Abstract
Prior research in the general population has found that social support can buffer the adverse effects of stressors on health. However, both stressors and social support may be qualitatively different for those living in urban poverty. We examined the effects of social support and poverty-specific stressors on self-rated health. We used data from the Welfare Client Longitudinal Survey (WCLS), a 5-year longitudinal study of 718 public aid recipients. We measured received social support and “net social support,” defined as the difference between support received and that given to others. We used restricted cubic splines to model the stress-buffering effects of social support on self-rated health as a function of stressful life events and neighborhood disorder. Increased exposure to stressors was associated with poorer self-rated health. Evidence of stress buffering was confined to those with the heaviest exposure to stressors, and its effects decreased across increasing levels of social support. Analyses using net social support had generally more modest effects than those using received social support. Social support does not buffer the effects of stressors on health uniformly for individuals living in conditions of urban poverty. Researchers and policymakers should be cautious in overestimating the beneficial effects that social support may have on health for marginalized populations.
Keywords: Social support, Stressors, Self-rated health, Social environment, Urban poverty
Introduction
The positive effects of social support on health have been well documented in social epidemiological research.1–3 One pathway through which social support is thought to affect health is “stress buffering.” This occurs when supportive social networks help individuals cope with the negative effects of social stressors.4 Studies of stress buffering have largely examined general population samples.5,6
Both the nature of social stressors and network support may differ for those in poverty. It is clear that neighborhood environments and life contexts of the urban poor subject people to distinctly different social stressors than the general population and arguably, at greater levels of intensity.7,8 Poverty-specific stressors may include chronic exposure to crime, drug-saturated neighborhoods, unemployment, overcrowded residences, unstable work and interpersonal relationships, as well as residential segregation.9,10 Acute stressors may include episodes of violent victimization, neighborhood police sweeps, family economic crises, and accidental injuries.11–13 Poverty-specific stressors such as these have been consistently associated with poor health.8,14,15
Qualities of social networks may also differ for people in poverty.16 Social networks of the poor tend to be comparatively small, isolated, and comprised of other, equally poor, individuals.17,18 Some anthropological studies have romanticized the tight networks of poor individuals, where the exchange of small loans, shared housing, and help caring for children is believed to provide an “informal safety-net” that allows families to “make ends meet.”19,20 However, the general resource depletion of these communities may also mean that there are fewer resources to spread around.21 Unequal reciprocity—an imbalance between giving and receiving social support—may be more common in low-income communities, and could constitute a source of stress in and of itself.22–24 Health-related studies have not, however, directly measured reciprocity,25,26 despite suggestions that it could matter for health.27
For this study, we examined the relationships between poverty-specific stressors, social support, and self-rated health in a longitudinal cohort of urban poor. We hypothesized that the stress-buffering effects of social support may not apply to the types of stressors that characterize life in poverty. Specific objectives were: (1) to examine whether poverty-specific stressors were associated with self-rated health, and (2) to test whether social support moderates the effect of stressors on self-rated health.
Methods
Study Population
We drew on data from the Welfare Client Longitudinal Survey that followed a representative sample of 718 individuals from a large California county. Study participants were recruited as they applied for public aid in 2001 and annually re-interviewed over 5 years. The sample was stratified to capture both women and men in poverty by including women with children on Temporary Assistance to Needy Families and single adults on General Assistance. The majority of study participants (73.5 %) were female, with a mean age at entry into the cohort of 33.4 years. All reported low annual household incomes, with only 24.3 % earning greater than $25,000 in a county where the median income was over $75,000. Most participants were African American (42.3 %), with whites constituting the second largest racial/ethnic category (31.5 %).
The cohort was recruited from an ethnically diverse, largely urban, county in Northern California with over 1 million inhabitants. Participants were recruited at all county welfare offices using interval sampling from intake rosters. After obtaining written informed consent, professional survey interviewers administered hour-long survey instruments in English and Spanish annually over the five waves of data collection. All time-varying measures were repeated at each wave in an identical format. Through an intensive tracking approach, we were able to retain 81 % of the cohort at the final wave, including substantial numbers of “hard to reach” participants who had moved residence, become homeless, incarcerated, as well as those who had moved out of poverty and into stable employment.28 More information on the data can be found in prior published studies.29–36 The Welfare Client Longitudinal Survey (WCLS) study was approved by institutional review boards at the University of California San Francisco and the Public Health Institute.
