Abstract
OBJECTIVE
To investigate temporal improvements in blood pressure (BP) control in subjects with diabetes and policy changes regarding generic antihypertensives.
RESEARCH DESIGN AND METHODS
In a cross-sectional study we used logistic regression models to investigate the temporal relationship between access to generic antihypertensive medications and BP control (<130/80 mmHg) in 5,375 subjects (mean age, 66 ± 9 years; 61% African American) with diabetes and hypertension (HTN) enrolled in the national Results from the REasons for Geographic And Racial Differences in Stroke (REGARDS) cohort study between 2003 and 2007. At enrollment, BP was measured and medications in the home determined by medication label review by a trained professional. Generic antihypertensive medication status was ascertained from the U.S. Food and Drug Administration.
RESULTS
The percentage of subjects accessing generically available antihypertensive medications increased significantly from 66% in 2003 to 81% in 2007 (P < 0.0001), and the odds of achieving a BP <130/80 mmHg in 2007 was 66% higher (odds ratio 1.66 [95% CI 1.30–2.10]) than in 2003. Nevertheless, <50% of participants achieved this goal. African American race, male sex, limited income, and medication nonadherence were significant predictors of inadequate BP control. There was no significant relationship between access to generic antihypertensives and BP control when other demographic factors were included in the model (0.98 [0.96–1.00]).
CONCLUSIONS
Among African American and white subjects with HTN and diabetes, BP control remained inadequate relative to published guidelines, and racial disparities persisted. Although access to generic antihypertensives increased, this was not independently associated with improved BP control, suggesting that poor BP control is multifactorial.
Although recent controversy exists regarding the optimal target blood pressure (BP) value (1), it remains clear that consistent control of BP in patients with diabetes is important for limiting microvascular and macrovascular complications (2,3). However, our data (4) and other recent evidence (5) suggests that half or more of individuals with diabetes and hypertension are not meeting currently published target BP values (<130/80 mmHg), and we and others (4–6) have shown that racial disparities in BP control persist. Inadequate control is clearly multifactorial in origin (7), but evidence suggests that African Americans with hypertension are prescribed more antihypertensive agents, presumably to improve control and limit this disparity (6).
Our group (4) and Wang (8) have demonstrated a modest temporal improvement in BP control among diabetic subjects during recent years (2000–2007). We (4) have shown that this pattern of improvement was evident in both African American and white individuals. Although some data (9) suggest that this improvement results from longitudinal effects of the promulgation of the 2003 Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure guidelines (10), other factors may also be operative. Several temporal factors may be associated with improvement in BP control. In 2006, the introduction of both Medicare Part D drug coverage and inexpensive generic drug formularies (e.g., pharmacies at Wal-Mart) provided the potential for improved cost-related medication adherence. Another factor may be access to additional effective antihypertensive agents. Recent evidence from Briesacher et al. (11) has shown in adjusted models that the use of generic medications among diabetic patients can lead to modest but significant improvements in medication adherence. However, their study used employer-sponsored medical claims data to assess individuals beginning new drug therapy for chronic conditions, thus limiting the study’s generalizability. Therefore, we explored the relationship between increased access to generic medications and patterns of BP control in a population-based sample. We evaluated secular trends in access to generic antihypertensive drugs in hypertensive diabetic subjects from 2003 through 2007. In addition, we determined if there were discernible differences in these trends by race and whether this access to generic antihypertensives was associated with improved BP control.
RESEARCH DESIGN AND METHODS
The REasons for Geographic And Racial Disparities in Stroke (REGARDS) study is a study of health disparities and stroke incidence, the methods of which have been described in detail elsewhere (12). In short, REGARDS is a population-based, longitudinal cohort study of 30,239 subjects aged ≥45 years; 45% are men and 55% are women; 41% are African American and 59% are white; and 55% are from the “Stroke Belt” region (southeastern U.S.) and 45% are from the rest of the continental U.S. The REGARDS study is designed to examine the potential causes of excess stroke mortality in the Stroke Belt relative to the rest of the nation and among African Americans relative to whites. REGARDS provides a unique opportunity to examine recent trends in access to generic medications and BP control among African American and white hypertensive adults with diabetes. The study is national in scope and includes large numbers of adults with diabetes and hypertension.
