Abstract
Nicotine addiction accounts for 4.9 million deaths each year. Furthermore, although smoking represents a significant health burden in the United States, at present there are only three FDA-approved pharmacotherapies currently on the market: (1) nicotine replacement therapy, (2) bupropion, and (3) varenicline. Despite this obvious gap in the market, the complexity of nicotine addiction in addition to the increasing cost of drug development makes targeted drug development prohibitive. Furthermore, using combinations of mouse and human studies, additional treatments could be developed from off-the-shelf, currently approved medication lists. This article reviews translational studies targeting manipulations of the cholinergic system as a viable therapeutic target for nicotine addiction.
Nearly 80% of nicotine users stop smoking once treated with varenicline (Chantix). Its success suggests that compounds modulating the cholinergic system may serve as promising drugs for smoking cessation treatment.
Smoking is the cause of 4.9 million deaths each year (Ebbert et al. 2010). Although the detrimental effects of smoking are commonly understood and 70% of smokers indicate that they want to quit, successful attempts among smokers remain below 5% (Nides 2008). Many factors contribute to the development and maintenance of nicotine addiction, and these processes have been investigated in both human populations and animal models to better understand underlying mechanisms. Cessation of chronic nicotine produces withdrawal symptoms in both animals (Grabus et al. 2005; Malin et al. 1992) and humans (Hughes 2007; Hendricks et al. 2006), and avoidance of withdrawal symptoms is one factor that contributes to the maintenance of smoking and relapse during quit attempts. Conversely, studies have also shown that the severity and duration of nicotine withdrawal symptoms strongly predict relapse (Piasecki et al. 1998, 2000). Therefore, recent endeavors in medication development are targeted at attenuation of nicotine withdrawal symptoms.
Currently, there are three “first-line” pharmacotherapies for nicotine addiction: nicotine replacement therapy, bupropion (a mixed norepinephrine/dopamine reuptake inhibitor), and varenicline (a nicotinic acetylcholine receptor [nAChR] partial agonist). The most promising of the current pharmacotherapies is varenicline (Chantix), which results in maintenance of smoking cessation in nearly 80% of treatment-seeking participants (Cahill et al. 2011). The success of varenicline, which targets α4β2 nAChRs, suggests that compounds modulating the cholinergic system and/or nicotinic receptors would serve as promising drugs for utilization as a smoking cessation therapy. Therefore, the central theme of this translational article focuses on modulation of the cholinergic system as a viable candidate for smoking cessation treatment, whether this be through modulation of the endogenous system via synthesis and release or through the direct activation of nAChRs.
NEUROBIOLOGY UNDERLYING THE ADDICTIVE NATURE OF NICOTINE
Neurochemisty of Nicotine
Nicotine, the major psychoactive component in tobacco smoke, is thought to mediate both tobacco reinforcement and dependence (Le Foll and Goldberg 2006). Once in the bloodstream, nicotine, a highly lipophilic compound, rapidly crosses the blood–brain barrier (Gahring and Rogers 2005) and can be sequestered in lipid-rich, slightly basic reservoirs, such as glia (Crooks 1999). This compartmentalization of nicotine can lead to its accumulation in the brain during chronic administration (Ghosheh et al. 2001), potentially producing continued effects following termination of nicotine exposure. Once in the brain, nicotine binds to nAChRs. These receptors are pentameric ion channels, which pass Na+, K+, and Ca2+ ions and thus have the ability to alter cellular activity. Entry of these ions can either directly impact cell excitability or trigger calcium-sensitive molecules, such as protein kinase C (PKC) (Soliakov and Wonnacott 2001), protein kinase A (PKA) (Dajas-Bailador et al. 2002), calmodulin-dependent protein kinase II (CAMKII) (Steiner et al. 2007), and extracellular signal-regulated kinases (ERKs) (Dajas-Bailador et al. 2002; Steiner et al. 2007). These calcium-sensitive kinases then have myriad downstream effects, including activation of transcription factors such as CREB (Chang and Berg 2001; Pandey et al. 2001; Hu et al. 2002; Brunzell et al. 2003; Walters et al. 2005) (for a review of signaling effects of nicotine, see Shen and Yakel 2009).
Nicotinic receptors come in two moieties, homomeric receptors (e.g., α7) or heteromeric receptors (e.g., α4β2) (for more information on specific subtypes, see Fowler et al. 2008). However, in this work, we will be focusing on the α4β2 heteromeric receptor in terms of its translational importance. In contrast to other subtypes, the α4β2 nAChR subtype has been shown to readily up-regulate following chronic exposure to nicotine, as evidenced by findings in cell culture (Xiao and Kellar 2004), rodents (Schwartz and Kellar 1983; Marks et al. 1985), monkeys (Picciotto et al. 2008), and humans (Mukhin et al. 2008). The up-regulation of receptors in the face of increased agonist is a characteristic unique to nicotine, and its full importance is not understood. However, PET imaging in human smokers following different periods of abstinence suggest that this up-regulation may directly contribute to smoking relapse. Cosgrove and colleagues showed that β2-containing nAChRs remain significantly up-regulated after 1 mo of abstinence and their density was positively correlated to craving (Cosgrove et al. 2009). Although correlational, this study suggests that the phenomenon of receptor up-regulation could directly contribute to failed smoking cessation.
