calcium channels have recently emerged as potential targets in PH. They are low voltage activated channels encoded by the Ca(v)3 family of genes which have been shown to be key source for Ca2+ influx to regulate cell cycle progression and, therefore, in the regulation of PASMC proliferation [12,13]. In normal PASMC, the Ca(v)3.1 isoform has been identified and its inhibition prevented entry into the cell cycle preventing a proliferative response [13]. Ca(v)3.1 has been specifically linked to the expression and activation of cyclin D further supporting its importance in regulating cell cycle suppressing [14]. In pulmonary artery endothelial cells (PAEC), isolated from the CH induced experimental model of PH, a decreased ATP-dependent and depolarization induced Ca2+ entry via mibefradil-sensitive T-type channels has been observed [15]. Such function regulation would imply a potential role in PH and in particular in pulmonary vascular remodeling. It will be important to fully explore the regulation of T-type channels in experimental models of PH and in human disease cells.
STORE OPERATED CALCIUM ENTRY (SOCE): TRP, STIM AND ORAI
Hypoxic pulmonary vasoconstriction (HPV) is one of the first responses adopted by the pulmonary vasculature in response to decreased partial pressure of oxygen. After sensing a decreased oxygen tension the pulmonary arteries constrict to divert the blood flow to match oxygen tension to perfusion. When HPV is sustained it can lead to more permanent changes in the pulmonary vasculature such as pulmonary vascular remodeling and the development of PH. While it is known that HPV is mediated by decreased K+ channel currents causing depolarization activated Ca2+ influx through voltage-gated channels there was an uncertainty as to why HPV was reliant upon a high degree of pre-constriction in isolated rat pulmonary artery. Back in 2000, Robertson et al. investigated the involvement of intracellular stores [16]. These studies were amongst the first to show voltage dependent and voltage independent phases contributing to HPV. The voltage independent phase was contingent upon a store depletion mediated capacitive Ca2+ entry (CCE) [16]. Since these observations there has been a distinct focus on identifying the molecular correlates for this store operated calcium entry (SOCE) pathway.
The precise identity of the channels constituting SOCE in PASMC has been debated over recent years, however evidence suggests that transient receptor potential channels (TRP), stromal interaction molecule 1 (STIM1) and Orai (a fundamental Ca2+ release activated Ca2+ channel pore-forming subunit in the plasma membrane) may act in concert or independently to drive SOCE. Responses to hypoxia are greater in distal PASMC over more proximally isolated cells. Using a combination of Ca2+-free extracellular solutions and cyclopiazonic acid to deplete the endoplasmic/sarcoplasmic reticulum (ER/SR) stores of Ca2+ Lu et al. were able to show that SOCE is important in HPV and that the response of the more distal pulmonary artery is greater most likely due to the increased SOCE [17]. Although the identity of the SOCE channel was not determined, expression of STIM1 and TRPC1, 3, 4, and 6 isoforms were detected at higher protein and mRNA levels in the distal pulmonary artery. TRP are a family of non-selective ion channels that are known to encode the store-operated Ca2+ channels (SOC) activated by Ca2+ store depletion (reviewed by [18]). CCE via TRP channels is thought to be important in human PASMC proliferation [19,20] and in enhanced [Ca2+]cyt during exposure to chronic hypoxia [21] and in a hypoxia inducible factor-1 (HIF-1) dependent manner [22,23]. TRPC6 is also known to be upregulated in PASMC from IPAH patients [24]. STIM1 acts as a sensor of ER/SR Ca2+ concentration. At rest it is diffusely present in the ER/SR membrane, upon depletion of Ca2+ from the ER/SR, it oligomerizes and translocates to discrete punctae in the ER/SR membrane that are in close proximity to the plasma membrane [25]. Using a fluorescence resonance energy transfer (FRET) technique, Navarro-Borelly and colleagues demonstrated a direct redistribution and interaction of both STIM-1 and Orai-1 in response to store depletion of Ca2+ [26]. Around the same time Liao et al. used a combination of electrophysiological techniques and intracellular Ca2+ imaging to demonstrate a similar STIM-1 interaction between both Orai-1 and TRPC subunits [27]. These observations have also been demonstrated in mouse pulmonary artery smooth muscle cells where Ng and colleagues showed co-immunoprecipitation of TRPC1 with STIM1 and of Orai with STIM-1 [28,29]. Post store depletion the precipitation level and co-localization of STIM-1 and Orai increased [28,29].
SOCE is shown to be a feature of several other known proponents of pulmonary hypertension, for example endothelin-1 (ET-1) and platelet derived growth factor (PDGF) mediated signaling. ET-1 production is enhanced and expression of its receptors upregulated in PH [30-32]. ET-1 induced pulmonary vasoconstriction of monocrotaline treated rats is partially inhibited by SOCE blockers including gadolinium (Gd3+), lanthanum (La3+), SKF-96365 and TRPC inhibitor BTP-2 [33]. PDGF is a potent mitogen which has been shown, along with its receptor, to be upregulated in models of PH and proposed to have a pertinent role in pulmonary vascular remodeling [34,35]. PDGF mediated PASMC proliferation is, in part, due to an upregulation of TRPC6 channels [36]. More recent data also linked PDGF with the activation of the Akt/mTOR pathway and, subsequently, to enhanced SOCE and cell proliferation in human PASMC. Inhibition of Akt attenuated the increase in [Ca2+]cyt and correlated with a significant downregulation of both STIM and Orai [37].
In addition to the TRPC channels, the TRPV channels have received some recent attention [38]. Stimulation of TRPV1 and V4 channels, identified in PASMC, leads to increased [Ca2+]cyt and PASMC migration with a correlating reorganization of the F-actin cytoskeleton and intermediate filament network [39]. Furthermore, TRPV4 appears to be important in the development of hypoxia-induced PH due to facilitated Ca2+ influx increasing pulmonary vasoconstriction and pulmonary vascular remodeling. This was supported by an enhanced myogenic tone and pulmonary vascular remodeling in hypoxic TRPV4 knockout mice [40]. The precise pathway linking TRP, STIM and Orai still remains to be fully elucidated; data does support an important role for all of the SOCE molecular correlates in the regulation of PASMC homeostasis and potentially implicated important roles in the development and pathogenesis of PH.
