Abstract
Background
Although research shows that healthcare professionals' support improves breastfeeding duration, many physicians do not believe they have adequate time to address breastfeeding concerns during office visits. This study evaluated the impact of a pediatric practice's postnatal lactation consultant intervention. To improve breastfeeding support, the study practice changed policy and began using a lactation consultant overseen by a physician, to conduct the initial postpartum office visit for all breastfeeding infants.
Methods
A retrospective chart review was performed on consecutive newborns before (n = 166) and after (n = 184) implementation of the program. Feeding method was assessed at each well child visit during the infant's first 9 months. χ2 and logistic growth curve analyses were used to test the association between implementation status and non-formula feeding (NFF).
Results
Mothers and infants in 2007 and 2009 were similar with regard to type of insurance, parity, gestational age, multiple births, and cesarean sections. Overall, NFF improved after program implementation (odds ratio = 1.12, 95% confidence interval 1.02–1.23). In 2009, NFF rates at 2 months, 4 months, 6 months, and 9 months were greater than 2007 rates by 10%, 15%, 11%, and 9%, respectively. Logistic growth curve analysis indicated the difference across these time points was significant between 2007 and 2009.
Conclusion
A routine post-discharge outpatient lactation visit coordinated within a primary care practice improved breastfeeding initiation and intensity. This effect was sustained for 9 months.
Introduction
Although breastfeeding is known to be the ideal form of infant nutrition, providing numerous health benefits to both mother and child,1 the United States continues to struggle with improving breastfeeding duration and exclusivity.2 Recent promotion efforts, including the Baby Friendly Hospital Initiative (BFHI), have improved breastfeeding initiation,3–6 but studies show continued outpatient support is needed to improve breastfeeding duration.6,7 Meta-analyses of prenatal and postnatal primary care interventions suggest that interventions with face-to-face support, lay support, and a combination of pre- and postnatal breastfeeding interventions are more likely to increase breastfeeding rates and duration than less intensive support.8,9 Other studies show educating physicians to provide breastfeeding support improves breastfeeding rates10,11 as does breastfeeding counseling of patients by physicians.10–13 Yet, physicians cite lack of time and specific breastfeeding knowledge as barriers to providing this support.9,12
Outpatient lactation consultant (LC) visits provide more face-to-face time and education than physician support alone, yet few studies have investigated the effectiveness of outpatient LC visits on breastfeeding duration. LCs are specially trained to provide general breastfeeding support and to specifically address women's concerns of nipple pain and low milk supply, two reasons often cited for breastfeeding cessation.14–16 One study documenting the integration of an LC into an outpatient clinic reported preliminary data showing 53% of patients with an LC visit were breastfeeding at 4–6 months compared with only 23% of patients not seen by the LC.17 A study performed in a low income, inner-city population evaluating a comprehensive program of breastfeeding education and lactation support (prenatal and postpartum) found increased breastfeeding rates at initiation through 2 months post-delivery.18
Combining the physician and LC evaluation in the outpatient setting may address the need for breastfeeding support when physician time or specialized training is limited. We undertook this study to determine if an office visit with both a physician and an LC within 24–72 hours of discharge from the newborn hospitalization could have a positive impact on breastfeeding rates and exclusivity throughout the first year of life.
Subjects and Methods
Study site
The study was conducted at a suburban pediatric practice in Cleveland, OH viewed by the community as breastfeeding friendly. The practice is staffed by two nurse practitioners, five pediatricians, and one family physician with a typical patient volume of approximately 350 newborns per year. At baseline, the total breastfeeding rates for the practice were above the state average (82% vs. 65% initiation in 2007).2 At the time of the study, no hospital in the Cleveland area was designated Baby Friendly.
Newborns to the practice were delivered primarily at one of two local hospitals: an inner city hospital with breastfeeding discharge rates of 60.3% in 2007 and 63.9% in 2009 or a suburban hospital with breastfeeding discharge rates of 75% in June 2009 (2007 data were not available). The suburban hospital also reported a breastfeeding improvement effort involving banning formula discharge bags in March 2009 (as noted in electronic communications from community education staff at local hospitals).