Measures
We used self-reported health as the dependent variable. This is a widely used indicator of overall health that predicts mortality in diverse populations37,38 and is applicable to low-income populations.39,40 We dichotomized the original four-way Likert format item for these analyses as fair/poor (=1) and good/excellent (=0).
Key independent variables included two types of stressors—stressful life events and neighborhood disorder—developed to capture acute and chronic poverty-related stressors. We obtained a poverty-specific scale for stressful life events from a survey of welfare recipients conducted by the University of Michigan.41 Participants were indexed on whether or not they had experienced each in the prior year: having a relative/close friend in jail, having people living with them who one wished were not there, having someone close who died/was killed, living with/being close to someone with alcohol or drug problems, being hassled by bill collectors/collection agencies, experiencing a life-threatening accident, experiencing a fire/flood/natural disaster, and having a family member seriously ill/injured.
The second stressor was measured using an index of neighborhood disorder developed through an extensive item development and pretesting effort.42,43 Participants were asked whether the following events occurred “never,” “sometimes,” or “frequently” in their neighborhoods during the prior year: drug arrests/busts, muggings, drug selling, drive-by shootings, people sleeping in public places, home robberies, arrests for public drunkenness, and teenagers hanging out during school hours. Cronbach’s alpha for all items was 0.87.
After combining the response categories “sometimes” and “frequently” on the neighborhood disorder measure, both indexes ranged from 0 to 8. We confirmed normal distributions and linear relationships with the dependent variable for each, and trichotomized the distributions into “heavy,” “moderate,” and “low” levels of exposure to stressors.
Measures of social support were based on prior literature and careful pretesting.44 While most investigations of social support examine perceptions of resource availability,45–47 we measured instances of actual behaviors. Assessing actual transfer is well suited to the dense, frequently accessed networks of the urban poor.48 Parallel items were asked about providing and receiving support from family/close friends during the prior year: help when upset/depressed/needed to talk, when sick, help with food/clothing, leads for jobs, running errands, watching children, providing transportation, and financial support. Response categories were “frequently,” “sometimes,” or “never.”
After weighting items to account for the differing number of questions addressing instrumental, informational, and emotional support, we summed all endorsements of obtaining help into a continuous measure of “received social support,” with values ranging from 0 to 16. Cronbach’s alpha was 0.81. We developed a continuous measure of “net social support” by subtracting the value of support given from the value of support received on an item-by-item basis, then summing the weighted scores. Values could range from −16 to 16. Negative values indicate a net social support deficit (i.e., giving more than receiving), values closer to zero suggest more balanced reciprocity, and positive value indicate a net surplus (i.e., receiving help from others more than giving).
Covariates measured at baseline included education (high school completion), race/ethnicity (white, black, Latino, other), and age. A continuous measure of household income was included as a time-varying covariate.
Data Analysis
We analyzed data using generalized estimating equations (GEE) with an exchangeable working correlation structure and robust standard errors. Logistic models predicted self-rated health as a function of covariates, and time-varying measures of stressors and social support. Because self-rated health at any given point in time may be highly correlated with self-rated health from the prior year, we also entered this variable’s value lagged by 1 year as a covariate.28 Sampling weights were used throughout to account for sample design and non-response at each wave of follow up.49
We began by specifying GEE models to examine the effects of stressful life events and neighborhood disorder on self-rated health, after entering covariates. Next, we examined the stress-buffering hypothesis using GEE models to examine whether social support modified the effects of stressors on self-rated health, as represented by interaction terms. Preliminary analysis suggested that social support had non-linear relationships with self-rated health. To address this, we modeled social support using restricted cubic splines that allow for non-linear but smooth effects.50
Results from non-linear interaction models such as these can be difficult to interpret, so we present the regression results in two ways. First, we plotted adjusted curves for received and net social support across low, moderate, and high levels of exposure to stressful life events and neighborhood disorder. Second, we calculated adjusted odds ratios that capture the effects of a one-unit increase in received and net support, again stratified by level of exposure to stressors. Because interpretation of these effects is dependent on the reference level of social support under the non-linear spline models, we present adjusted odds ratios calculated at three different thresholds of social support: the 10th, 50th, and 90th percentiles. Confidence intervals were obtained using the delta method.51
Results
Reports of fair/poor health as well as exposure to stressors were common in this sample. At baseline, over one third (38 %) of study participants rated their overall health as fair or poor. There was a high rate of exposure to poverty-related stressors, with 68 % of participants reported two or more stressful life events, and 61 % reported two or more episodes of neighborhood disorder.