CALCIUM-DEPENDENT REGULATION OF NFAT
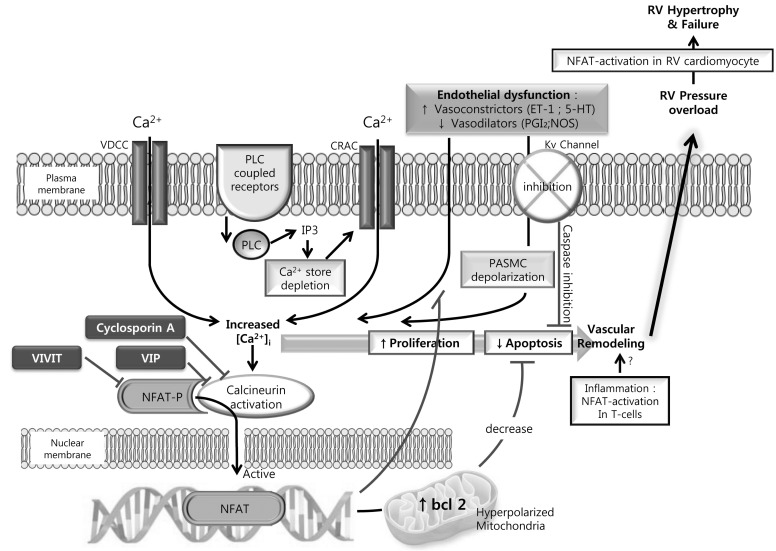
As mentioned above a down regulation of Kv channels in PASMC and PA from patients with PH is now widely accepted. The associated membrane depolarization activate voltage dependent calcium channels leading to increased [Ca2+]cyt which has the knock on effects of contributing to increased contractility, enhanced cell proliferation and decreased cell apoptosis. It is, however still unclear what leads to the down regulation of these potassium channels. NFAT (nuclear factor of activated T cells) is a calcium/calcineurin-sensitive transcription factor which has recently been shown to be elevated in PASMC and circulating leukocytes in PH patients. NFAT isoform c2 inhibition did correlate to a restoration in Kv1.5 expression and function ultimately decreasing [Ca2+]cyt [41]. Another study using the chronic hypoxia mouse induced model of PH identified a requirement for NFAT isoform c3 [42]. CH induced endothelin-1 expression is a well-established phenomenon. In isolated mouse pulmonary resistance arteries NFATc3 was activated by endothelin-1, a response verified in human PASMC to involve Rho A kinase and actin polymerization [43]. A pathway whereby CH induced endothelin-1 expression enhances [Ca2+]cyt, Rho A kinase activity and actin polymerization (recently reviewed in [44,45]) leads to the activation of calcineurin, dephosphorylating NFATc3 and enhancing its translocation to the nucleus to become transcriptionally active can thus be implied from the current data (Fig. 1).
Fig. 1.
The calcineurin-NFAT pathway as an integrator of multiple signaling pathways in the pathogenesis of pulmonary hypertension (PH). NFAT resides in the cytoplasm of resting cells in a phosphorylated and inactive state. Endothelial dysfunction occurs early in PH and results in an increased release of vasoconstrictors (Endothelin-1 [ET-1] and 5-Hydroxytryptamine [5-HT]) and decreased vasodilators (Prostaglandin [PGI2] and nitric oxide synthase [NOS]). These vasoconstrictors can stimulate phospholipase C (PLC) coupled cell surface receptors leading to mobilization of calcium ions (Ca2+) from intracellular stores via inositol trisphosphate (IP3). The elevated intracellular calcium ([Ca2+]i) can cause further Ca2+ influx via Ca2+ release-activated Ca2+ channels (CRAC). Addtionally, the down-regulation of Kv1.5 depolarized PASMC and will lead to the influx of via L-type voltage dependent Ca2+ channels (VDCC). The elevated [Ca2+]i activates phosphatase calcineurin which dephosphorylates NFAT allowing for its translocation to the nucleus. Here it is involved in the regulation of multiple genes. Multiple NFAT binding elements are present in the promoter regions of both the Kv1.5 and bcl-2 genes leading to a promotion of cell proliferation and suppressing mitochondrial-dependent apoptosis. Cyclosporin A inhibits calcineurin-ubstrate interactions and VIVITs electively inhibits NFAT activation.
It is interesting to again reflect on some of the similarities between mechanisms involved in the development of PH and of cancer. In mouse osteosarcoma FBJ-S1 and Lewis lung carcinoma cells an L-type VDCC/[Ca2+]cyt/calcineurin/NFAT signaling pathway has been shown to transcriptionally regulate the expression of caveolin-1 [46]. Caveolin-1 is already known to be an integral component in the pulmonary vascular remodeling in PH. Although data is somewhat conflicting between animal models and human cells it has been shown that its expression is increased in PASMC from patients with IPAH [47,48]. Caveolin-1 is an integral structural component of caveolae; a subset of membrane lipid rafts which serve as regions to coordinate cellular signaling. Thus targeting NFAT may be key to targeting several of the known pathways involved in the development and progression of PH.
Increased [Ca2+]cyt is a prerequisite for nuclear translocation of NFAT. As discussed above increased SOCE is now considered a key mechanism in the pathogenesis of PH. In addition to the entry of calcium via voltage dependent ion channels studies have shown that SOCE and CCE dependent increases in cytoplasmic calcium are directly linked to increased nuclear translocation of NFAT in the pulmonary vasculature [49,50]. Reports suggest that the anti-proliferative effects of sildenafil in PH are due to a mechanism in addition to the known NO/cGMP axis [51,52]. Wang and colleagues nicely demonstrated that the anti-proliferative effects of sildenafil in PASMC are due to the SOCE/[Ca2+]cyt/NFAT pathway [49]. Sildenafil successfully suppressed the hypoxia mediated increase in TRPC1 gene and protein levels and increased SOCE mediated nuclear translocation of NFAT in human PASMC increasing cell proliferation rates [49]. In calf PAEC NFATc1 translocates to the nucleus after elevation of [Ca2+]cyt by agonists like bradykinin or ATP. However, in the absence of extracellular calcium, CCE does not occur and translocation to the nucleus appears to be inhibited and therefore independent of Ca2+ release from the ER [50].
NFAT has been shown to crosstalk with both calcineurin and PPARγ; a role for PPAR in the pathogenesis of PH has become strikingly evident over the past decade. Peroxisome proliferator activated receptor (PPAR) is a member of the nuclear hormone receptor superfamily of ligand activated transcription factors [53]. Two isoforms exist differing in N terminal domains only but with distinct tissue distribution; isoform PPARγ2 is mostly associated with adipose tissue expression whereas the PPARγ1 is more widely expressed including brain, vascular tissues and lymphatic cells. In the lung expression has been shown in the pulmonary vasculature including both smooth muscle cells and endothelial cells, with decreased expression levels observed in PH patient derived cells and in in vivo animal models of PH [54]. In the case of cardiac hypertrophy, where this interaction has been more widely studied, elevation of PPARγ using ligands, such as rosiglitazone, has been shown to inhibit endothelin-1 mediated hypertrophy via NFAT/calcineurin signaling [55].
The PPAR family of transcription factors also includes two other isoforms: delta and beta. Like PPARγ they act by heterodimerizing with the RXR (retanoid X receptor) and then bind to peroxisome proliferator hormone response elements to regulate transcription of target genes. PPARβ/δ has been reported to modulate gene regulation in response to prostacyclin analogues like sildenafil. Like the sildenafil dependent regulation of SOCE/[Ca2+]cyt/NFAT pathway mentioned above, evidence for another NO/cGMP independent pathway of action exists: in this recent study acute prostacyclin-induced Ca2+-activated K+ channel activation in human PASMC was found to be reliant upon PPARβ/δ signaling [56].
MICRORNA REGULATION
Micro RNAs (miR) were first identified in 1993 by Lee and colleagues [57]. It was not until the 2000's that they become more widely recognized as biological regulators with distinct and conserved functions. miR are short nucleotide sequences of ~22 nucleotide that act as post transcriptional regulators binding to the complementary sequence in the 3'UTR of target genes. Each miR is capable of targeting hundreds of genes with an estimated 60% of genes targeted. Over 700 miR are currently identified in humans with a predicted 800 to exist. Over the past 10 years miR has been shown to be both regulators of normal cell function and to be deregulated in disease. Their involvement in disease pathogenesis is seemingly endless. One of the most pertinent discoveries seems to be their ability to serve as biomarkers in, but not limited to; cancer [58-61], cardiovascular disease [62,63], multiple sclerosis [64], inflammatory bowel disease [65], schizophrenia [66] and rheumatoid arthritis [67].
