Abstract
OBJECTIVE
Few studies are currently available regarding the influence of sleep duration on glycemic control in diabetic patients. The objective of the current study was to examine the relationship between sleep duration, obesity, and the glycemic level in type 2 diabetic patients.
RESEARCH DESIGN AND METHODS
A total of 4,870 Japanese type 2 diabetic patients aged ≥20 years were divided into six groups according to their self-reported sleep duration: less than 4.5 h, 4.5–5.4 h, 5.5–6.4 h, 6.5–7.4 h, 7.5–8.4 h, and more than 8.5 h. The associations of sleep duration with obesity and the HbA1c levels were examined in a cross-sectional manner.
RESULTS
The HbA1c levels showed a quadratic association with sleep duration; namely, a shorter or longer sleep duration was associated with a higher level compared with a sleep duration of 6.5–7.4 h (P for quadratic trend <0.001). This association remained significant after adjusting for potential confounders, including the total energy intake and depressive symptoms. Furthermore, additional adjustments for obesity, which also showed a U-shaped relationship with sleep duration, did not attenuate the U-shaped sleep-HbA1c association. A significant interaction between sleep duration and age or the use of insulin was observed for the HbA1c levels.
CONCLUSIONS
Sleep duration was shown to have U-shaped associations with obesity and the HbA1c levels in type 2 diabetic patients, independent of potential confounders, and therefore may be an important modifiable factor for the clinical management of patients with type 2 diabetes.
An increasing prevalence of type 2 diabetes and its complications, including macro- and microvascular diseases, is a growing public health concern in both developing and developed countries (1). This is probably because of population growth, aging, and the increasing prevalence of obesity, which results from environmental factors such as urbanization, physical inactivity, and the increased consumption of food. More recently, it has been reported that the habitual sleep duration has decreased (2) as a result of the modern lifestyle and 24-h society, and epidemiological evidence has suggested that this is associated with adverse consequences such as obesity or weight gain (3,4), hypertension (5), cardiovascular diseases (6,7), and increased mortality (6). The negative impacts of prolonged sleep duration on these outcomes have also been described (3–7), thus suggesting that there is a U-shaped relationship between sleep duration and health disorders. A possible association between an inadequate sleep duration and the development of type 2 diabetes among nondiabetic subjects has been described as well (8–14), but epidemiological evidence concerning the relationship between sleep duration and glycemic control or obesity among diabetic patients is scarce (15–17). Furthermore, to the best of our knowledge, no study has so far examined this relationship among diabetic patients in Asia, despite the fact that racial differences have been suggested in the association between sleep and diabetes (12,18). In this context, the objective of the current study was to investigate the association of sleep duration with the HbA1c levels, as well as with obesity, which is the major factor related to poor glycemic control, among Japanese type 2 diabetic patients.
RESEARCH DESIGN AND METHODS
Study subjects
The Fukuoka Diabetes Registry is a multicenter prospective study designed to investigate the influence of modern treatments on the prognoses of diabetic patients regularly attending teaching hospitals certified by the Japan Diabetes Society or certified diabetes clinics in Fukuoka Prefecture, Japan (UMIN Clinical Trial Registry 000002627). A total of 5,131 diabetic patients aged 20 years or older were registered between April 2008 and October 2010. The exclusion criteria were 1) patients with drug-induced diabetes or undergoing steroid treatment; 2) patients under renal replacement therapy; 3) patients with serious diseases other than diabetes, such as advanced malignancies, decompensated liver cirrhosis, etc.; and 4) patients unable to visit diabetologists regularly. After excluding 261 subjects with type 1 diabetes, the remaining 4,870 subjects (2,775 males, 2,095 females) were enrolled in this cross-sectional study. This study was conducted with the approval of the Kyushu University Institutional Review Board, and written informed consent was obtained from all of the participants.