The REGARDS cohort was recruited between January 2003 and October 2007. Enrollment of the cohort occurred during the implementation of Medicare Part D and generic formulary systems (e.g., pharmacies at Wal-Mart). REGARDS included a detailed computer-assisted telephone interview with each subject to collect demographic characteristics, including age, race (each subject self-reported race and, by design, Hispanic and Latino subjects were excluded; the REGARDS study compared only non-Hispanic African American and white subjects), and sex. Additional data collected through this interview included the following: annual household income (<$20,000, $20,000–$34,000, $35,000–$74,000, and ≥$75,000); education level (less than high school education, high school graduate, some college, and college graduate or higher); health insurance (yes or no); and health behaviors. Health behavior data included smoking (categorized as nonsmoker, past smoker, or current smoker); exercise (how often per week the subject exercised enough to work up a sweat, categorized as never, one to three times per week, or four or more times per week); alcohol consumption (categorized as none, moderate [one to seven drinks per week for women and one to 14 drinks per week for men], and heavy [anything more than moderate alcohol consumption]), and medical history information.
After the telephone interview, each subject completed an in-home visit conducted by a trained health professional, which included measurement of height and weight via standard procedures. BMI was calculated as the weight in kilograms divided by the height in meters squared. BP was obtained with an aneroid sphygmomanometer, using the appropriate cuff size, and was measured after the subject had been seated with both feet on the floor for at least 3 min. The average value of two BP measurements was used in analyses. At the home visit, blood specimens were obtained and total and HDL cholesterol levels were measured in accordance with the National Cholesterol Education Program guidelines (13). All prescription medication names were recorded verbatim from the pharmacy label during the home visit. Self-reported medication adherence or nonadherence was assessed using the previously validated four-item Morisky scale (14). This cross-sectional study of baseline data at the time of enrollment included all subjects who reported in their telephone interview that a physician had told them they had both hypertension/high blood pressure and diabetes. No in-home blood pressure or blood glucose measurements were used as a diagnostic measure for inclusion. Excluded from these analyses were any subjects who did not have both systolic BP and diastolic BP measurements (n = 22). The study was approved by the Institutional Review Board at the University of Alabama-Birmingham, and each subject provided informed consent.
The primary exposure was the percentage of antihypertensive medications belonging to the participant at the time of their in-home visit that were available on the market as a generic medication. For each participant, the percentage of generically available antihypertensive medications was determined as the number of antihypertensive medications being taken that was generically available at the time of the in-home visit divided by the total number of antihypertensive medications being taken by the participant. The generic status of each antihypertensive medication was determined from the U.S. Food and Drug Administration (FDA) website (www.fda.gov) by identifying the approval date for the marketing of one or more generic products containing that specific antihypertensive medication or combination of medications. The date of generic medication approval on the FDA website then was compared with the date of the REGARDS-related in-home visit to determine if the antihypertensive medication was generically available at the time of the in-home visit. Each antihypertensive medication was also categorized by pharmacological class (ACE inhibitors, angiotensin receptor blockers [ARBs], α-blocker, β-blocker, calcium channel blocker, central α-agonist, diuretic, vasodilator), and the number of agents from different classes was computed.
The initial analysis estimated the pattern of access to generic antihypertensive medications over the 2003–2007 time period by graphically portraying the percentage of all antihypertensives in use that were generically available during each year of enrollment. We then assessed the relationship between the percentage of generic antihypertensive medications available and both mean systolic and diastolic BP values (obtained during the in-home visit) as well as the percentage of subjects meeting American Diabetes Association (ADA) guideline-recommended BP goals (<130/80 mmHg). Temporal trends in the potential relationship between BP level and both number of antihypertensive medications and percentage that were available as generics over the time period 2003–2007 was assessed using a general linear model, with adjustment for age, sex, race, income, education, insurance, and medication adherence. The percentage of hypertensive diabetic subjects whose BP was <130/80 mmHg also was examined in a series of logistic regression models, stratified by race, that adjusted for the same factors. All analyses were performed using SAS version 9 (SAS Inc, Cary, NC).
