Abstract
Introduction and Objectives:
To prospectively document the perioperative complications of percutaneous nephrolithotomy (PCNL) using the modified Clavien grading system. Evaluation of complications and clearance rates according to stone complexity using the validated Guy's Stone Score (GSS) was also done.
Materials and Methods:
A total of 221 renal units underwent 278 PCNL procedures at a urology resident training center between September 2010 and September 2011 and data were recorded prospectively in our registry. Patients with co-morbidities like diabetes, renal failure, hypertension and cardiopulmonary diseases were excluded. Stone complexity was classified according to the GSS while peri-operative complications were recorded using the modified Clavien grading system.
Results:
Two hundred and forty-five complications were encountered in 278 PCNL procedures involving 116 renal units (41.72%). Complications of Grades 1, 2, 3a, 3b, 4a, 4b and 5 were seen in 52 (18.7%), 122 (43.8%), 42 (15.1%), 18 (6.4%), 6 (2.1%), 4 (1.4%) and 1 (0.3%) renal units respectively. There were 68, 98, 50 and 5 renal units in GSS I, II, III and IV groups, respectively. All grades of complications were more common in GSS III and IV (P<0.05). For GSS I, II, III and IV 100%, 74%, 56% and 0% of renal units, respectively, were stone-free after one session and 0%, 24%, 44% and 60% respectively needed two sessions to be stone-free.
Conclusion:
Although the complication rates were higher most were of low grade and self-limiting. Complications were significantly more common with higher GSS and the GSS effectively predicted stone-free rates.
Keywords: Complication, Guy's Stone Score, modified Clavien grading system, percutaneous nephrolithotomy
INTRODUCTION
Percutaneous nephrolithotomy (PCNL) is a well-established, minimally invasive treatment modality for the management of renal calculi. It is the first-line treatment option for large or multiple kidney stones and stones in the inferior calyx. Greater surgeon experience and improvements in instruments (i.e., flexible pyeloscopes and ureteroscopes) as well as lithotripsy technology (i.e., ultrasound/pneumatic devices, holmium/yttrium-aluminum-garnet laser) have increased the efficacy of PCNL, yielding stone-free rates of >90%.[1] However, PCNL is not without complications with a recent multi-center study showing the overall complication rate of 20.5%.[2] Complication rates as high as up to 83% have also been reported.[3]
Earlier there was no consensus on how to define complications and stratify them by severity. This hampered comparison of outcome data and generated difficulties in informing patients about complications. A new classification (modified Clavien system) has been proposed to grade perioperative complications of general surgery and has been validated in a cohort of 6336 patients.[4] The same classification system has recently been used by urologists to grade perioperative complications following radical prostatectomy,[5] laparoscopic live donor nephrectomy,[6] laparoscopic pyeloplasty,[7] laparoscopic and open partial nephrectomy[8] and most recently Transurethral Resection of Prostate.[9] Results of this new classification to grade complications after PCNL have also been described.[10–12]
The rate of complications in PCNL can vary according to the complexity of stone disease. Calculi are generally classified into simple or complex, or into pelvic or caliceal based on location, or into single or multiple. However, none of the above mentioned classification systems could become a standard method due to the inherent fallacies of each system and also their inability to successfully predict outcome after PCNL. Thus to avoid the gray zones in the classification system and for predicting outcomes after PCNL, Guy's Stone Score (GSS) was conceived, validated and found to be an easy, reproducible and reliable method for describing the nature of calculi and predicting the stone-free rates.
Most previous studies describing the complications of PCNL using the modified Clavien system have described the complexity of stone disease using a simple classification system. We report our perioperative complications of PCNL according to the modified Clavien system in which the stone complexity has been classified using the validated GSS. We have compared complications amongst various GSSs. We have also have compared GSSs with stone-free rates after PCNL.
