Abstract
OBJECTIVE
To evaluate whether assessment of barriers to self-care and strategies to cope with these barriers in older adults with diabetes is superior to usual care with attention control. The American Diabetes Association guidelines recommend the assessment of age-specific barriers. However, the effect of such strategy on outcomes is unknown.
RESEARCH DESIGN AND METHODS
We randomized 100 subjects aged ≥69 years with poorly controlled diabetes (A1C >8%) in two groups. A geriatric diabetes team assessed barriers and developed strategies to help patients cope with barriers for an intervention group. The control group received equal amounts of attention time. The active intervention was performed for the first 6 months, followed by a “no-contact” period. Outcome measures included A1C, Tinetti test, 6-min walk test (6MWT), self-care frequency, and diabetes-related distress.
RESULTS
We assessed 100 patients (age 75 ± 5 years, duration 21 ± 13 years, 68% type 2 diabetes, 89% on insulin) over 12 months. After the active period, A1C decreased by −0.45% in the intervention group vs. −0.31% in the control group. At 12 months, A1C decreased further in the intervention group by −0.21% vs. 0% in control group (linear mixed-model, P < 0.03). The intervention group showed additional benefits in scores on measures of self-care (Self-Care Inventory-R), gait and balance (Tinetti), and endurance (6MWT) compared with the control group. Diabetes-related distress improved in both groups.
CONCLUSIONS
Only attention between clinic visits lowers diabetes-related distress in older adults. However, communication with an educator cognizant of patients’ barriers improves glycemic control and self-care frequency, maintains functionality, and lowers distress in this population.
Diabetes is a major public health problem affecting an increasing number of older individuals (1). Treating older adults with diabetes is complicated by the presence of coexisting chronic conditions, including cognitive dysfunction, depression (2), physical disabilities (3), and polypharmacy (4). Although these conditions, collectively referred to as geriatric syndrome, are not specifically associated with diabetes, they may act as barriers by interfering with patients’ abilities to perform self-care tasks such as glucose monitoring, understanding the role of diet and exercise on glucose excursions, and following complex insulin regimens (5,6). Some comorbidities have subtle presentations and may remain unidentified by medical providers (7). Unaddressed barriers in older adults may lead to nonadherence with diabetes self-care recommendations, treatment complications such as hypoglycemia, and an overall decline in health and quality-of-life. The American Geriatrics Society (4) and the American Diabetes Association (8) recommend assessment for age-specific barriers in older adults to improve diabetes management. However, practical tools, methods of implementing this strategy, and the impacts of these recommendations on outcomes are unknown.
Older adults with diabetes frequently encounter fluctuations in their glucose levels when clinical (e.g., acute infections or exacerbation of heart disease or other chronic diseases), functional (e.g., falls or deconditioning), or social (e.g., illness or death in the family, caregiver stress of aging spouse) circumstances change. Strategies to adjust insulin regimens for fluctuations in blood glucose or dose-adjustment for sick-days commonly used in younger adults are difficult to follow for older patients with multiple medical comorbidities, especially during times of stress. Consequently, when older adults are seen by their medical providers at an interval of 3 to 6 months, small changes made during clinic visits are frequently inadequate to improve overall glycemia.
Phone consultations and telemedicine are a frequently tested approach to improve outcomes in the management of chronic diseases, such as congestive heart failure, particularly when ongoing adjustments in doses of medications, such as diuretics, are required (9). In recent years, successful management of diabetes via telemedicine in older patients living in medically underserved areas has been shown to be successful (10). However, telephone follow-up between clinic visits is typically not used for glycemic management as part of chronic disease management in patients with diabetes. Community-living older adults with poorly controlled diabetes are a vulnerable population with a high risk of acute illnesses and hospitalizations. For these patients, phone calls by diabetes educators to adjust insulin doses or provide coping strategies to maintain self-care may be an effective and inexpensive method for decreasing wide glucose excursions from hyperglycemia and hypoglycemia.
In this study, we hypothesized that providing coping strategies for age-related barriers to self-care by phone contact between clinic visits would be superior to attention alone in improving glycemic control in older adults with poorly controlled diabetes.
RESEARCH DESIGN AND METHODS
The institutional review boards of the Joslin Diabetes Center, the Beth Israel Deaconess Medical Center, and the Human Research Protection Office of the U.S. Department of Defense approved this study.