RESULTS
Data were available for 5,375 subjects who reported having hypertension and diabetes; baseline data by race are presented in Table 1. Sixty-one percent of subjects with diabetes and hypertension were African American. As shown in Table 2, mean systolic and diastolic BP values were higher among African Americans than whites in each year. Likewise, the percentage of African American subjects receiving one or more antihypertensive medications was slightly higher, and the percentage using four or more antihypertensive medications was notably higher than that of whites at each time point. From 2003 to 2007, the use of ACE inhibitors seemed to decrease modestly without a discernible pattern by race. There was also a small increase in ARB use, again without a discernible pattern by race. There was a notable racial difference in the use of centrally acting α-agonists (e.g., clonidine), with African Americans being prescribed these agents more than twice as often as whites in most years.
Table 1.
Demographic and cardiovascular risk characteristics by race of the REGARDS study population with self-reported hypertension and diabetes (N = 5,375)

Table 2.
Antihypertensive medication prescribing patterns and BP control by race in diabetic hypertensive subjects, 2003–2007
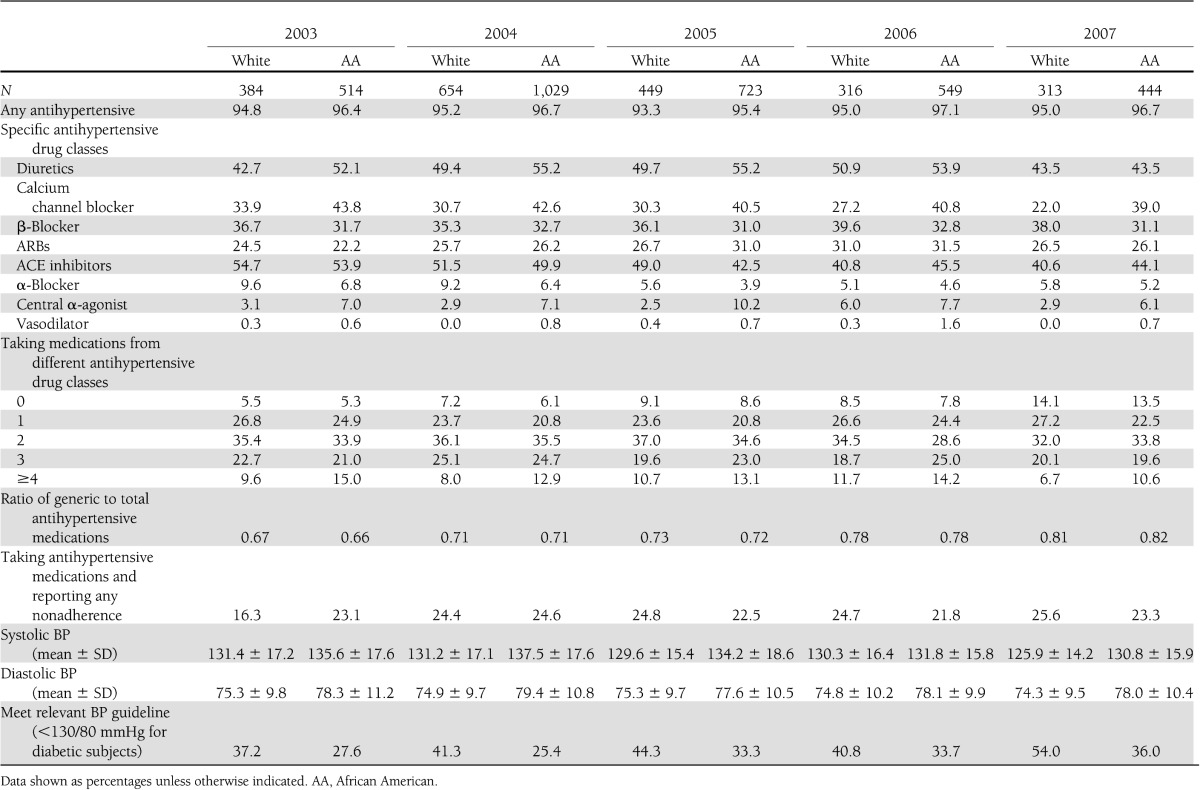
Twenty-three percent of subjects reported medication nonadherence. Although a contributor to BP control, the percentage of subjects reporting medication nonadherence did not vary significantly across the time period (see Table 2). However, as shown in Table 2, self-reported medication nonadherence was higher among African Americans enrolled in 2003, approximately equal by race in 2004, and then was higher in whites than African Americans enrolled in 2005–2007.