Clinical evaluation and laboratory measurements
Participants completed a self-administered questionnaire covering their sleep duration, duration of diabetes, alcohol intake, smoking habits, physical activity level, diet, and depressive symptoms. Sleep duration was self-reported and assessed by an answer to the question, “How long is your habitual sleep duration, including naps?” The subjects were divided into six groups according to their sleep duration: less than 4.5 h, 4.5–5.4 h, 5.5–6.4 h, 6.5–7.4 h, 7.5–8.4 h, and more than 8.5 h. Alcohol intake and smoking habits were classified as either current use or not. Subjects engaging in sports regularly during their leisure time were defined as the regular exercise group. The dietary survey was conducted using a brief-type self-administered diet history questionnaire regarding the food frequency of 58 items (BDHQ; Gender Medical Research Inc., Tokyo, Japan). The validity of ranking the energy-adjusted intakes of many nutrients has been studied previously in an adult Japanese population (19). The presence of depressive symptoms was assessed by using the Center for Epidemiologic Studies Depression Scale (CES-D) (20), and subjects who scored more than 16 out of 60 points were defined as having depressive symptoms. The subjects were categorized as either taking insulin therapy or not. BMI was calculated from the height and weight, and obesity was defined as a BMI ≥25 kg/m2. Blood was collected by venipuncture. HbA1c was determined by high-performance liquid chromatography (Tosoh Corporation, Tokyo, Japan).
Statistical analysis
The differences in the mean values or proportions of the characteristics of the studied subjects were tested by an ANOVA or χ2 test, as appropriate. The age- and sex-adjusted or multivariate-adjusted odds ratios (ORs) and their 95% CIs for obesity were calculated using a logistic regression model. The HbA1c values were log-transformed for the statistical analyses because of their skewed distribution. The age- and sex-adjusted or multivariate-adjusted mean values for log-transformed HbA1c were calculated by an ANCOVA, back-transformed, and reported as adjusted geometric means and their 95% CIs. The age- and sex-adjusted partial regression coefficients and their 95% CIs for log-transformed HbA1c were determined using a multiple regression analysis. The quadratic trends of each value across sleep duration categories were tested using a quadratic regression analysis. The effect of the interaction between sleep duration and other confounding factors on the HbA1c levels was examined by adding an interaction term to the statistical model. All analyses were performed using the SAS software package version 9.2 (SAS Institute Inc., Cary, NC). Values of P < 0.05 were considered to be statistically significant in all analyses.
RESULTS
Table 1 shows the characteristics of the studied subjects. The mean age, the proportion of male patients, duration of diabetes, and total energy intake increased as sleep duration became longer. Current smokers and current drinkers showed no statistically significant differences between sleep-duration categories. Short sleepers tended to exercise less and have depressive symptoms, whereas long sleepers were likely to be insulin users. The BMI and the proportions of obese subjects decreased in association with increases in sleep duration.
Table 1.
The clinical characteristics of the studied subjects according to sleep duration
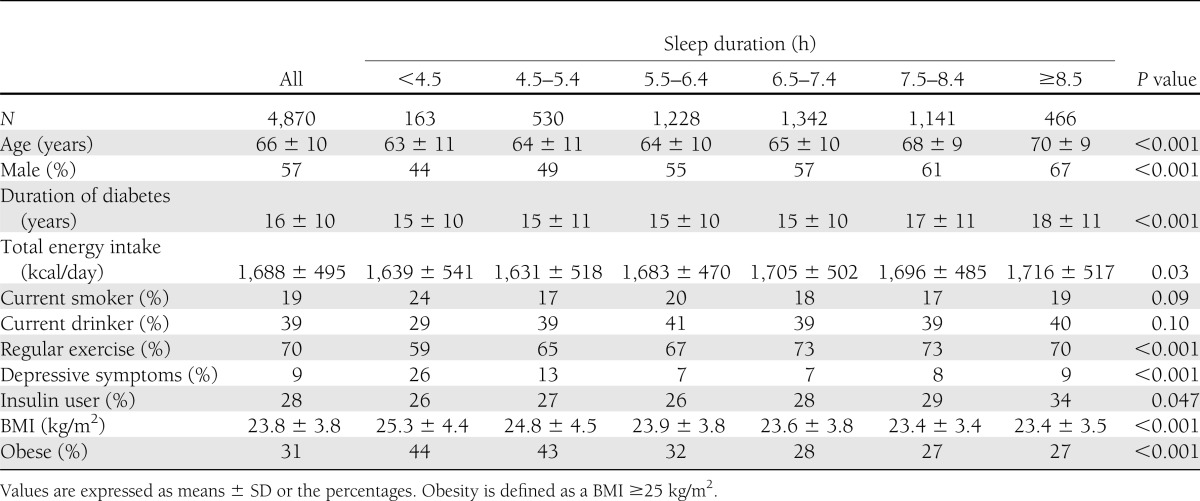
As shown in Table 2, the age- and sex-adjusted ORs for obesity tended to increase in subjects with a shorter or longer sleep duration, compared with those with a sleep duration of 6.5–7.4 h. The U-shaped relationship between sleep duration and obesity was substantially unchanged, even after controlling for age, sex, duration of diabetes, total energy intake, current smoking, current drinking, regular exercise, use of insulin, and depressive symptoms.