MATERIALS AND METHODS
Data of all patients (n=262) operated between September 2010 and September 2011 were entered and maintained prospectively in our registry. Ethical clearance for this study was obtained from the Institutional Review Board. Co-morbidities such as renal insufficiency (n=22), diabetes (n=16), hypertension (n=20) or cardiopulmonary diseases (n=4) further increase the risk of complications and therefore patients with these problems were excluded from analysis;[13–15] as a result 200 patients were included in the study. Preoperative complete blood count, serum creatinine, bleeding and coagulation profile, and urine cultures were obtained from all patients. Radiologic evaluation included X-ray Kidney Ureter and Bladder (KUB), intravenous urography (IVU) and ultrasonography of KUB and Non Contrast Computerised Tomography (NCCT) if needed. NCCT scan was performed in cases with radiolucent calculus, in a few patients with Grade III and IV calculus, and in all patients (n=13) with abnormal anatomy. The stone burden was determined by radiographic studies, and stones were classified using the GSS as Guy's I, II, III and IV.[16] The score comprised four grades: Grade I, solitary stone in mid/lower pole or solitary stone in the pelvis with simple anatomy; Grade II, solitary stone in the upper pole or multiple stones in a patient with simple anatomy or a solitary stone in a patient with abnormal anatomy; Grade III, multiple stones in a patient with abnormal anatomy or stones in a caliceal diverticulum or partial staghorn calculus, and Grade IV, staghorn calculus or any stone in a patient with spina bifida or spinal injury.
Patient underwent PCNL as per the standard protocol after ensuring sterile urine.[17] Cystoscopy and insertion of a ureteral catheter were the initial step. Patients were then placed prone and percutaneous access was obtained using C-armed fluoroscopy and air pyelogram.[18] Tract was dilated with Alken's serial dilator (Karl Storz) and a 28/30 F or 30/34 F Amplatz sheath was placed. Nephroscopy was performed with a rigid, 26F rigid nephroscope (Karl Storz). Calculi were identified and fragmented with pneumatic lithoclast. Stone clearance was confirmed intra-operatively by fluoroscopy. If needed, another puncture was made or the method of intra-operative percutaneous caliceal irrigation[19] (IPCI) was used to achieve stone clearance. Double-J stent was placed using the antegrade approach at the end of the procedure, if needed. An external ureteral catheter was left in situ if the patient was planned for relook PCNL or if DJ stent placement was not done. A 20F nephrostomy tube was placed into the renal pelvis or the punctured calyx at the end of the procedure in most of the cases. The PCNL procedure was performed by either consultants or urology residents.
Antibiotic prophylaxis was given to all the patients. Fever of >100° F was considered significant. Serum creatinine levels and blood counts were obtained in all patients postoperatively. On postoperative Day 1, plain film of the kidneys, ureters, and bladder was obtained. If complete stone clearance was documented and the urine was not significantly hematuric, the nephrostomy tube was removed. After 12 h, if there was no urine leak from the nephrostomy site the urethral Foley and ureteral catheters were removed. If urine leak persisted for more than 24 h than DJ stent placement was done. DJ stent if placed, was removed after three to four weeks. If residual fragments were seen on postoperative X-ray, then re-look PCNL using either the same tract or new tract was done after two to four days. Although all patients needing intervention under general anesthesia is considered a Grade 3b complication, it was not considered a complication in the present study and has been mentioned separately. All patients were then followed up at one week and at one month after discharge from the hospital. The PCNL procedure was considered successful if the patient was either stone-free or had any clinically significant residual stones (CIRFs), defined as <4 mm, non- obstructive, non-infectious, and asymptomatic residual fragments.[20]
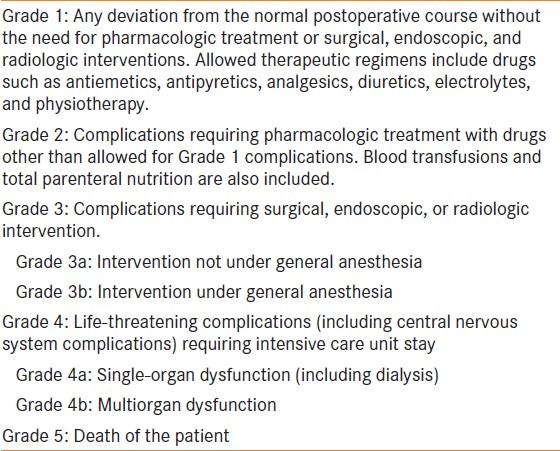
Data recorded included the age, sex, stone complexity score according to GSS, clearance after first and second session, mean number of punctures, site of punctures, and mean duration of surgery. The modified Clavien grading system [Table 1] was used for evaluating perioperative and postoperative complications of PCNL.[10] Complications in the same patient undergoing re-look procedures were counted independently as separate complications.
Table 1.