It was only recently that a handful of miRs have been identified in the pulmonary vasculature with proposed pathophysiological roles in PH [68-70]. From these select few studies it is evident that the formation of plexiform lesions and pulmonary vascular remodeling involve regulation by miR activity [68-72]. Comparing plexiform lesions and concentric lesions dissected from the arteries of pulmonary arterial hypertension and control patients one study demonstrated that smooth muscle specific miRs 143 and 145 were significantly higher in concentric lesions; data supported by similar up-regulation of the miR target genes myocardin and smooth muscle heavy chain. miR-126, on the other hand, was augmented in plexiform lesions. VEGF-A is the major target of miR-126 and thus elevation of this miR enhances angiogenesis and thus helps to explain the pronounced angiogenic phenotype of these lesions [73,74]. In PASMC a correlating down-regulation of miR-204, acting by promotion of a STAT3 feedback loop leading to sustained activation of STAT3, was also observed supporting an enhanced cell proliferation [75]. Inhibition of the src/STAT3/Pim1 axis has been shown to improve monocrotaline-induced hypertension in rats by increasing apoptosis through depolarization of mitochondria and decreasing vessel contractility and proliferation due to decreased [Ca2+]cyt [76]. miR-328 is another miR identified in the pulmonary vasculature with a proposed role in chronic hypoxia mediated secondary pulmonary hypertension via regulation of L-Type calcium channels [70]. A miR-328 binding site in the 3'UTR of the L-Type Calcium channel isoform 1ac leads to an inhibition of its expression. In PH, miR-328 is significantly down-regulated leading to a concomitant up-regulation of L-Type calcium channels and thus an increased potential for elevation of [Ca2+]cyt [70]. In many essential ways the regulation of miR in pulmonary hypertension mirrors that in cancer with roles leading to increased cell proliferation and oncogenesis.
CALCIUM SENSING RECEPTOR (CaSR)
A Calcium Sensing Receptor (CaSR) was first characterized and cloned from bovine parathyroid back in 1993 after a role in parathyroid hormone secretion was identified [77,78]. Soon after it was cloned and mapped to chromosome 3q13.3-21 in humans [79,80]. The CaSR is a 1078 amino acid encoded member of the G-protein-coupled receptor family. Its expression is most commonly associated with the parathyroid and kidney where it senses extracellular calcium levels to regulate parathyroid hormone (PTH) secretion and renal tubular calcium reabsorption in response to alterations in extracellular calcium. Since then its expression has been identified in a wide variety of tissues including, but not limited to; sensory nerves [81-83], pancreatic islet cells [84], osteoclasts [85,86], epithelial cells [87,88], hepatocytes [89,90], cardiomyocytes [91,92] and B cells [93]. Furthermore, mutations in the receptor have been identified and functionally linked to diseases like hyper- and hypo-calcemia, Bratter's Syndrome and hypoparathyroidism [94-98]. A variety of cancers have also been associated by an absence or loss of CaSR; pituitary adenomas and colorectal cancer [99-101]. In colorectal cancer a decreased CaSR expression in the colonic epithelium is evident; it is believed at CaSR acts to promote the down-regulation of beta-catenin-mediated transcriptional activation having subsequent effects on cell proliferation [87,102,103]. Functional expression is also identified in the cardiovascular system [91,104,105] and, most recently, in the pulmonary vasculature where it has been implicated in the pathogenesis of PH [106-109].
Given the importance of calcium in the development and pathogenesis of PH, it comes as no surprise that the CaSR is present in the pulmonary artery. Studies in isolated rat pulmonary arteries and PASMCs first identified functional CaSR [109]. This study demonstrated the presence of CaSR in PASMC and showed that it was involved in regulating pulmonary arterial tension by signaling through PLC and IP3 [109]. The same group followed this study by investigating how the CaSR was regulated in hypoxic condition; a pathway involving CaSR dependent MEK/ERK and PI3K activation contributed to the hypoxia induced increased proliferative rate of the PASMC [108]. While these studies implicated a role for CaSR in pulmonary vascular disease a more recent study by Yamamura and colleagues took IPAH patient cells and utilized the monocrotaline-induced animal model of PH to more specifically look at the role of CaSR in pulmonary disease [107]. In the IPAH cells, calcium influx was enhanced with calcimimetic R568 or decreased with calcylitic NPS2143 additionally, the expression of CaSR was significantly higher. More interestingly the development of PH and right ventricular hypertrophy in both monocrotaline-treated and hypoxia-exposed rats was prevented after injection of the calcilytic [107]. This study is really the first to show a pathogenic role for CaSR in PH and it will be interesting to see if CaSR promises to be a potent therapeutic target in patients with PH.
This review has highlighted some of the most recent advances in calcium signaling and regulation in PH. Hopefully, more studies will start to identify small molecules or other ways to manipulate the signaling pathways described and push more selective therapeutic approaches into the clinic.
ACKNOWLEDGEMENTS
Amy L. Firth is funded by a postdoctoral training fellowship from the California Institute of Regenerative Medicine (CIRM). This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MEST) (2010-0021126, 2011-0028573, 2012-M3A9C7050093).