Table 2.
Adjusted ORs (95% CIs) for obesity and the adjusted geometric means (95% CIs) of HbA1c according to sleep duration
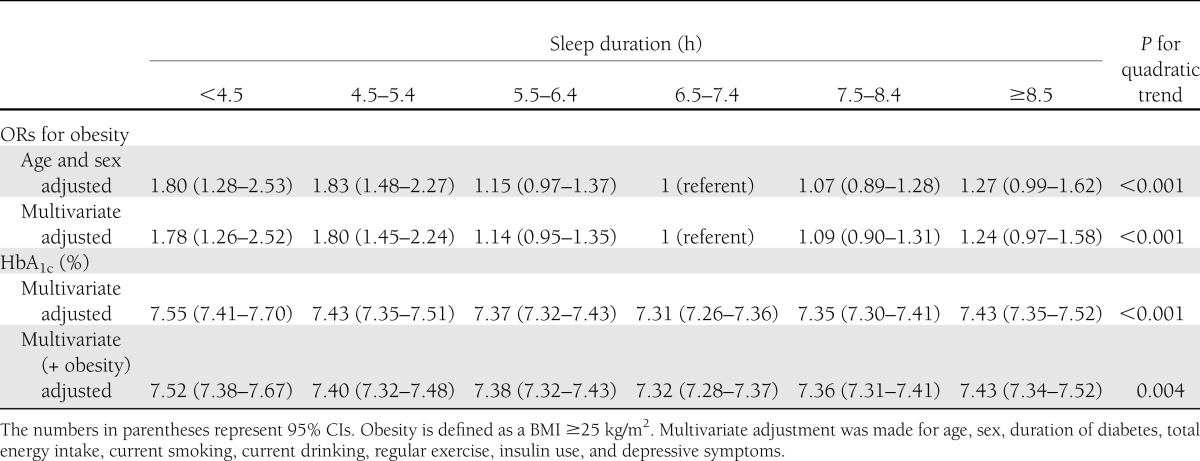
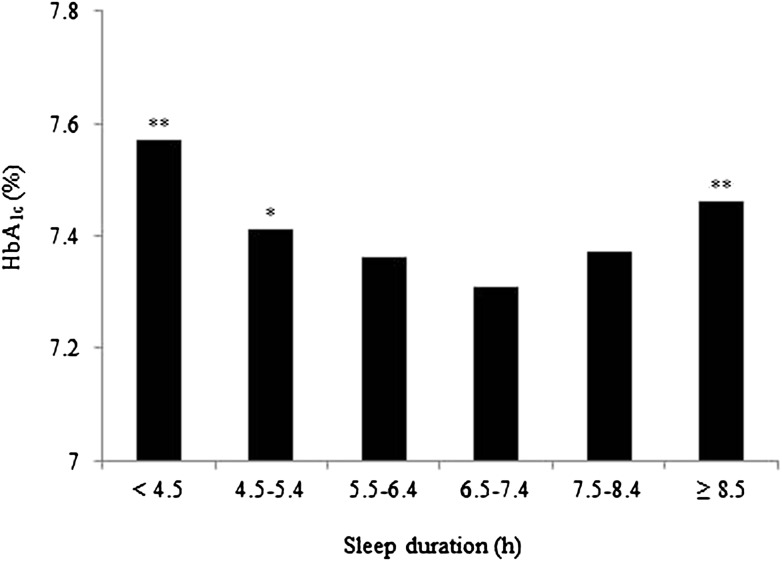
Figure 1 depicts the age- and sex-adjusted geometric mean values of HbA1c according to sleep duration, with mean levels of 7.57% (95% CI 7.42–7.73) for subjects sleeping less than 4.5 h, 7.41% (7.33–7.50) for 4.5–5.4 h, 7.36% (7.30–7.41) for 5.5–6.4 h, 7.31% (7.26–7.36) for 6.5–7.4 h, 7.37% (7.31–7.43) for 7.5–8.4 h, and 7.46% (7.37–7.56) for those sleeping more than 8.5 h. Both subjects with a short and long sleep duration had higher HbA1c levels compared with subjects sleeping for 6.5–7.4 h (P for the quadratic trend <0.001), thus indicating an association occurring in a U-shaped fashion. This relationship remained significant after adjusting for the above-mentioned confounders (Table 2). Furthermore, additional adjustment for obesity did not attenuate sleep-HbA1c association.