Baseline standard of care
In 2007 the practice standard of care was for all infants to be seen in the office by 2 weeks of age. Only infants having in-hospital problems with jaundice or weight gain were seen within days of discharge. An International Board Certified LC (IBCLC) worked at the practice 3 days a week to help with breastfeeding difficulties either through phone support or scheduled in-person consultations. Because the IBCLC was an R.N., the 3 days were not exclusively dedicated to breastfeeding support; she also answered general medical calls for the practice.
Intervention
In October 2008, approximately 8 months after the addition of a family practitioner specializing in breastfeeding medicine, office policy for all breastfeeding infants changed. In order to be consistent with American Academy of Pediatrics policy,19,20 all healthy term breastfeeding infants were seen in the office by 3–5 days of life, depending on age at discharge. This visit was routinely scheduled with an IBCLC and precepted by a physician.
During these visits the IBCLC discussed the history and breastfeeding evaluation with an available physician, who also examined the patient and then decided on the necessary treatment plan. Visit length varied, depending on patient need, but typically lasted 45–60 minutes with the physician spending approximately 5 minutes in the room. IBCLC follow-up visits and phone calls were scheduled as needed. Routinely, infants were seen again by 2 weeks of age, by their primary physician, for a well newborn visit. To facilitate regular LC coverage, the IBCLC position changed to 5 days a week for 4 hours/day. The position became a dedicated IBCLC position and no longer shared R.N. responsibilities for the general pediatric practice. The 20 hours/week position was shared by two to three IBCLCs.
Study design
Data were collected from retrospective chart review of consecutive newborns to the practice born in the first 6 months of 2007 and 2009, pre- and post-implementation of the LC program. Patients who transferred into the practice after the newborn period were excluded from the study.
Measures
Feeding method was assessed from each well child note during the infant's first 9 months (2 weeks and 2, 4, 6, and 9 months). Well child notes were standardized forms with feeding method recorded via check boxes (one check box for breastfeeding and one for formula feeding). Non-formula feeding (NFF), the main outcome measure, was recorded if no formula use was documented in the medical record (i.e., when only the breastfeeding box was checked). NFF includes exclusive breastfeeding and continued NFF after the introduction of complementary foods. Partial breastfeeding was recorded if both formula and breastfeeding were marked for feeding method. Formula feeding was recorded if formula use only was recorded. Total breastfeeding rate at the practice (NFF and partial breastfeeding combined) was also assessed and is reported with initiation measured at 2 weeks and continued total breastfeeding at 6 months.
Other variables collected included infant gestational age, maternal age and parity, mode of delivery, neonatal intensive care unit admissions, and insurance status. Preterm infants were defined as infants less than 38 weeks of gestational age. The exact time of introduction of complementary feeding could not be evaluated as it was not consistently recorded in the chart, but typically occurred by 6 months of age. Secondary outcomes explored included number of days between hospital discharge and first office visit, as well as frequency of IBCLC visits.
Assessment of mothers' perception of program
After the LC program had been in place for 6 months, a subset of primiparous (n = 24) and multiparous (n = 16) mothers were chosen for a telephone survey to assess perception of the program. Questions asked included: “What did you think about having the first visit scheduled with a lactation consultant?,” “What, if anything, was helpful about the visit?,” and “What was your biggest breastfeeding challenge?”
Analyses
Categorical variables were described with frequency and percentage and compared using Pearson χ2 tests. Continuous variables were described as means and range or median and SD as appropriate. Logistic growth curve and χ2 analyses were used to test the association between intervention status and NFF and trends over time. The total number of cases available for the analyses (n = 350) provides 80% power for a χ2 test, one-sided p value of 0.05, to detect modest differences between the women seen in 2007 and those seen in 2009.
The study procedures were approved by the Institutional Review Board of University Hospitals of Cleveland.
Results
The final sample included 350 patients (166 in 2007 and 184 in 2009). Median maternal age was 32 years, and median gestational age was 39 weeks. Multiple birth rate and cesarean rate were 5% and 32%, respectively, with most patients (84%) having private insurance. Mothers and infants in 2007 and 2009 were found to be similar in regard to type of insurance, parity, gestational age, and rate of multiple births and cesarean sections (Table 1). Percentage preterm and full-term births were also similar by year, although significantly more infants were admitted to the neonatal intensive care unit in 2007 compared with 2009 (p = 0.004).
