Type 2 diabetes is a serious, costly, and potentially preventable public health problem in the U.S., and both the prevalence and incidence of diabetes have increased rapidly since the mid-1990s (1). Currently, >7% of adults in the U.S. have been diagnosed with type 2 diabetes, and diabetes-related care accounts for 11% of all U.S. health care expenditures (2).
African Americans bear a disproportionate burden from diabetes and its complications. Compared with Caucasians, African Americans are almost twice as likely to suffer from type 2 diabetes and to experience diabetes-related blindness and lower-limb amputations, and two to six times more likely to have kidney disease (3). Furthermore, these disparities are enhanced when in tandem with other axes of inequality, such as geographic region, age, or sex (4).
Health inequalities in diabetes care can be conceptualized as differences in the quality of diabetes self-management (DSM) and of the medical care received. African Americans with diabetes experience more difficulties in DSM than Caucasians (5,6). Several reasons contribute to the observed differences, namely that African Americans often present cultural beliefs about their medical care and difficulties with language or low health literacy, which interfere with the success of DSM activities. Additionally, racial disparities in health services access and delivery are also thought to contribute to the observed differences, as African Americans are less likely to have routine glycosylated hemoglobin (HbA1c) testing, lipid panels, and retinopathy screening than their Caucasian counterparts (7,8).
In the past decade, there has been a surge in the development and implementation of quality improvement interventions led by the health care sector, which aim to decrease the burden of social inequalities in diabetes care. According to the Chin et al. (9) conceptual framework, those interventions can be classified as targeted to the patients, the health care system, or both. Patient-level interventions are focused on the improvement of DSM, tackling aspects such as medication intake, diet, exercise, self-monitoring, and the appropriate use of health care services (10). Interventions targeting the health care system are a broad type of interventions that address the quality of medical care. These can be focused on the improvement of the structure and/or process of care.
A considerable part of these interventions has specifically targeted African Americans with diabetes. However, to the best of our knowledge, there have been only a few attempts to systematically review the quality improvement interventions aimed at this relevant vulnerable group. Previous systematic reviews have analyzed the topic more broadly, focusing either on socially disadvantaged diabetic patients (11,12) or on ethnic minorities (9,10,13–15), observing that health care–promoted interventions can be effective in improving both processes of care and health outcomes. A recently published systematic review evaluated the effect of food-related interventions for African American women with type 2 diabetes, observing improvements in food practices and/or in glycemic control (16).
Because of the increased prevalence and worsened outcomes of type 2 diabetes in African Americans, along with the idiosyncratic characteristics of diabetes care, which, as before mentioned, include both individual and system-related variables, it is thus timely to conduct a systematic review specifically focusing on the interventions for this population. Therefore, the main goals of this systematic review were to identify and characterize health care–led interventions aimed at improving the quality of care in African Americans with diabetes. Additional goals were to assess the effectiveness of each intervention, to establish the characteristics associated with a greater probability of success, and to analyze how the interventions and its features evolved over the years.
RESEARCH DESIGN AND METHODS
The present work is part of a broader systematic review aimed to identify and analyze health care interventions to reduce social inequalities in diabetes care. The review and its procedures were planned, conducted, and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (17).
Data sources and searches
A comprehensive core search strategy was developed for Medline through Ovid (combining MeSH terms and keywords) and then adapted and implemented in EMBASE, Current Contents Connect, and CINAHL (Supplementary Table 1). Gray literature and additional articles were searched in 10 more bibliographic sources. The search was not restricted by language or publication date. Backward and forward citation searches of all the selected articles were performed in ISI Web of Knowledge. All searches were conducted in July 2012. Detailed information regarding the bibliographic databases searched, including the date when the search was performed and the number of references retrieved, is available in Supplementary Table 2. A bibliographical database was created using Reference Manager Professional Edition (version 10) and used to store and manage the retrieved references.
Study selection
We included randomized controlled trials (RCTs) and quasi-experimental studies (QEs) evaluating the effectiveness of health care–led interventions aimed at improving the quality of type 2 diabetes care in African Americans (including both self-care and medical care).
Specifically, we selected quality improvement interventions targeting patients, the health care system, or both. Health care–promoted, patient-targeted interventions were defined as those interventions led by health care professionals and aimed at improving any aspect of DSM (promotion of physical activity, nutritional/dietary education, glycemic self-monitoring, use of health care services, etc.). Interventions targeting health care were defined as those aimed at improving the quality of care provided by the health care system (primary, secondary, and tertiary), including the implementation of changes in the structure or processes of care provided to African Americans. Multifaceted interventions were defined as those interventions that included two or more components targeting both patients and the health care system, as previously defined.
We did not apply sex, age, language, or date of publication restrictions. Because some of the studies included patients from different ethnic groups, we only included those with participants that were predominantly African Americans (90% or more).
The titles and abstracts of the documents retrieved by the search strategy were screened for eligibility, and full texts of those meeting the selection criteria were obtained and read. Those that met the criteria described above were included. Two reviewers independently screened citations, and any disagreements about the document eligibility were resolved by a third reviewer.
Data extraction and quality assessment
A data extraction form was developed to record the general characteristics of the study (number of participants, epidemiological design, and outcome measures) and specific characteristics of the intervention (target of the intervention, duration, providers, population of study, setting, and type of intervention, including its main components). For articles that referenced previous publications (e.g., describing needs assessments or interventions), the original publication was retrieved and relevant data summarized. The results were later transferred to a Microsoft Access database.