Figure 1.
The age- and sex-adjusted geometric mean values of HbA1c according to sleep duration in Japanese type 2 diabetic patients. *P < 0.05; **P < 0.01 vs. sleep duration of 6.5–7.4 h per day.
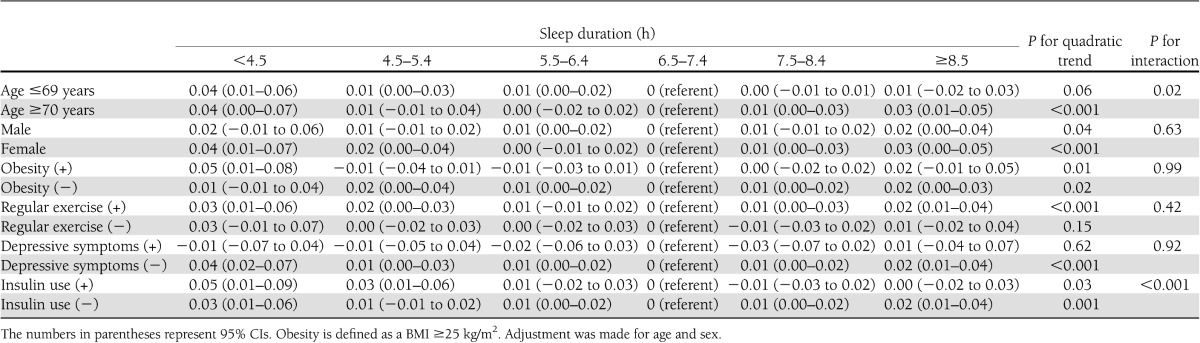
In addition, the interaction analyses between sleep duration and possible confounding factors on the HbA1c levels were conducted (Table 3). A significant interaction was observed between patients being stratified into a younger group (<70 years) and an older group (≥70 years) (P for interaction = 0.02). On the other hand, there was no significant interaction between sleep duration and sex, the presence or absence of obesity, regular exercise, and depressive symptoms. However, a significant interaction was also observed between subjects based on their use of insulin therapy (P for interaction <0.001).
Table 3.
The age- and sex-adjusted partial regression coefficients (95% CIs) of log-transformed HbA1c according to sleep duration by the presence or absence of confounding factors
Finally, we tested the quadratic trends for all of the associations in the current study by modeling sleep duration as a continuous variable instead of as a category and found similar results (P for the quadratic trend <0.001 for all the analyses in Table 2).
CONCLUSIONS
The present analysis demonstrated that both a short and long sleep duration relative to the intermediate sleep duration were significantly associated with higher HbA1c levels in Japanese type 2 diabetic patients. This association remained significant even after adjusting for confounding factors, including the total energy intake, regular exercise, depressive symptoms, and obesity. To the best of our knowledge, this is the first large-scale epidemiological study to indicate that there is a U-shaped curvilinear relationship between sleep duration and glycemic level in type 2 diabetic patients.