ABBREVIATIONS
- CaSR
calcium sensing receptor
- CCE
capacitive Ca2+ entry
- CH
chronic hypoxia
- CO
cardiac output
- ET-1
endothelin-1
- HIF-1
hypoxic inducible factor-1
- HPV
hypoxic pulmonary vasoconstriction
- 5-HT
5-hydroxytryptamine
- HVA
high voltagegated dihydropyridine-sensitive L-type channels
- IP3
inositol triphosphate
- IPAH
idiopathic pulmonary arterial hypertension
- LVA
low voltage-gated T-type channels
- miR
micro RNAs
- mPAP
mean pulmonary artery pressure
- NFAT
nuclear factor of activated T cells
- NOS
nitric oxide synthase
- PAEC
pulmonary artery endothelial cells
- PASMC
pulmonary arterial smooth muscle cell
- PGI2
prostaglandin
- PH
pulmonary hypertension
- PLC
phospholipase C
- PPAR
peroxisome proliferator activated receptor
- PVR
pulmonary vascular resistance
- SOCE
store operated calcium entry
- STIM1
stromal interaction molecule 1
- TRP
transient receptor potential
- VDCC
voltage dependent Ca2+ channels
References
- 1.Simonneau G, Robbins IM, Beghetti M, Channick RN, Delcroix M, Denton CP, Elliott CG, Gaine SP, Gladwin MT, Jing ZC, Krowka MJ, Langleben D, Nakanishi N, Souza R. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2009;54(1 Suppl):S43–S54. doi: 10.1016/j.jacc.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 2.Yoon CH, Park HJ, Cho YW, Kim EJ, Lee JD, Kang KR, Han J, Kang D. Cigarette smoke extract-induced reduction in migration and contraction in normal human bronchial smooth muscle cells. Korean J Physiol Pharmacol. 2011;15:397–403. doi: 10.4196/kjpp.2011.15.6.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuhr FK, Smith KA, Song MY, Levitan I, Yuan JX. New mechanisms of pulmonary arterial hypertension: role of Ca2+ signaling. Am J Physiol Heart Circ Physiol. 2012;302:H1546–H1562. doi: 10.1152/ajpheart.00944.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang YX, Zheng YM. ROS-dependent signaling mechanisms for hypoxic Ca2+ responses in pulmonary artery myocytes. Antioxid Redox Signal. 2010;12:611–623. doi: 10.1089/ars.2009.2877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shimoda LA, Wang J, Sylvester JT. Ca2+ channels and chronic hypoxia. Microcirculation. 2006;13:657–670. doi: 10.1080/10739680600930305. [DOI] [PubMed] [Google Scholar]
- 6.Firth AL, Remillard CV, Platoshyn O, Fantozzi I, Ko EA, Yuan JX. Functional ion channels in human pulmonary artery smooth muscle cells: Voltage-dependent cation channels. Pulm Circ. 2011;1:48–71. doi: 10.4103/2045-8932.78103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Platoshyn O, Yu Y, Ko EA, Remillard CV, Yuan JX. Heterogeneity of hypoxia-mediated decrease in I(K(V)) and increase in [Ca2+](cyt) in pulmonary artery smooth muscle cells. Am J Physiol Lung Cell Mol Physiol. 2007;293:L402–L416. doi: 10.1152/ajplung.00391.2006. [DOI] [PubMed] [Google Scholar]
- 8.Wang J, Juhaszova M, Rubin LJ, Yuan XJ. Hypoxia inhibits gene expression of voltage-gated K+ channel alpha subunits in pulmonary artery smooth muscle cells. J Clin Invest. 1997;100:2347–2353. doi: 10.1172/JCI119774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yuan XJ, Tod ML, Rubin LJ, Blaustein MP. Hypoxic and metabolic regulation of voltage-gated K+ channels in rat pulmonary artery smooth muscle cells. Exp Physiol. 1995;80:803–813. doi: 10.1113/expphysiol.1995.sp003888. [DOI] [PubMed] [Google Scholar]
- 10.Yuan XJ. Voltage-gated K+ currents regulate resting membrane potential and [Ca2+]i in pulmonary arterial myocytes. Circ Res. 1995;77:370–378. doi: 10.1161/01.res.77.2.370. [DOI] [PubMed] [Google Scholar]
- 11.Park SJ, Yoo HY, Kim HJ, Kim JK, Zhang YH, Kim SJ. Requirement of pretone by thromboxane A(2) for hypoxic pulmonary vasoconstriction in precision-cut lung slices of Rat. Korean J Physiol Pharmacol. 2012;16:59–64. doi: 10.4196/kjpp.2012.16.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rodman DM, Harral J, Wu S, West J, Hoedt-Miller M, Reese KA, Fagan K. The low-voltage-activated calcium channel CAV3.1 controls proliferation of human pulmonary artery myocytes. Chest. 2005;128(6 Suppl):581S–582S. doi: 10.1378/chest.128.6_suppl.581S. [DOI] [PubMed] [Google Scholar]
- 13.Rodman DM, Reese K, Harral J, Fouty B, Wu S, West J, Hoedt-Miller M, Tada Y, Li KX, Cool C, Fagan K, Cribbs L. Low-voltage-activated (T-type) calcium channels control proliferation of human pulmonary artery myocytes. Circ Res. 2005;96:864–872. doi: 10.1161/01.RES.0000163066.07472.ff. [DOI] [PubMed] [Google Scholar]
- 14.Pluteanu F, Cribbs LL. Regulation and function of Cav3.1 T-type calcium channels in IGF-I-stimulated pulmonary artery smooth muscle cells. Am J Physiol Cell Physiol. 2011;300:C517–C525. doi: 10.1152/ajpcell.00107.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paffett ML, Riddle MA, Kanagy NL, Resta TC, Walker BR. Altered protein kinase C regulation of pulmonary endothelial store- and receptor-operated Ca2+ entry after chronic hypoxia. J Pharmacol Exp Ther. 2010;334:753–760. doi: 10.1124/jpet.110.165563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robertson TP, Hague D, Aaronson PI, Ward JP. Voltage-independent calcium entry in hypoxic pulmonary vasoconstriction of intrapulmonary arteries of the rat. J Physiol. 2000;525:669–680. doi: 10.1111/j.1469-7793.2000.t01-1-00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu W, Wang J, Shimoda LA, Sylvester JT. Differences in STIM1 and TRPC expression in proximal and distal pulmonary arterial smooth muscle are associated with differences in Ca2+ responses to hypoxia. Am J Physiol Lung Cell Mol Physiol. 2008;295:L104–L113. doi: 10.1152/ajplung.00058.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Firth AL, Remillard CV, Yuan JX. TRP channels in hypertension. Biochim Biophys Acta. 2007;1772:895–906. doi: 10.1016/j.bbadis.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Golovina VA, Platoshyn O, Bailey CL, Wang J, Limsuwan A, Sweeney M, Rubin LJ, Yuan JX. Upregulated TRP and enhanced capacitative Ca2+ entry in human pulmonary artery myocytes during proliferation. Am J Physiol Heart Circ Physiol. 2001;280:H746–H755. doi: 10.1152/ajpheart.2001.280.2.H746. [DOI] [PubMed] [Google Scholar]
- 20.Sweeney M, Yu Y, Platoshyn O, Zhang S, McDaniel SS, Yuan JX. Inhibition of endogenous TRP1 decreases capacitative Ca2+ entry and attenuates pulmonary artery smooth muscle cell proliferation. Am J Physiol Lung Cell Mol Physiol. 2002;283:L144–L155. doi: 10.1152/ajplung.00412.2001. [DOI] [PubMed] [Google Scholar]