Cholinergic System: Synthesis, Release, and Activation of nAChRs
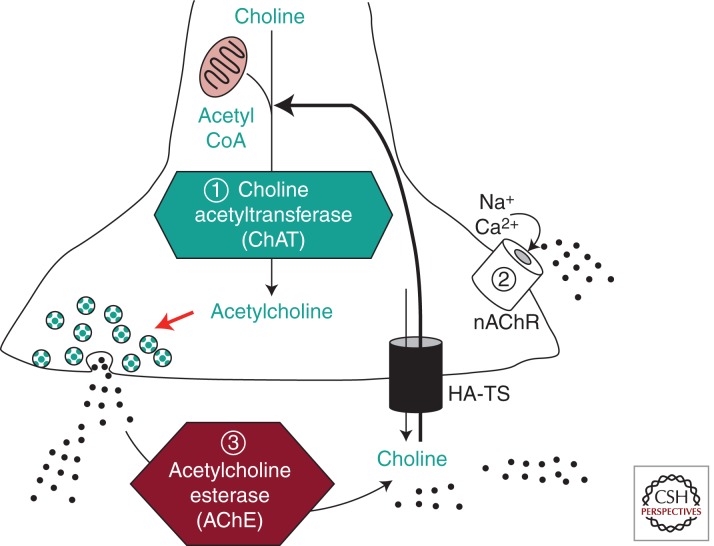
Nicotinic receptors are endogenously activated through the binding of acetylcholine (ACh) (Fig. 1). The rate-limiting step in the synthesis of acetylcholine (ACh) is the availability of choline in the cell (Jope 1979). Therefore, cholinergic cells possess a high-affinity choline transporter (HA-TS) on their terminals, in addition to the low-affinity choline transporter found on all neuronal cell types (Simon and Kuhar 1975; Okuda et al. 2000). ACh is actively synthesized via choline acetyltransferase (ChAT), which is located in the presynaptic nerve terminals near synaptic vesicles (Jope 1979). Because this enzyme is exclusive to the synthesis of ACh, it is a reliable marker of cholinergic neurons (Eckenstein and Sofroniew 1983). Cholinergic neurons can be subdivided into two major pools: (1) projection neurons arising from cholinergic nuclei and (2) subpopulations of cholinergic interneurons (Hoover et al. 1978). The major cholinergic projection neurons in the brain arise from two main sets of nuclei: the basal forebrain cholinergic complex, which includes the nucleus basalis, diagonal band of Broca, and medial septal nuclei and the pontomesencephalotegmental cholinergic complex, which includes the pedunculopontine nucleus and dorsolateral tegmental nuclei (Hoover et al. 1978; Eckenstein and Sofroniew 1983). Projections arising from these cholinergic nuclei innervate diverse brain areas, and thus impinge on numerous neural networks controlling such states as cognition, reward, and affect (Johnston et al. 1979; Muir et al. 1993). The second major pool of acetylcholine in the central nervous system (CNS) arises from cholinergic interneurons (Hoover et al. 1978). These GABAergic cells, which have been most thoroughly investigated in the cerebellum (Kalinichenko and Okhotin 2005), hippocampus (Lawrence 2008; Drever et al. 2011), and striatum (Oldenburg and Ding 2011), corelease ACh during high frequency stimulation, leading to strong modulation of local circuitry within the specific brain regions (Witten et al. 2010). Following release of ACh from either cholinergic projection neurons or cholinergic interneurons, ACh is inactivated through rapid degradation in the synapse by the enzyme acetylcholinesterase (AChE), rather than reuptake as is the case with many neurotransmitters (Zimmerman and Soreq 2006).
Figure 1.
Diagram of endogenous cholinergic transmission in the brain. Choline acetyltransferase (ChAT, 1) enzymatically produces acetylcholine from the precursors choline and acetyl CoA. Following synthesis, acetylcholine is packaged in presynaptic vesicles and released, where it can act on nicotinic acetylcholine receptors (nAChR, 2). Termination of acetylcholine activity is accomplished via enzymatic breakdown by acetylcholine esterase (AChE, 3), yielding choline and acetate. Choline is then actively transported back into the cell by the high-affinity choline transporter (HA-TS) and resynthesized into acetylcholine. Viable smoking cessation drug targets in the cholinergic system include synthesis (1), receptor activation (2), and degradation (3).
Although cholinergic projection neurons and interneurons are widely distributed throughout the CNS, nAChRs are predominantly found on presynaptic terminals. Thus, the main effect of nicotine is to modulate the release of numerous other neurotransmitters, including serotonin, norepinephrine, dopamine, acetylcholine, glutamate, and GABA (for a review, see Wonnacott et al. 2006). This presynaptic modulatory role of nicotinic receptors in the CNS may in fact underlie many of the problems in developing a successful smoking cessation aid. For example, in order for a pharmacotherapy to be successful, it needs to address not only central nicotinic signaling, but also nicotine’s potential effects on diverse other neurotransmitter systems. Further complicating this issue is that knowledge of how the cholinergic system is altered in a smoker remains largely unknown. Therefore, examination of human and animal studies investigating alterations to or polymorphisms within the cholinergic system may lead to more effective novel therapeutics for nicotine dependence.
TRANSLATIONAL STUDIES TARGETING MANIPULATIONS OF THE CHOLINERGIC SYSTEM
Acetylcholine (ACh) Synthesis Pathway—Rate-Limiting Steps and Genetic Influences
ChAT Studies in Smokers
Genetic studies in smokers have found significant association of single-nucleotide polymorphisms (SNPs) in the ChAT gene with smoking cessation phenotypes. An initial pharmacogenetic study found that a single ChAT SNP (rs1917810) was associated with higher abstinence rates in smokers with the minor allele (Heitjan et al. 2008). Follow-up studies in both treatment-seeking smokers (Ray et al. 2010) as well as nontreatment seekers (Wei et al. 2010) also showed significant association of ChAT SNPs or haplotypes with multiple measures of smoking and nicotine dependence. In the treatment seekers, a systems-based genetic association analysis was performed assessing smoking relapse following 8 wk of transdermal nicotine therapy. This approach highlighted a cluster of ChAT SNPs that were significantly associated with relapse (Ray et al. 2010). A replication and extension of this finding in non-treatment seekers examined SNPs in the ChAT gene for association with a number of nicotine dependence parameters, including smoking quantity and heaviness of smoking. This study, which used a haplotype-based association analysis, identified several ChAT haplotypes that were significantly associated with all parameters of nicotine dependence (Wei et al. 2010). In total, these human studies support additional investigation of ChAT manipulations for potential smoking cessation therapeutics.