There have been an increasing number of epidemiological studies that have examined the link between sleep duration and the development of type 2 diabetes. Several large-scale studies have reported an association between a short sleep duration and a higher risk for diabetes (8–14). With regard to a long sleep duration, habitual long sleep was also found to increase the risk for type 2 diabetes (8,10–13). Recently, a meta-analysis of the various prospective studies revealed an increased risk of the development of type 2 diabetes both in subjects with a short sleep duration (≤5 to 6 h per night, relative risk 1.28, 95% CI 1.03–1.60) and in those with a long sleep duration (>8 to 9 h per night, relative risk 1.48, 95% CI 1.13–1.96) (21). Especially in Japanese persons without a family history of diabetes, those with a sleep duration of ≤5 h were more likely to develop diabetes, and this increased risk was more than 5 times that of patients with a sleep duration of 7 h in an occupational-based 4-year prospective study (14). Taken together, these findings indicate that both a short and long sleep duration increase the risk of type 2 diabetes, thus suggesting that there is a U-shaped relationship between sleep duration and incidence of type 2 diabetes. On the other hand, few epidemiological studies have reported an association between sleep duration and glycemic control among diabetic patients. A cross-sectional study among 161 African American type 2 diabetic patients revealed that higher natural log of HbA1c levels were correlated with a shorter weekly sleep duration (r = −0.17, P = 0.03) (15), whereas sleep duration measured by wrist actigraphy showed no clear association with glycemic control in type 2 diabetic patients, although those studies included fewer than 50 subjects (16,17). The differences in sleep duration-glycemic level association among diabetic patients in these studies might be partly explained by the methods used to measure sleep duration, as well as the small sample sizes. The current study demonstrated that a self-reported short or long sleep duration was significantly associated with higher HbA1c levels, even after adjustment for confounding factors. In addition, our findings also revealed a U-shaped relationship between sleep duration and obesity, which has been shown in healthy subjects (3,4), but this relationship has never been reported previously in diabetic patients.
There are several potential mechanisms through which the relationship between sleep loss and higher glycemic level may be mediated. Sleep curtailment decreases the satiety hormone leptin and increases the appetite-stimulating hormone ghrelin (4,22), which may lead to an increase in appetite (22), hunger (22,23), and energy intake (23), and consequently lead to obesity and an elevated glycemic level. Because short sleep duration is strongly related to obesity, obesity is generally considered to confound the association between sleep deprivation and an elevated glycemic level. In the current study, however, the HbA1c levels significantly increased in both short and long sleepers in comparison with moderate sleepers, even after adjusting for total energy intake and obesity. These findings raise the possibility that mechanisms other than those related to these factors may underlie the association between sleep curtailment and dysregulated glucose metabolism. The other possible reasons may include changes in counter-regulatory hormones and proinflammatory cytokines. Sleep restriction was previously reported to be significantly associated with increases in cortisol (24), interleukin 6, and tumor necrosis factor-α (25). These changes may contribute to insulin resistance. The sympathetic nervous system is activated by sleep deprivation (24), and it may also play a role in the relationship between reduced sleep and glucose intolerance via impaired insulin secretion and insulin resistance. In addition to these pathways, a decrease in brain glucose utilization after sleep deprivation might lead to an increase in the glycemic level (26).
On the other hand, the mechanisms underlying the association between a long duration of sleep and a higher glycemic level are unclear. Depression and physical inactivity were associated with long sleep in the Nurses’ Health Study II (27), as well as in the current study (Table 1), and may have confounded the association. In the current study, however, significant increases in the HbA1c levels in subjects with long sleep duration were demonstrated even after controlling for depression and regular exercise, which indicates the presence of other contributing mechanisms. Sleep-disordered breathing (SDB), characterized by repetitive episodes of upper airway obstructions or partial collapses that occur during sleep, may also have confounded the association. Snoring, a characteristic symptom of SDB, has also been shown to be associated with a self-reported long sleep duration (more than 9 h) compared with a normal sleep duration (7 to 8 h) (27). SDB may lead to insulin resistance and glucose intolerance through the activation of the sympathetic nervous system, hypothalamic-pituitary axis, and inflammatory pathways as a consequence of chronic intermittent hypoxia and sleep fragmentation (28). The prevalence of SDB was shown to be high (ranging from 58% to 86%) (28) even among relatively lean Japanese type 2 diabetic patients (45%) (29), and the severity of SDB was associated with poor glycemic control (28). Restless legs syndrome (RLS), a condition characterized by unpleasant leg sensations that usually occur mostly during sleep and make individuals want to constantly move their legs, has also been associated with a self-reported long duration of sleep compared with normal sleep duration (27). This syndrome may have also contributed to the impaired glucose metabolism via the activation of the hypothalamic-pituitary-adrenal axis and sympathetic nervous system (30). RLS was also associated with poor sleep quality (31) and was highly prevalent in type 2 diabetic patients (17.7%) compared with nondiabetic control subjects (5.5%) (32). Patients with RLS had a significantly higher glycemic level than healthy control subjects (30). However, although subjects with SDB or RLS may have a longer self-reported sleep duration, it was reported that the polysomnography-measured sleep duration was shorter in subjects with SDB than in those without SDB, and the actigraphy-measured sleep duration was not different between those with and without SDB (33). This suggests that the subjects with SDB or RLS might spend more time in bed, but not sleep. Therefore, it is probable that these disorders may confound the association not just in subjects with longer sleep duration but also in those with short or intermediate sleep duration, depending on the methods used to measure the duration of sleep. It is also possible that a decline in cerebral and systemic glucose use (34) and counter-regulatory hormone release during sleep (35) may explain the association between the elevation of the HbA1c levels and extended sleep. Another possibility is the confounding effect of other unmeasured factors or diseases, which lead to extended sleep duration. Further research into potential mechanisms mediating the effect of long sleep duration on the elevated glycemic level is needed.