Table 1.
Mother and Infant Characteristics
| Sample characteristic | Total (n = 350) | 2007 (n = 166) | 2009 (n = 184) | p valuea |
|---|---|---|---|---|
| Infant | ||||
| Gestational ageb | 39 (26–42) | 38.6 (2.4) | 38.9 (1.6) | 0.157 |
| Preterm | 62 (18%) | 27 (16%) | 35 (19%) | 0.598 |
| Full term | 273 (78%) | 129 (78%) | 144 (78%) | 0.598 |
| Admitted to NICU | 33 (9%) | 24 (15%) | 9 (5%) | 0.004 |
| Mother | ||||
| Ageb | 32 (18–46) | 31.5 (5.5) | 31.7 (5.0) | 0.660 |
| First pregnancy | 133 (38%) | 67 (40%) | 66 (36%) | 0.471 |
| First delivery | 165 (47%) | 80 (48%) | 85 (46%) | 0.768 |
| Twin or triplet pregnancy | 19 (5%) | 11 (7%) | 8 (4%) | 0.347 |
| Cesarean section | 113 (32%) | 50 (30%) | 63 (34%) | 0.425 |
| Private insurance | 294 (84%) | 141 (85%) | 153 (83%) | 0.720 |
For continuous variables, independent t test p values are reported; for categorical variables, Pearson χ2 test p values are reported.
For continuous variables, median (range) is reported for the total sample, and mean (SD) is reported for the stratified sample; otherwise, for categorical variables, frequency (%) is reported.
NICU, neonatal intensive care unit.
Use of IBCLCs increased significantly once the routine post-discharge LC program was in place. In the first 6 months of 2009, practice IBCLCs saw 80.4% of newborns at the practice at least once, compared with only 20.5% in 2007. Total number of IBCLC visits increased from 51 visits in 2007 to 311 in 2009, with 45.7% of mothers visiting a IBCLC more than once in 2009 compared with only 7.2% in 2007 (p < 0.001).
Mean age at which infants were first seen in the practice also significantly improved after the LC program was implemented from 11.9 days of life in 2007 to 6.3 days of life in 2009 (p < 0.001). Days between hospital discharge and first clinic visit also decreased from 7.1 days to 3.0 days (p < 0.001). Total breastfeeding initiation in 2009 was 89%, compared with 82% in 2007 (p = 0.057), and total breastfeeding rate at 6 months was 61% in 2009 compared with 54% at baseline (p = 0.251).
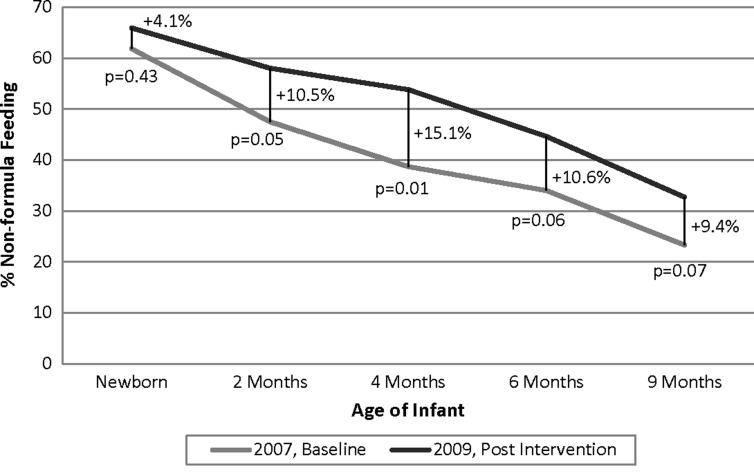
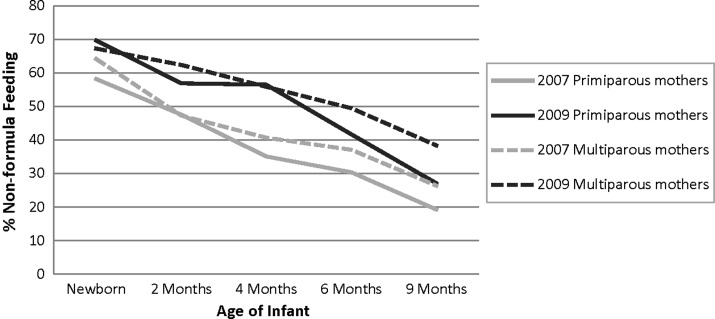
NFF rates were seen to improve after program implementation. Follow-up through 9 months was completed for 87% of enrolled patients, and this rate was similar between the two years. Those lost to follow-up, including patients who transferred out of the practice, were treated as missing data for the remaining analyses. In 2009, NFF rates at 2 months, 4 months, 6 months, and 9 months were greater than 2007 rates by 10%, 15%, 11%, and 9%, respectively (Fig. 1). Logistic growth curve analysis indicated these differences across time points were significant when controlling for neonatal intensive care unit admission (odds ratio = 1.12, 95% confidence interval 1.02–1.23). Figure 2 shows NFF rates were consistently higher for both primiparous and multiparous mothers over 9 months, after implementation of the LC program.
FIG. 1.
Non-formula feeding rates pre- and post-implementation of lactation consultant program.
FIG. 2.
Non-formula feeding rates for primiparous and multiparous mothers pre- and post-implementation of lactation consultant program.