Classification of surgical complications according to the modified Clavien system[10]
Statistical analysis
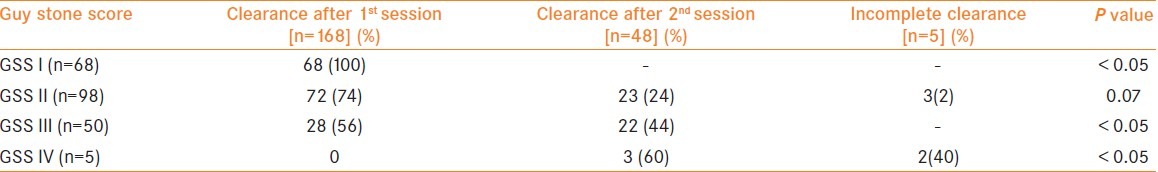
The data were entered into an Excel™ (Microsoft, Redmond, WA) database and analyzed with an EPI-Info statistical software package. Complication rates of various GSS grades [Table 2] and stone-free rates [Table 3] were compared using the chi-square test. P value < 0.05 was considered statistically significant. Due to lesser number of cases in GSS IV (n=5), it was combined with GSS III (n=50) for statistical analysis of complication rates with various GSS grades.
Table 2.
Comparison of complications classified according to the modified Calvien system between and calculi classified according to GSS
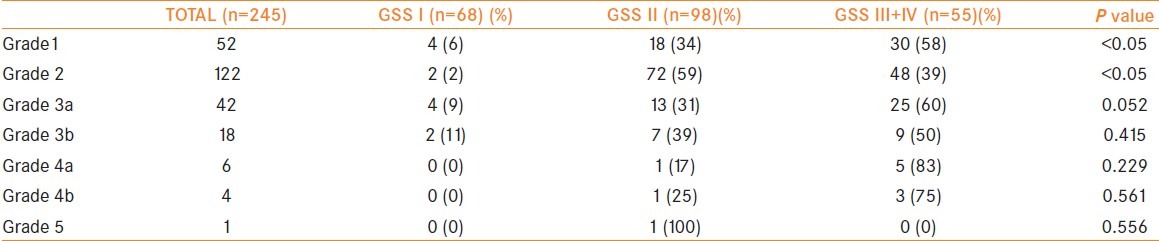
Table 3.
Comparison between GSS and stone-free rates
RESULTS
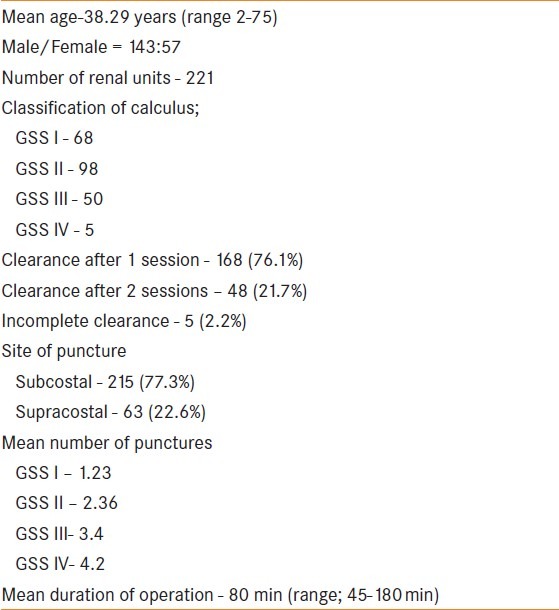
Descriptive data of the cohort are summarized in Table 4. Two hundred and sixty-two consecutive patients underwent PCNL during the study period and after exclusion 200 patients were included in the study. Because 21 patients had bilateral stone disease and were treated by PCNL in the same admission the total number of renal units treated were 221. According to the GSS there were 68, 98, 50 and 5 patients in GSS I, II, III and IV groups, respectively. GSS I (n=68) included 34 pelvic, 8 mid-pole and 26 inferior pole calculi. GSS II (n=98) included 70 multiple calculi, 20 upper-polar calculi and single pelvic calculus with pelviureteric junction obstruction in 5, horseshoe kidney in 2 and polycystic kidney disease in 1 renal unit respectively. GSS III (n=50) included 45 partial staghorn calculi and multiple renal calculi with pelviureteric junction obstruction in 3, and horseshoe kidney in 2 renal units respectively. All renal units in GSS IV (n=5) had complete staghorn calculus. In 168 renal units one session of PCNL were required, while in 48 renal units two sessions of PCNL were required to achieve stone free status.In 5 renal units complete clearance could not be achieved even after a total of 14 procedures (2 renal units each required 2 and 3 PCNL procedures respectively and 1 renal unit needed 4 procedures) were performed. Thus, overall 278 PCNL procedures were performed. In 29 (10.43%) of renal units clinically insignificant residual fragments (CIRFs) remained (considered successful).