- 21.Lin MJ, Leung GP, Zhang WM, Yang XR, Yip KP, Tse CM, Sham JS. Chronic hypoxia-induced upregulation of store-operated and receptor-operated Ca2+ channels in pulmonary arterial smooth muscle cells: a novel mechanism of hypoxic pulmonary hypertension. Circ Res. 2004;95:496–505. doi: 10.1161/01.RES.0000138952.16382.ad. [DOI] [PubMed] [Google Scholar]
- 22.Wang J, Weigand L, Lu W, Sylvester JT, Semenza GL, Shimoda LA. Hypoxia inducible factor 1 mediates hypoxia-induced TRPC expression and elevated intracellular Ca2+ in pulmonary arterial smooth muscle cells. Circ Res. 2006;98:1528–1537. doi: 10.1161/01.RES.0000227551.68124.98. [DOI] [PubMed] [Google Scholar]
- 23.Lee KH. CaMKII inhibitor KN-62 blunts tumor response to hypoxia by inhibiting HIF-1α in hepatoma cells. Korean J Physiol Pharmacol. 2010;14:331–336. doi: 10.4196/kjpp.2010.14.5.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu Y, Fantozzi I, Remillard CV, Landsberg JW, Kunichika N, Platoshyn O, Tigno DD, Thistlethwaite PA, Rubin LJ, Yuan JX. Enhanced expression of transient receptor potential channels in idiopathic pulmonary arterial hypertension. Proc Natl Acad Sci USA. 2004;101:13861–13866. doi: 10.1073/pnas.0405908101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luik RM, Wang B, Prakriya M, Wu MM, Lewis RS. Oligomerization of STIM1 couples ER calcium depletion to CRAC channel activation. Nature. 2008;454:538–542. doi: 10.1038/nature07065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Navarro-Borelly L, Somasundaram A, Yamashita M, Ren D, Miller RJ, Prakriya M. STIM1-Orai1 interactions and Orai1 conformational changes revealed by live-cell FRET microscopy. J Physiol. 2008;586:5383–5401. doi: 10.1113/jphysiol.2008.162503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liao Y, Erxleben C, Abramowitz J, Flockerzi V, Zhu MX, Armstrong DL, Birnbaumer L. Functional interactions among Orai1, TRPCs, and STIM1 suggest a STIM-regulated heteromeric Orai/TRPC model for SOCE/Icrac channels. Proc Natl Acad Sci USA. 2008;105:2895–2900. doi: 10.1073/pnas.0712288105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ng LC, Ramduny D, Airey JA, Singer CA, Keller PS, Shen XM, Tian H, Valencik M, Hume JR. Orai1 interacts with STIM1 and mediates capacitative Ca2+ entry in mouse pulmonary arterial smooth muscle cells. Am J Physiol Cell Physiol. 2010;299:C1079–C1090. doi: 10.1152/ajpcell.00548.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ng LC, McCormack MD, Airey JA, Singer CA, Keller PS, Shen XM, Hume JR. TRPC1 and STIM1 mediate capacitative Ca2+ entry in mouse pulmonary arterial smooth muscle cells. J Physiol. 2009;587:2429–2442. doi: 10.1113/jphysiol.2009.172254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cacoub P, Dorent R, Nataf P, Carayon A, Riquet M, Noe E, Piette JC, Godeau P, Gandjbakhch I. Endothelin-1 in the lungs of patients with pulmonary hypertension. Cardiovasc Res. 1997;33:196–200. doi: 10.1016/s0008-6363(96)00189-7. [DOI] [PubMed] [Google Scholar]
- 31.Li H, Chen SJ, Chen YF, Meng QC, Durand J, Oparil S, Elton TS. Enhanced endothelin-1 and endothelin receptor gene expression in chronic hypoxia. J Appl Physiol. 1994;77:1451–1459. doi: 10.1152/jappl.1994.77.3.1451. [DOI] [PubMed] [Google Scholar]
- 32.Yorikane R, Miyauchi T, Sakai S, Sakurai T, Yamaguchi I, Sugishita Y, Goto K. Altered expression of ETB-receptor mRNA in the lung of rats with pulmonary hypertension. J Cardiovasc Pharmacol. 1993;22(Suppl 8):S336–S338. doi: 10.1097/00005344-199322008-00088. [DOI] [PubMed] [Google Scholar]
- 33.Liu XR, Zhang MF, Yang N, Liu Q, Wang RX, Cao YN, Yang XR, Sham JS, Lin MJ. Enhanced store-operated Ca2+ entry and TRPC channel expression in pulmonary arteries of monocrotaline-induced pulmonary hypertensive rats. Am J Physiol Cell Physiol. 2012;302:C77–C87. doi: 10.1152/ajpcell.00247.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barst RJ. PDGF signaling in pulmonary arterial hypertension. J Clin Invest. 2005;115:2691–2694. doi: 10.1172/JCI26593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Katayose D, Ohe M, Yamauchi K, Ogata M, Shirato K, Fujita H, Shibahara S, Takishima T. Increased expression of PDGF A- and B-chain genes in rat lungs with hypoxic pulmonary hypertension. Am J Physiol. 1993;264:L100–L106. doi: 10.1152/ajplung.1993.264.2.L100. [DOI] [PubMed] [Google Scholar]
- 36.Yu Y, Sweeney M, Zhang S, Platoshyn O, Landsberg J, Rothman A, Yuan JX. PDGF stimulates pulmonary vascular smooth muscle cell proliferation by upregulating TRPC6 expression. Am J Physiol Cell Physiol. 2003;284:C316–C330. doi: 10.1152/ajpcell.00125.2002. [DOI] [PubMed] [Google Scholar]
- 37.Ogawa A, Firth AL, Smith KA, Maliakal MV, Yuan JX. PDGF enhances store-operated Ca2+ entry by upregulating STIM1/Orai1 via activation of Akt/mTOR in human pulmonary arterial smooth muscle cells. Am J Physiol Cell Physiol. 2012;302:C405–C411. doi: 10.1152/ajpcell.00337.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jin Y, Kim J, Kwak J. Activation of the cGMP/Protein kinase G pathway by nitric oxide can decrease TRPV1 activity in cultured rat dorsal root ganglion neurons. Korean J Physiol Pharmacol. 2012;16:211–217. doi: 10.4196/kjpp.2012.16.3.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martin E, Dahan D, Cardouat G, Gillibert-Duplantier J, Marthan R, Savineau JP, Ducret T. Involvement of TRPV1 and TRPV4 channels in migration of rat pulmonary arterial smooth muscle cells. Pflugers Arch. 2012;464:261–272. doi: 10.1007/s00424-012-1136-5. [DOI] [PubMed] [Google Scholar]