Follow-up phone interviews were completed by a total of 14 mothers (six primiparous and eight multiparous). These data indicated most mothers saw value in the LC program and were pleased with the breastfeeding support provided: “Loved the lactation support” and “Really excellent support.” Almost all mothers, primiparous and multiparous, used the word “helpful” when they were asked their thoughts about having their babies' first clinic visit scheduled with the LC: “Definitely helpful” and “This visit was more helpful than last ones with previous children.” However, one multiparous mother who had successfully breastfed her previous four children felt it was a “hassle” to come in so early after birth, although she noted the visit would have been helpful if she had breastfeeding difficulties.
When asked what was most helpful about the visit, primiparous mothers were more likely to mention something specific, typically regarding comfort or usefulness: “Helped make the process more calm” and “Helped a lot with positioning.” Multiparous mothers cited specifics less, unless they reported experiencing breastfeeding challenges (e.g., trouble latching, milk supply concerns); then they were more likely to cite instruction about specific techniques when asked what was helpful. It was unclear how valuing the support corresponded with the current feeding method.
Discussion
When compared with usual care, home visits, peer counselors, and clinic visits for breastfeeding support of mothers have all been identified as beneficial for increasing breastfeeding initiation and duration.7,9,10,18–21 The few previous studies exploring outpatient lactation support also showed increases in breastfeeding rates, although for limited duration.9,18 In support of these findings the current study shows that in-person, in-office, early breastfeeding support can increase breastfeeding initiation, short-term duration, and long-term duration, consistent with the U.S. Preventive Services Task Force review.8
Our intervention differed from previous studies in that we routinely scheduled each breastfeeding mother with an IBCLC early postpartum. Any available physician in the office precepted the IBCLC visit. Although breastfeeding support was present in the practice prior to the LC program, the systematic implementation of IBCLCs was seen to significantly improve NFF rates through 9 months, even with a single postnatal-only intervention. This visit format allows for more time intensive breastfeeding support to be provided by the IBCLC while still showing clinician support of breastfeeding. Furthermore, clinician supervision of the visit enables appropriate monitoring of jaundice and weight gain as recommended by American Academy of Pediatrics guidelines.22,23
These findings are limited by the biases of a retrospective study. Precise distinction of NFF and partial breastfeeding could be limited by the degree of documentation in the medical record. We were unable to comment on the duration of exclusive breastfeeding before the introduction of complementary foods and continued breastfeeding past the 9-month well child visit since that information was not routinely recorded. However, these limitations are unlikely to have substantively differed for the two data collection years and therefore minimize the bias. Even with these limitations, the findings show a significant increase in breastfeeding intensity following the study intervention.