Table 4.
Descriptive data of patients (n = 200)
Two hundred and forty-five complications were seen in 278 PCNL procedures involving 116 renal units (41.72%); these are elaborated in Table 5.
Table 5.
Complications of PCNL classified according to modified Clavien system
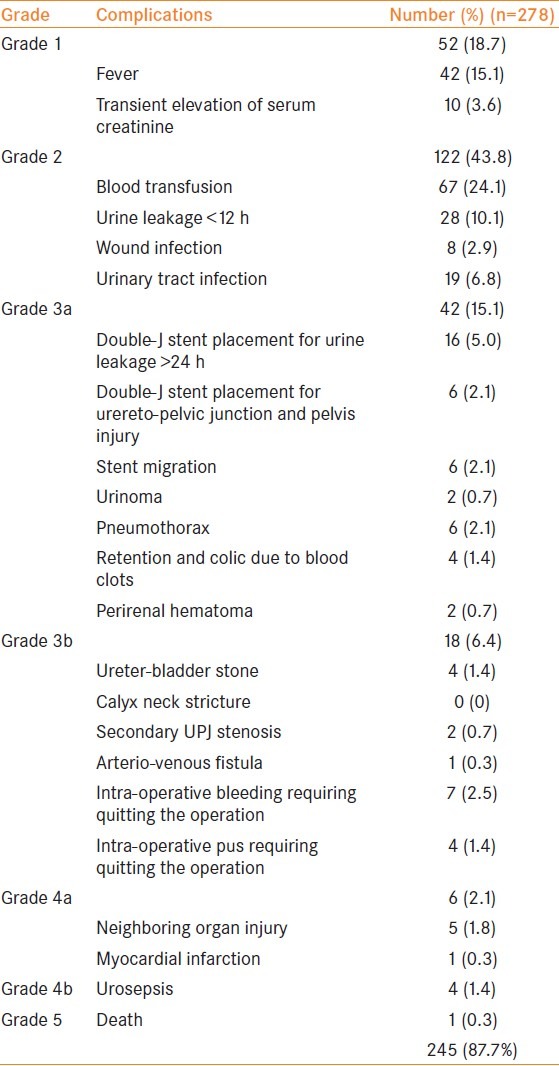
The occurrence of complications in patients with various GSS grades was compared and is shown in Table 4. All grades of complications were more common in patients with GSS III and IV (P<0.05). Comparison was also done between GSS and stone-free rates (SFRs) in Table 5. For renal units with GSS I, II, III and IV, 100%, 74%, 56% and 0% of renal units respectively were stone-free after one session while 0%, 24%,44% and 60% of renal units respectively needed two sessions to become stone-free.
DISCUSSION
In spite of the high success rates, percutaneous renal surgery involves serious complications such as blood loss, adjacent organ injuries and life-threatening infections.[11,13] In a large multicentric study,[3] retrospective analysis of complications in >1000 PCNL procedures was performed and the complications were stratified into minor or major. Minor complications reported were extravasation (7.2%), transfusion (11.2–17.5%), and fever (21.0–32.1%), whereas major complications were septicemia (0.3–4.7%) and colonic (0.2–0.8%) or pleural injury (0.0–3.1%). However, terms such as minor and major are not standardized and therefore, an informative comparison of complications is difficult. Modified Clavien grading system, has been shown to be a reliable tool for more objective outcome comparisons after renal stone treatment.[9–12,21] Complications stratified as Clavien Grade 1 and 2 are considered as minor while Grades 3, 4, and 5 are considered major according to other classification systems.[3] However, the modified Clavien system is more objective and reproducible, representing a compelling tool for quality assessment and allows comparison of results between various studies.
The overall complication rate of 41.7% seen in our patients is much higher than that reported in a large multi-center study[2] of 5724 PCNL procedures, which reported a rate of 20.5% (in 1175 patients out of a total of 5724 patients). One reason for this difference could be that many of the procedures performed in our group of patients were by trainee residents. It is a well-known fact the complications are higher during the learning phase.[22,23] Another reason could be the prospective evaluation of the complications by a single observer (SM) as opposed to retrospective data in other studies.