The current study indicated no interactions between the various confounding factors and sleep duration on the HbA1c levels, with the exceptions of age and the use of insulin. The association of long sleep duration with the HbA1c levels seemed to be attenuated in subjects aged less than 70 years and in those with insulin therapy. The mechanisms responsible for this attenuation remain to be elucidated, because the association between long sleep duration and higher glycemic level was not fully explained by the current study, as mentioned above. However, an age-related decline in insulin sensitivity and insulin secretion (36) may affect the association between sleep duration and glycemic level in older patients. In addition, insulin therapy may somehow weaken the influence of longer sleep on the glycemic control in type 2 diabetic patients.
The strengths of the current study include the inclusion of a sufficient number of type 2 diabetic patients with a wide range of ages. Furthermore, we took into consideration various potential confounding factors, such as the total energy intake and presence of depressive symptoms. Although these factors were closely associated with both sleep duration and metabolic risk factors, few prior epidemiological studies have used them as confounders. It is probable that adjustment for the total energy intake may be over-adjusting, because it may be part of the causal pathway between sleep duration and poor glycemic control. However, adjustment for this factor would likely bias our results toward the null hypothesis of no association. In addition, we also demonstrated significant associations of sleep duration and HbA1c levels in the analyses stratified by potential risk factors. Therefore, the present results may have higher accuracy with regard to the relationship between sleep duration and HbA1c levels, and may be more easily generalized in clinical settings, at least in Japanese people.
Nevertheless, some limitations should be discussed. First, we evaluated sleep duration by a self-reported questionnaire, as has been done in many prior epidemiological studies, so sleep was not measured objectively. However, several studies that compared the self-reported sleep duration with sleep duration assessed by polysomnography or actigraphy have been reported (37–39). A study among 36 insomniacs reported that a significant difference was not observed between the self-reported sleep duration and sleep duration assessed by polysomnography or actigraphy (37). Another study showed a moderate correlation (r = 0.57) between the self-reported and actigraphy-evaluated sleep duration in 49 blind subjects (38). A recent analysis from the Coronary Artery Risk Development in Young Adults (CARDIA) Sleep Study comparing the self-reported sleep duration with sleep duration measured by actigraphy in over 600 healthy adults also indicated a moderate correlation (r = 0.45) (39). Second, we did not study the quality of sleep. A previous study showed that the majority of type 2 diabetic patients had poor sleep quality (40), and a relationship between poor sleep quality and higher glycemic levels in diabetic patients has been reported (15–17). Furthermore, we could not assess the presence of sleep disorders such as SDB or RLS. Given the high prevalence of these disorders among diabetic patients and their relationship with metabolic disorders, the lack of measurements may be a major limitation. Third, we cannot prove the existence of a cause-and-effect relationship because of the cross-sectional design of our study. Finally, there may be other confounding factors besides those used in the current study.
In conclusion, the current study is the first epidemiological study to demonstrate the U-shaped associations of sleep duration with obesity and glycemic level in patients with type 2 diabetes. Our findings suggest that patients with either a short or long sleep duration should be considered high-risk patients for poor glycemic control, and this may have important implications for the clinical management of diabetes.
Acknowledgments
This work was supported in part by JSPS KAKENHI grant numbers 23249037 and 23659353 for M.I.