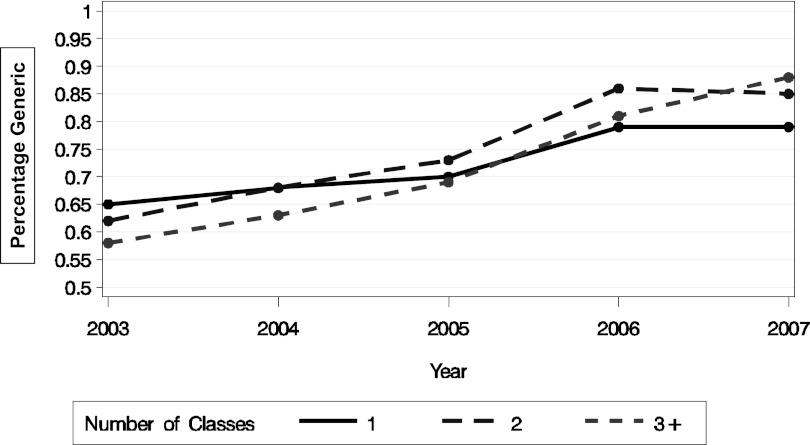
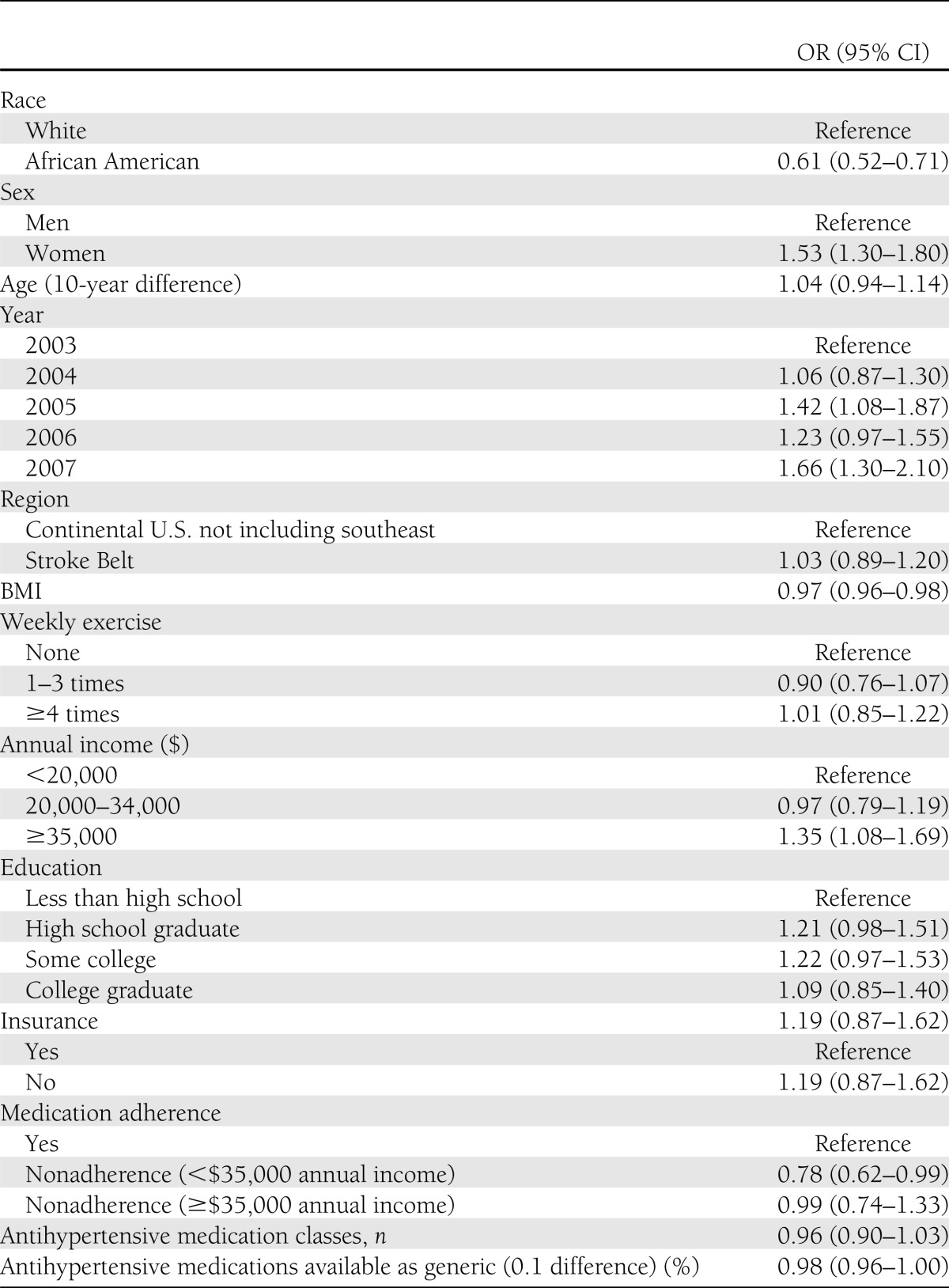
As shown in Fig. 1, the percentage of antihypertensive medications that were available as a generic medication increased significantly from 2003 to 2007 (P for trend < 0.001). The highest percentage of antihypertensive medications available as generic medications in 2007 was observed in subjects taking three or more antihypertensive medications. During this same time period, mean systolic BP and the odds ratio of subjects meeting ADA guideline-recommended target BP values (<130/80 mmHg) improved (P for trend < 0.001). The results of the general linear model predicting systolic BP demonstrate that multiple factors, including younger age, race (African American), sex (male), and self-reported medication nonadherence, were independently associated with higher systolic BP values (P < 0.05). However, the percentage of medications available generically was not significantly associated with systolic BP values (P > 0.05). In the logistic regression model examining the percentage of subjects with a BP <130/80 mmHg, African American race, male sex, annual income <$35,000, and medication nonadherence among those with an annual income <$35,000 were significant (P < 0.05) predictors of inadequate BP control (see Table 3). The percentage of antihypertensive medication available in generic form was not an independent predictor of BP control after adjustment for these factors. Residence in the southeastern U.S. (the Stroke Belt) was also not an independent predictor of inadequate BP control. When separate logistic regression models were examined for each race, after adjustment for other factors in the model, neither the percentage of antihypertensive medications available in generic form nor the number of antihypertensive classes being taken was an independent predictor of BP control.
Figure 1.
Percentage of antihypertensive medications available in a generic form by number of antihypertensive classes, 2003–2007. Data are least squared mean values adjusted for region (P value for trend < 0.0001).