Complications of Grade II severity were most common in our patients. Bleeding, necessitating blood transfusion was the most common individual complication, observed in 24% (67 out of 278) of procedures and was much higher in comparison to the 5.7% reported in the recent multicentric study by the CROES (Clinical Research Office of the Endourological Society) group.[12] However, an overall blood transfusion rate ranging from 5–18% has been reported in the literature.[24–28] This high rate of transfusion can be explained by the increased incidence of multiple calculus (n=70), staghorn calculi (n=50) and calculi in abnormal renal anatomy (n=13) in the present study, necessitating multiple percutaneous accesses and also due to the learning curve of residents.Another reason was that 172 out 200 patients had a mean preoperative blood hemoglobin level of less than 11 (range: 9–12.5 g%) and also had poor body reserve[29] (common in poor countries). Postoperative blood transfusion was done when hemoglobin dropped below 8 g/dl (because of low preoperative hemoglobin and also due to intra-operative blood loss). Blood transfusion rates also varied based on GSS as 3%, 15%, 72% and 100% of renal units with GSS I, II, III, and IV, respectively, required transfusion. High transfusion in GSS III and IV were probably due to the fact that most of these patients were managed by multiple punctures and also needed re-look procedures (n=48). Most of our patients prefer only PCNL for complete clearance and do not opt for extracorporeal shock wave lithotripsy (ESWL) for residual stones due to limited access to healthcare, financial restraints, and the inability of ESWL to predict stone fragmentation and clearance of a particular stone by observing its radiological image. Therefore, sometimes separate puncture had to be made for removal of even a single small stone lodged in an inaccessible calyx. In another seven (2.5%) patients the operation had to be terminated due to severe bleeding (Grade 3b complication) leading to hemodynamic instability and poor visualization. One patient (0.3%) needed angio-embolization for control of bleeding.
Fever in the postoperative period was the second most common complication (after blood transfusion) and was seen in 15.1% of procedures. The reported incidence of fever after PCNL has varied from as low as 2.8%[11] to as high as 27.6%[30] (usually between 6.5--13%[12,16,23]) and can be because of different patient populations and the policy regarding the use of antibiotics. Furthermore, fever due to other complications such as urinary tract infection (UTI), wound infection, urinoma, perinephritic abscess and urosepsis, as well as a side-effect of blood transfusion were not included in this group (they are classified separately into other categories, see Table 5). Factors predisposing to fever after PCNL include preexisting untreated UTI, infected urinary stones,[31] renal insufficiency,[32] duration of surgery (< 90 min),[33] amount and pressure of irrigation fluid.[31]
Wound infection occurred in eight renal units. All of them had pyonephrosis for which preoperative nephrostomy tube was placed for a long duration before undergoing PCNL. Wound infection was referred to as the infection of the skin and subcutaneous tissue at the nephrostomy site. All cases responded to proper cleaning, application of povidine iodine, and removal of nephrostomy tube after PCNL. The procedure had to be abandoned in four patients due to unsuspected intra-operative finding of pyonephrosis. The reason why pyonephrosis was missed could be because the clinical picture of sepsis was absent due to previous antibiotic intake and could also be because ultrasonography is an operator-dependent investigation.
Pleural injury was seen in five (1.8%) renal units. These patients had supra-costal puncture and constituted 8% of all supra-costal punctures. This is in concordance with the literature that reports 3-7% risk of pleural injury in supra-costal punctures.[34–36]
Major or significant complications were generally uncommon. Skolarikos and de la Rosette[32] in a current review with a systematic search for manuscripts on classification and grading of PCNL-related complications have reported that the frequency of major complications after PCNL was 0.9–4.7% for septicemia, 0.6–1.4% for renal hemorrhage necessitating intervention, 2.3–3.1% for pleural injury, and 0.2–0.8% for colonic injury. In our series frequency of urosepsis/septicemia, pleural effusion and renal hemorrhage necessitating intervention were reported in 1.4%, 2.1% and 0.3% respectively, and colonic injury was not reported. Septicemia can occur as a result of infection introduced via the access to the kidney or if the stones are infected.
Low number of cases in GSS IV (n=5) was not due to the fact that complete staghorn calculi are rare in our setting but maybe because some of them undergo anatropic pyelolithotomy (eight patients underwent this procedure in the same time period).
