Abstract
Refractory bleeding following percutaneous nephrolithotomy (PCNL) is mainly due to formation of pseudoaneurysm. Transarterial embolization is required to control the bleeding in such cases. We report a case of post-PCNL hematuria in whom angioembolization was done. An early erosion of the embolization coil from the renal vasculature into the urinary collecting system occurred, causing urinary tract obstruction and urinary tract infection (UTI). The coil was retrieved ureteroscopically after control of UTI with antibiotics. Migration of embolization coil into urinary collecting system is a rare but important cause of urinary tract obstruction. The treating physician as well as the patient should be aware of this complication.
Keywords: Angioembolization, migrated coil, pseudoaneurysm
INTRODUCTION
Hemorrhage after percutaneous nephrolithotomy (PCNL) is a significant complication that occurs in a small percentage of cases. Hemorrhage may be venous or arterial. Venous hemorrhage is usually managed conservatively.[1,2] However, arterial injuries sometimes require transarterial embolization to control the refractory bleeding. In patient presenting with refractory bleeding, pseudoaneurysm formation is the most common cause with a reported incidence of 0.6-1%.[3,4] Super-selective angioembolization is a safe and effective procedure with minimal complications.[5,6] We report a case of early erosion of an embolization coil from the renal vasculature into the urinary collecting system causing urinary tract obstruction and urosepsis.
CASE REPORT
A 23-year-old male underwent left URS and PCNL for a left upper ureteric calculus and a 2.5-cm lower pole renal calculus in a community hospital in December, 2010. One week after nephrostomy tube removal, the patient experienced gross hematuria with clot retention. The patient underwent endoscopic bladder clot evacuation and DJ stent removal in the same hospital. Two weeks later, again he developed gross hematuria with fever and a significant decrease in hematocrit. After resuscitation the patient was referred to our centre. On angiography, there was a pseudoaneurysm in the lower segmental renal artery. Three 6-mm coils were positioned proximal and distal to the neck of the pseudoaneurysm. A check angiogram demonstrated no leak of contrast. Postembolization recovery was uneventful.
After 3 months of embolization, the patient presented with high-grade fever, left flank pain and burning micturiton. On X-ray KUB 2 coils were seen in left renal area, whereas 1 coil was seen in L3 transverse process area. Ultrasonography revealed left moderate hydroureteronephrosis till upper 1/3 of ureter. Axial noncontrast and contrast-enhanced CT images showed left hydronephrosis with dilated upper ureter and an embolization coil in the upper ureter [Figure 1]. Urosepsis was controlled with antibiotics. Subsequently the patient underwent left ureteroscopic removal of the embolization coil. He was discharged on postoperative day 1.
Figure 1.
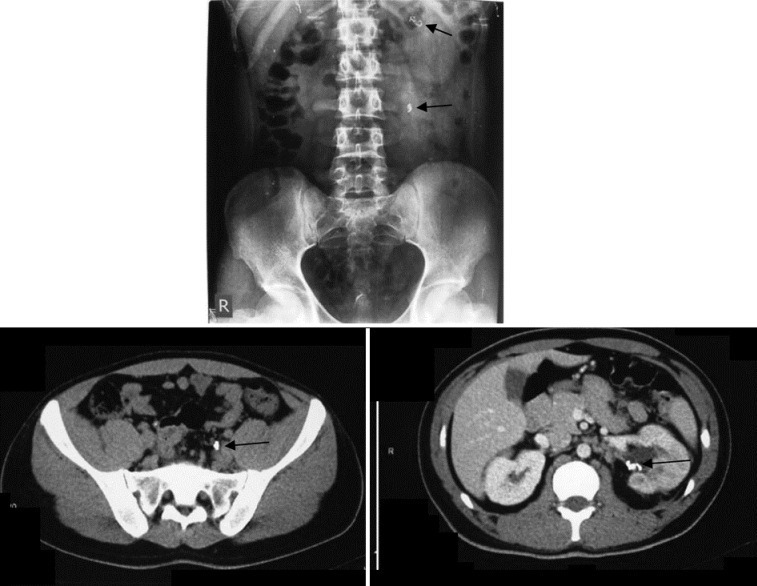
X ray KUB shows 2 coils in left renal area, 1 coil in L3 transverse process area. CT Urogram shows left hydronephrosis with dilated upper ureter and 2 coils in left kidney &1 coil in upper ureter
DISCUSSION
In 1975, angioembolization for renal pseudoaneurysm was reported in a human patient when an autologous blood clot was used to embolize a bleeding pseudoaneurysm as a temporary measure before nephrectomy.[7]
Coil embolization of pseudoaneurysm is the safe procedure without significant long-term complications. Coil erosion or migration into the collecting system is a rare phenomenon. We found only three case reports in which embolization coil migrated to the collecting system.[8–10] In all these case reports the coil eroded after 1 year following embolization. All the three patients presented with hematuria and renal colic. In our case, patient presented early (3 months) with complaints of renal colic and persistent fever after coil embolization.