Table 3.
Logistic regression model predicting odds of BP control (<130/80 mmHg) among hypertensive diabetic subjects (n = 3,485)
CONCLUSIONS
Nonadherence to antihypertensive medications is associated with poor BP control among patients with diabetes, and cost-related nonadherence is a major contributor (15,16). Although national efforts to improve outcomes is focused on the dissemination of evidence-based guidelines (8,10) and public funding for prescription costs (17), little is known about the impact of these strategies. This article adds to the literature by demonstrating important temporal trends in the equality of diabetes care. Those trends include a lower mean systolic BP, improvement in the percentage of subjects whose BP is at or below ADA guideline-recommended goals, and an increase in access to generic antihypertensive medications from 2003 to 2007 among those with concurrent diabetes and hypertension. However, despite improving BP values and increasing access to generic antihypertensive medications, the percentage of antihypertensive medications that are available in a generic form is not independently associated with improved BP control in multivariable analysis after adjustment for demographic and clinical variables. This finding is contrary to our hypothesis of an association between increased access to generic antihypertensives and improved BP control. Access to generic medication is only one of the factors influencing behavior with taking antihypertensive medication and BP control, and other unmeasured factors that impact both behavior with taking medication and BP control may be operative. These factors may include the patient’s perceptions regarding the severity of illness and the necessity of taking the medication, the patient’s trust in the prescriber, the patient’s health literacy and comprehension of instructions about medication use, and the patient’s perception of harms or risks associated with taking antihypertensive medications (18).