We excluded patients with co-morbidities because co-morbidity acts as a confounding factor leading to higher complications rates in this group of patients. We were justified because the latest study on Carlson's co-morbidity index[37] showed that preoperative co-morbidities increase the risk of postoperative complication after PCNL.
Surgical complications can be reported in a variety of ways, and the means through which data are obtained and reported probably have as much impact on the “complication rate” as the procedure.[38] At first glance, one might be surprised by the fairly high incidence of complications reported; however, the reader who is familiar with the Clavien system will recognize that the vast majority of complications are minor in severity and would not have been reported if a non-standardized reporting system had been used.[38]
As in a previous study by Thomas et al.,[16] the GSS accurately predicted the SFR after PCNL in our study also. It was an easy-to-use, reproducible, objective and reliable method for describing the complexity of stones and predicting the SFR after PCNL. All renal units with GSS I were stone-free after one session of PCNL, GSS II needed one session in 74% and two session in 24% renal units, GSS III needed one session in 56% and two session in 44% renal units and GSS IV needed two session in 60% renal units and remaining 40% renal units could not be made stone free inspite of multiple sessions.Therefore increasing stone complexity led to decreasing stone clearance rates.
The prospective nature of this study is the biggest strength of the present study as most studies documenting the post-PCNL complications according to modified Clavien grading are retrospective in nature. To the best of our knowledge, the present study is also the first to compare complications of PCNL using the modified Clavien grading system with GSS [Table 2]. GSS and stone-free rates were also compared [Table 3]. Our study is also the first study to externally validate the ability of GSS to predict stone-free rates.
The limitations of the present study are the small sample size and the non-blinded study protocol.
CONCLUSION
In this study involving a relatively lesser number of cases from a tertiary care and resident training institute, the complication rate following PCNL was 41.7%. Grade 1, 2 and 3 complications, which were managed conservatively or by minimally invasive endourological procedures constituted the main bulk of complications (>90%) while Grade 4 and 5 complications were less common. Complications of all grades were more common with higher GSS. The GSS also predicted the stone-free rates, with higher GSS more often needing second-look procedures for complete clearance.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Turk C, Knoll T, Petrik A, Sarica K, Straub M, Seitz C. Guidelines on urolithiasis. Eur Assoc Urol. 2010:1–106. [Google Scholar]
- 2.Labate G, Modi P, Timoney A, Cormio L, Zhang X, Louie M, et al. The percutaneous nephrolithotomy global study: Classification of complications. J Endourol. 2011;25:1275–80. doi: 10.1089/end.2011.0067. [DOI] [PubMed] [Google Scholar]
- 3.Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol. 2007;51:899–906. doi: 10.1016/j.eururo.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 4.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of a 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rabbani F, Herran Yunis L, Pinochet R, Nogueira L, Vora KC, Eastham JA, et al. Comprehensive standardized report of complications of retropubic and laparoscopic radical prostatectomy. Eur Urol. 2010;57:371–86. doi: 10.1016/j.eururo.2009.11.034. [DOI] [PubMed] [Google Scholar]
- 6.Ramasamy R, Afaneh C, Katz M, Chen X, Aull MJ, Leeser DB, et al. Comparison of complications of laparoscopic versus laparo-endoscopic single site donor nephrectomy using the modified clavien grading system. J Urol. 2011;186:1386–90. doi: 10.1016/j.juro.2011.05.053. [DOI] [PubMed] [Google Scholar]