Participants
Participants were recruited from the Joslin Diabetes Center and the Beth Israel Deaconess Medical Center. Patients aged ≥69 years with type 1 or type 2 diabetes of at least 1-year duration, with poorly controlled diabetes (A1C >8%), were eligible. Exclusion criteria included terminal diseases, living >25 miles from Boston, living in an institutional setting (e.g., nursing home, group home), and inability to complete outcome assessments (e.g., poor vision, severe cognitive decline, unable to speak, read, or write English). Study participants continued to receive their medical care, including diabetes management, from their endocrinologists and/or primary care physicians throughout the study. All patients provided informed written consent.
Study design
Participants were followed up for 1 year. First, all patients were randomized to an intervention or attention control group. Then, the intervention group was further divided randomly to two groups, described below. Randomization was computer-generated and remained independent of participant enrollment. The adequacy of randomization was checked periodically, and patients were stratified once due to unequal number of patients with different durations of diabetes. During the first 6 months of the study, all patients received active intervention or attention as determined by their random assignment. From 6 to 12 months, all patients entered an “independence period” during which there was no contact between the study personnel and patients from either group. The independence period assessed the sustainability of the interventions’ impact.
Group 1: Intervention group
The patients in this group underwent evaluation for barriers to self-care by a diabetes educator well versed with age-specific barriers. A geriatric diabetes team (GDT), consisting of a geriatric diabetologist, a diabetes educator, and a nutritionist, identified strategies to help patients cope with their barriers after consideration of patients’ clinical and psychosocial environments and comorbid conditions. The strategies were designed to optimize patients’ ability to perform self-care leading to better adherence with treatment recommendations given by their medical providers. Importantly, the study staff did not make changes to patients’ diabetes treatment plans. This was important to protect the integrity of the study, particularly the ability to interpret the effect of management of barriers versus change in treatment regimen.
The strategies to cope with barriers were provided to the patients in intervention group via two methods by further randomizing patients into two groups. In one group, an office-based diabetes educator provided the strategy by phone calls, speaking with patients up to 11 times during the intervention period. The initial phone call included educating patients regarding their barriers and providing strategy options to cope with these barriers. Follow-up phone calls included continued assessment and encouragement to cope with barriers, as described in Table 1. In the second group, a non–health professional care manager, trained and briefed by the GDT, provided coping recommendations. The recommendations were conveyed to the patients in this group by the care manager. The care manager visited the patients’ homes to assess safety issues or other needs not known to the study team and helped the patients and caregivers with all aspects of care coordination, including making medical appointments and arranging transportation. Patients in this group received phone contact from the care manager as often as needed during the intervention period.