The methodological quality of the studies was assessed using “The Quality Assessment Tool for Quantitative Studies” (18), which evaluates both internal and external validity. The methodological quality of each article was classified according to three categories (strong, moderate, or weak) based on six aspects: selection bias, study design, confounders, blinding, data collection, and withdrawals and dropouts. Two reviewers independently conducted the quality assessment, and a third reviewer solved any discrepancies.
Data synthesis and analysis
Results were summarized both qualitatively and quantitatively. Interventions were classified into three groups: interventions targeting patients, the health care system, or both (multifaceted).
The qualitative summary included a description of the features and main outcomes of each group of interventions, whereas in the quantitative component, frequencies and percentages were calculated for the categorical variables, and median, minimum, and maximum were calculated for the continuous variables (duration of the intervention and number of participants). The overall effectiveness of each intervention was estimated. When data were available, meta-analyses of the effect of the intervention on glycemic control were also conducted.
Estimation of the overall effectiveness.
Due to the high number and heterogeneity of the outcome measures used to assess the interventions in most of the studies, an assessment of the overall effectiveness of each intervention was performed based on the percentage of outcome variables that showed statistically significant improvement, established as P < 0.05, after the intervention. Specifically, for those interventions conducted and assessed through an RCT, the percentage of outcome measures that improved significantly after the intervention in the experimental group in comparison with the control group was calculated. Similarly, for those interventions that used a before-after quasi-experimental without control group method, the percentage of outcome measures that improved significantly after the intervention, when compared with baseline measures, was also calculated. Accordingly, the following categories of effectiveness were established: 1) highly effective interventions, for those interventions that showed statistically significant improvements in >75% of the total outcome measures; 2) partially effective interventions, for improvements between 25 and 75% of the outcome measures; and 3) low-effectiveness interventions, when improvement was observed in less than one-quarter of the outcome measures. Some interventions also differentiated between primary and secondary outcomes. In order to incorporate this differentiation in our estimation of the effectiveness, primary outcome measures, as specified by the authors, were given a 10-fold weight. This categorization was adopted to manage the heterogeneity between studies, which used a high number of outcome measures.
Finally, a temporal trend analysis of characteristics, methodological quality, and effectiveness of the interventions was conducted. χ2 test was used in order to assess differences between groups in the temporal trend analysis.
Meta-analyses.
Three independent meta-analyses were planned in order to estimate the effects of the three main types of interventions conceptualized (targeted to patients, the health care system, or both) on HbA1c. This was achieved through the comparison of the final mean HbA1c between the intervention and the control group. Selection criteria for the meta-analyses included RCTs comparing the intervention with usual care or minimal intervention and reporting HbA1c in the control and experimental group before and after the completion of the intervention. According to these criteria, it was only possible to conduct the meta-analysis of the interventions targeting patients. The HbA1c levels in each study were extracted as mean ± SD. This information was transformed into weighted mean difference, and 95% CIs were calculated for all eligible studies in the meta-analysis and combined using random-effects models. Heterogeneity was quantified by the I2 statistic, where I2 ≥50% was considered evidence of substantial heterogeneity (19). Sources of heterogeneity were investigated by a Galbraith chart. A sensitivity analysis, excluding the studies with higher risk of bias, was also conducted. Publication bias was quantitatively assessed with Begg and Egger tests.
A meta-regression analysis was also performed to assess the possible effects of characteristics deemed potentially relevant, namely, duration of the intervention, number of sessions, setting (primary care, secondary/tertiary care, or nonclinical), sociodemographic characteristics of the participants (age, sex, and geographic region), intervention culturally adapted to the target population (yes or no), professional background of the providers (general practitioner, nurse, dietitian/nutritionist, or endocrinologist), use of at least one peer provider (yes or no), provision of telephone reinforcement (yes or no), and intervention format (individual, group, or combination of both).
Both the overall assessment of the effectiveness and the meta-analyses included a sensitivity analysis, which was performed to assess whether our findings were related to the methodological quality of the included studies, by excluding those with low methodological quality.
Descriptive analyses were conducted with the software IBM SPSS Statistics, version 20. Temporal trend charts were generated with Microsoft Excel 2010. Meta-analyses and meta-regressions were conducted with Stata, version 11.2. For all the analyses, statistical significance was accepted at P < 0.05.
RESULTS
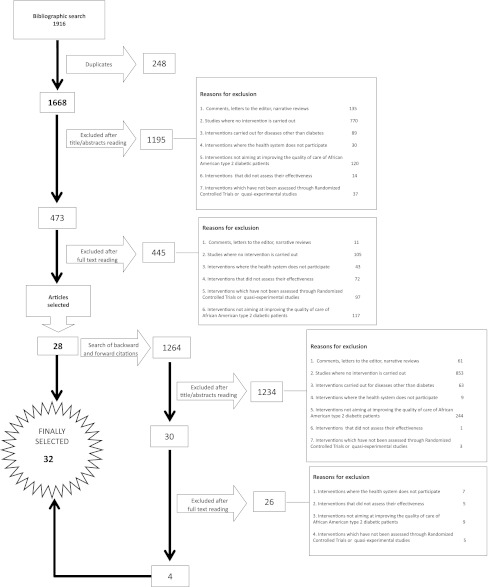
Search results are summarized in the PRISMA flow diagram (Fig. 1). The initial search identified a total of 1,916 citations, 248 of which were duplicated. Title and abstract screening of the remaining 1,668 citations resulted in the inclusion of 473 citations for further review. After examination of full text articles, 28 articles were identified as being eligible. The search of backward and forward citations of these 28 articles retrieved 4 additional articles, resulting in 32 articles included (20–51), which reported 31 studies.