No potential conflicts of interest relevant to this article were reported.
T.O., H.F., and M.I. were responsible for the study concept and design. T.O. and M.I. drafted the manuscript and conducted the analyses. H.F., Y.K., S.O., Y.I., H.I., Y.D., Y.H., U.N., and T.K. helped with interpreting the data and contributed to the discussion. All authors participated in critically revising the manuscript and approved the final version. M.I. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank Drs. Shigenobu Kanba, Dongchon Kang, Shuzo Kumagai, Hiro Kishimoto (Kyushu University), Nobutaka Tsutsu, Nobuhiro Sasaki, Sakae Nohara, Chie Miyagawa, Yuji Komorida (Fukuoka Red Cross Hospital), Kiyohide Nunoi, Yuichi Sato, Hirofumi Imoto, Masae Toyonaga, Ayumi Yamauchi, Chisa Matsumoto (St. Mary’s Hospital), Kazushi Amano, Kaori Itoh (Steel Memorial Yawata Hospital), Daisuke Gotoh, Toshitaka Himeno, Tamaki Jodai, Chie Sejima (Kyushu Central Hospital), Noriyasu Shinohara, Ayako Tsutsumi, Akiko Sumi (Fukuoka Higashi Medical Center), Masahiro Nakano, Mina Matsuo, Shoko Morimoto, Tomoko Hyodo (Hakujyuji Hospital), Masae Minami (Clinic Minami Masae), Miya Wada (Wada Miya Naika Clinic), Yoshifumi Yokomizo (Yokomizo Naika Clinic), Masanori Kikuchi (Kikuchi Naika Clinic), Riku Nomiyama (Suzuki Naika Clinic), Shin Nakamura (Nakamura Naika Clinic), Kenji Tashiro (Oshima Eye Hospital), Mototaka Yoshinari (Yoshinari Naika Clinic), Kojiro Ichikawa (Fukutsu Naika Clinic), and Teruo Omae (Hisayama Research Institute For Lifestyle Diseases); clinical research coordinators Chiho Ohba, Yumi Ono (Hisayama Research Institute For Lifestyle Diseases), and Kayoko Sekioka (Kyushu University); and administrative staff members Tomoko Matake (Hisayama Research Institute For Lifestyle Diseases) and Junko Ishimatsu (Kyushu University).
References
- 1.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:4–14 [DOI] [PubMed] [Google Scholar]
- 2.Kronholm E, Partonen T, Laatikainen T, et al. Trends in self-reported sleep duration and insomnia-related symptoms in Finland from 1972 to 2005: a comparative review and re-analysis of Finnish population samples. J Sleep Res 2008;17:54–62 [DOI] [PubMed] [Google Scholar]
- 3.Chaput JP, Després JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep 2008;31:517–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 2004;1:e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep 2006;29:1009–1014 [DOI] [PubMed] [Google Scholar]
- 6.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep 2007;30:1659–1666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med 2003;163:205–209 [DOI] [PubMed] [Google Scholar]
- 8.Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care 2003;26:380–384 [DOI] [PubMed] [Google Scholar]
- 9.Mallon L, Broman JE, Hetta J. High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care 2005;28:2762–2767 [DOI] [PubMed] [Google Scholar]
- 10.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care 2006;29:657–661 [DOI] [PubMed] [Google Scholar]
- 11.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large U.S. sample. Sleep 2007;30:1667–1673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beihl DA, Liese AD, Haffner SM. Sleep duration as a risk factor for incident type 2 diabetes in a multiethnic cohort. Ann Epidemiol 2009;19:351–357 [DOI] [PubMed] [Google Scholar]
- 13.Tuomilehto H, Peltonen M, Partinen M, et al. Finnish Diabetes Prevention Study Group Sleep duration, lifestyle intervention, and incidence of type 2 diabetes in impaired glucose tolerance: The Finnish Diabetes Prevention Study. Diabetes Care 2009;32:1965–1971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kita T, Yoshioka E, Satoh H, et al. Short sleep duration and poor sleep quality increase the risk of diabetes in Japanese workers with no family history of diabetes. Diabetes Care 2012;35:313–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knutson KL, Ryden AM, Mander BA, Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med 2006;166:1768–1774 [DOI] [PubMed] [Google Scholar]
- 16.Trento M, Broglio F, Riganti F, et al. Sleep abnormalities in type 2 diabetes may be associated with glycemic control. Acta Diabetol 2008;45:225–229 [DOI] [PubMed] [Google Scholar]