Social interactions were common among participants, with 98 % reporting receiving support, and 99 % reporting giving support. In terms of net support, 12 % were in reciprocal exchanges at baseline. The majority (47 %) received more support than they gave. Slightly fewer (41 %) gave more support than they received.
To evaluate the impact of stressors on health, we predicted the odds of reporting fair/poor health as a function of stressful life events and neighborhood disorder after adjusting for age, gender, race, education, income, and fair/poor health the previous year (Table 1). Exposure to increased levels of stressful life events (p value for trend = 0.01) and neighborhood disorder (p value for trend = 0.004) were associated with greater odds of fair/poor self-rated health. Heavy exposure to neighborhood disorder increased the likelihood of reporting fair/poor health by 44 %. Heavy exposure to stressful life events had an even greater impact, increasing the odds of poor health by 71 %. Being male and having a higher income decreased the odds of fair/poor health.
Table 1.
Adjusted odds of fair/poor self-rated health
| OR (CI 95) | |
|---|---|
| Age | 1.04 (1.03, 1.05) |
| Sex (reference: female) | 0.67 (0.51, 0.88) |
| Race | |
| African American | 1.13 (0.88, 1.45) |
| Latino | 1.13 (0.83, 1.55) |
| Other | 1.08 (0.75, 1.56) |
| Income | 0.92 (0.89, 0.96) |
| Fair/poor health prior year | 4.05 (3.22, 5.09) |
| Neighborhood stressors | |
| Medium | 1.21 (0.97, 1.52) |
| High | 1.44 (1.12, 1.84) |
| Stressful life events | |
| Medium | 1.26 (1.04, 1.54) |
| High | 1.71 (1.29, 2.27) |
Results are weighted to account for sampling and non-response
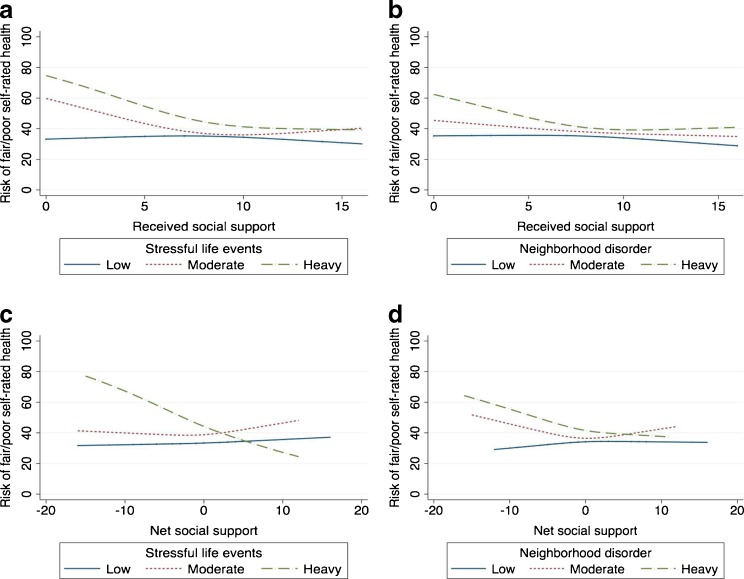
To test the stress-buffering hypothesis, we examined whether received and net social support moderate the relationships between stressors and health. We plotted the adjusted mean proportions of the sample reporting fair/poor health across levels of social support, comparing curves for study participants with low, moderate, and heavy exposure to stressors (Figure 1). The results show that the stress-buffering effect is largely confined to those with heaviest exposure to stressors. The effects of received and net social support are both modified by stressful life events. (p for interaction = 0.02 in both models; panels a and c) This is evident in the model that includes stressful life events and received social support (panel a) where heavy exposure to stressful life events increases the likelihood of fair/poor health, but primarily for those with low levels of received social support. In the model including stressful life events and net social support (panel c), the effects are only evident among those with the greatest exposure to stressful life events. Patterns appear qualitatively similar in plots for neighborhood disorder (panels b and d), but the interaction terms are not statistically significant (p for interaction = 0.40 in both models).