- 7.Szydełko T, Kasprzak J, Apoznañski W, Tupikowski K, Pupka A, Janczak D, et al. Clavien classification of complications after 150 laparoscopic pyeloplasties. Urology. 2011;77:1359–64. doi: 10.1016/j.urology.2010.12.025. [DOI] [PubMed] [Google Scholar]
- 8.Ramasamy R, Reifsnyder J, Shin B, DiPietro J, Shariat S, Pizzo JD. Laparoscopic and open partial nephrectomy: Comparison of complications using clavien grading system. J Urol. 2011;85:e610. [Google Scholar]
- 9.Mamoulakis C, Efthimiou I, Kazoulis S, Christoulakis I, Sofras F. The modified Clavien classification system: A standardized platform for reporting complications in transurethral resection of the prostate. World J Urol. 2011;29:205–10. doi: 10.1007/s00345-010-0566-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morgan M, Smith NS, Thomas K, Murphy DG. Is Clavien the new standard for reporting urological complications? BJU Int. 2009;104:434–6. doi: 10.1111/j.1464-410X.2009.08516.x. [DOI] [PubMed] [Google Scholar]
- 11.Tefekli A, Ali Karadag M, Tepeler K, Sari E, Berberoglu Y, Baykal M, et al. Classification of percutaneous nephrolithotomy complications using the modified Clavien grading system: Looking for a standard. Eur Urol. 2008;53:184–90. doi: 10.1016/j.eururo.2007.06.049. [DOI] [PubMed] [Google Scholar]
- 12.Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpaet R, et al. The clinical research office of the endourological society percutaneous nephrolithotomy global study: Indications, complications, and outcomes in 5803 patients. J Endourol. 2011;25:11–7. doi: 10.1089/end.2010.0424. [DOI] [PubMed] [Google Scholar]
- 13.Patel SR, Haleblian GE, Pareek G. Percutaneous nephrolithotomy can be safely performed in the high-risk patient. Urology. 2010;75:51–5. doi: 10.1016/j.urology.2009.06.064. [DOI] [PubMed] [Google Scholar]
- 14.Duvdevani M, Nott L, Ray AA, Ko R, Denstedt JD, Razvi H. Percutaneous nephrolithotripsy in patients with diabetes mellitus. J Endourol. 2009;23:21–6. doi: 10.1089/end.2008.0282. [DOI] [PubMed] [Google Scholar]
- 15.Kukreja R, Desai M, Patel S, Desai MR. Factors affecting blood loss during percutaneous nephrolithotomy: Prospective study. J Endourol. 2004;18:715–22. doi: 10.1089/end.2004.18.715. [DOI] [PubMed] [Google Scholar]
- 16.Thomas K, Smith NC, Hegarty N, Glasse JM. The Guy's stone score—Grading the complexity of percutaneous nephrolithotomy procedures. Urology. 2011;77:277–81. doi: 10.1016/j.urology.2010.12.026. [DOI] [PubMed] [Google Scholar]
- 17.Knoll T, Michel MS, Alken P. Percutaneous nephrolithotomy: The Mannheim technique. BJU Int. 2007;99:213–31. doi: 10.1111/j.1464-410X.2007.06613.x. [DOI] [PubMed] [Google Scholar]
- 18.Lipkin ME, Mancini JG, Zilberman DE, Raymundo ME, Yong D, Ferrandino MN, et al. Reduced radiation exposure with the use of an air retrograde pyelogram during fluoroscopic access for percutaneous nephrolithotomy air pyelogram. J Endourol. 2011;4:563–7. doi: 10.1089/end.2010.0431. [DOI] [PubMed] [Google Scholar]
- 19.Ahlawat R, Dalela D. Intra-operative percutaneous caliceal irrigation--a technique for clearing caliceal residue during percutaneous surgery. Br J Urol. 1993;72:990. doi: 10.1111/j.1464-410x.1993.tb16329.x. [DOI] [PubMed] [Google Scholar]
- 20.Muslumanoglu AY, Tefekli A, Karadag MA, Tok A, Sari E, Berberoglu Y. Impact of percutaneous access point number and location on complication and success rates in percutaneous nephrolithotomy. Urol Int. 2006;77:340–6. doi: 10.1159/000096339. [DOI] [PubMed] [Google Scholar]
- 21.de la Rosette JJ, Zuazu JR, Tsakiris P, Elsakka AM, Zudaire JJ, Laguna MP, et al. Prognostic factors and percutaneous nephrolithotomy morbidity: A multivariate analysis of a contemporary series using the Clavien classification. J Urol. 2008;180:2489–93. doi: 10.1016/j.juro.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 22.de la Rosette JJ, Laguna MP, Rassweiler JJ, Conort P. Training in percutaneous nephrolithotomy–a critical review. Eur Urol. 2008;54:994–1001. doi: 10.1016/j.eururo.2008.03.052. [DOI] [PubMed] [Google Scholar]