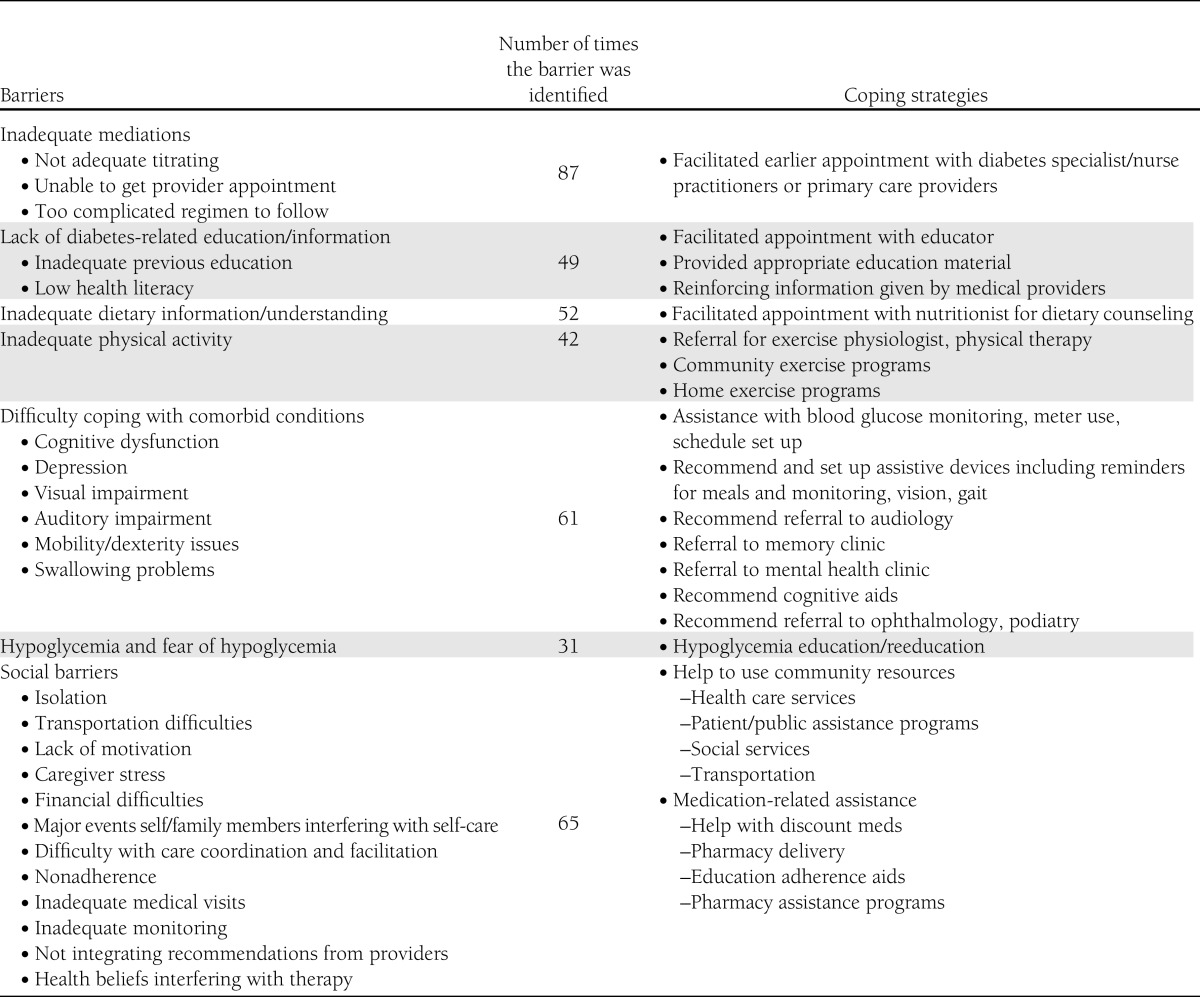
Table 1.
Commonly found barriers and strategies recommended to overcome the barriers
Group 2: Attention control group
An educator (different from the one involved with the intervention), called participants in this group for total of 11 times within the first 6 months to provide similar attention time. The phone calls differed from the intervention calls in that the educator did not provide any diabetes-related advice or strategies and only discussed non–diabetes-related life events. Participants who asked specific questions related to diabetes management were advised to contact their medical providers.
Outcomes
All study participants underwent the outcome assessment at baseline and at 6 and 12 months, whereas the primary outcome (A1C) was measured at baseline and at 3, 6, and 12 months.
Clinical measures.
The primary outcome of the study was glycemic control (A1C), before and after interventions. Other clinical outcomes included blood pressure, BMI, lipids, questionnaire for frequency of hypoglycemia and medication compliance, frequency of self-care activity (Self-Care Inventory-R [SCI-R]) (11), dietary assessment (Determine Your Nutritional Health checklist) (12), and cognition (clock-in-a-box test [7,13], Trail-Making Test A and B [14], and verbal fluency test [15]).
Functional measures.
Functional measures included activities of daily living (16) and instrumental activities of daily living (17) number of falls and fear of falls, 6-min walk test (6MWT) (18), and the Tinetti test for gait and balance (19).
Psychosocial measures.
Psychosocial measures included a Geriatric Depression Scale (GDS) (20) and/or a diagnosis of depression, diabetes-related distress (Problem Areas in Diabetes [PAID]) (21), and social resource assessment (Older Americans Resources and Services Multidimensional Functional Assessment Questionnaire) (22).
Economic measures.
Economic measures included the number of emergency department (ED) visits, hospitalizations, and outpatient care utilization (clinic visits).
Statistical methods
We performed an intent-to-treat analysis with the last observation carried forward. We used paired t tests to assess changes within groups from baseline to 6 months and 12 months. We also compared between-group changes in outcomes at baseline, 6 months (end of intervention period), and 12 months (end of study) with mixed-models, using time and group as fixed factors, interaction between time and group, random intercepts, and an unstructured covariance matrix. A two-sided P value <0.05 indicated statistical significance. Results were confirmed using multiple imputations (15) for missing data using PROC MI in SAS (the Markov chain Monte Carlo method).