- 40.Yang XR, Lin AH, Hughes JM, Flavahan NA, Cao YN, Liedtke W, Sham JS. Upregulation of osmo-mechanosensitive TRPV4 channel facilitates chronic hypoxia-induced myogenic tone and pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol. 2012;302:L555–L568. doi: 10.1152/ajplung.00005.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bonnet S, Rochefort G, Sutendra G, Archer SL, Haromy A, Webster L, Hashimoto K, Bonnet SN, Michelakis ED. The nuclear factor of activated T cells in pulmonary arterial hypertension can be therapeutically targeted. Proc Natl Acad Sci USA. 2007;104:11418–11423. doi: 10.1073/pnas.0610467104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Frutos S, Spangler R, Alo D, Bosc LV. NFATc3 mediates chronic hypoxia-induced pulmonary arterial remodeling with alpha-actin up-regulation. J Biol Chem. 2007;282:15081–15089. doi: 10.1074/jbc.M702679200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Frutos S, Diaz JM, Nitta CH, Sherpa ML, Bosc LV. Endothelin-1 contributes to increased NFATc3 activation by chronic hypoxia in pulmonary arteries. Am J Physiol Cell Physiol. 2011;301:C441–C450. doi: 10.1152/ajpcell.00029.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Firth AL, Choi IW, Park WS. Animal models of pulmonary hypertension: Rho kinase inhibition. Prog Biophys Mol Biol. 2012;109:67–75. doi: 10.1016/j.pbiomolbio.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 45.Connolly MJ, Aaronson PI. Key role of the RhoA/Rho kinase system in pulmonary hypertension. Pulm Pharmacol Ther. 2011;24:1–14. doi: 10.1016/j.pupt.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 46.Yang XY, Huang CC, Kan QM, Li Y, Liu D, Zhang XC, Sato T, Yamagata S, Yamagata T. Calcium regulates caveolin-1 expression at the transcriptional level. Biochem Biophys Res Commun. 2012;426:334–341. doi: 10.1016/j.bbrc.2012.08.079. [DOI] [PubMed] [Google Scholar]
- 47.Patel HH, Zhang S, Murray F, Suda RY, Head BP, Yokoyama U, Swaney JS, Niesman IR, Schermuly RT, Pullamsetti SS, Thistlethwaite PA, Miyanohara A, Farquhar MG, Yuan JX, Insel PA. Increased smooth muscle cell expression of caveolin-1 and caveolae contribute to the pathophysiology of idiopathic pulmonary arterial hypertension. FASEB J. 2007;21:2970–2979. doi: 10.1096/fj.07-8424com. [DOI] [PubMed] [Google Scholar]
- 48.Cogolludo A, Moreno L, Lodi F, Frazziano G, Cobeno L, Tamargo J, Perez-Vizcaino F. Serotonin inhibits voltage-gated K+ currents in pulmonary artery smooth muscle cells: role of 5-HT2A receptors, caveolin-1, and KV1.5 channel internalization. Circ Res. 2006;98:931–938. doi: 10.1161/01.RES.0000216858.04599.e1. [DOI] [PubMed] [Google Scholar]
- 49.Wang C, Li JF, Zhao L, Liu J, Wan J, Wang YX, Wang J, Wang C. Inhibition of SOC/Ca2+/NFAT pathway is involved in the anti-proliferative effect of sildenafil on pulmonary artery smooth muscle cells. Respir Res. 2009;10:123. doi: 10.1186/1465-9921-10-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rinne A, Banach K, Blatter LA. Regulation of nuclear factor of activated T cells (NFAT) in vascular endothelial cells. J Mol Cell Cardiol. 2009;47:400–410. doi: 10.1016/j.yjmcc.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tantini B, Manes A, Fiumana E, Pignatti C, Guarnieri C, Zannoli R, Branzi A, Galie N. Antiproliferative effect of sildenafil on human pulmonary artery smooth muscle cells. Basic Res Cardiol. 2005;100:131–138. doi: 10.1007/s00395-004-0504-5. [DOI] [PubMed] [Google Scholar]
- 52.Kim JE, Sung JY, Woo CH, Kang YJ, Lee KY, Kim HS, Kwun WH, Choi HC. Cilostazol Inhibits Vascular Smooth Muscle Cell Proliferation and Reactive Oxygen Species Production through Activation of AMP-activated Protein Kinase Induced by Heme Oxygenase-1. Korean J Physiol Pharmacol. 2011;15:203–210. doi: 10.4196/kjpp.2011.15.4.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Park SY, Bae JU, Hong KW, Kim CD. HO-1 Induced by Cilostazol Protects Against TNF-α-associated Cytotoxicity via a PPAR-γ-dependent Pathway in Human Endothelial Cells. Korean J Physiol Pharmacol. 2011;15:83–88. doi: 10.4196/kjpp.2011.15.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ameshima S, Golpon H, Cool CD, Chan D, Vandivier RW, Gardai SJ, Wick M, Nemenoff RA, Geraci MW, Voelkel NF. Peroxisome proliferator-activated receptor gamma (PPAR-gamma) expression is decreased in pulmonary hypertension and affects endothelial cell growth. Circ Res. 2003;92:1162–1169. doi: 10.1161/01.RES.0000073585.50092.14. [DOI] [PubMed] [Google Scholar]
- 55.Bao Y, Li R, Jiang J, Cai B, Gao J, Le K, Zhang F, Chen S, Liu P. Activation of peroxisome proliferator-activated receptor gamma inhibits endothelin-1-induced cardiac hypertrophy via the calcineurin/NFAT signaling pathway. Mol Cell Biochem. 2008;317:189–196. doi: 10.1007/s11010-008-9848-8. [DOI] [PubMed] [Google Scholar]
- 56.Li Y, Connolly M, Nagaraj C, Tang B, Balint Z, Popper H, Smolle-Juettner FM, Lindenmann J, Kwapiszewska G, Aaronson PI, Wohlkoenig C, Leithner K, Olschewski H, Olschewski A. Peroxisome proliferator-activated receptor-β/δ, the acute signaling factor in prostacyclin-induced pulmonary vasodilation. Am J Respir Cell Mol Biol. 2012;46:372–379. doi: 10.1165/rcmb.2010-0428OC. [DOI] [PubMed] [Google Scholar]
- 57.Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75:843–854. doi: 10.1016/0092-8674(93)90529-y. [DOI] [PubMed] [Google Scholar]
- 58.Gadducci A, Guerrieri ME, Greco C. Tissue biomarkers as prognostic variables of cervical cancer. Crit Rev Oncol Hematol. 2012 doi: 10.1016/j.critrevonc.2012.09.003. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 59.Qi J, Mu D. MicroRNAs and lung cancers: from pathogenesis to clinical implications. Front Med. 2012;6:134–155. doi: 10.1007/s11684-012-0188-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cortez MA, Welsh JW, Calin GA. Circulating microRNAs as noninvasive biomarkers in breast cancer. Recent Results Cancer Res. 2012;195:151–161. doi: 10.1007/978-3-642-28160-0_13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Papaconstantinou I, Karakatsanis A, Gazouli M, Polymeneas G, Voros D. The role of microRNAs in liver cancer. Eur J Gastroenterol Hepatol. 2012;24:223–228. doi: 10.1097/MEG.0b013e3283505063. [DOI] [PubMed] [Google Scholar]
- 62.Tijsen AJ, Pinto YM, Creemers EE. Circulating microRNAs as diagnostic biomarkers for cardiovascular diseases. Am J Physiol Heart Circ Physiol. 2012;303:H1085–H1095. doi: 10.1152/ajpheart.00191.2012. [DOI] [PubMed] [Google Scholar]
- 63.Li C, Pei F, Zhu X, Duan DD, Zeng C. Circulating microRNAs as novel and sensitive biomarkers of acute myocardial Infarction. Clin Biochem. 2012;45:727–732. doi: 10.1016/j.clinbiochem.2012.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Thamilarasan M, Koczan D, Hecker M, Paap B, Zettl UK. MicroRNAs in multiple sclerosis and experimental autoimmune encephalomyelitis. Autoimmun Rev. 2012;11:174–179. doi: 10.1016/j.autrev.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 65.Iborra M, Bernuzzi F, Invernizzi P, Danese S. MicroRNAs in autoimmunity and inflammatory bowel disease: crucial regulators in immune response. Autoimmun Rev. 2012;11:305–314. doi: 10.1016/j.autrev.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 66.Beveridge NJ, Cairns MJ. MicroRNA dysregulation in schizophrenia. Neurobiol Dis. 2012;46:263–271. doi: 10.1016/j.nbd.2011.12.029. [DOI] [PubMed] [Google Scholar]