These findings have policy implications related to the limited impact on BP control that may result from improved access to generically available antihypertensive medications. Although generic antihypertensive use should continue because of the reduced health care costs, it should not be assumed that simply reducing medication costs alone will insure medication adherence and improved BP control. Broader strategies to seek an understanding of adherence to medication regimens as a behavior shaped by the beliefs and perceptions of the patient may be needed to affect adherence. Insurance and health systems that can provide information to the provider from pharmacy claims databases regarding the filling/refilling of generic antihypertensives may inform the provider’s ability to provide tailored health coaching regarding adherence and BP control. Finally, increased availability of cost-effective generic antihypertensive drugs in multiple pharmacologic classes should also facilitate intensification of treatment by the provider in the setting of uncontrolled BP.
These findings support the work of other investigators. The growth in access to generic medications is well described, and a recent systematic review (19) suggests comparable clinical outcomes with brand name and generic antihypertensive drugs. The growth in generic prescribing and the potential influence of electronic prescribing systems have been demonstrated by Stenner et al. (20). Van Wijk et al. (21) has shown that generic drug substitution among subjects with hypertension leads to a lower rate of nonadherence; however, they have not examined the effect on BP control. The present analysis demonstrates a temporal pattern of increased access to generically available antihypertensive medications that is paralleled by improvement in both mean BP values and the percentage of hypertensive subjects with diabetes and controlled BP. Furthermore, in subjects with a limited income, we show that medication nonadherence is a significant contributor that limits the percentage of subjects achieving ADA guideline-recommended BP control. It is perhaps reassuring to note that the percentage of subjects reporting medication nonadherence changed little across the time period studied despite increasing access to generic antihypertensive medications. This suggests trust in a comparable level of efficacy from generic medications relative to brand name medications. As reported above, there is an interesting trend by race: self-reported medication nonadherence was higher in African Americans enrolled in 2003 but higher in whites enrolled in 2005–2007.
It is possible that cost-related nonadherence may have been higher in African Americans with a limited income than whites in 2003 and may have been affected in later years by the increase in the availability of generic forms of antihypertensive medications. This finding warrants further investigation.
As we have reported previously (4), disparities in BP control between African Americans and whites with diabetes continue to persist. Our finding that African American men in particular have inadequate BP control despite improved access to generic medications suggests that additional research needs to focus on this high-risk subgroup. Additional research is necessary to clearly understand the relevance of generic medications and other factors that may be associated with BP control. Subsequently, culturally tailored interventions designed to specifically impact these contemporary factors affecting BP control among African American men with hypertension and diabetes might be developed and evaluated.
This study has important limitations. The examination of temporal trends is based on cross-sectional data collected during enrollment visits that occur across this time period and are examined by year of enrollment. The study examines BP control among African American and white adults ≥45 years of age, and results cannot be extrapolated to other racial groups or younger adults. No insurance information for these subjects is available to identify the subset of individuals who participated in Medicare Part D, nor is information available about the subjects’ participation in specific formulary programs.
Medication data were collected during an in-home visit; concurrence of these medication lists with prescribed medications in medical records was not confirmed. Medication adherence was examined using a validated self-reported measure but was not verified by pill counts, refill data, or data from electronically enabled medication bottles/caps. Despite these limitations, this study provided important data about the growth of access to generic antihypertensive medications and patterns of BP control during a critical time period of changing health policies in a large population of African American and white diabetic hypertensive subjects from across the U.S.
In conclusion, among a national sample of African American and white subjects with diabetes and hypertension, BP control has improved; however, it remains inadequate relative to published guidelines, and racial disparities in control persist. Moreover, although generically available antihypertensive medications have increased, this does not seem to be independently associated with patterns of improved BP control.
Acknowledgments
This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurologic Disorders and Stroke, National Institutes of Health, Department of Health and Human Services.