Figure 1.
PRISMA flowchart of the selection process.
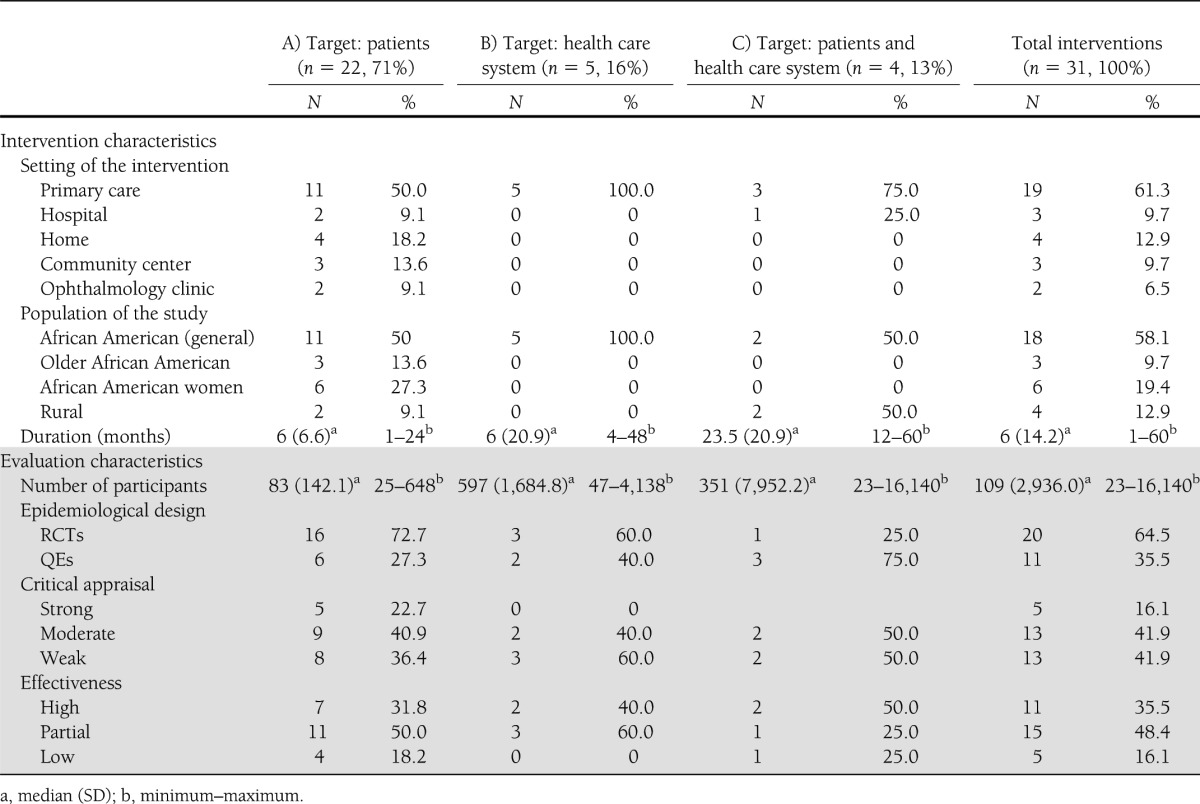
Features and effectiveness of the interventions
Table 1 provides aggregated information of the characteristics and outcomes of the interventions. Twenty-two interventions (71%) targeted patients (20–24,26,27,29,30,32,35–37,39,40,42,44–47,50,51), five (16%) targeted the health care system (31,34,41,43,48,49), and four (13%) (25,28,33,38) were multifaceted, addressing both patients and the health care system. The length of the interventions ranged from 1 to 60 months (median 6 months), and the number of participants varied between 23 and 16,140, with a median of 170 participants. The majority of the interventions (61%) took place in primary care, with the remaining being conducted in secondary or tertiary care or in nonclinical settings (specifically in community centers or participants’ homes).
Seventy percent of the studies were RTCs, whereas approximately one-third used a QE procedure. Physiological measures were the most frequently used outcome. Several studies also incorporated measures related to diabetes self-care habits or diabetes knowledge. Of the 31 studies critically appraised, 5 were considered methodologically strong, 13 moderate, and 13 weak. Most frequent methodological flaws were high risk of selection and confounding bias. Eleven interventions were considered highly effective (36%), 15 were partially effective (48%), and 5 had low effectiveness (16%). Sensitivity analyses excluding results of the studies rated as methodologically weak indicated similar proportions (33, 50, and 17% for high, medium, and low effectiveness, respectively).
1) Interventions targeting diabetic African American patients.
Full details of the characteristics and outcomes of each intervention are provided in Supplementary Table 3. Two of the 22 interventions targeting patients aimed to increase patient’s attendance to screening services for the prevention of diabetes complications (23,32), whereas the remaining 20 aimed at promoting diabetes self-management. This included different strategies, mainly diabetes education, coping skills training, physical activity promotion, and dietary advice. Most of these interventions were culturally adapted, which mainly consisted of adapting the educational components to African American cultural characteristics and the inclusion of peer providers.