- 67.Filkova M, Jungel A, Gay RE, Gay S. MicroRNAs in rheumatoid arthritis: potential role in diagnosis and therapy. BioDrugs. 2012;26:131–141. doi: 10.2165/11631480-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 68.Yang S, Banerjee S, Freitas Ad, Cui H, Xie N, Abraham E, Liu G. miR-21 regulates chronic hypoxia-induced pulmonary vascular remodeling. Am J Physiol Lung Cell Mol Physiol. 2012;302:L521–L529. doi: 10.1152/ajplung.00316.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pullamsetti SS, Doebele C, Fischer A, Savai R, Kojonazarov B, Dahal BK, Ghofrani HA, Weissmann N, Grimminger F, Bonauer A, Seeger W, Zeiher AM, Dimmeler S, Schermuly RT. Inhibition of microRNA-17 improves lung and heart function in experimental pulmonary hypertension. Am J Respir Crit Care Med. 2012;185:409–419. doi: 10.1164/rccm.201106-1093OC. [DOI] [PubMed] [Google Scholar]
- 70.Guo L, Qiu Z, Wei L, Yu X, Gao X, Jiang S, Tian H, Jiang C, Zhu D. The microRNA-328 regulates hypoxic pulmonary hypertension by targeting at insulin growth factor 1 receptor and L-type calcium channel-α1C. Hypertension. 2012;59:1006–1013. doi: 10.1161/HYPERTENSIONAHA.111.185413. [DOI] [PubMed] [Google Scholar]
- 71.Bockmeyer CL, Maegel L, Janciauskiene S, Rische J, Lehmann U, Maus UA, Nickel N, Haverich A, Hoeper MM, Golpon HA, Kreipe H, Laenger F, Jonigk D. Plexiform vasculopathy of severe pulmonary arterial hypertension and microRNA expression. J Heart Lung Transplant. 2012;31:764–772. doi: 10.1016/j.healun.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 72.Caruso P, MacLean MR, Khanin R, McClure J, Soon E, Southgate M, MacDonald RA, Greig JA, Robertson KE, Masson R, Denby L, Dempsie Y, Long L, Morrell NW, Baker AH. Dynamic changes in lung microRNA profiles during the development of pulmonary hypertension due to chronic hypoxia and monocrotaline. Arterioscler Thromb Vasc Biol. 2010;30:716–723. doi: 10.1161/ATVBAHA.109.202028. [DOI] [PubMed] [Google Scholar]
- 73.Nicoli S, Standley C, Walker P, Hurlstone A, Fogarty KE, Lawson ND. MicroRNA-mediated integration of haemodynamics and Vegf signalling during angiogenesis. Nature. 2010;464:1196–1200. doi: 10.1038/nature08889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fish JE, Santoro MM, Morton SU, Yu S, Yeh RF, Wythe JD, Ivey KN, Bruneau BG, Stainier DY, Srivastava D. miR-126 regulates angiogenic signaling and vascular integrity. Dev Cell. 2008;15:272–284. doi: 10.1016/j.devcel.2008.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Paulin R, Courboulin A, Barrier M, Bonnet S. From oncoproteins/tumor suppressors to microRNAs, the newest therapeutic targets for pulmonary arterial hypertension. J Mol Med (Berl) 2011;89:1089–1101. doi: 10.1007/s00109-011-0788-5. [DOI] [PubMed] [Google Scholar]
- 76.Paulin R, Meloche J, Jacob MH, Bisserier M, Courboulin A, Bonnet S. Dehydroepiandrosterone inhibits the Src/STAT3 constitutive activation in pulmonary arterial hypertension. Am J Physiol Heart Circ Physiol. 2011;301:H1798–H1809. doi: 10.1152/ajpheart.00654.2011. [DOI] [PubMed] [Google Scholar]
- 77.Brown EM, Gamba G, Riccardi D, Lombardi M, Butters R, Kifor O, Sun A, Hediger MA, Lytton J, Hebert SC. Cloning and characterization of an extracellular Ca2+-sensing receptor from bovine parathyroid. Nature. 1993;366:575–580. doi: 10.1038/366575a0. [DOI] [PubMed] [Google Scholar]
- 78.Pollak MR, Brown EM, Chou YH, Hebert SC, Marx SJ, Steinmann B, Levi T, Seidman CE, Seidman JG. Mutations in the human Ca2+-sensing receptor gene cause familial hypocalciuric hypercalcemia and neonatal severe hyperparathyroidism. Cell. 1993;75:1297–1303. doi: 10.1016/0092-8674(93)90617-y. [DOI] [PubMed] [Google Scholar]
- 79.Janicic N, Soliman E, Pausova Z, Seldin MF, Riviere M, Szpirer J, Szpirer C, Hendy GN. Mapping of the calcium-sensing receptor gene (CASR) to human chromosome 3q13.3-21 by fluorescence in situ hybridization, and localization to rat chromosome 11 and mouse chromosome 16. Mamm Genome. 1995;6:798–801. doi: 10.1007/BF00539007. [DOI] [PubMed] [Google Scholar]
- 80.Aida K, Koishi S, Tawata M, Onaya T. Molecular cloning of a putative Ca2+-sensing receptor cDNA from human kidney. Biochem Biophys Res Commun. 1995;214:524–529. doi: 10.1006/bbrc.1995.2318. [DOI] [PubMed] [Google Scholar]
- 81.Ferry S, Traiffort E, Stinnakre J, Ruat M. Developmental and adult expression of rat calcium-sensing receptor transcripts in neurons and oligodendrocytes. Eur J Neurosci. 2000;12:872–884. doi: 10.1046/j.1460-9568.2000.00980.x. [DOI] [PubMed] [Google Scholar]
- 82.Vizard TN, O'Keeffe GW, Gutierrez H, Kos CH, Riccardi D, Davies AM. Regulation of axonal and dendritic growth by the extracellular calcium-sensing receptor. Nat Neurosci. 2008;11:285–291. doi: 10.1038/nn2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang Y, Awumey EK, Chatterjee PK, Somasundaram C, Bian K, Rogers KV, Dunn C, Bukoski RD. Molecular cloning and characterization of a rat sensory nerve Ca2+-sensing receptor. Am J Physiol Cell Physiol. 2003;285:C64–C75. doi: 10.1152/ajpcell.00543.2002. [DOI] [PubMed] [Google Scholar]
- 84.Rasschaert J, Malaisse WJ. Expression of the calcium-sensing receptor in pancreatic islet B-cells. Biochem Biophys Res Commun. 1999;264:615–618. doi: 10.1006/bbrc.1999.1577. [DOI] [PubMed] [Google Scholar]
- 85.Marie PJ. The calcium-sensing receptor in bone cells: a potential therapeutic target in osteoporosis. Bone. 2010;46:571–576. doi: 10.1016/j.bone.2009.07.082. [DOI] [PubMed] [Google Scholar]
- 86.Kameda T, Mano H, Yamada Y, Takai H, Amizuka N, Kobori M, Izumi N, Kawashima H, Ozawa H, Ikeda K, Kameda A, Hakeda Y, Kumegawa M. Calcium-sensing receptor in mature osteoclasts, which are bone resorbing cells. Biochem Biophys Res Commun. 1998;245:419–422. doi: 10.1006/bbrc.1998.8448. [DOI] [PubMed] [Google Scholar]
- 87.Rey O, Chang W, Bikle D, Rozengurt N, Young SH, Rozengurt E. Negative cross-talk between calcium-sensing receptor and β-catenin signaling systems in colonic epithelium. J Biol Chem. 2012;287:1158–1167. doi: 10.1074/jbc.M111.274589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Milara J, Mata M, Serrano A, Peiro T, Morcillo EJ, Cortijo J. Extracellular calcium-sensing receptor mediates human bronchial epithelial wound repair. Biochem Pharmacol. 2010;80:236–246. doi: 10.1016/j.bcp.2010.03.035. [DOI] [PubMed] [Google Scholar]