ChAT Studies in Rodents
Because of the link between human SNPs in the ChAT gene and smoking behavior, it could be hypothesized that endogenous cholinergic tone afforded by ChAT activity may influence nicotine withdrawal behaviors. Indeed, animal studies probing the mechanistic effects of chronic nicotine during adolescence or adulthood have shown long-term alterations of ChAT activity (Abreu-Villaca et al. 2003; Ribeiro-Carvalho et al. 2009). Specifically, chronic exposure to nicotine during adolescence was shown to increase ChAT activity in adulthood in the cortex and hippocampus of male rodents (Abreu-Villaca et al. 2003; Ribeiro-Carvalho et al. 2009). This effect appears to be sex specific, because chronic nicotine treatment in adolescent female rodents results in a decreased ChAT activity profile during adulthood when compared to untreated female littermates (Ribeiro-Carvalho et al. 2008). However, it remains unknown whether these alterations are driven hormonally or through inherent sex differences in the cholinergic system.
In addition to adolescent studies, it has also been shown that chronic nicotine treatment during adulthood impacts ChAT activity as well. Adult exposure in male rodents resulted in decreased ChAT activity in the midbrain (Ciani et al. 2005), striatum, and cortex (Slotkin et al. 2008) following chronic nicotine treatment. However, following 72 h of nicotine withdrawal, ChAT activity was elevated in males, but not females (Slotkin et al. 2008), suggesting a homeostatic response in males but not females to the nicotine withdrawal state. This finding, in addition to the sex-specific effects observed following adolescent exposure (Ribeiro-Carvalho et al. 2009), may contribute to the differential nicotine reward and withdrawal profiles reported in women (for a review, see Perkins et al. 1999). The combined observations of rodent ChAT studies and human ChAT SNP studies suggest that modulation of endogenous ACh may be a viable candidate for future smoking cessation medication development.
Potential Therapeutics
Increased ACh Synthesis via Dietary Supplementation
Long-lasting alterations in the cholinergic system may indicate a need for increased modulation of the endogenous cholinergic system in treatment of nicotine dependence and withdrawal. Manipulations of acetylcholine synthesis via dietary choline supplementation have been shown to increase nAChR-binding sites in the hippocampus, frontal cortex, and striatum to levels similar to that seen following chronic nicotine administration (Coutcher et al. 1992). Furthermore, dietary supplementation with choline or other nutrients, like acetyl-l-carnitine and huperzine A, which have also been shown to increase acetylcholine levels in the brain, have been shown to rescue cognitive impairments in a number of animal models (De Bruin et al. 2003; Teather and Wurtman 2005, 2006; Wang et al. 2007; Holguin et al. 2008a,b). Although a clinical report in healthy young subjects did not report any significant effects on cognitive performance following dietary choline supplementation (Deuster et al. 2002), nutrient supplementation targeting increased synthesis of acetylcholine in persons with traumatic brain injury reported significant improvements in general cognitive functioning (Amen et al. 2011). These data suggest the benefit of increased ACh is evident only under conditions in which deficits are present. A clinical hallmark of nicotine withdrawal is cognitive impairment; therefore, these animal and human studies suggest that modulation of central acetylcholine levels via dietary supplementation may be a valid adjunctive treatment during smoking cessation.
Increased ACh Levels via Acetylcholinesterase Inhibitors
Because the actions of ACh in the synapse are terminated by degradation of the neurotransmitter by the enzyme acetylcholinesterase (AChE), an alternative approach to increase cholinergic tone in the synapse is through administration of AChE inhibitors. Inhibition of AChE is the primary mode of action of rivastigmine, donepezil, and galantamine, all of which are commonly prescribed medications for cognitive impairment and first-line medications for Alzheimer’s disease (Mehta et al. 2012). In nicotine-dependent animals, studies utilizing these drugs during withdrawal show that increasing endogenous ACh tone via inhibition of AChE can rescue some aspects of cognitive withdrawal deficits (Wilkinson and Gould 2011). Furthermore, although galantamine has not been successful at reducing smoking behavior in schizophrenic patients (Kelly et al. 2008), treatment with galantamine in alcohol-dependent smokers had promising results (Diehl et al. 2006).
nAChR Signaling—Polymorphisms in Subunits and Subsequent Downstream Effects
nAChR Polymorphism Studies in Smokers
Polymorphic alterations in the subunits comprising nAChRs can also impact smoking behaviors. Whether using a candidate gene approach or a genome-wide association studies (GWAS) approach, a number of studies have implicated SNPs occurring in nicotinic subunit genes in the etiology of smoking. The most widely evaluated example of this is the CHRNA5-CHRNA3-CHRNB4 gene cluster, which has been examined for associations with nicotine dependence phenotypes, withdrawal symptoms, and smoking cessation. A number of recent GWAS and pathway-based studies have identified SNPs in this gene cluster associated with heaviness of smoking and/or nicotine dependence (Berrettini et al. 2008; Bierut et al. 2007; Caporaso et al. 2009; Saccone et al. 2007; Thorgeirsson and Stefansson 2008; Thorgeirsson et al. 2010). Other aspects of nicotine dependence, such as nicotine tolerance, craving, withdrawal severity, and inability to stop smoking, have also been associated with CHRNA5-CHRNA3-CHRNB4 SNPs (Baker et al. 2009). However, although this highly reproducible finding implicates this gene cluster in various aspects of nicotine dependence, whether it predicts cessation rates is unclear. For example, in both retrospective and prospective studies no evidence was found for associations of SNPs in the CHRNA5-CHRNA3-CHRNB4 gene cluster with smoking cessation (Conti et al. 2008; Breitling et al. 2009; Ray et al. 2010). Yet, two SNPs in the CHRNA5 and CHRNB4 genes were identified as predictors of abstinence at 52-wk followup (Sarginson et al. 2011), and in pharmacogenetic studies, SNPs in this gene cluster appear to predict success rates with either nicotine or varenicline treatment (Munafo et al. 2011; King et al. 2012).