Figure 1.
Regression curves estimating percent risk of fair/poor self-rated health by stressor and social support. a Stressful life events and received social support, b neighborhood disorder and received social support, c stressful life events and net social support, d neighborhood disorder and net social support. Adjusted for self-rated health at t−1, age, sex, race, education, and income. Data are weighted to account for sampling and non-response. Negative values of net social support represent giving more support than receiving, zero represents reciprocity, positive values represent receiving more than giving.
Table 2 provides a different vantage on the results. As the stress-buffering effects are not constant across all levels of social support, we present odds ratios that represent the extent of change in fair/poor health that corresponds to a one-unit increase in social support at three different thresholds of the social support distribution. The results indicate that social support, whether net or received, only appears to make a significant difference in health for those at the 10th and 50th percentiles of their distributions and among those with greater exposure to stressors. The effect sizes corresponding to received social support in every case are greater than those corresponding to net social support.
Table 2.
Adjusted odds of fair/poor self-rated health per one-unit increase in social support
| Low | Moderate | Heavy | ||
|---|---|---|---|---|
| OR (CI 95) | OR (CI 95) | OR (CI 95) | ||
| Stressful life events | ||||
| Received social support | 10th percentile | 1.02 (0.94, 1.1) | 0.87 (0.79, 0.96)* | 0.83 (0.73, 0.95)* |
| 50th percentile | 0.99 (0.95, 1.03) | 0.95 (0.91, 0.99)* | 0.91 (0.85, 0.97)* | |
| 90th percentile | 0.97 (0.89, 1.05) | 1.04 (0.94, 1.15) | 0.99 (0.85, 1.15) | |
| Net social support | 10th percentile | 1.00 (0.93, 1.08) | 0.99 (0.92, 1.07) | 0.91 (0.83, 0.99)* |
| 50th percentile | 1.01 (0.97, 1.04) | 1.01 (0.97, 1.06) | 0.92 (0.86, 0.98)* | |
| 90th percentile | 1.01 (0.95, 1.08) | 1.04 (0.95, 1.13) | 0.93 (0.80, 1.08) | |
| Neighborhood disorder | ||||
| Received social support | 10th percentile | 1.00 (0.91, 1.10) | 0.96 (0.88, 1.05) | 0.88 (0.80, 0.97)* |
| 50th percentile | 0.98 (0.94, 1.02) | 0.97 (0.93, 1.01) | 0.95 (0.90, 0.99)* | |
| 90th percentile | 0.96 (0.87, 1.06) | 0.99 (0.90, 1.08) | 1.02 (0.91, 1.13) | |
| Net social support | 10th percentile | 1.02 (0.93, 1.12) | 0.95 (0.89, 1.03) | 0.94 (0.88, 1.01) |
| 50th percentile | 1.01 (0.96, 1.05) | 1.00 (0.96, 1.03) | 0.97 (0.93, 1.01) | |
| 90th percentile | 1.00 (0.91, 1.09) | 1.03 (0.95, 1.12) | 0.99 (0.90, 1.08) | |
Odds ratios are adjusted for self-rated health at t−1, age, sex, race, education, and income. Results are weighted to account for sampling and non-response
*p < 0.05
Discussion
The results of this study illustrate some of the complexities in how the social environment of urban poverty influences health. We hypothesized that the stress-buffering effects of social support may not necessarily apply to the types of stressors and social networks that characterize life in poverty. We found that the effects of social support on health were largely confined to those facing the heaviest burden of exposure to stressors, including both stressful life events and neighborhood disorder. Because social networks of the poor tend to include others who are resource deprived, there may be limits to the extent that they buffer individuals from the harmful effects of stress on health.