- 23.Tanriverdi O, Boylu U, Kendirci M, Kadihasanoglu M, Horasanli K, Miroglu C. The learning curve in the training of percutaneous nephrolithotomy. Eur Urol. 2007;52:206. doi: 10.1016/j.eururo.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 24.Netto NR, Jr, Ikonomodis J, Ikari O, Claro JA. Comparative study of percutaneous access for staghorn calculi. Urology. 2005;65:659–63. doi: 10.1016/j.urology.2004.10.081. [DOI] [PubMed] [Google Scholar]
- 25.Kim SC, Kuo RL, Lingeman JE. Percutaneous nephrolithotomy: An update. Curr Opin Urol. 2003;13:235–41. doi: 10.1097/00042307-200305000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Liatsikos EN, Kapoor R, Lee B, Jabbour M, Barbalias G, Smith AD. “Angular percutaneous renal access”. Multiple tracts through a single incision for staghorn calculous treatment in a single session. Eur Urol. 2005;48:832–7. doi: 10.1016/j.eururo.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Srivastava A, Singh KJ, Suri A, Dubey D, Kumar A, Kapoor R, et al. Vascular complications after percutaneous nephrolithotomy: Are there any predictive factors? Urology. 2005;66:38–40. doi: 10.1016/j.urology.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 28.Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS. Chapter 1: AUA guideline on management of staghorn calculi: Diagnosis and treatment recommendations. J Urol. 2005;173:1991–2000. doi: 10.1097/01.ju.0000161171.67806.2a. [DOI] [PubMed] [Google Scholar]
- 29.Larke A, Crews DE. Parental investment, late reproduction, and increased body reserve capacity are associated with longevity in humans. J Physiol Anthropol. 2006;25:119–31. doi: 10.2114/jpa2.25.119. [DOI] [PubMed] [Google Scholar]
- 30.Osman M, Wendt-Nordahl G, Heger K, Michel MS, Alken P, Knoll T. Percutaneous nephrolithotomy with ultrasonography- guided renal access: Experience from over 300 cases. BJU Int. 2005;96:875–8. doi: 10.1111/j.1464-410X.2005.05749.x. [DOI] [PubMed] [Google Scholar]
- 31.Takeuchi H, Ueda M, Nonomura M, Nishio Y, Nishimura K, Hida S, et al. Fever attack in percutaneous nephrolithotomy and transurethral ureterolithotripsy. Hinyokika Kiyo. 1987;33:1357–63. [PubMed] [Google Scholar]
- 32.Skolarikos A, de la Rosette J. Prevention and treatment of complications following percutaneous nephrolithotomy. Curr Opin Urol. 2008;18:229–34. doi: 10.1097/MOU.0b013e3282f46afc. [DOI] [PubMed] [Google Scholar]
- 33.Dogan HS, Sahin A, Cetinkaya Y, Akdogan B, Ozden E, Kendi S. Antibiotic prophylaxis in percutaneous nephrolithotomy: Prospective study in 81 patients. J Endourol. 2002;16:649–53. doi: 10.1089/089277902761402989. [DOI] [PubMed] [Google Scholar]
- 34.Raza A, Moussa S, Smith G, Tolley DA. Upper-pole puncture in percutaneous nephrolithotomy: A retrospective review of treatment safety and efficacy. BJU Int. 2008;101:599–602. doi: 10.1111/j.1464-410X.2007.07388.x. [DOI] [PubMed] [Google Scholar]
- 35.Aron M, Yadav R, Goel R, Kolla SB, Gautam G, Hemal AK, et al. Multi-Tract Percutaneous Nephrolithotomy for Large Complete Staghorn Calculi. Urol Int. 2005;75:327–32. doi: 10.1159/000089168. [DOI] [PubMed] [Google Scholar]
- 36.Gupta R, Kumar A, Kapoor R, Srivastava A, Mandhani A. Prospective evaluation of safety and efficacy of the supracostal approach for percutaneous nephrolithotomy. BJU Int. 2002;90:809–13. doi: 10.1046/j.1464-410x.2002.03051.x. [DOI] [PubMed] [Google Scholar]
- 37.Unsal A, Resorlu B, Atmaca AF, Akif Diri A, Goktug HN, Can CE, et al. Prediction of morbidity and mortality after percutaneous nephrolithotomy by using the Charlson Comorbidity Index. Urology. 2012;79:55–60. doi: 10.1016/j.urology.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 38.Graefen M. The modified clavien system: A plea for a standardized reporting system for surgical complications. Eur Urol. 2010;57:387–9. doi: 10.1016/j.eururo.2009.12.020. [DOI] [PubMed] [Google Scholar]