Other nicotinic subunits have also been implicated in nicotine dependence. For example, SNPs in CHRNA6 and CHRNB3, the genes encoding the α6 and β3 subunits, have been associated with nicotine dependence, subjective response to nicotine, and self-reported number of unsuccessful quit attempts (Bierut et al. 2007; Greenbaum et al. 2006; Saccone et al. 2007; Zeiger et al. 2008; Hoft et al. 2009). Additional studies have implicated the gene encoding for the α4 subunit, CHRNA4, in various smoking phenotypes (Breitling et al. 2009; Wessel et al. 2010; Han et al. 2011; Xie et al. 2011). Furthermore, polymorphisms in the CHRNA4 gene have been significantly associated with abstinence rates while on nicotine replacement therapy (Hutchison et al. 2007) or varenicline (King et al. 2012), suggesting a potential role for CHRNA4 as a target for therapeutic intervention.
nAChR Polymorphism Studies in Rodents
Studies from nicotinic receptor knockout mice have helped to elucidate the relative contributions of specific subunits to discrete behaviors pertinent to nicotine dependence and withdrawal (for a review, see Fowler et al. 2008). For example, β2 knockout mice do not show nicotine self-administration (Picciotto et al. 1998), nor do they show many of the classical behavioral responses to nicotine (Shoaib et al. 2002; Besson et al. 2006; Walters et al. 2006). However, the dramatic alterations inherent to complete loss of a nAChR subunit are not likely to reflect the general smoking population. Therefore, in terms of translational relevance, studies of rodent polymorphisms in nAChR subunits may be more representative of the repercussions of nAChR SNPs in the clinical population.
As an example of this, there is a missense polymorphism in the mouse Chrna4, which results in altered receptor function, including regulation of receptor stoichiometry (Dobelis et al. 2002; Kim et al. 2003). Studies using multiple mouse strains with differing genotypes at this polymorphism show that this SNP influences both nicotine preference and consumption in mice (Butt et al. 2005). To confirm that this SNP is sufficient for the behavioral alterations, studies using a knockin mouse with this same polymorphism showed that the threonine to alanine substitution results in reduced nicotine consumption, reduced nicotine reward, as well as altered α4β2* receptor function (Wilking et al. 2010). Although the equivalent of this SNP has not been identified in humans, these studies highlight the importance of examining natural occurring variation, in which a single-nucleotide alteration results in significant behavioral effects, in lieu of knockout mice or overexpression systems that may not be representative of human genetic variation. Furthermore, given the altered receptor function or altered stoichiometry arising from these murine SNPs, a similar situation may underlie the α4 SNPs and their associated phenotypes in human studies. However, further studies are necessary to directly evaluate this possibility.
To date, there are no mouse models that recapitulate variants of the human SNPs for the CHRNA5-CHRNA3-CHRNB4 gene cluster, or for the CHRNA6, CHRNA4, and CHRNB3 receptors. To approach this knockin mice could be generated that specifically harbor the human SNPs, or the mouse equivalent of these SNPs. The generation of such mice would allow for the examination of molecular mechanisms that mediate the associated behavioral consequences and thus contribute to a better understanding of their impact in nicotine dependence.
Potential Therapeutics
Coordinated Pharmacogenetic Cessation Treatment
Pharmacogenetic approaches to smoking cessation attempt to individualize treatment through the tailoring of a person’s therapy with their genetic information. Currently, the most successful pharmacotherapy for smoking cessation is varenicline (Chantix), an α4β2 nicotinic partial agonist. However, its efficacy rates appear to be variable in the general population. This variability could in fact be owing to differential effects in persons with polymorphisms in the genes encoding for varenicline’s target nicotinic receptor subunits, α4 and β2. In fact, a recent clinical trial investigating the pharmacogenetics of smoking cessation aids showed that continuous abstinence rates while on varenicline treatment is highly associated with SNPs in these subunits (King et al. 2012). Although perhaps economically unfeasible at present, this avenue of treatment may be more realistic in the future, with increased cost efficiency of individualized genotyping owing to higher throughput and improved methodology in genetic sequencing technology (Wu and Fuhlbrigge 2008; Olgiati et al. 2012). Furthermore, pharmacogenetic information is currently included with over 60 FDA-approved drugs (Frueh et al. 2008), indicating a progressive shift in the applicability of this approach. Therefore, further translational investigations highlighting gene by drug interactions may prove highly beneficial in the future.
CONCLUDING REMARKS
The cost of designed drug discovery is $1.8 billion dollars per drug, with a multitude of failed drugs along the way (Paul et al. 2010). Thus, investing in new approaches to bridge animal and human studies to evaluate novel therapeutics could significantly improve success rates. Furthermore, using combinations of mouse and human studies, additional treatments could be developed from off-the-shelf, currently approved medication lists. For example, bupropion is an antidepressant originally developed for the treatment of mood disorders. Numerous studies have shown a high degree of comorbidity between mood disorders and nicotine dependence, which supported bupropion’s utility as a smoking cessation aid (Totterdell 2006). This logical extension proved rewarding, as it is currently the second most efficacious smoking cessation aid on the market after varenicline. There is a similar case for therapeutics used in other disease states. For example, nicotine is protective against Alzheimer’s disease and other forms of dementia (for a review, see Shimohama and Kihara 2001). However, the novel application of cognitive impairment therapeutics for the treatment of nicotine dependence is gaining traction with increased animal and human studies evaluating cognitive enhancing drugs for smoking cessation. Perhaps future studies examining the underlying benefits of or vulnerabilities to nicotine within other comorbid populations will prove valuable in developing new smoking cessation therapies. However, this type of coordinated understanding will only be attainable through increased translational studies and communication between the animal and human side of nicotine dependence research.
ACKNOWLEDGMENTS
This work was supported by the National Cancer Institute at the National Institutes of Health (P50-CA-143187) and by the National Institute on Drug Abuse at the National Institutes of Health (1-F32-DA026236).