At the most basic level, our analyses drive home the extent that poverty-specific stressors have adverse consequences for health. Stressful life events had larger effects on health than neighborhood disorder throughout our analyses suggesting possible differences between acute and chronic stressors. Our findings are consistent with the growing body of research on the stressors of low-income neighborhoods and their impact on individual-level health outcomes.8,14,15,45,46
Results from this study also support the view that stress buffering is relevant to life in poverty, but suggest the caveat that these benefits are not necessarily widespread. Measures of received social support moderated the effects of stressful life events on health. However, this relationship was not constant across all levels of social support, nor did it apply to all levels of exposure to stressors. The primary health benefit was seen in a narrow segment of the population that experienced the combination of heavy exposure to stressors and low levels of support. This may represent an attenuation effect, where higher degrees of support have progressively decreasing effects. Alternatively, increasing receipt of social support may create interpersonal tensions, thereby attenuating or counteracting the stress-buffering aspects.47 In their ethnographic study of poor women, for example, Dominguez and Watkins found that those who received help during times of need often felt that the support came with “strings attached,” in the form of an open-ended burden to return the help during better times.21
This interpretation was illustrated by our comparisons of net and received social support where the effect sizes for received social support were uniformly larger than those for net social support. This suggests that failure to take account of unequal reciprocity, runs the risk of overestimating the stress-buffering effects of social networks. When we considered a nontraditional measure of net social support that takes this into account, the moderating effects of stressors on health became less pronounced. Only for individuals experiencing the very highest levels of stressful life events did we find evidence consistent with the stress-buffering hypothesis.
Individuals experiencing the highest levels of stressful life events and neighborhood disorder are presumably the most marginalized with the fewest resources, potentially with the least access to social networks. They may have a perceived need of social support—something we did not measure—that outstrips actual receipt.
Reverse causation is a threat to the validity of these findings. Despite our attempts to address this with a longitudinal cohort and transition models, it remains a limitation. Stressors, especially those that are chronic, may influence self-rated health in a delayed manner. Due to the data collection interval of 1 year, such changes may not be reflected in the data. Another methodological limitation pertains to the generalizability of results. While this sample was representative of populations seeking aid in a large urban county, demographic and policy variations could limit applicability to populations elsewhere in the USA. To maximize generalizability, we selected a large study site that captured the demographic diversity of the US population.
The social environment of urban poverty presents complex interrelating challenges to population health. Our findings raise some key questions about how we understand and intervene upon different aspects of this environment to protect health. Researchers and policymakers should be cautious in overestimating the beneficial effects that interpersonal characteristics such as social support have on health for the urban poor. Assumptions drawn from the middle-class may not hold true among socially marginalized populations. Consideration of reciprocity in the social interactions of low-income individuals is appropriate because of high degrees of reliance on informal safety nets and extensive networks of exchange.48 Future work should apply social network methods to questions of health in the urban poor, examining how network size, density, and isolation might relate to the buffering of poverty-specific stressors, and potentially the utilization of social and medical services.
Acknowledgments
This study was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) P50 AA05595, R01 AA13136, R01 AA0149918, and R21AA015397. Dr. Moskowitz was supported by the Primary Care Research Fellowship at UCSF, funded by the Department of Health and Human Services, Health Resources and Services Administration D55HP05165. Dr. Schmidt’s effort was supported by the Philip R. Lee Institute for Health Policy Studies Fellowship Program and NIAAA grant R01AA017197.