- 17.Knutson KL, Van Cauter E, Zee P, Liu K, Lauderdale DS. Cross-sectional associations between measures of sleep and markers of glucose metabolism among subjects with and without diabetes: the Coronary Artery Risk Development in Young Adults (CARDIA) Sleep Study. Diabetes Care 2011;34:1171–1176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vishnu A, Shankar A, Kalidindi S. Examination of the association between insufficient sleep and cardiovascular disease and diabetes by race/ethnicity. Int J Endocrinol 2011;2011:789358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kobayashi S, Honda S, Murakami K, et al. Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J Epidemiol 2012;22:151–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401 [Google Scholar]
- 21.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 2010;33:414–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 2004;141:846–850 [DOI] [PubMed] [Google Scholar]
- 23.Brondel L, Romer MA, Nougues PM, Touyarou P, Davenne D. Acute partial sleep deprivation increases food intake in healthy men. Am J Clin Nutr 2010;91:1550–1559 [DOI] [PubMed] [Google Scholar]
- 24.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet 1999;354:1435–1439 [DOI] [PubMed] [Google Scholar]
- 25.Vgontzas AN, Zoumakis E, Bixler EO, et al. Adverse effects of modest sleep restriction on sleepiness, performance, and inflammatory cytokines. J Clin Endocrinol Metab 2004;89:2119–2126 [DOI] [PubMed] [Google Scholar]
- 26.Thomas M, Sing H, Belenky G, et al. Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity. J Sleep Res 2000;9:335–352 [DOI] [PubMed] [Google Scholar]
- 27.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep 2006;29:881–889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pamidi S, Aronsohn RS, Tasali E. Obstructive sleep apnea: role in the risk and severity of diabetes. Best Pract Res Clin Endocrinol Metab 2010;24:703–715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Furukawa S, Miyake T, Yamamoto S, et al. Sleep-disordered breathing as a modifiable risk factor for microvascular complications in Japanese type 2 diabetes mellitus (Abstract). Diabetes 2012;61(Suppl. 1):A139–A140 [Google Scholar]
- 30.Innes KE, Selfe TK, Agarwal P. Restless legs syndrome and conditions associated with metabolic dysregulation, sympathoadrenal dysfunction, and cardiovascular disease risk: A systematic review. Sleep Med Rev 2012;16:309–339 [DOI] [PubMed] [Google Scholar]
- 31.Cuellar NG, Ratcliffe SJ. A comparison of glycemic control, sleep, fatigue, and depression in type 2 diabetes with and without restless legs syndrome. J Clin Sleep Med 2008;4:50–56 [PMC free article] [PubMed] [Google Scholar]
- 32.Merlino G, Fratticci L, Valente M, et al. Association of restless legs syndrome in type 2 diabetes: a case-control study. Sleep 2007;30:866–871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aronsohn RS, Whitmore H, Van Cauter E, Tasali E. Impact of untreated obstructive sleep apnea on glucose control in type 2 diabetes. Am J Respir Crit Care Med 2010;181:507–513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boyle PJ, Scott JC, Krentz AJ, Nagy RJ, Comstock E, Hoffman C. Diminished brain glucose metabolism is a significant determinant for falling rates of systemic glucose utilization during sleep in normal humans. J Clin Invest 1994;93:529–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Takahashi Y, Kipnis DM, Daughaday WH. Growth hormone secretion during sleep. J Clin Invest 1968;47:2079–2090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DeFronzo RA. Glucose intolerance and aging. Diabetes Care 1981;4:493–501 [DOI] [PubMed] [Google Scholar]
- 37.Hauri PJ, Wisbey J. Wrist actigraphy in insomnia. Sleep 1992;15:293–301 [DOI] [PubMed] [Google Scholar]
- 38.Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res 1999;8:175–183 [DOI] [PubMed] [Google Scholar]
- 39.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology 2008;19:838–845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cunha MC, Zanetti ML, Hass VJ. Sleep quality in type 2 diabetics. Rev Lat Am Enfermagem 2008;16:850–855 [DOI] [PubMed] [Google Scholar]