Footnotes
Editors: R. Christopher Pierce and Paul J. Kenny
Additional Perspectives on Addiction available at www.perspectivesinmedicine.org
REFERENCES
- Abreu-Villaca Y, Seidler FJ, Qiao D, Tate CA, Cousins MM, Thillai I, Slotkin TA 2003. Short-term adolescent nicotine exposure has immediate and persistent effects on cholinergic systems: Critical periods, patterns of exposure, dose thresholds. Neuropsychopharmacology 28: 1935–1949 [DOI] [PubMed] [Google Scholar]
- Amen DG, Wu JC, Taylor D, Willeumier K 2011. Reversing brain damage in former NFL players: Implications for traumatic brain injury and substance abuse rehabilitation. J Psychoactive Drugs 43: 1–5 [DOI] [PubMed] [Google Scholar]
- Baker TB, Weiss RB, Bolt D, von Niederhausern A, Fiore MC, Dunn DM, Piper ME, Matsunami N, Smith SS, Coon H, et al. 2009. Human neuronal acetylcholine receptor A5-A3-B4 haplotypes are associated with multiple nicotine dependence phenotypes. Nicotine Tob Res 11: 785–796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrettini W, Yuan X, Tozzi F, Song K, Francks C, Chilcoat H, Waterworth D, Muglia P, Mooser V 2008. α-5/α-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol Psychiatry 13: 368–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besson M, David V, Suarez S, Cormier A, Cazala P, Changeux JP, Granon S 2006. Genetic dissociation of two behaviors associated with nicotine addiction: β-2 containing nicotinic receptors are involved in nicotine reinforcement but not in withdrawal syndrome. Psychopharmacology (Berl) 187: 189–199 [DOI] [PubMed] [Google Scholar]
- Bierut LJ, Madden PAF, Breslau N, Johnson EO, Hatsukami D, Pomerleau OF, Swan GE, Rutter J, Bertelsen S, Fox L, et al. 2007. Novel genes identified in a high-density genome wide association study for nicotine dependence. Hum Mol Genet 16: 24–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitling LP, Dahmen N, Mittelstrass K, Rujescu D, Gallinat J, Fehr C, Giegling I, Lamina C, Illig T, Muller H, et al. 2009. Association of nicotinic acetylcholine receptor subunit α4 polymorphisms with nicotine dependence in 5500 Germans. Pharmacogenomics J 9: 219–224 [DOI] [PubMed] [Google Scholar]
- Brunzell DH, Russell DS, Picciotto MR 2003. In vivo nicotine treatment regulates mesocorticolimbic CREB and ERK signaling in C57Bl/6J mice. J Neurochem 84: 1431–1441 [DOI] [PubMed] [Google Scholar]
- Butt CM, King NM, Hutton SR, Collins AC, Stitzel JA 2005. Modulation of nicotine but not ethanol preference by the mouse Chrna4 A529T polymorphism. Behav Neurosci 119: 26–37 [DOI] [PubMed] [Google Scholar]
- Cahill K, Stead LF, Lancaster T 2011. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev 16: CD006103. [DOI] [PubMed] [Google Scholar]
- Caporaso N, Gu F, Chatterjee N, Sheng-Chih J, Yu K, Yeager M, Chen C, Jacobs K, Wheeler W, Landi MT, et al. 2009. Genome-wide and candidate gene association study of cigarette smoking behaviors. PLoS ONE 4: e4653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang KT, Berg DK 2001. Voltage-gated channels block nicotinic regulation of CREB phosphorylation and gene expression in neurons. Neuron 32: 855–865 [DOI] [PubMed] [Google Scholar]
- Ciani E, Severi S, Bartesaghi R, Contestabile A 2005. Neurochemical correlates of nicotine neurotoxicity on rat habenulo-interpeduncular cholinergic neurons. Neurotoxicology 26: 467–474 [DOI] [PubMed] [Google Scholar]
- Conti DV, Lee W, Li D, Liu J, Van Den Berg D, Thomas PD, Bergen AW, Swan GE, Tyndale RF, Benowitz NL, et al. 2008. Nicotinic acetylcholine receptor β2 subunit gene implicated in a systems-based candidate gene study of smoking cessation. Hum Mol Genet 17: 2834–2848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosgrove KP, Batis J, Bois F, Maciejewski PK, Esterlis I, Kloczynski T, Stiklus S, Krishnan-Sarin S, O’Malley S, Perry E, et al. 2009. β2-Nicotinic acetylcholine receptor availability during acute and prolonged abstinence from tobacco smoking. Arch Gen Psychiatry 66: 666–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coutcher JB, Cawley G, Wecker L 1992. Dietary choline supplementation increases the density of nicotine binding sites in rat brain. J Pharmacol Exper Therapeut 262: 1128–1132 [PubMed] [Google Scholar]
- Crooks PA 1999. Chemical properties of nicotine and other tobacco-related compounds. In Analytical determination of nicotine and related compounds and their metabolites (ed. Gorrod JW III, Jacob P), pp. 69–147 Elsevier, Oxford [Google Scholar]
- Dajas-Bailador FA, Soliakov L, Wonnacott S 2002. Nicotine activates the extracellular signal-regulated kinase 1/2 via the α7 nicotinic acetylcholine receptor and protein kinase A, in SH-SY5Y cells and hippocampal neurones. J Neurochem 80: 520–530 [DOI] [PubMed] [Google Scholar]
- De Bruin NM, Kiliaan AJ, De Wilde MC, Broersen LM 2003. Combined uridine and choline administration improves cognitive deficits in spontaneously hypertensive rats. Neurobiol Learn Mem 80: 63–79 [DOI] [PubMed] [Google Scholar]
- Deuster PA, Singh A, Coll R, Hyde DE, Becker WJ 2002. Choline ingestion does not modify physical or cognitive performance. Mil Med 167: 1020–1025 [PubMed] [Google Scholar]
- Diehl A, Nakovics H, Croissant B, Smolka MN, Batra A, Mann K 2006. Galantamine reduces smoking in alcohol-dependent patients: A randomized, placebo-controlled trial. Int J Clin Pharmacol Ther 44: 614–622 [DOI] [PubMed] [Google Scholar]
- Dobelis P, Marks MJ, Whiteaker P, Balogh SA, Collins AC, Stitzel JA 2002. A polymorphism in the mouse neuronal α4 nicotinic receptor subunit results in an alteration in receptor function. Mol Pharmacol 62: 334–342 [DOI] [PubMed] [Google Scholar]
- Drever BD, Riedel G, Platt B 2011. The cholinergic system and hippocampal plasticity. Behav Brain Res 221: 505–514 [DOI] [PubMed] [Google Scholar]