References
- 1.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alemeda County residents. Am J Epidemiol. 1979;109(2):186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 2.House J, Landis K, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 3.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119(3):488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 4.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- 5.Rosengren A, Orth-Gomer K, Wedel H, Wilhelmsen L. Stressful life events, social support, and mortality in men born in 1933. BMJ. 1993;307(6912):1102–1105. doi: 10.1136/bmj.307.6912.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Falk A, Hanson BS, Isacsson SO, Ostergren PO. Job strain and mortality in elderly men: social network, support, and influence as buffers. Am J Public Health. 1992;82(8):1136–1139. doi: 10.2105/AJPH.82.8.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feldman PJ, Steptoe A. How neighborhoods and physical functioning are related: the roles of neighborhood socioeconomic status, perceived neighborhood strain, and individual health risk factors. Ann Behav Med. 2004;27(2):91–99. doi: 10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- 8.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42(3):258–276. doi: 10.2307/3090214. [DOI] [PubMed] [Google Scholar]
- 9.Wacquant L. Urban outcasts: a comparative sociology of advanced marginality. Cambridge: Polity; 2007. [Google Scholar]
- 10.Currie E. Reckoning: drugs, the cities, and the American future. New York: Hill and Wang; 1993. [Google Scholar]
- 11.Venkatesh SA. American project: the rise and fall of a Modern Ghetto. Cambridge: Harvard University Press; 2000. [Google Scholar]
- 12.Conley D. Being black, living in the red: race, wealth, and social policy in America. London: University of California Press; 1999. [Google Scholar]
- 13.Dohan D. The price of poverty: money, work and culture in the Mexican-American Barrio. Berkeley: University of California Press; 2003. [Google Scholar]
- 14.Sundquist K, Theobald H, Yang M, et al. Neighborhood violent crime and unemployment increase the risk of coronary heart disease: a multilevel study in an urban setting. Soc Sci Med. 2006;62(8):2061–2071. doi: 10.1016/j.socscimed.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 15.Chaix B, Lindstrom M, Rosvall M, Merlo J. Neighbourhood social interactions and risk of acute myocardial infarction. J Epidemiol Community Health. 2008;62(1):62–68. doi: 10.1136/jech.2006.056960. [DOI] [PubMed] [Google Scholar]
- 16.Berkman L, Kawachi I. Social epidemiology. London: Oxford University Press; 2000. [Google Scholar]
- 17.Tigges LM, Browne I, Green GP. Social isolation of the urban poor: race, class, and neighborhood effects on social resources. Sociol Q. 1998;39(1):53–77. doi: 10.1111/j.1533-8525.1998.tb02349.x. [DOI] [Google Scholar]
- 18.Cattell V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Soc Sci Med. 2001;52(10):1501–1516. doi: 10.1016/S0277-9536(00)00259-8. [DOI] [PubMed] [Google Scholar]
- 19.Edin K, Lein L. Making ends meet: how single mothers survive welfare and low-wage work. New York: Russell Sage; 1997. [Google Scholar]
- 20.Stack C. All our kin: strategies for survival in a black community. New York: Harper and Row; 1974. [Google Scholar]
- 21.Domínguez S, Watkins C. Creating networks for survival and mobility: social capital among African-American and Latin-American low-income mothers. Soc Probl. 2003;50(1):111–135. doi: 10.1525/sp.2003.50.1.111. [DOI] [Google Scholar]
- 22.Newman K. Chutes and ladders: navigating the low-wage labor market. New York: Russell Sage; 2006. [Google Scholar]
- 23.Belle D. Poverty and women’s mental health. Am Psychol. 1990;45(3):385–398. doi: 10.1037/0003-066X.45.3.385. [DOI] [Google Scholar]
- 24.Knowlton AR, Yang C, Bohnert A, Wissow L, Chander G, Arnsten JA. Informal Care and Reciprocity of Support are Associated with HAART Adherence Among Men in Baltimore, MD, USA. AIDS Behav. 2011; 15(7): 1429–1436. [DOI] [PMC free article] [PubMed]
- 25.Antonucci TC, Fuhrer R, Jackson JS. Social support and reciprocity—a cross-ethnic and cross national perspective. J Soc Pers Relatsh. 1990;7:519–530. doi: 10.1177/0265407590074008. [DOI] [Google Scholar]
- 26.Ziersch AM, Baum FE, Macdougall C, Putland C. Neighbourhood life and social capital: the implications for health. Soc Sci Med. 2005;60(1):71–86. doi: 10.1016/j.socscimed.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 27.Abbott S, Freeth D. Social capital and health: starting to make sense of the role of generalized trust and reciprocity. J Health Psychol. 2008;13(7):874–883. doi: 10.1177/1359105308095060. [DOI] [PubMed] [Google Scholar]
- 28.Diggle PJ, Heagerty P, Liang K-Y, Zeger SL. Analysis of longitudinal data. 2. Oxford: Oxford University Press; 2002. [Google Scholar]
- 29.Mulia N, Schmidt L, Bond J, Jacobs L, Korcha R. Stress, social support and problem drinking among women in poverty. Addiction. 2008;103(8):1283–1293. doi: 10.1111/j.1360-0443.2008.02234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lown EA, Schmidt L, Wiley J. Unraveling lives: interpersonal violence among women seeking welfare. Paper presented at: Research Society on Alcohol. Santa Barbara, CA; June 2005.