No potential conflicts of interest relevant to this article were reported.
D.M.C. wrote and revised the manuscript. A.J.L. performed biostatistical analyses and helped draft parts of the manuscript. G.H. and V.J.H. supervised data collection, entry, and analysis and reviewed and revised the manuscript. M.M.S., V.P., and P.M. reviewed and revised the manuscript. D.M.C. and A.J.L are the guarantors of this work and, as such, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions.
Footnotes
A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurologic Disorders and Stroke or the National Institutes of Health. Representatives of the funding agency reviewed the manuscript but played no role in the conduct of the study, collection of data, management of the study, analysis of data, or interpretation of data.
References
- 1.Cushman WC, Evans GW, Byington RP, et al. ACCORD Study Group Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Diabetes Association Standards of medical care in diabetes—2011. Diabetes Care 2011;34(Suppl. 1):S11–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UK Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703–713 [PMC free article] [PubMed] [Google Scholar]
- 4.Cummings DM, Doherty L, Howard G, et al. Blood pressure control in diabetes: temporal progress yet persistent racial disparities: national results from the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. Diabetes Care 2010;33:798–803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA 2010;303:2043–2050 [DOI] [PubMed] [Google Scholar]
- 6.Safford MM, Halanych JH, Lewis CE, Levine D, Houser S, Howard G. Understanding racial disparities in hypertension control: intensity of hypertension medication treatment in the REGARDS study. Ethn Dis 2007;17:421–426 [PubMed] [Google Scholar]
- 7.Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 2008;51:1403–1419 [DOI] [PubMed] [Google Scholar]
- 8.Wang YR. Lack of effect of guideline changes on hypertension control for patients with diabetes in the U.S., 1995-2005. Diabetes Care 2007;30:49–52 [DOI] [PubMed] [Google Scholar]
- 9.Krousel-Wood M, Muntner P, Carson A, et al. Hypertension control among newly treated patients before and after publication of the main ALLHAT results and JNC 7 guidelines. J Clin Hypertens (Greenwich) 2012;14:277–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–2572 [DOI] [PubMed] [Google Scholar]
- 11.Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Medication adherence and use of generic drug therapies. Am J Manag Care 2009;15:450–456 [PMC free article] [PubMed] [Google Scholar]
- 12.Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology 2005;25:135–143 [DOI] [PubMed] [Google Scholar]
- 13.National Cholesterol Education Program Expert Panel. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel: detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III), final report. Bethesda, MD, National Cholesterol Education Program, National Heart, Lung, and Blood Institute, National Institutes of Health, September 2002 (NIH publ. no. 02-5215)
- 14.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986;24:67–74 [DOI] [PubMed] [Google Scholar]
- 15.Fung V, Huang J, Brand R, Newhouse JP, Hsu J. Hypertension treatment in a medicare population: adherence and systolic blood pressure control. Clin Ther 2007;29:972–984 [DOI] [PubMed] [Google Scholar]
- 16.Muszbek N, Brixner D, Benedict A, Keskinaslan A, Khan ZM. The economic consequences of noncompliance in cardiovascular disease and related conditions: a literature review. Int J Clin Pract 2008;62:338–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Polinski JM, Kilabuk E, Schneeweiss S, Brennan T, Shrank WH. Changes in drug use and out-of-pocket costs associated with Medicare Part D implementation: a systematic review. J Am Geriatr Soc 2010;58:1764–1779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heisler M, Hofer TP, Klamerus ML, et al. Study protocol: the Adherence and Intensification of Medications (AIM) study—a cluster randomized controlled effectiveness study. Trials 2010;11:95–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kesselheim AS, Misono AS, Lee JL, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA 2008;300:2514–2526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stenner SP, Chen Q, Johnson KB. Impact of generic substitution decision support on electronic prescribing behavior. J Am Med Inform Assoc 2010;17:681–688 PubMed [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Wijk BLG, Klungel OH, Heerdink ER, de Boer A. Generic substitution of antihypertensive drugs: does it affect adherence? Ann Pharmacother 2006;40:15–20 [DOI] [PubMed] [Google Scholar]