- Ebbert JO, Hays JT, Hurt RD 2010. Combination pharmacotherapy for stopping smoking: What advantages does it offer? Drugs 70: 643–650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckenstein F, Sofroniew MV 1983. Identification of central cholinergic neurons containing both choline acetyltransferase and acetylcholinesterase and of central neurons containing only acetylcholinesterase. J Neurosci 3: 2286–2291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler CD, Arends MA, Kenny PJ 2008. Subtypes of nicotinic acetylcholine receptors in nicotine reward, dependence, and withdrawal: Evidence from genetically modified mice. Behav Pharmacol 19: 461–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frueh FW, Amur S, Mummaneni P, Epstein RS, Aubert RE, DeLuca TM, Verbrugge RR, Burckart GJ, Lesko LJ 2008. Pharmacogenomic biomarker information in drug labels approved by the United States food and drug administration: Prevalence of related drug use. Pharmacotherapy 28: 992–998 [DOI] [PubMed] [Google Scholar]
- Gahring LC, Rogers SW 2005. Neuronal nicotinic acetylcholine receptor expression and function on nonneuronal cells. AAPS J 7: E885–E894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosheh OA, Dwoskin LP, Miller DK, Crooks PA 2001. Accumulation of nicotine and its metabolites in rat brain after intermittent or continuous peripheral administration of [2′-14C]nicotine. Drug Metab Dispos 29: 645–651 [PubMed] [Google Scholar]
- Grabus SD, Martin BR, Batman AM, Tyndale RF, Sellers E, Damaj MI 2005. Nicotine physical dependence and tolerance in the mouse following chronic oral administration. Psychopharmacology (Berl) 178: 183–192 [DOI] [PubMed] [Google Scholar]
- Greenbaum L, Kanyas K, Karni O, Merbl Y, Olender T, Horowitz A, Yakir A, Lancet D, Ben-Asher E, Lerer B 2006. Why do young women smoke? I. Direct and interactive effects of environment, psychological characteristics and nicotinic cholinergic receptor genes. Mol Psychiatry 11: 312–322 [DOI] [PubMed] [Google Scholar]
- Han S, Yang BZ, Kranzler HR, Oslin D, Anton R, Gelernter J 2011. Association of CHRNA4 polymorphisms with smoking behavior in two populations. Am J Med Genet B Neuropsychiatr Genet 156B: 421–429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heitjan DF, Guo M, Ray R, Wileyto EP, Epstein LH, Lerman C 2008. Identification of pharmacogenetic markers in smoking cessation therapy. Am J Med Genet B Neuropsychiatr Genet 147B: 712–719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks PS, Ditre JW, Drobes DJ, Brandon TH 2006. The early time course of smoking withdrawal effects. Psychopharmacology (Berl) 187: 385–396 [DOI] [PubMed] [Google Scholar]
- Hoft NR, Corley RP, McQueen MB, Huizinga D, Menard S, Ehringer MA 2009. SNPs in CHRNA6 and CHRNB3 are associated with alcohol consumption in a nationally representative sample. Genes Brain Behav 8: 631–637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holguin S, Huang Y, Liu J, Wurtman R 2008a. Chronic administration of DHA and UMP improves the impaired memory of environmentally impoverished rats. Behav Brain Res 191: 11–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holguin S, Martinez J, Chow C, Wurtman R 2008b. Dietary uridine enhances the improvement in learning and memory produced by administering DHA to gerbils. FASEB J 22: 3938–3946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoover DB, Muth EA, Jacobowitz DM 1978. A mapping of the distribution of acetycholine, choline acetyltransferase and acetylcholinesterase in discrete areas of rat brain. Brain Res 153: 295–306 [DOI] [PubMed] [Google Scholar]
- Hu M, Liu QS, Chang KT, Berg DK 2002. Nicotinic regulation of CREB activation in hippocampal neurons by glutamatergic and nonglutamatergic pathways. Mol Cell Neurosci 21: 616–625 [DOI] [PubMed] [Google Scholar]
- Hughes JR 2007. Effects of abstinence from tobacco: Valid symptoms and time course. Nicotine Tob Res 9: 315–327 [DOI] [PubMed] [Google Scholar]
- Hutchison KE, Allen DL, Filbey FM, Jepson C, Lerman C, Benowitz NL, Stitzel J, Bryan A, McGeary J, Haughey HM 2007. CHRNA4 and tobacco dependence: From gene regulation to treatment outcome. Arch Gen Psychiatry 64: 1078–1086 [DOI] [PubMed] [Google Scholar]
- Johnston MV, McKinney M, Coyle JT 1979. Evidence for a cholinergic projection to neocortex from neurons in basal forebrain. Proc Natl Acad Sci 76: 5392–5396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jope RS 1979. High affinity choline transport and acetylCoA production in brain and their roles in the regulation of acetylcholine synthesis. Brain Res 180: 313–344 [DOI] [PubMed] [Google Scholar]
- Kalinichenko SG, Okhotin VE 2005. Unipolar brush cells—A new type of excitatory interneuron in the cerebellar cortex and cochlear nuclei of the brainstem. Neurosci Behav Physiol 35: 21–36 [DOI] [PubMed] [Google Scholar]
- Kelly DL, McMahon RP, Weiner E, Boggs DL, Dickinson D, Conley RR, Buchanan RW 2008. Lack of beneficial galantamine effect for smoking behavior: A double-blind randomized trial in people with schizophrenia. Schizophr Res 103: 161–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Flanagin BA, Qin C, Macdonald RL, Stitzel JA 2003. The mouse Chrna4 A529T polymorphism alters the ratio of high to low affinity α4β2 nAChRs. Neuropharmacology 45: 345–354 [DOI] [PubMed] [Google Scholar]
- King DP, Paciga S, Pickering E, Benowitz NL, Bierut LJ, Conti DV, Kaprio J, Lerman C, Park PW 2012. Smoking cessation pharmacogenetics: Analysis of varenicline and bupropion in placebo-controlled clinical trials. Neuropsychopharmacology 37: 641–650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence JJ 2008. Cholinergic control of GABA release: Emerging parallels between neocortex and hippocampus. Trends Neurosci 31: 317–327 [DOI] [PubMed] [Google Scholar]