- 31.Schmidt LA, Weisner CM, Wiley JA. Substance abuse and the course of welfare dependency. Am J Public Health. 1998;88(11):1616–1622. doi: 10.2105/AJPH.88.11.1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schmidt LA, Wiley JA, Dohan D, et al. Changing patterns of addiction and public aid receipt: tracking the unintended consequences of welfare reform policy. J Health Polit Policy Law. 2006;31(5):945–980. doi: 10.1215/03616878-2006-013. [DOI] [PubMed] [Google Scholar]
- 33.Schmidt L, Dohan D, Wiley J, Zabkiewicz D. Addiction and welfare dependency: interpreting the connection. Soc Probl. 2002;49:221–241. doi: 10.1525/sp.2002.49.2.221. [DOI] [Google Scholar]
- 34.Schmidt L, Zabkiewicz D, Henderson S, Wiley J, Jacobs L. On the declining health status of welfare caseloads: emerging dilemmas in serving the poor. Soc Work Publ Health. 2011; 26(2): 181–211. [DOI] [PMC free article] [PubMed]
- 35.Schmidt L, Zabkiewicz D, Jacobs L, Wiley J. Substance abuse and employment among welfare mothers: from welfare to work and back again? Subst Use Misuse. 2007;42(7):1069–1087. doi: 10.1080/10826080701409644. [DOI] [PubMed] [Google Scholar]
- 36.Zabiewicz D, Schmidt LA. The mental health benefits of work: do they apply to welfare mothers with a drinking problem? J Behav Health Serv Res. 2009;36(1):96–110. doi: 10.1007/s11414-008-9148-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGee DL, Liao Y, Cao G, Cooper RS. Self-reported health status and mortality in a multiethnic US cohort. Am J Epidemiol. 1999;149(1):41–46. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- 38.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- 39.Stewart AL, Napoles-Springer A. Health-related quality-of-life assessments in diverse population groups in the United States. Med Care. 2000;38(9 Suppl):102–124. [PubMed] [Google Scholar]
- 40.Burstrom B, Fredlund P. Self rated health: is it as good a predictor of subsequent mortality among adults in lower as well as in higher social classes? J Epidemiol Community Health. 2001;55(11):836–840. doi: 10.1136/jech.55.11.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.University of Michigan Ford School of Public Policy. The women’s health study: wave 1 survey instrument. http://www.fordschool.umich.edu/research/poverty/wes/instrument/wave_1.php. Accessed 1 February 2010.
- 42.Ewart CK, Suchday S. Discovering how urban poverty and violence affect health: development and validation of a Neighborhood Stress Index. Health Psychol. 2002;21(3):254–262. doi: 10.1037/0278-6133.21.3.254. [DOI] [PubMed] [Google Scholar]
- 43.Perkins DD, Taylor RB. Ecological assessments of community disorder: their relationship to fear of crime and theoretical implications. Am J Community Psychol. 1996; 24(1): 63–107. [DOI] [PubMed]
- 44.Mulia N, Schmidt L. Conflicts and trade-offs due to alcohol and drugs: clients’ accounts of leaving welfare. Soc Serv Rev. 2003;77(4):499–522. doi: 10.1086/378326. [DOI] [Google Scholar]
- 45.Kawachi I, Subramanian SV, Kim D. Social capital and health. New York: Springer; 2008. [Google Scholar]
- 46.Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann Behav Med. 2001;23(3):177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- 47.Knowlton AR, Curry A, Hua W, Wissow L. Depression and social context: primary supporter relationship factors associated with depressive symptoms among a disadvantaged population with HIV/AIDS. J Community Psychol. 2009;37(4):526–541. doi: 10.1002/jcop.20311. [DOI] [Google Scholar]
- 48.Venkatesh SA. Off the books: the underground economy of the urban poor. Cambridge: Harvard University Press; 2006. [Google Scholar]
- 49.Odierna DH, Schmidt LA. The effects of failing to include hard-to-reach respondents in longitudinal surveys. Am J Public Health. 2009;99(8):1515–1521. doi: 10.2105/AJPH.2007.111138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551–561. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 51.Oehlert G. A note on the delta method. Am Stat. 1992;46(1):27–29. [Google Scholar]