Sixteen of the studies analyzing the effectiveness of interventions targeting patients conducted an RCT (72%). Five studies were rated as methodologically strong, nine moderate, and eight weak. Eighteen interventions (82%) were rated as highly or partially effective, showing a positive impact both on process measures (such as diabetes knowledge or adherence to medication) and clinical and psychological outcomes and quality of life.
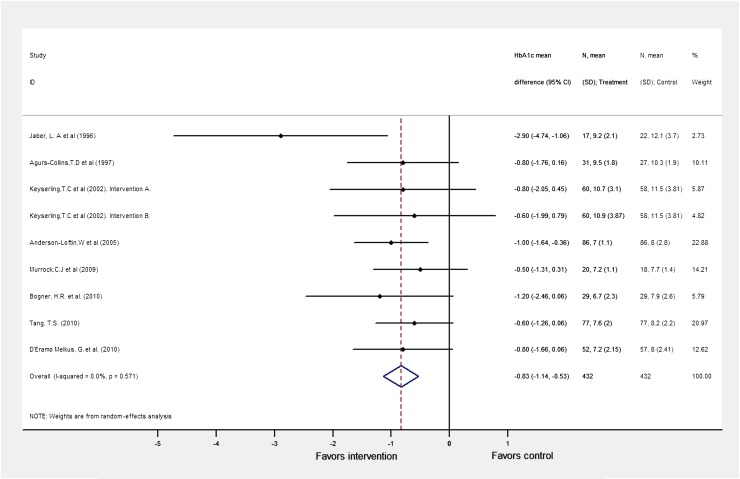
Nine studies met the selection criteria for the meta-analyses (20,22,24,27,30,36,37,42,45). A first meta-analysis was conducted to assess possible baseline HbA1c differences between intervention and control groups, observing no statistically significant differences (HbA1c mean difference = −0.02 [95% CI −0.37 to 0.33]). Subsequently, a second meta-analysis was conducted in order to estimate the pooled difference in the %HbA1c between the intervention and control group after the interventions. The heterogeneity among the studies was high; 50.2% of the total variability observed after the intervention was explained by the heterogeneity among studies. Using a Galbraith chart, it was possible to identify that one of the studies greatly contributed to the heterogeneity (22), and its exclusion reduced the variability due to heterogeneity from 50.2 to <0.1%. Eight studies describing nine interventions were thus included in the meta-analysis, reporting on 864 patients (432 in the intervention and 432 in the control group). As ascertained by a random-effects model, the combined effect of the intervention produced a significant reduction in the overall HbA1c of 0.83 points (95% CI −1.14 to −0.53) (Fig. 2). There was no evidence of publication bias (P = 0.07 using Egger test; P = 0.08 using Begg test). A sensitivity analysis was also conducted by excluding the study with a higher risk of bias (36), showing similar results (overall HbA1c mean difference = −0.77 [95% CI −1.08 to −0.47]). The meta-regression showed that none of the features analyzed were significantly associated with increased effectiveness.
Figure 2.
Forest plot of RCTs investigating the effect of patient-targeted interventions on HbA1c. (A high-quality color representation of this figure is available in the online issue.)
2) Interventions targeted to the health care system.
Six articles reported five interventions targeting the health care system (31,34,41,43,48,49). These aimed to improve the quality of health care in general practices with a high percentage of African American patients through the implementation of changes in the structure and/or process of care. The interventions were eclectic, including the development of educational interventions for health care providers (31,43), the implementation of systems for the rapid turnaround of HbA1c (41,48), the establishment of circumscribed appointments, the incorporation of additional support staff, or increasing the follow-up effort through home visits or telephone/mailing contact (34).
Three of the interventions were assessed by RCTs and two by QEs. Two studies were rated as methodologically moderate and the remaining as weak. In relation to the effectiveness, two were highly effective and three were partially effective. The former were very similar, consisting of the implementation of a system to provide a rapid turnaround of HbA1c availability. Results showed that these interventions facilitated diabetes management, increased the frequency of intensification of therapy, and lowered HbA1c levels in patients with type 2 diabetes (41,48).
3) Multifaceted interventions.
Four multifaceted interventions were identified (25,28,33,38). They were complex interventions, combining diabetes DSM education programs and the implementation of organizational changes in the health care structure (e.g., the implementation of reminder systems and incorporation of case management or new clinical algorithms). Although no statistical differences were tested because of the low number of interventions, in comparison with the other two types of interventions previously described, multifaceted interventions were longer (median 23.5 months) and incorporated a higher number of participants (median 351).
Three studies conducted a QE, with only one following an RCT design. As for methodological characteristics, two were rated as methodologically moderate and two as weak. Two interventions displayed high effectiveness, whereas the other two were rated as having partial and low effectiveness.
Temporary trend
Although the first intervention to improve the quality of health care in African Americans with diabetes identified in this systematic review was published in 1996, almost 90% of the studies were published from 2000 onwards. Interventions targeting patients were the first type of intervention published and they increased constantly over time (Fig. 3). The first intervention targeting health care was published in 1999, whereas the first multifaceted intervention was published in 2002. The setting of the interventions switched from secondary/tertiary care, when interventions started being conducted, to primary care from 2001 onwards (a period in which 65% of interventions took place in general practices). However, in the last 4 years (from 2008 to 2012), the proportion of interventions taking place in nonclinical settings has increased by 200%. Differences between groups were statistically significant (P < 0.05).