- Le Foll B, Goldberg SR 2006. Nicotine as a typical drug of abuse in experimental animals and humans. Psychopharmacology (Berl) 184: 367–381 [DOI] [PubMed] [Google Scholar]
- Malin DH, Lake JR, Newlin-Maultsby P, Roberts LK, Lanier JG, Carter VA, Cunningham JS, Wilson OB 1992. Rodent model of nicotine abstinence syndrome. Pharmacol Biochem Behav 43: 779–784 [DOI] [PubMed] [Google Scholar]
- Marks M, Stitzel J, Collins A 1985. Time course study of the effects of chronic nicotine infusion on drug response and brain receptors. J Pharmacol Exp Ther 235: 619–628 [PubMed] [Google Scholar]
- Mehta M, Adem A, Sabbagh M 2012. New acetylcholinesterase inhibitors for Alzheimer’s disease. Int J Alzheimers Dis 2012: 728983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muir JL, Page KJ, Sirinathsinghji DJ, Robbins TW, Everitt BJ 1993. Excitotoxic lesions of basal forebrain cholinergic neurons: Effects on learning, memory and attention. Behav Brain Res 57: 123–131 [DOI] [PubMed] [Google Scholar]
- Mukhin AG, Kimes AS, Chefer SI, Matochik JA, Contoreggi CS, Horti AG, Vaupel DB, Pavlova O, Stein EA 2008. Greater nicotinic acetylcholine receptor density in smokers than in nonsmokers: A PET study with 2–18F-FA-85380. J Nucl Med 49: 1628–1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munafò MR, Johnstone EC, Walther D, Uhl GR, Murphy MF, Aveyard P 2011. CHRNA3 rs1051730 genotype and short-term smoking cessation. Nicotine Tob Res 13: 982–988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nides M 2008. Update on pharmacologic options for smoking cessation treatment. Am J Med 121(Suppl 1): S20–S31 [DOI] [PubMed] [Google Scholar]
- Okuda T, Haga T, Kanai Y, Endou H, Ishihara T, Katsura I 2000. Identification and characterization of the high-affinity choline transporter. Nat Neurosci 3: 120–125 [DOI] [PubMed] [Google Scholar]
- Oldenburg IA, Ding JB 2011. Cholinergic modulation of synaptic integration and dendritic excitability in the striatum. Curr Opin Neurobiol 21: 425–432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olgiati P, Bajo E, Bigelli M, De Ronchi D, Serretti A 2012. Should pharmacogenetics be incorporated in major depression treatment? Economic evaluation in high- and middle-income European countries. Prog Neuropsychopharmacol Biol Psychiatry 36: 147–154 [DOI] [PubMed] [Google Scholar]
- Pandey SC, Roy A, Xu T, Mittal N 2001. Effects of protracted nicotine exposure and withdrawal on the expression and phosphorylation of the CREB gene transcription factor in rat brain. J Neurochem 77: 943–952 [DOI] [PubMed] [Google Scholar]
- Paul SM, Mytelka DS, Dunwiddie CT, Persinger CC, Munos BH, Lindborg SR, Schacht AL 2010. How to improve R&D productivity: The pharmaceutical industry’s grand challenge. Nat Rev Drug Discov 9: 203–214 [DOI] [PubMed] [Google Scholar]
- Perkins KA, Donny E, Caggiula AR 1999. Sex differences in nicotine effects and self-administration: Review of human and animal evidence. Nicotine Tob Res 1: 301–315 [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Fiore MC, Baker TB 1998. Profiles in discouragement: Two studies of variability in the time course of smoking withdrawal symptoms. J Abnorm Psychol 107: 238–251 [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Niaura R, Shadel WG, Abrams D, Goldstein M, Fiore MC, Baker TB 2000. Smoking withdrawal dynamics in unaided quitters. J Abnorm Psychol 109: 74–86 [DOI] [PubMed] [Google Scholar]
- Picciotto MR, Zoli M, Rimondini R, Lena C, Marubio LM, Pich EM, Fuxe K, Changeux JP 1998. Acetylcholine receptors containing the β2 subunit are involved in the reinforcing properties of nicotine. Nature 391: 173–177 [DOI] [PubMed] [Google Scholar]
- Picciotto MR, Addy NA, Mineur YS, Brunzell DH 2008. It is not “either/or”: Activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog Neurobiol 84: 329–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray R, Mitra N, Baldwin D, Guo M, Patterson F, Heitjan DF, Jepson C, Wileyto EP, Wei J, Payne T, et al. 2010. Convergent evidence that choline acetyltransferase gene variation is associated with prospective smoking cessation and nicotine dependence. Neuropsychopharmacology 35: 1374–1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro-Carvalho A, Lima CS, Filgueiras CC, Manhaes AC, Abreu-Villaca Y 2008. Nicotine and ethanol interact during adolescence: Effects on the central cholinergic systems. Brain Res 1232: 48–60 [DOI] [PubMed] [Google Scholar]
- Ribeiro-Carvalho A, Lima CS, Medeiros AH, Siqueira NR, Filgueiras CC, Manhaes AC, Abreu-Villaca Y 2009. Combined exposure to nicotine and ethanol in adolescent mice: Effects on the central cholinergic systems during short and long term withdrawal. Neuroscience 162: 1174–1186 [DOI] [PubMed] [Google Scholar]
- Saccone SF, Hinrichs AL, Saccone NL, Chase GA, Konvicka K, Madden PA, Breslau N, Johnson EO, Hatsukami D, Pomerleau O, et al. 2007. Cholinergic nicotinic receptor genes implicated in a nicotine dependence association study targeting 348 candidate genes with 3713 SNPs. Hum Mol Genet 16: 36–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarginson JE, Killen JD, Lazzeroni LC, Fortmann SP, Ryan HS, Schatzberg AF, Murphy GM Jr 2011. Markers in the 15q24 nicotinic receptor subunit gene cluster (CHRNA5-A3-B4) predict severity of nicotine addiction and response to smoking cessation therapy. Am J Med Genet B Neuropsychiatr Genet 156B: 275–284 [DOI] [PubMed] [Google Scholar]
- Schwartz R, Kellar K 1983. Nicotinic cholinergic receptor binding sites in the brain: Regulation in vivo. Science 220: 214–216 [DOI] [PubMed] [Google Scholar]
- Shen JX, Yakel JL 2009. Nicotinic acetylcholine receptor-mediated calcium signaling in the nervous system. Acta Pharmacol Sin 30: 673–680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimohama S, Kihara T 2001. Nicotinic receptor-mediated protection against β-amyloid neurotoxicity. Biol Psychiatry 49: 233–239 [DOI] [PubMed] [Google Scholar]