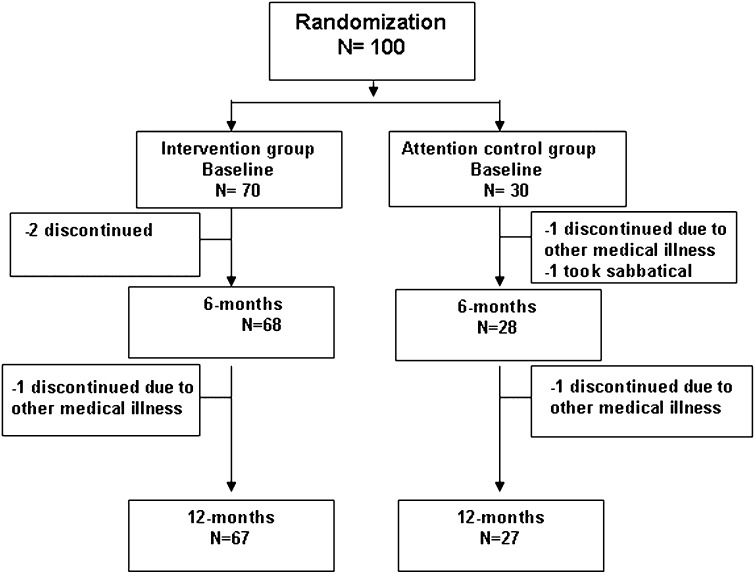
RESULTS
Between August 2007 and May 2010, 103 patients were enrolled and 100 patients were randomized (3 patients dropped out after the screening but before the first study visit). Patients were randomized 2-to-1 in the intervention arm (n = 70 with care manager and n = 35 with office-based educator) versus control (n = 30). The Consolidated Standards of Reporting Trials study flow diagram is shown in Fig. 1.
Figure 1.
Randomization and completion of the 6- and 12-month evaluations.
The two intervention subgroups with different implementation strategies were compared for baseline characteristics and for all outcome measures. These subgroups did not differ in baseline characteristics or outcome variables at 6 or 12 months and were for this analysis.
Table 1 summarizes the types of barriers, the number of times these barriers were present, and the coping strategies recommended by the GDT. The most frequent barrier identified in intervention patients was “inadequate medications” due to lack of dose titration between the clinic visits. In addition, participants needed knowledge of insulin action, medication-adherence, and the effect of diet on blood glucose. Comorbidities interfering with diabetes management were another frequent barrier. Multiple social barriers were also identified.
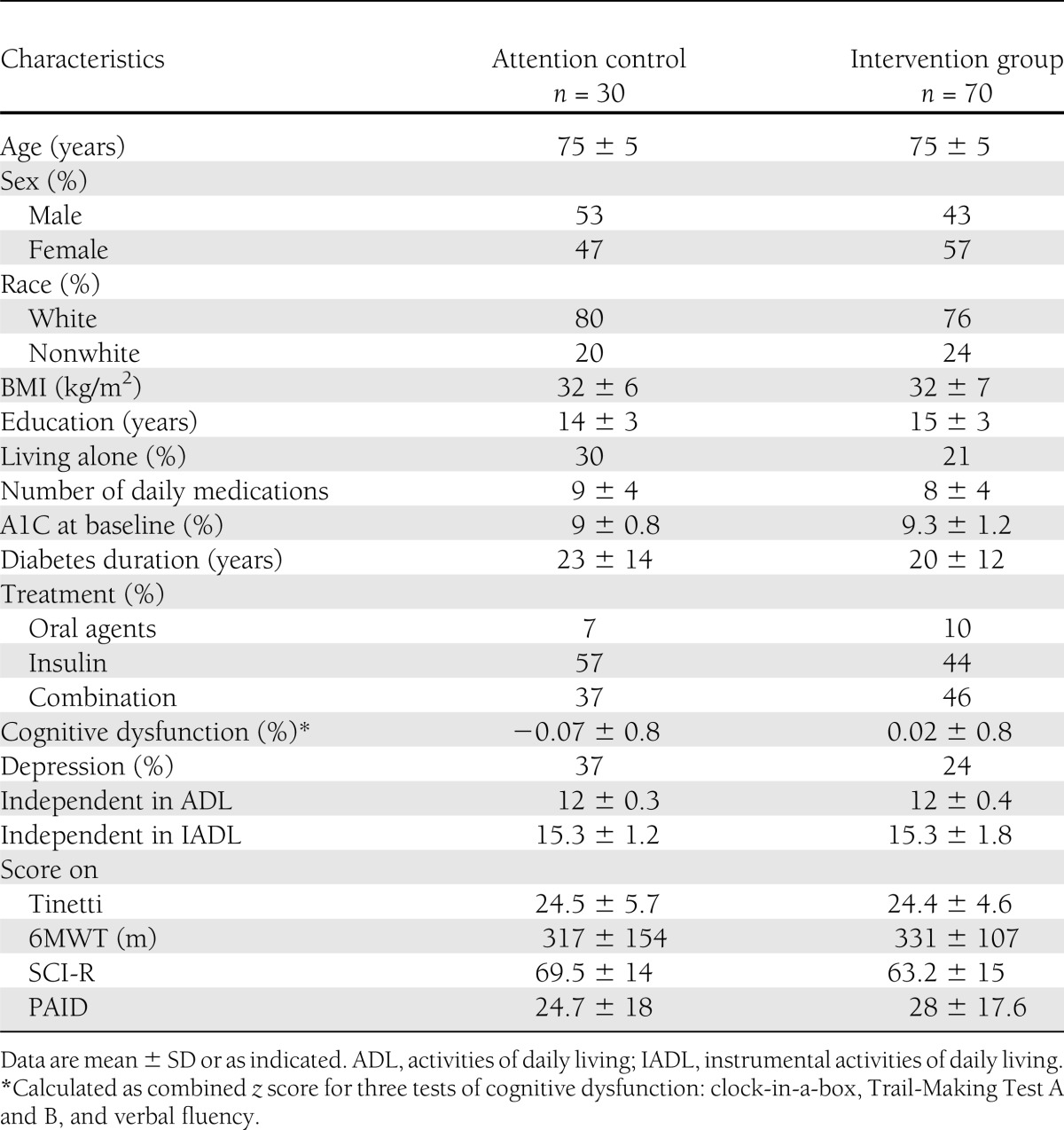
Baseline characteristics
Table 2 reports the baseline characteristics of patients by group. The study population was an average age of 75 ± 5 years, duration of diabetes was 21 ± 13 years, 68% had type 2 diabetes, 54% were women, and 77% were Caucasian. Patients in the two groups did not differ on any baseline variable.
Table 2.
Baseline characteristics of the subjects
Intervention period