- 89.Xing WJ, Kong FJ, Li GW, Qiao K, Zhang WH, Zhang L, Bai SZ, Xi YH, Li HX, Tian Y, Ren H, Wu LY, Wang R, Xu CQ. Calcium-sensing receptors induce apoptosis during simulated ischaemia-reperfusion in Buffalo rat liver cells. Clin Exp Pharmacol Physiol. 2011;38:605–612. doi: 10.1111/j.1440-1681.2011.05559.x. [DOI] [PubMed] [Google Scholar]
- 90.Canaff L, Petit JL, Kisiel M, Watson PH, Gascon-Barre M, Hendy GN. Extracellular calcium-sensing receptor is expressed in rat hepatocytes. coupling to intracellular calcium mobilization and stimulation of bile flow. J Biol Chem. 2001;276:4070–4079. doi: 10.1074/jbc.M009317200. [DOI] [PubMed] [Google Scholar]
- 91.Sun J, Murphy E. Calcium-sensing receptor: a sensor and mediator of ischemic preconditioning in the heart. Am J Physiol Heart Circ Physiol. 2010;299:H1309–H1317. doi: 10.1152/ajpheart.00373.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sun YH, Liu MN, Li H, Shi S, Zhao YJ, Wang R, Xu CQ. Calcium-sensing receptor induces rat neonatal ventricular cardiomyocyte apoptosis. Biochem Biophys Res Commun. 2006;350:942–948. doi: 10.1016/j.bbrc.2006.09.142. [DOI] [PubMed] [Google Scholar]
- 93.Hammond CM, White D, Tomic J, Shi Y, Spaner DE. Extracellular calcium sensing promotes human B-cell activation and function. Blood. 2007;110:3985–3995. doi: 10.1182/blood-2007-05-088468. [DOI] [PubMed] [Google Scholar]
- 94.Guarnieri V, Valentina D'Elia A, Baorda F, Pazienza V, Benegiamo G, Stanziale P, Copetti M, Battista C, Grimaldi F, Damante G, Pellegrini F, D'Agruma L, Zelante L, Carella M, Scillitani A. CASR gene activating mutations in two families with autosomal dominant hypocalcemia. Mol Genet Metab. 2012;107:548–552. doi: 10.1016/j.ymgme.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 95.Forrest DL, Nevill TJ, Naiman SC, Le A, Brockington DA, Barnett MJ, Lavoie JC, Nantel SH, Song KW, Shepherd JD, Sutherland HJ, Toze CL, Davis JH, Hogge DE. Second malignancy following high-dose therapy and autologous stem cell transplantation: incidence and risk factor analysis. Bone Marrow Transplant. 2003;32:915–923. doi: 10.1038/sj.bmt.1704243. [DOI] [PubMed] [Google Scholar]
- 96.Thakker RV. Diseases associated with the extracellular calcium-sensing receptor. Cell Calcium. 2004;35:275–282. doi: 10.1016/j.ceca.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 97.Watanabe S, Fukumoto S, Chang H, Takeuchi Y, Hasegawa Y, Okazaki R, Chikatsu N, Fujita T. Association between activating mutations of calcium-sensing receptor and Bartter's syndrome. Lancet. 2002;360:692–694. doi: 10.1016/S0140-6736(02)09842-2. [DOI] [PubMed] [Google Scholar]
- 98.Li Y, Song YH, Rais N, Connor E, Schatz D, Muir A, Maclaren N. Autoantibodies to the extracellular domain of the calcium sensing receptor in patients with acquired hypoparathyroidism. J Clin Invest. 1996;97:910–914. doi: 10.1172/JCI118513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Manning AT, O'Brien N, Kerin MJ. Roles for the calcium sensing receptor in primary and metastatic cancer. Eur J Surg Oncol. 2006;32:693–697. doi: 10.1016/j.ejso.2006.03.047. [DOI] [PubMed] [Google Scholar]
- 100.Peters U, Chatterjee N, Yeager M, Chanock SJ, Schoen RE, McGlynn KA, Church TR, Weissfeld JL, Schatzkin A, Hayes RB. Association of genetic variants in the calcium-sensing receptor with risk of colorectal adenoma. Cancer Epidemiol Biomarkers Prev. 2004;13:2181–2186. [PubMed] [Google Scholar]
- 101.Yano S, Sugimoto T, Tsukamoto T, Chihara K, Kobayashi A, Kitazawa S, Maeda S, Kitazawa R. Decrease in vitamin D receptor and calcium-sensing receptor in highly proliferative parathyroid adenomas. Eur J Endocrinol. 2003;148:403–411. doi: 10.1530/eje.0.1480403. [DOI] [PubMed] [Google Scholar]
- 102.Chowdhury P, Pore D, Mahata N, Karmakar P, Pal A, Chakrabarti MK. Thermostable direct hemolysin down-regulates human colon carcinoma cell proliferation with the involvement of E-cadherin, and β-catenin/Tcf-4 signaling. PLoS One. 2011;6:e20098. doi: 10.1371/journal.pone.0020098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Whitfield JF. Calcium, calcium-sensing receptor and colon cancer. Cancer Lett. 2009;275:9–16. doi: 10.1016/j.canlet.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 104.Molostvov G, James S, Fletcher S, Bennett J, Lehnert H, Bland R, Zehnder D. Extracellular calcium-sensing receptor is functionally expressed in human artery. Am J Physiol Renal Physiol. 2007;293:F946–F955. doi: 10.1152/ajprenal.00474.2006. [DOI] [PubMed] [Google Scholar]
- 105.Marz W, Seelhorst U, Wellnitz B, Tiran B, Obermayer-Pietsch B, Renner W, Boehm BO, Ritz E, Hoffmann MM. Alanine to serine polymorphism at position 986 of the calcium-sensing receptor associated with coronary heart disease, myocardial infarction, all-cause, and cardiovascular mortality. J Clin Endocrinol Metab. 2007;92:2363–2369. doi: 10.1210/jc.2006-0071. [DOI] [PubMed] [Google Scholar]
- 106.Zhang J, Zhou J, Cai L, Lu Y, Wang T, Zhu L, Hu Q. Extracellular calcium-sensing receptor is critical in hypoxic pulmonary vasoconstriction. Antioxid Redox Signal. 2012;17:471–484. doi: 10.1089/ars.2011.4168. [DOI] [PubMed] [Google Scholar]
- 107.Yamamura A, Guo Q, Yamamura H, Zimnicka AM, Pohl NM, Smith KA, Fernandez RA, Zeifman A, Makino A, Dong H, Yuan JX. Enhanced Ca2+-sensing receptor function in idiopathic pulmonary arterial hypertension. Circ Res. 2012;111:469–481. doi: 10.1161/CIRCRESAHA.112.266361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Li GW, Xing WJ, Bai SZ, Hao JH, Guo J, Li HZ, Li HX, Zhang WH, Yang BF, Wu LY, Wang R, Yang GD, Xu CQ. The calcium-sensing receptor mediates hypoxia-induced proliferation of rat pulmonary artery smooth muscle cells through MEK1/ERK1,2 and PI3K pathways. Basic Clin Pharmacol Toxicol. 2011;108:185–193. doi: 10.1111/j.1742-7843.2010.00639.x. [DOI] [PubMed] [Google Scholar]
- 109.Li GW, Wang QS, Hao JH, Xing WJ, Guo J, Li HZ, Bai SZ, Li HX, Zhang WH, Yang BF, Yang GD, Wu LY, Wang R, Xu CQ. The functional expression of extracellular calcium-sensing receptor in rat pulmonary artery smooth muscle cells. J Biomed Sci. 2011;18:16. doi: 10.1186/1423-0127-18-16. [DOI] [PMC free article] [PubMed] [Google Scholar]