Insulin resistance, metabolic syndrome, and adipokine dysregulation are now implicated in hypertensive pulmonary vascular disease (1–3). Even in nonobese humans with idiopathic pulmonary arterial hypertension (IPAH), the prevalence of insulin resistance is nearly 50% (1,2), suggesting a link between glucose dysregulation and IPAH. Additionally, IPAH develops spontaneously in animal models of obesity and adipokine alterations (4). The underlying mechanisms by which metabolic mediators exacerbate or cause pulmonary vascular disease are unknown. We tested the hypothesis that improvements in metabolic hormones are associated with amelioration of pulmonary hemodynamics in a 48-year-old morbidly obese female IPAH patient who underwent bariatric surgery. Despite no change in IPAH therapy, she had dramatic hemodynamic improvement coupled with reduced insulin resistance, plasma lipids, and cholesterol levels.
The IPAH patient was New York Heart Association functional class III and desired bariatric surgery. After counseling about elevated surgical risk associated with anesthesia in IPAH patients, she underwent laparoscopic Roux-en-Y gastric bypass. Postoperative course was uncomplicated. She was stable on bosentan and sildenafil for 4 years preoperatively and postoperatively.
The patient had mild obstructive sleep apnea and was compliant with therapy throughout her course. She did not have obesity hypoventilation syndrome or a diagnosis of diabetes preoperatively, and her peripheral oxygen saturation was normal preoperatively without supplemental oxygen.
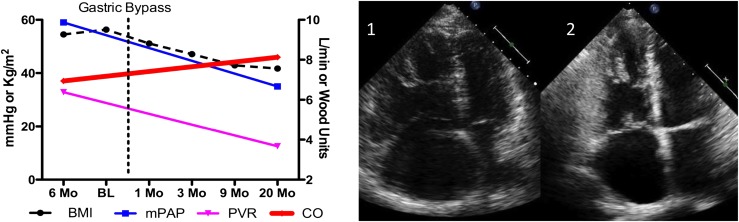
The patient’s BMI fell from 54 to 41 kg/m2, and body fat fell from 57 to 31% over 20 months (Fig. 1). She reported improved exercise tolerance and became functional class II. Within 1 month of the procedure, before significant weight loss, right ventricular function improved by echocardiography (Fig. 1). Right heart catheterization 20 months after surgery (Fig. 1) demonstrated marked improvement, including elevation in cardiac output despite 43 kg weight loss. Plasma markers of insulin resistance (homeostasis model assessment of insulin resistance), lipids, and adipokines were measured at three points over 20 months. There was a drop in homeostasis model assessment of insulin resistance from 2.60 to 1.18. Free fatty acid levels fell from 1.27 to 0.86 mmol/L, LDL fell from 143.8 to 109.6 mg/dL, and HDL rose from 47 to 63 mg/dL and triglycerides from 56 to 67 mg/dL. Plasma adipokines demonstrated decreased leptin level from 39.49 to 29.25 ng/mL. Ghrelin, adiponectin, and resistin showed substantial variation in plasma levels over 20 months. Weight loss and hemodynamic improvements correlated with reduction of insulin resistance, HDL, LDL, and free fatty acids. Although leptin dropped, there was no correlation between adiponectin, resistin, or ghrelin levels and hemodynamic improvement.
Figure 1.
Hemodynamic variables and echocardiography before and after bariatric surgery. A time course of effects of bariatric surgery on BMI and invasively measured hemodynamics are shown on the left panel. The right panel demonstrates right ventricular size before (1) and 1 month (mo) after (2) bariatric surgery. BL, baseline.
This single patient represents an experiment in nature in which modest improvement in morbid obesity through bariatric surgery in IPAH correlated with marked rapid improvement in pulmonary vascular disease severity, despite no change in IPAH-directed therapy. These dramatic hemodynamic improvements are not seen either spontaneously in IPAH or as a response after several years of stable oral therapy. These data point to insulin resistance, lipid metabolism, and possibly, leptin as potential mediators of pulmonary vascular disease and suggest that adiponectin, ghrelin, and resistin may be less important to human IPAH development. This patient experience illustrates new potential pathways of importance in metabolic regulation that may have therapeutic potential for this devastating disease.
Acknowledgments
This study was supported in part by National Institutes of Health Vanderbilt Clinical and Translational Science Award Grant UL1 RR024975.
No potential conflicts of interest relevant to this article were reported.
M.E.P. collected data and wrote the manuscript. J.H.N. edited the manuscript. D.B.W. contributed to discussion and reviewed and edited the manuscript. E.B. analyzed data and reviewed and edited the manuscript. I.M.R. collected data. A.R.H. collected and analyzed data and contributed to manuscript preparation. A.R.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Zamanian RT, Hansmann G, Snook S, et al. Insulin resistance in pulmonary arterial hypertension. Eur Respir J 2009;33:318–324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pugh ME, Robbins IM, Rice TW, West J, Newman JH, Hemnes AR. Unrecognized glucose intolerance is common in pulmonary arterial hypertension. J Heart Lung Transplant 2011;30:904–911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heresi GA, Aytekin M, Newman J, DiDonato J, Dweik RA. Plasma levels of high-density lipoprotein cholesterol and outcomes in pulmonary arterial hypertension. Am J Respir Crit Care Med 2010;182:661–668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Summer R, Fiack CA, Ikeda Y, et al. Adiponectin deficiency: a model of pulmonary hypertension associated with pulmonary vascular disease. Am J Physiol Lung Cell Mol Physiol 2009;297:L432–L438 [DOI] [PMC free article] [PubMed] [Google Scholar]