Changes in variables between the intervention and control groups from baseline to 6 months (during the intervention period) are as follows: Mean A1C was decreased by −0.45% (95% CI −0.7 to −0.2, P < 0.007) in the intervention group compared with −0.31% (−0.7 to −0.1, P = NS) in the control group. The mean SCI-R increased by 6.4 (4.2–8.5, P < 0.0001) in the intervention group but did not change the control group (1.2 [−1.7 to 4.1], P = NS). The Tinetti test and 6MWT scores worsened in the control group (−1.6 [−2.9 to −0.3], P = 0.02; and −42 [−86 to 2.6], P = 0.06, respectively) but remained unchanged in the intervention group (0.8 [−0.1 to 1.7], P = NS; and 4 [−10.7 to 19.2], P = NS, respectively). PAID scores decreased in the intervention (−7.9 [−11.4 to 4.4], P < 0.0001) and control groups (−5.2 [−9.5 to −0.9], P = 0.02).
Follow-up period
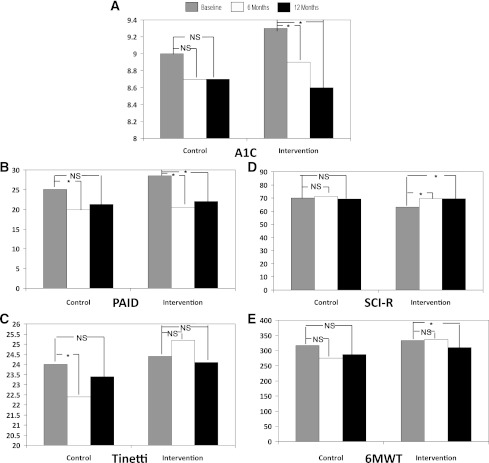
The change in variables between the intervention and control groups between 6 and 12 months are as follows (Fig. 2): The mean (95% CI) A1C decreased further in the intervention group by −0.21% (−0.4 to −0.04, P = 0.02) whereas no change (0%) occurred in the control group (−0.3 to 0.3, P = NS). In the control group, scores did not change on the SCI-R (−1.4 [−5.3 to 2.5], P = NS), PAID (1.3 [−2.9 to 5.6], P = NS), Tinetti (1.0 [−0.1 to 2.1], P = NS), or 6MWT (18 [−3 to 38], P = NS). The scores in the intervention group did not change on SCI-R (−0.2 [−1.7 to 1.4], P = NS) or PAID (1.5 [−1.4 to 4.4], P = NS). However, the scores on Tinetti and 6MWT declined in the intervention group (−1.1 [−2 to 0.3], P = 0.007; and −27 [−46 to −8], P = 0.006, respectively) from the 6- to 12-month period. Figure 1 shows changes in variables during the intervention and the follow-up periods.
Figure 2.