Figure 3.
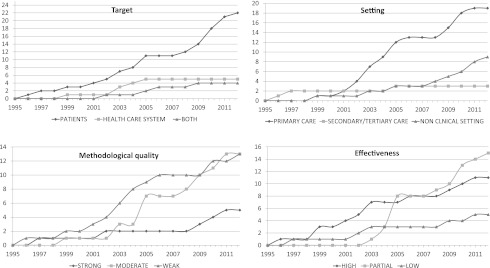
Temporal trends analysis. The y-axis represents the number of publications, and the x-axis represents the years.
The methodological quality of the studies improved over time, showing a turning point in 2008, the year after which the proportion of low-quality studies decreased from 53 to 25% and the proportion of high- and moderate-quality studies increased from 47 to 75% (no significant differences). Similarly, although no statistically significant differences were observed, the effectiveness of interventions improved in recent years: 73% of the interventions published prior to 2004 were highly or partially effective, and this proportion increased to 90% of the subsequently published interventions.
Table 1.
Characteristics of the interventions and of the studies evaluating their effectiveness
CONCLUSIONS
This systematic review identified 31 health care–promoted interventions specifically aimed at improving the quality of diabetes care in African Americans, most of which targeted patients. The evidence gathered showed that interventions targeting African American diabetic patients, which mainly included culturally adapted DSM education, reduced the percentage of HbA1c by 0.8%. A lower level of evidence was observed in relation to interventions targeting the health care system and multiple-target interventions, although available evidence suggests that they can be effective and have the potential to improve diabetes care and health outcomes.
Previous revisions have broadly evaluated strategies for improving the quality of diabetes care (52), the use of community-based approaches to prevent diabetes (53), and the effectiveness of DSM education (13,54). Also, research has been conducted to assess the effect of these interventions on racial/ethnic minority groups (9,10,14,15), and some recent studies have specifically reviewed the effect of dietary interventions on African Americans with diabetes or obesity patients (16,55). However, to the best of our knowledge, this is the first review focusing on health care system–promoted interventions to improve the quality of diabetes care in African Americans patients, i.e., on analyzing what the health care system has done until now in order to improve the quality of care of African American diabetic patients. The fact that most of the interventions analyzed have proven to be at least partially effective (only one out of five interventions analyzed showed to be ineffective) is consistent with what was previously observed in other reviews of interventions to reduce ethnic inequalities in health, both in the case of diabetes (10,11,13,15) and other chronic diseases such as cancer, asthma, or mental health (14). This is certainly a positive result and should encourage the implementation of actions that will ultimately contribute to decreasing health inequalities, thus promoting equal chances of having the maximum development for health.
The main strength of this study is the comprehensiveness of the search. Systematic and manual searches were performed in the most relevant bibliographic databases on biomedical research. Specific sites of gray literature were also searched, and searches were not restricted by language or publication year. As for the limitations of this review, results could have been constrained by the high proportion of studies with low methodological quality, especially among health care and multifaceted interventions, thus impacting the internal validity of the results. However, the sensitivity analysis, which excluded studies with a higher risk of bias, showed that the proportion of effective interventions remained similar, with ∼85% of the interventions displaying medium or high effectiveness. It is also a limitation that only experimental designs have been included, as sound methodological nonexperimental designs might reveal important information about the effectiveness of interventions (56). However, they also pose obstacles to the generalizability of results and it is not always possible to draw conclusions about causality, hence the decision to exclude them. Another limitation that is common to systematic reviews is the risk of publication bias, because interventions with demonstrated benefit are more likely to be published than those with no benefit, thus overestimating the effect of the interventions. Efforts have been made to minimize this possible bias, which included a thorough bibliographic search. Finally, because the studies examined different interventions and health outcomes at different levels and used distinct research methods and outcome variables, it was only possible to conduct a meta-analysis using pooled data for interventions targeting patients. To address this gap, a qualitative assessment was conducted by adapting a previously described method (12,57), which classified the effectiveness of each intervention in different categories. However, this method presents some limitations and its results should be taken cautiously as it is based on the proportion of outcome measures that achieved statistically significant improvement after the intervention, without taking into account the clinical significance of this improvement or the fact that some outcome measures might be more important than others.
Despite its limitations, this systematic review presented relevant and timely results. First of all, interventions exclusively focusing on patients were the most frequent type of intervention identified. However, the results of the present work showed a greater proportion of high effectiveness among those interventions targeting improvements in the structure or process of care, either by themselves or in tandem with patient-targeted interventions. This is consistent with previous findings, which demonstrated that interventions directed toward organizational structures and resources, which went beyond traditional diabetes education programs, were more likely to be successful (12). In this sense, the current review showed that this trend has been changing over the years, and more recent interventions frequently incorporate different elements to improve the quality of care.
The results obtained by the meta-analysis, regarding the effect on HbA1c of quality improvement strategies targeted to patients, are similar to those reported by Peek et al. (10), who observed a reduction of a mean HbA1c value of 0.69% in a multiethnic minority group of diabetic patients receiving culturally tailored interventions. Two additional meta-analyses assessed the effect of DSM education in a general diabetic population and also observed similar HbA1c reductions: 0.84 (54) and 0.48 (52). The meta-regression analysis tried to identify the common features of the highly effective patient-targeted interventions; however, it was not possible to identify consistent patterns, not even in the use of peer providers, the incorporation of individualized sessions, or cultural adaptation, which have been suggested to improve the effectiveness of DSM interventions in ethnic minority groups (9,10,12). These results seem to reinforce the hypothesis that at least in the research of interventions to improve quality of care, not all socially disadvantaged or ethnic minority groups can be considered and/or analyzed together, as there might be important sociocultural differences that can determine the features associated with a higher likelihood of success.