Hypothetically three mechanisms of coil erosion have been proposed.[10] First, the diameter of arteriocaliceal communication might be larger than the embolization coil, and the coil gets extruded through the communication soon after placement. Second, the arteriocaliceal communication could get dilated over time because of inflammation due to infection or the constant irritation from the indwelling coil itself, leading to eventual erosion into the collecting system. Finally, rupture of the weakened wall of a pseudoaneurysm exposed to high arterial pressure may lead to erosion. According to the first hypothesis, if the arteriocaliceal communication was larger than the embolization coil than all three coils would have extruded through the communication and gross hematuria would have reappeared. The third mechanism would have lead to massive hematuria in addition to the coil migration. In this case the patient presented with high-grade fever and left flank pain but not hematuria. Therefore in this case the second mechanism seems to be the most likely cause of erosion of the embolization coil.
CONCLUSIONS
One of the important but rare causes of urinary tract obstruction is the migration of embolization coil into urinary collecting system. The treating physician should have knowledge of this complication. He should inform the patient as well.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ngo TC, Lee JJ, Gonzalgo ML. Renal pseudoaneurysm: An overview. Nat Rev Urol. 2010;7:619–25. doi: 10.1038/nrurol.2010.163. [DOI] [PubMed] [Google Scholar]
- 2.Ramchandani P, Cardella JF, Grassi CJ, Roberts AC, Sacks D, Schwartzberg MS, et al. SCVIR Standards of Practice Committee.Quality improvement guidelines for percutaneous nephrostomy. J Vasc Interv Radiol. 2001;12:1247–51. doi: 10.1016/s1051-0443(07)61546-2. [DOI] [PubMed] [Google Scholar]
- 3.Kessaris DN, Bellman GC, Pardalidis NP, Smith AG. Management of hemorrhage after percutaneous renal surgery. J Urol. 1995;153:604–8. doi: 10.1097/00005392-199503000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Jain R, Kumar S, Phadke RV, Baijal SS, Gujral RB. Intra-arterial embolization of lumbar artery pseudoaneurysm following percutaneous nephrolithotomy. Australas Radiol. 2001;45:383–6. doi: 10.1046/j.1440-1673.2001.00880.x. [DOI] [PubMed] [Google Scholar]
- 5.Basiri A, Najjaran Toussi V, Mohammadi Sichani M, Ardestani Zadeh A. Spontaneous resolution of severe hemorrhagic intrarenal pseudoaneurysm after percutaneous nephrolithotomy. Urol J. 2010;7:10–1. [PubMed] [Google Scholar]
- 6.Tan TJ, Teh HS, Pua U, Ho SH. Endovascular management of iatrogenic renal vascular injuries complicating percutaneous nephrolithotripsy: Role of renal angiography and superselective coil embolisation. J HK Coll Radiol. 2008;11:103–7. [Google Scholar]
- 7.Adler O, Rosenberger A. Autologous blood clot embolisation into a bleeding renal artery pseudoaneurysm. Radiol Clin (Basel) 1975;44:601–6. [PubMed] [Google Scholar]
- 8.Blaut S, Zecha H, Schneider M, Druschel S, Werner M, Lohmann J, et al. Foreign body in proximal ureter after selective embolisation of a renal artery. Urologe A. 2008;47:1607–10. doi: 10.1007/s00120-008-1886-z. [DOI] [PubMed] [Google Scholar]
- 9.Rutchik S, Wong P. Migration of arterial embolization coils as nidus for renal stone formation. J Urol. 2002;167:2520. [PubMed] [Google Scholar]
- 10.Reed A, Suri R, Marcovich R. Passage of embolization coil through urinary collecting system one year after embolization. Urology. 2007;70:1222.e17–18. doi: 10.1016/j.urology.2007.09.007. [DOI] [PubMed] [Google Scholar]