It is also worth noting that the study was conducted in a breastfeeding-supportive practice on a generally well-educated patient population. We did not provide specific physician education, but it is possible that the presence of a physician specializing in breastfeeding medicine may have increased the general breastfeeding knowledge at the practice. These factors should be considered when implementing this intervention to other practice settings as physician breastfeeding knowledge has been shown to be important in regard to breastfeeding success.10–13
Changes in local delivery hospitals' breastfeeding policies may also confound these results. Although local breastfeeding initiation may be increasing, comparable local breastfeeding duration data were not available to address this limitation. However, previous research has shown that while hospital-based promotion efforts like the BFHI can help to improve exclusive breastfeeding initiation, continued support is needed to maintain rates post-discharge.7 The current study offers one such program.
The significant strength of this study is that the intervention embraces the existing medical system structure. Our intervention did not require special change to practice routine beyond integrating an initial newborn lactation visit with the early breastfeeding newborn visit that is recommended by the American Academy of Pediatrics policy.22,23 Because the physician evaluates the patient, the visit is reimbursed as a general medical visit. We have found these reimbursements sufficiently cover LC salaries; a study evaluating the financial soundness of an expanded practice LC program at another middle-sized private pediatric practice noted a profit.24 Our follow-up data also indicate patients were pleased with the intervention, finding the support helpful, thus suggesting the program may improve patient satisfaction.
The 9-month follow-up of breastfeeding rates is an additional noteworthy strength, as similar studies reported more limited follow-up.17,18
Conclusion
A routine post-discharge outpatient lactation visit coordinated within a primary care practice is one way to support breastfeeding mothers and to improve breastfeeding initiation and duration.
Future studies will need to evaluate program implementation in other settings. Given that other programs have noted the benefits of early postpartum support on breastfeeding rates,18,21 it is reasonable to expect that similar consistent outpatient support would improve breastfeeding initiation and duration in other settings. Future studies will also need to evaluate the feasibility of this program in settings with a lower volume of newborn visits.
Acknowledgments
Special thanks to Shelly Senders, M.D. and the staff at Senders Pediatrics for their continued support in improving breastfeeding practices. Thanks to Maya Bolman, Beth Hurd, Vida LePage, Anne Vanic, and Darlene Walker for their excellent patient care and their assistance with data collection. This project was completed in part by the Culture of Inquiry Fellowship, funded by a Title VII grant from the Health Resources and Services Administration (DHHS/HRSA D54HP05444-01-00, 2008).
Disclosure Statement
No competing financial interests exist.
References
- 1.Ip S. Chung M. Raman G, et al. Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries. Agency for Healthcare Research and Quality; Rockville, MD: 2007. Evidence Report/Technology Assessment No. 153. AHRQ Publication Number 07-E007. [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. www.cdc.gov/breastfeeding/data/NIS_data/ [Sep 15;2010 ]. www.cdc.gov/breastfeeding/data/NIS_data/
- 3.World Health Organization. Global Strategy for Infant and Young Child Feeding. Fifty-Fifth World Health Assembly, World Health Organization; Geneva: 2003. [Google Scholar]
- 4.World Health Organization. Ten Steps to Successful Breastfeeding. World Health Organization; Geneva: 1998. [Google Scholar]
- 5.World Health Organization. Evidence for the Ten Steps to Successful Breastfeeding. World Health Organization; Geneva: 1998. [Google Scholar]