In relation to health care system–targeted interventions, two highly effective and similar interventions were identified, both focused on the improvement of the structure of care, specifically in the implementation of a system to make HbA1c values available at the time of a patient’s visit. These results suggest that this system could facilitate diabetes management, increase the frequency of intensification of therapy, and lower HbA1c levels in patients with type 2 diabetes (41,48). Notwithstanding the need to study this type intervention in more depth to confirm its effectiveness, these are important results, as this is a relatively simple and low-cost intervention that can easily be implemented in health centers.
The present work presents a review of the first 16 years (from 1996 to 2012) of interventions specifically aimed to improve the quality of diabetes care in African Americans. Temporal trend analysis showed that since its inception, these interventions have been evolving in different aspects. In this way, although interventions have been conducted mainly in clinical settings, initially in hospitals and later in general practices, the proportion of interventions taking place in nonclinical settings has increased in recent years. Moreover, the degree of sophistication of the interventions has grown over the years, with an increased number of participants and components being registered in the last years. As for the studies assessing the effectiveness of the interventions, it was also observed that their methodological quality is improving, and the proportion of interventions of low effectiveness is decreasing. All these findings suggest that research on these specific types of interventions has made significant progress in recent years.
However, there are still some challenges that need to be highlighted. First of all, it should be taken into consideration that although interventions conducted with African American patients with diabetes seem to be effective, it does not mean that interventions carried out with other ethnic minority groups will be equally effective. Different ethnic groups have different cultural characteristics that generate differences in diabetes self-care activities (e.g., nutritional habits, physical activity undertaken, and beliefs or myths about the disease and how to manage it) as well as the interaction between the patient and the health care system. That is why most of these interventions are tailored to the target population characteristics and therefore should be adapted prior to their implementation in other groups. Therefore, the results found in this review should not be extrapolated to other ethnic minorities; instead, specific revisions for each of these minority groups should be made.
The lack of methodologically high-quality studies has also been observed previously (14), representing an area for improvement. There is a notable need to conduct methodologically robust studies that target health care and multifaceted interventions. Although recent work has shown them to be useful in addressing general racial/ethnic disparities (5), evidence on African Americans is still scarce. Finally, although important cost-effectiveness analysis of these types of interventions has already been performed (58,59), ideally, future research should consider the systematic incorporation of an evaluation of the costs of the interventions to improve health care, in order to make decisions about the allocation of resources.
In conclusion, despite the methodological issues described above, this systematic review provides evidence about the key role that health care can play in reducing ethnic disparities in African American patients with type 2 diabetes by designing and conducting interventions aimed at this specific purpose.
Supplementary Material
Acknowledgments
This study was supported by the National Institute of Health Carlos III (Study PS09/00747) in partnership with the Andalusian Regional Ministry of Health (Study PI-0152).
No potential conflicts of interest relevant to this article were reported.
I.R.-C. and A.N.-C. selected articles, extracted information, and critically appraised and drafted the manuscript. I.R.-P. selected articles and reviewed the manuscript. M.R.-B. conducted the meta-analysis and contributed to the elaboration of the final version of the manuscript. L.S. and D.C.G. contributed to discussion and reviewed and edited the manuscript.
The authors thank Victor Sarmiento (Andalusian Agency for Health Technology Assessment, Andalusia, Spain) for conducting the bibliographic searches.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc12-1057/-/DC1.
References
- 1.Beckles GL, Zhu J, Moonesinghe R, Centers for Disease Control and Prevention (CDC) Diabetes - United States, 2004 and 2008. MMWR Surveill Summ 2011;60(Suppl.):90–93 [PubMed] [Google Scholar]
- 2.Dall TM, Zhang Y, Chen YJ, Quick WW, Yang WG, Fogli J. The economic burden of diabetes. Health Aff (Millwood) 2010;29:297–303 [DOI] [PubMed] [Google Scholar]
- 3.Brewer-Lowry AN, Arcury TA, Bell RA, Quandt SA. Differentiating approaches to diabetes self-management of multi-ethnic rural older adults at the extremes of glycemic control. Gerontologist 2010;50:657–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mullins CD, Blatt L, Gbarayor CM, Yang HWK, Baquet C. Health disparities: a barrier to high-quality care. Am J Health Syst Pharm 2005;62:1873–1882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golden SH, Brown A, Cauley JA, et al. Health disparities in endocrine disorders: biological, clinical, and nonclinical factors—an endocrine society scientific statement. J Clin Endocrinol Metab 2012;97:E1579–E1639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amoako E, Skelly AH. Managing uncertainty in diabetes: an intervention for older African American women. Ethn Dis 2007;17:515–521 [PubMed] [Google Scholar]