- Shoaib M, Gommans J, Morley A, Stolerman IP, Grailhe R, Changeux JP 2002. The role of nicotinic receptor β-2 subunits in nicotine discrimination and conditioned taste aversion. Neuropharmacology 42: 530–539 [DOI] [PubMed] [Google Scholar]
- Simon JR, Kuhar MG 1975. Impulse-flow regulation of high affinity choline uptake in brain cholinergic nerve terminals. Nature 255: 162–163 [DOI] [PubMed] [Google Scholar]
- Slotkin TA, Bodwell BE, Ryde IT, Seidler FJ 2008. Adolescent nicotine treatment changes the response of acetylcholine systems to subsequent nicotine administration in adulthood. Brain Res Bull 76: 152–165 [DOI] [PubMed] [Google Scholar]
- Soliakov L, Wonnacott S 2001. Involvement of protein kinase C in the presynaptic nicotinic modulation of [(3)H]-dopamine release from rat striatal synaptosomes. Br J Pharmacol 132: 785–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiner RC, Heath CJ, Picciotto MR 2007. Nicotine-induced phosphorylation of ERK in mouse primary cortical neurons: Evidence for involvement of glutamatergic signaling and CaMKII. J Neurochem 103: 666–678 [DOI] [PubMed] [Google Scholar]
- Teather LA, Wurtman RJ 2005. Dietary CDP-choline supplementation prevents memory impairment caused by impoverished environmental conditions in rats. Learn Mem 12: 39–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teather LA, Wurtman RJ 2006. Chronic administration of UMP ameliorates the impairment of hippocampal-dependent memory in impoverished rats. J Nutr 136: 2834–2837 [DOI] [PubMed] [Google Scholar]
- Thorgeirsson TE, Stefansson K 2008. Genetics of smoking behavior and its consequences: The role of nicotinic acetylcholine receptors. Biol Psychiatry 64: 919–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorgeirsson TE, Gudbjartsson DF, Surakka I, Vink JM, Amin N, Geller F, Sulem P, Rafnar T, Esko T, Walter S, et al. 2010. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat Genet 42: 448–453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Totterdell S 2006. The anatomy of co-morbid neuropsychiatric disorders based on cortico-limbic synaptic interactions. Neurotox Res 10: 65–85 [DOI] [PubMed] [Google Scholar]
- Walters CL, Cleck JN, Kuo YC, Blendy JA 2005. Mu-opioid receptor and CREB activation are required for nicotine reward. Neuron 46: 933–943 [DOI] [PubMed] [Google Scholar]
- Walters CL, Brown S, Changeux JP, Martin B, Damaj MI 2006. The β2 but not α7 subunit of the nicotinic acetylcholine receptor is required for nicotine-conditioned place preference in mice. Psychopharmacology (Berl) 184: 339–344 [DOI] [PubMed] [Google Scholar]
- Wang L, Albrecht MA, Wurtman RJ 2007. Dietary supplementation with uridine-5′-monophosphate (UMP), a membrane phosphatide precursor, increases acetylcholine level and release in striatum of aged rat. Brain Res 1133: 42–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei J, Ma JZ, Payne TJ, Cui W, Ray R, Mitra N, Lerman C, Li MD 2010. Replication and extension of association of choline acetyltransferase with nicotine dependence in European and African American smokers. Hum Genet 127: 691–698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessel J, McDonald SM, Hinds DA, Stokowski RP, Javitz HS, Kennemer M, Krasnow R, Dirks W, Hardin J, Pitts SJ, et al. 2010. Resequencing of nicotinic acetylcholine receptor genes and association of common and rare variants with the Fagerstrom test for nicotine dependence. Neuropsychopharmacology 35: 2392–2402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilking JA, Hesterberg KG, Crouch EL, Homanics GE, Stitzel JA 2010. Chrna4 A529 knock-in mice exhibit altered nicotine sensitivity. Pharmacogenet Genomics 20: 121–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson DS, Gould TJ 2011. The effects of galantamine on nicotine withdrawal-induced deficits in contextual fear conditioning in C57BL/6 mice. Behav Brain Res 223: 53–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witten IB, Lin SC, Brodsky M, Prakash R, Diester I, Anikeeva P, Gradinaru V, Ramakrishnan C, Deisseroth K 2010. Cholinergic interneurons control local circuit activity and cocaine conditioning. Science 330: 1677–1681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonnacott S, Barik J, Dickinson J, Jones IW 2006. Nicotinic receptors modulate transmitter cross talk in the CNS: Nicotinic modulation of transmitters. J Mol Neurosci 30: 137–140 [DOI] [PubMed] [Google Scholar]
- Wu AC, Fuhlbrigge AL 2008. Economic evaluation of pharmacogenetic tests. Clin Pharmacol Ther 84: 272–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Y, Kellar KJ 2004. The comparative pharmacology and up-regulation of rat neuronal nicotinic receptor subtype binding sites stably expressed in transfected mammalian cells. J Pharmacol Exp Ther 310: 98–107 [DOI] [PubMed] [Google Scholar]
- Xie P, Kranzler HR, Krauthammer M, Cosgrove KP, Oslin D, Anton RF, Farrer LA, Picciotto MR, Krystal JH, Zhao H, et al. 2011. Rare nonsynonymous variants in α-4 nicotinic acetylcholine receptor gene protect against nicotine dependence. Biol Psychiatry 70: 528–536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeiger JS, Haberstick BC, Schlaepfer I, Collins AC, Corley RP, Crowley TJ, Hewitt JK, Hopfer CJ, Lessem J, McQueen MB, et al. 2008. The neuronal nicotinic receptor subunit genes (CHRNA6 and CHRNB3) are associated with subjective responses to tobacco. Hum Mol Genet 17: 724–734 [DOI] [PubMed] [Google Scholar]
- Zimmerman G, Soreq H 2006. Termination and beyond: Acetylcholinesterase as a modulator of synaptic transmission. Cell Tissue Res 326: 655–669 [DOI] [PubMed] [Google Scholar]