- 6.Kramer MS. Promotion of Breastfeeding Intervention Trial (PROBIT): A randomized trial in the Republic of Belarus. JAMA. 2001;285:413–420. doi: 10.1001/jama.285.4.413. [DOI] [PubMed] [Google Scholar]
- 7.Coutinho SB. Lira PIC. Lima MC, et al. Comparison of the effect of two systems for the promotion of exclusive breastfeeding. Lancet. 2005;366:1094–1100. doi: 10.1016/S0140-6736(05)67421-1. [DOI] [PubMed] [Google Scholar]
- 8.Chung M. Raman G. Trikalinos T, et al. Interventions in primary care to promote breastfeeding: An evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149:565–582. doi: 10.7326/0003-4819-149-8-200810210-00009. [DOI] [PubMed] [Google Scholar]
- 9.Oliveira MIC. Camacho LAB. Tedstone AE. Extending breastfeeding duration through primary care: A systematic review of prenatal and postnatal interventions. J Hum Lact. 2001;17:326–343. doi: 10.1177/089033440101700407. [DOI] [PubMed] [Google Scholar]
- 10.Labarer J. Gelbert-Baudino N. Ayral A, et al. Efficacy of breastfeeding support provided by trained clinicians during an early, routine, preventive visit: A prospective, randomized, open trial of 226 mother-infant pairs. Pediatrics. 2005;115:e139–e146. doi: 10.1542/peds.2004-1362. [DOI] [PubMed] [Google Scholar]
- 11.Feldman-Winter L. Barone L. Milcarek B, et al. Residency curriculum improves breastfeeding care. Pediatrics. 2010;126:289–297. doi: 10.1542/peds.2009-3250. [DOI] [PubMed] [Google Scholar]
- 12.Taveras EM. Li R. Grummer-Strawn L, et al. Opinions and practices of clinicians associated with continuation of exclusive breastfeeding. Pediatrics. 2004;113:e283–e290. doi: 10.1542/peds.113.4.e283. [DOI] [PubMed] [Google Scholar]
- 13.Taveras EM. Capra AM. Braveman PA, et al. Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics. 2003;112:108–115. doi: 10.1542/peds.112.1.108. [DOI] [PubMed] [Google Scholar]
- 14.Ahluwalia IB. Morrow B. Hsia J. Why do women stop breastfeeding? Findings from the Pregnancy Risk Assessment and Monitoring System. Pediatrics. 2005;116:1408–1412. doi: 10.1542/peds.2005-0013. [DOI] [PubMed] [Google Scholar]
- 15.Declercq E. Sakala C. Corry M, et al. Listening to mothers: Report of the first national US survey of women's childbearing experiences. J Perinat Med. 2003;31:350–351. doi: 10.1111/j.1552-6909.2002.tb00087.x. [DOI] [PubMed] [Google Scholar]
- 16.Sheehan D. Krueger P. Watt S, et al. The Ontario Mother and Infant Survey: Breastfeeding outcomes. J Hum Lact. 2001;17:211. doi: 10.1177/089033440101700304. [DOI] [PubMed] [Google Scholar]
- 17.Lukac M. Riley JK. Humphrey AD. How to integrate a lactation consultant in an outpatient clinic environment. J Hum Lact. 2006;22:99–103. doi: 10.1177/0890334405283622. [DOI] [PubMed] [Google Scholar]
- 18.Brent NB. Redd B. Dworetz A, et al. Breast-feeding in a low-income population. Program to increase incidence and duration. Arch Pediatr Adolesc Med. 1995;149:798–803. doi: 10.1001/archpedi.1995.02170200088014. [DOI] [PubMed] [Google Scholar]
- 19.Britton C. McCormick FM. Renfrew MJ, et al. Support for breastfeeding mothers. Cochrane Database Syst Rev. 2009;1:CD001141. doi: 10.1002/14651858.CD001141.pub3. [DOI] [PubMed] [Google Scholar]
- 20.Anderson AK. Damio G. Young S, et al. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Arch Pediatr Adolesc Med. 2005;159:836–841. doi: 10.1001/archpedi.159.9.836. [DOI] [PubMed] [Google Scholar]
- 21.McKeever P. Stevens B. Miller K, et al. Home versus hospital breastfeeding support for newborns: A randomized controlled trial. Birth. 2002;29:258–265. doi: 10.1046/j.1523-536x.2002.00200.x. [DOI] [PubMed] [Google Scholar]
- 22.Maisels M. Baltz R. Bhutani V, et al. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316. doi: 10.1542/peds.114.1.297. [DOI] [PubMed] [Google Scholar]
- 23.Gartner LM. Morton J. Lawrence RA, et al. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 24.Dahlquist N. Rosqvist J. Lactation support in a busy pediatric practice; who pays the price? [abstract 8] Breastfeed Med. 2007;2:180. [Google Scholar]