- 7.Brown AF, Gregg EW, Stevens MR, et al. Race, ethnicity, socioeconomic position, and quality of care for adults with diabetes enrolled in managed care: the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care 2005;28:2864–2870 [DOI] [PubMed] [Google Scholar]
- 8.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in medicare managed care. JAMA 2002;287:1288–1294 [DOI] [PubMed] [Google Scholar]
- 9.Chin MH, Walters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev 2007;64(Suppl.):7S–28S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peek ME, Cargill A, Huang ES. Diabetes health disparities: a systematic review of health care interventions. Med Care Res Rev 2007;64(Suppl.):101S–156S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eakin EG, Bull SS, Glasgow RE, Mason M. Reaching those most in need: a review of diabetes self-management interventions in disadvantaged populations. Diabetes Metab Res Rev 2002;18:26–35 [DOI] [PubMed] [Google Scholar]
- 12.Glazier RH, Bajcar J, Kennie NR, Willson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care 2006;29:1675–1688 [DOI] [PubMed] [Google Scholar]
- 13.Hawthorne K, Robles Y, Cannings-John R, Edwards AG. Culturally appropriate health education for type 2 diabetes in ethnic minority groups: a systematic and narrative review of randomized controlled trials. Diabet Med 2010;27:613–623 [DOI] [PubMed] [Google Scholar]
- 14.Beach MC, Gary TL, Price EG, et al. Improving health care quality for racial/ethnic minorities: a systematic review of the best evidence regarding provider and organization interventions. BMC Public Health 2006;6:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saxena S, Misra T, Car J, Netuveli G, Smith R, Majeed A. Systematic review of primary healthcare interventions to improve diabetes outcomes in minority ethnic groups. J Ambul Care Manage 2007;30:218–230 [DOI] [PubMed] [Google Scholar]
- 16.Sumlin LL, Garcia AA. Effects of food-related interventions for African American women with type 2 diabetes. Diabetes Educ 2012;38:236–249 [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs 2004;1:176–184 [DOI] [PubMed] [Google Scholar]
- 19.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 510 Oxford, U.K., Cochrane Collaboration, 2011. Available from www.cochranehandbook.org Accessed 18 August 2012
- 20.Agurs-Collins TD, Kumanyika SK, Ten Have TR, Adams-Campbell LL. A randomized controlled trial of weight reduction and exercise for diabetes management in older African-American subjects. Diabetes Care 1997;20:1503–1511 [DOI] [PubMed] [Google Scholar]
- 21.Amoako E, Skelly AH, Rossen EK. Outcomes of an intervention to reduce uncertainty among African American women with diabetes. West J Nurs Res 2008;30:928–942 [DOI] [PubMed] [Google Scholar]
- 22.Anderson RM, Funnell MM, Nwankwo R, Gillard ML, Oh M, Fitzgerald JT. Evaluating a problem-based empowerment program for African Americans with diabetes: results of a randomized controlled trial. Ethn Dis 2005;15:671–678 [PubMed] [Google Scholar]
- 23.Anderson RM, Musch DC, Nwankwo RB, et al. Personalized follow-up increases return rate at urban eye disease screening clinics for African Americans with diabetes: results of a randomized trial. Ethn Dis 2003;13:40–46 [PubMed] [Google Scholar]
- 24.Anderson-Loftin W, Barnett S, Bunn P, Sullivan P, Hussey J, Tavakoli A. Soul food light: culturally competent diabetes education. Diabetes Educ 2005;31:555–563 [DOI] [PubMed] [Google Scholar]
- 25.Anderson-Loftin W, Barnett S, Sullivan P, Bunn PS, Tavakoli A. Culturally competent dietary education for southern rural African Americans with diabetes. Diabetes Educ 2002;28:245–257 [DOI] [PubMed] [Google Scholar]
- 26.Basch CE, Walker EA, Howard CJ, Shamoon H, Zybert P. The effect of health education on the rate of ophthalmic examinations among African Americans with diabetes mellitus. Am J Public Health 1999;89:1878–1882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bogner HR, de Vries HF. Integrating type 2 diabetes mellitus and depression treatment among African Americans: a randomized controlled pilot trial. Diabetes Educ 2010;36:284–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bray P, Thompson D, Wynn JD, Cummings DM, Whetstone L. Confronting disparities in diabetes care: the clinical effectiveness of redesigning care management for minority patients in rural primary care practices. J Rural Health 2005;21:317–321 [DOI] [PubMed] [Google Scholar]
- 29.Carter EL, Nunlee-Bland G, Callender C. A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspect Health Inf Manag 2011;8:1b. [PMC free article] [PubMed] [Google Scholar]
- 30.D’Eramo Melkus G, Chyun D, Vorderstrasse A, Newlin K, Jefferson V, Langerman S. The effect of a diabetes education, coping skills training, and care intervention on physiological and psychosocial outcomes in black women with type 2 diabetes. Biol Res Nurs 2010;12:7–19 [DOI] [PubMed] [Google Scholar]
- 31.Din-Dzietham R, Porterfield DS, Cohen SJ, Reaves J, Burrus B, Lamb BM. Quality care improvement program in a community-based participatory research project: example of Project DIRECT. J Natl Med Assoc 2004;96:1310–1321 [PMC free article] [PubMed] [Google Scholar]