Changes in variables from baseline to 6 and 12 months for A1C (A), PAID score (B), Tinetti scores (C), SCI-R (D), and 6MWT (E). *P ≤ 0.05.
The linear mixed-models analysis examining each outcome over time found that the intervention group showed better outcomes for A1C (P < 0.03), SCI-R (P < 0.004), Tinetti (P < 0.009), and 6MWT (P < 0.01) than the control group. Scores on PAID did not differ between the groups (P = NS).
Utilization of medical resources
The GDT spent approximately 58 min/patient in the intervention group for the initial evaluation and assessment of barriers. The phone calls by an educator during the 6-month intervention lasted about 131 min/patient (11 phone calls of ∼12 min). We evaluated utilization of outpatient medical services (e.g., ophthalmologists, podiatrists, primary care) and inpatient services (ED visits, hospitalizations) in both groups. The intervention and control groups did not differ in utilization of outpatient medical visits (3.8 vs. 3.9 visits/year). During the 12-month period, 5 of 70 participants from the intervention group reported eight diabetes-related ED visits (3 patients with multiple hypoglycemia and 2 with hyperglycemia), whereas none of the 30 participants from the control group reported diabetes-related ED visits. One participant from intervention group was hospitalized with hypoglycemia. The difference between the numbers of hypoglycemic episodes between the two groups did not reach statistical significance.
Missing data
Overall, 3 of 70 patients dropped out from the intervention group and 4 of 30 from the control group.
Primary outcome.
A1C data were available for 100% of the study population at the 6-month interval. For patients who dropped out, A1C data were collected from nonstudy visits in 6 subjects (3 from the intervention group and 3 from the control group). A1C data were missing in 3 of 70 in the intervention group and in 3 of 30 in the control group at 12 months.
Secondary outcomes.
Eight subjects (4 from the intervention group and 4 from the control group) did not complete the 6-month or 12-month study visits for secondary outcomes. Some patients declined to complete assessments as follows: 6 participants from the intervention group and 7 from the control group refused PAID and SCI-R tests. The 6MWT and Tinetti test had a higher number of missing data because these tests require not only the questionnaire but also physical performance. Some subjects were unable to do these tests because of comorbidities such as arthritis and difficulty ambulating at various times. In the intervention group, data on the Tinetti test were missing in 7% at 6 months and in 13% at 12 months, whereas in the control group, data were missing in 10% at 6 months and in 13% at 12 months. Similarly, in the intervention group, the data were missing for 6MWT in 20% at 6 months and in 21% at 12 months. For the control group, data were missing in 10% at 6 months and in 13% at 12 months.
CONCLUSIONS
Assessment of age-specific barriers is recommended for management of diabetes in older adults (4). Our study is the first to evaluate the effect of assessing self-care barriers and recommending coping strategies in elderly in a randomized controlled fashion. We identified several self-care barriers in older adults with poorly controlled diabetes. The most common barrier was inadequate medications, primarily due to older patients’ reluctance to make changes in insulin doses between clinic visits or during illnesses. The medical providers for most of the patients had prescribed insulin dose self-adjustment during a clinic visit, but the patients felt uncomfortable acting on the advice without talking to a health care provider. High glucose excursions were noted during many clinical and social life-events. In the intervention group, 24% of the patients had at least one unfavorable life-event (e.g., hospitalization, ED visits for non–diabetes-related conditions, surgeries, or death of close family members) that required additional medication adjustment during a 6-month period. We found that untoward clinical and psychosocial events occurred frequently, and even highly functional, independent older adults needed encouragement from a diabetes care provider to adjust medications. This strategy is more likely to benefit elderly patients who are taking insulin because they require dose adjustments with changes in overall health status. Further studies are also needed to see the efficacy of such an approach in older patients during vulnerable periods, such as after hospitalizations or rehabilitation, where the need for insulin adjustment is unavoidable.
In our study, the intervention and control groups both showed improvement in glycemic control after contact with educators. However, the phone contact by an educator cognizant of patient’s age-related barriers (intervention group) showed the additional benefit of maintaining functionality during the intervention period. The results of the 6MWT need caution in interpretation due to some older patients’ inability or unwillingness to complete the test at each time period. Our results were unexpected because specific physical training programs were not included in coping strategies. Encouraging physical activity appropriate for the patient’s overall health and social situation based on assessment of barriers may have helped improve compliance. We encouraged simple solutions, such as going to the senior center, joining a senior-friendly gym, or walking the hallways in apartment buildings, and using “exercise pedals” to maintain physical activities during the inclement weather frequently seen in New England. Our results are very encouraging, because maintaining or improving functionality is a desired outcome for chronic disease management and leads to improvement in overall health and quality of life (23). During the independence period, functionality declined but remained above the baseline level. Our results underscore the need for periodical encouragement to improve functional capacity in elderly diabetic subjects, easily achievable by phone contact.
One of the strategies used for improving medication adjustment was encouraging earlier appointments with the health providers. We found that patients had difficulty navigating appointment systems and automated phone systems, and were hesitant or unable to send home monitoring numbers to providers for adjustment. Phone contact with the educators helped in facilitating communications. A large number of patients also lacked basic understanding of how medications work and/or dietary skills. Although most patients had previous education in these areas, they did not understand or remember the information. This was a discouraging finding in patients treated at a tertiary care diabetes clinic. Whether the need for reeducation is a function of aging should be studied further. This deficit in knowledge would likely be greater in communities where diabetes education is not readily available. In patients with adequate knowledge, we found that educator still needed to provide assurance regarding adjustment of insulin doses and encouragement to call providers when glucose levels were not well controlled. Thus, even though the control group educator did not perform an intervention, she encouraged contact with providers for any diabetes-related question. This may have led to therapeutic adjustments by patients’ providers that would not have otherwise taken place. We believe this may be the reason why the primary outcome (A1C) improved in both arms in our study, albeit more clinically significant improvement occurred in the intervention arm.
As expected, diabetes-related distress improved in both groups. Talking to an educator helped lower the stress levels concerning diabetes in elderly patients. We also showed that during the independence period, distress scores worsened in both groups; however, they did not return to the patients’ baseline levels. The frequency of self-care also improved in both groups during the intervention period, likely due to attention by the educators. The improvement was sustained only by the intervention group, probably due to the tailored strategies provided during the intervention period.
When we measured resource utilization, no difference in outpatient care was seen between the two groups. There were more diabetes-related ED visits and hospitalizations in the intervention group, although the numbers were too small to make definite conclusions. Our small sample size and relatively short study period limits the ability to generalize this information. However, when comparing two high-risk groups, improvement in surrogate markers (improved functionality and self-care, reduced diabetes-related stress) indicate potential for cost-benefits in a large population over a longer period of time.
In this study, no changes were recommended to the diabetes treatment provided by patients’ providers so that we could target the effect of overcoming barriers and not the change in treatment regimen. The interventions focused on optimizing patients’ environment to enhance their ability to follow provider-led treatment recommendations. The study team felt that many patients with multiple comorbidities were on complex regimens that were clearly beyond their coping abilities. Studies evaluating the effect of regimen change to accommodate individual barriers are needed to improve management in this population.
No difference was found between the two methods of providing strategies to the intervention group. We believe this was due to the nature of our study population, who were highly functional and well-educated individuals who used a tertiary care facility for diabetes management. This population was highly functional and did not require assistance once recommendations were provided by the study team. Thus, when strategies were suggested via phone calls by the educator, patients did as well as those who received additional assistance by care manager. These findings may differ for a frailer population that may require assistance to perform care-coordination and implement suggestions such as arranging transportation, finding exercise venues, and scheduling appointments with multiple providers. In this study, because the two methods for providing strategies were equally effective, simple phone calls by an educator cognizant of patients’ barriers may prove to be a less costly approach. This area needs further investigation.
Our study highlights the complex challenge in studying older patients with multiple medical comorbidities. First, it was difficult to recruit and retain older patients with chronic medical conditions for a 12-month period. We also found that changes in A1C due to non–diabetes-related health issues and adverse medical and social events occurred in a large portion of our population beyond anyone’s control. However, we believe this is a strength of the study, increasing its generalizability.
Our study indicates the importance of age-specific barrier assessment and provides a practical approach for intervention. The study also shows the important role of phone contact with an educator between clinic visits in elderly patients with diabetes. This inexpensive strategy, if proven beneficial in a larger population, would form the basis for long-term policy change.
Acknowledgments
The study was partly supported by a grant from a clinical research award from the American Diabetes Association, 1-07-CR-40 (M.N.M.), and partly from the U.S. Department of Defense Peer Reviewed Medical Research Program of the Office of the Congressionally Directed Medical Research Programs, W81XWH-07-1-0282 (M.N.M.).
M.N.M. received research funding from sanofi-aventis. No other potential conflicts of interest relevant to this article were reported.