- 32.Ellish NJ, Royak-Schaler R, Higginbotham EJ. Tailored and targeted interventions to encourage dilated fundus examinations in older African Americans. Arch Ophthalmol 2011;129:1592–1598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gary TL, Batts-Turner M, Yeh HC, et al. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med 2009;169:1788–1794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gary TL, Bone LR, Hill MN, et al. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med 2003;37:23–32 [DOI] [PubMed] [Google Scholar]
- 35.Hill-Briggs F, Lazo M, Peyrot M, et al. Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J Gen Intern Med 2011;26:972–978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jaber LA, Halapy H, Fernet M, Tummalapalli S, Diwakaran H. Evaluation of a pharmaceutical care model on diabetes management. Ann Pharmacother 1996;30:238–243 [DOI] [PubMed] [Google Scholar]
- 37.Keyserling TC, Samuel-Hodge CD, Ammerman AS, et al. A randomized trial of an intervention to improve self-care behaviors of African-American women with type 2 diabetes: impact on physical activity. Diabetes Care 2002;25:1576–1583 [DOI] [PubMed] [Google Scholar]
- 38.Mahotière T, Ocepek-Welikson K, Daley MB, Byssainthe JP. A program to reduce the disparity in the rate of biennial lipid profiles between African-American and white Medicare beneficiaries with diabetes mellitus in New York City. J Community Health 2006;31:263–288 [DOI] [PubMed] [Google Scholar]
- 39.Mayer-Davis EJ, D’Antonio A, Martin M, Wandersman A, Parra-Medina D, Schulz R. Pilot study of strategies for effective weight management in type 2 diabetes: Pounds Off with Empowerment (POWER). Fam Community Health 2001;24:27–35 [DOI] [PubMed] [Google Scholar]
- 40.D’Eramo Melkus G, Spollett G, Jefferson V, et al. A culturally competent intervention of education and care for black women with type 2 diabetes. Appl Nurs Res 2004;17:10–20 [DOI] [PubMed] [Google Scholar]
- 41.Miller CD, Barnes CS, Phillips LS, et al. Rapid A1c availability improves clinical decision-making in an urban primary care clinic. Diabetes Care 2003;26:1158–1163 [DOI] [PubMed] [Google Scholar]
- 42.Murrock CJ, Higgins PA, Killion C. Dance and peer support to improve diabetes outcomes in African American women. Diabetes Educ 2009;35:995–1003 [DOI] [PubMed] [Google Scholar]
- 43.Phillips LS, Ziemer DC, Doyle JP, et al. An endocrinologist-supported intervention aimed at providers improves diabetes management in a primary care site: improving primary care of African Americans with diabetes (IPCAAD) 7. Diabetes Care 2005;28:2352–2360 [DOI] [PubMed] [Google Scholar]
- 44.Skelly AH, Carlson J, Leeman J, Soward A, Burns D. Controlled trial of nursing interventions to improve health outcomes of older African American women with type 2 diabetes. Nurs Res 2009;58:410–418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tang TS, Funnell MM, Brown MB, Kurlander JE. Self-management support in “real-world” settings: an empowerment-based intervention. Patient Educ Couns 2010;79:178–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tang TS, Funnell MM, Noorulla S, Oh M, Brown MB. Sustaining short-term improvements over the long-term: results from a 2-year diabetes self-management support (DSMS) intervention. Diabetes Res Clin Pract 2012;95:85–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tang TS, Gillard ML, Funnell MM, et al. Developing a new generation of ongoing: diabetes self-management support interventions: a preliminary report. Diabetes Educ 2005;31:91–97 [DOI] [PubMed] [Google Scholar]
- 48.Thaler LM, Ziemer DC, Gallina DL, et al. Diabetes in urban African-Americans. XVII. Availability of rapid HbA1c measurements enhances clinical decision-making. Diabetes Care 1999;22:1415–1421 [DOI] [PubMed] [Google Scholar]
- 49.Vetter MJ, Bristow L, Ahrens J. A model for home care clinician and home health aide collaboration: diabetes care by nurse case managers and community health workers. Home Healthc Nurse 2004;22:645–648 [DOI] [PubMed] [Google Scholar]
- 50.Walker EA, Stevens KA, Persaud S. Promoting diabetes self-management among African Americans: an educational intervention. J Health Care Poor Underserved 2010;21(Suppl.):169–186 [DOI] [PubMed] [Google Scholar]
- 51.Ziemer DC, Berkowitz KJ, Panayioto RM, et al. A simple meal plan emphasizing healthy food choices is as effective as an exchange-based meal plan for urban African Americans with type 2 diabetes. Diabetes Care 2003;26:1719–1724 [DOI] [PubMed] [Google Scholar]
- 52.Tricco AC, Ivers NM, Grimshaw JM, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet 2012;379:2252–2261 [DOI] [PubMed] [Google Scholar]
- 53.Satterfield DW, Volansky M, Caspersen CJ, et al. Community-based lifestyle interventions to prevent type 2 diabetes. Diabetes Care 2003;26:2643–2652 [DOI] [PubMed] [Google Scholar]
- 54.Steinsbekk A, Rygg LO, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res 2012;12:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fitzgibbon ML, Tussing-Humphreys LM, Porter JS, Martin IK, Odoms-Young A, Sharp LK. Weight loss and African-American women: a systematic review of the behavioural weight loss intervention literature. Obes Rev 2012;13:193–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care 2001;24:561–587 [DOI] [PubMed] [Google Scholar]
- 57.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ 2005;330:765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang ES, Zhang Q, Brown SE, Drum ML, Meltzer DO, Chin MH. The cost-effectiveness of improving diabetes care in U.S. federally qualified community health centers. Health Serv Res 2007;42:2174–2193; discussion 2294–2323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chin MH. Quality improvement implementation and disparities: the case of the health disparities collaboratives. Med Care 2011;49(Suppl.):S65–S71 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.