M.N.M. researched data, contributed to discussion, and wrote the manuscript. A.R.S. researched data and edited the manuscript. E.Su., C.R., A.S., J.G., E.St., P.B., L.D.R., and R.M. researched data. Y.L. and S.F. analyzed data. K.W. researched data, contributed to discussion, and edited the manuscript. M.N.M. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented in poster form at the 71st Scientific Sessions of the American Diabetes Association, San Diego, California, 24–28 June 2011.
Footnotes
Clinical trial reg. nos. NCT01480804 and NCT01486290, clinicaltrials.gov.
References
- 1.Centers for Disease Control and Prevention. U.S. Department of Health and Human Services. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Available from http://www.cdc.gov/diabetes/pubs/factsheet11.htm Accessed 3 July 2012
- 2.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med 2000;160:3278–3285 [DOI] [PubMed] [Google Scholar]
- 3.Gregg EW, Beckles GL, Williamson DF, et al. Diabetes and physical disability among older U.S. adults. Diabetes Care 2000;23:1272–1277 [DOI] [PubMed] [Google Scholar]
- 4.Brown AF, Mangione CM, Saliba D, Sarkisian CA, California Healthcare Foundation/American Geriatrics Society Panel on Improving Care for Elders with Diabetes Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc 2003;51(5 Suppl. Guidelines):S265–S280 [DOI] [PubMed] [Google Scholar]
- 5.Araki A, Ito H. Diabetes mellitus and geriatric syndromes. Geriatr Gerontol Int 2009;9:105–114 [DOI] [PubMed] [Google Scholar]
- 6.Huang ES, John P, Munshi MN. Multidisciplinary approach for the treatment of diabetes in the elderly. Aging Health 2009;5:207–216 [Google Scholar]
- 7.Munshi M, Grande L, Hayes M, et al. Cognitive dysfunction is associated with poor diabetes control in older adults. Diabetes Care 2006;29:1794–1799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Diabetes Association Standards of medical care in diabetes—2012. Diabetes Care 2012;35(Suppl. 1):S11–S63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anker SD, Koehler F, Abraham WT. Telemedicine and remote management of patients with heart failure. Lancet 2011;378:731–739 [DOI] [PubMed] [Google Scholar]
- 10.Shea S, Weinstock RS, Teresi JA, et al. IDEATel Consortium A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc 2009;16:446–456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weinger K, Butler HA, Welch GW, La Greca AM. Measuring diabetes self-care: a psychometric analysis of the Self-Care Inventory-Revised with adults. Diabetes Care 2005;28:1346–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Posner BM, Jette AM, Smith KW, Miller DR. Nutrition and health risks in the elderly: the nutrition screening initiative. Am J Public Health 1993;83:972–978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishiwaki Y, Breeze E, Smeeth L, Bulpitt CJ, Peters R, Fletcher AE. Validity of the Clock-Drawing Test as a screening tool for cognitive impairment in the elderly. Am J Epidemiol 2004;160:797–807 [DOI] [PubMed] [Google Scholar]
- 14.Drane DL, Yuspeh RL, Huthwaite JS, Klingler LK. Demographic characteristics and normative observations for derived-trail making test indices. Neuropsychiatry Neuropsychol Behav Neurol 2002;15:39–43 [PubMed] [Google Scholar]
- 15.Abrahams S, Leigh PN, Harvey A, Vythelingum GN, Grisé D, Goldstein LH. Verbal fluency and executive dysfunction in amyotrophic lateral sclerosis (ALS). Neuropsychologia 2000;38:734–747 [DOI] [PubMed] [Google Scholar]
- 16.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The Index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963;185:914–919 [DOI] [PubMed] [Google Scholar]
- 17.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–186 [PubMed] [Google Scholar]
- 18.Bautmans I, Lambert M, Mets T. The six-minute walk test in community dwelling elderly: influence of health status. BMC Geriatr 2004;4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 1986;34:119–126 [DOI] [PubMed] [Google Scholar]
- 20.Montorio I, Izal M. The Geriatric Depression Scale: a review of its development and utility. Int Psychogeriatr 1996;8:103–112 [DOI] [PubMed] [Google Scholar]
- 21.Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care 1995;18:754–760 [DOI] [PubMed] [Google Scholar]
- 22.Fillenbaum GG, Smyer MA. The development, validity, and reliability of the OARS multidimensional functional assessment questionnaire. J Gerontol 1981;36:428–434 [DOI] [PubMed] [Google Scholar]
- 23.Huang ES, Gorawara-Bhat R, Chin MH. Self-reported goals of older patients with type 2 diabetes mellitus. J Am Geriatr Soc 2005;53:306–311 [DOI] [PMC free article] [PubMed] [Google Scholar]