Abstract
Background
Unemployment is associated with negative outcomes both during and after drug abuse treatment. Interventions designed to increase rates of employment may also improve drug abuse treatment outcomes. The purpose of this multi-site clinical trial was to evaluate the Job Seekers’ Workshop (JSW), a three session, manualized program designed to train patients in the skills needed to find and secure a job.
Method
Study participants were recruited through the NIDA Clinical Trials Network (CTN) from six psychosocial counseling (n=327) and five methadone maintenance (n=301) drug treatment programs. Participants were randomly assigned to either standard care (program-specific services plus brochure with local employment resources) (SC) or standard care plus JSW. Three 4-hr small group JSW sessions were offered weekly by trained JSW facilitators with ongoing fidelity monitoring.
Results
JSW and SC participants had similar 12- and 24-week results for the primary outcome measure (i.e., obtaining a new taxed job or enrollment in a training program), Specifically, one-fifth of participants at 12 weeks (20.1 – 24.3%) and nearly one-third at 24 weeks (31.4–31.9%) had positive outcomes, with “obtaining a new taxed job” accounting for the majority of cases.
Conclusion
JSW group participants did not have higher rates of employment/training than SC controls. Rates of job acquisition were modest for both groups, suggesting more intensive interventions may be needed. Alternate targets (e.g., enhancing patient motivation, training in job-specific skills) warrant further study as well.
Keywords: Substance Use Disorders, Vocational Rehabilitation, Treatment, Translational Research, Employment
1. Introduction
1.1 Substance Abuse and Unemployment
In the United States, unemployment is a chronic problem among persons with Substance Use Disorders (SUDs) (McCoy et al., 2007; Wong and Silverman, 2007). Recent national Drug and Alcohol Services Information System (DASIS) data confirm low rates of employment in a SUD treatment sample of persons 18 to 64 years of age (Substance Abuse and Mental Health Services Administration, 2008). Specifically, less than one-third of the sample (31%) was employed, with another one-third unemployed (33%) and the remaining 36% classified as “not in the labor force.” This latter group was comprised of labor force dropouts (61%), persons with disabilities (22%) and students, homemakers, inmates and retirees (17%).
Correlates of unemployment among persons with SUDs include poor work history, low motivation to become employed, and absence of skills necessary for available positions (Deren and Randell, 1990; Dunlap et al., 2007; Shepard and Reif, 2004; Zanis et al., 1994). In addition, persons with SUDs face barriers that make getting a job more difficult. Barriers can occur at multiple levels, including the client (e.g., family problems, poor social skills) and the treatment program (e.g., limited hours of operation) as well as society overall (e.g., social biases, weak labor market) (French et al., 1992). This is of concern, as SAMHSA found employment to be one of the best predictors of positive treatment outcome and an important measure of treatment success (Substance Abuse and Mental Health Services Administration, 2008).
Employed persons with SUDs have lower rates of relapse, less criminal activity, and fewer parole violations than unemployed persons (TOPPS II, 2003; Valliant, 1988). This finding is robust, and has been reported in both methadone maintenance (e.g., Jenner, 1998; Kidorf et al., 1994, 2004; McLellan et al., 1983; Platt, 1995) and abstinence-focused psychosocial (Kemp et al., 2004; Reif et al., 2004; Rosenheck and Seibyl, 1997) modalities of treatment.
Factors that contribute to the positive relationship between employment and SUD treatment outcomes are not fully understood. From a behavioral perspective, it is not surprising, as employment provides a compensated (reinforced) alternative to the behavior of drug use (Simpson et al., 1997; Koo et al., 2007). In addition, the social and economic contingencies are likely to promote continued abstinence. Alternatively, some posit a job provides a mechanism for reintroducing and reintegrating an individual back into his/her community (Kerrigan et al., 2000; Platt, 1995). Still others note that vocational services, delivered in concert with drug treatment, often strengthen self-esteem and contribute to self-efficacy, while enhancing problem solving and decision making skills (Shepard and Reif, 2004). In the long-term, employment-focused training and services can contribute to motivation, quality of life and psychological functioning (French et al., 1992; Kingree, 1997).
Despite high rates of client unemployment, research has shown that only 24–46% of community treatment programs offer some form of employment counseling (Freidmann et al., 2000; Henderson et al, 1999; Lee et al., 2001). In methadone maintenance treatment programs, Etheridge and colleagues (1995) found less than 4% of sites offered employment services. Resources to provide ancillary vocational services remain limited. In addition, some treatment providers believe employment counseling falls outside the authority of addiction counseling and should remain separate (Young, 2000). This is unfortunate, as the data suggest not only clinical, but also economic (cost) benefits could be found if more clients returned to productive employment (Shepard and Reif, 2004).
1.2 The Job Seekers’ Workshop (JSW)
The present study was spearheaded by several drug treatment program directors in the NIDA Clinical Trials Network (CTN) who identified unemployment as an area in need of additional resources and interventions. They also recognized that training in skills needed to find and secure a job (e.g., completing a resume, interviewing for a position) was integral to other employment-focused services. In addition, they believed a study focused on job-seeking skills training would afford the best opportunity for contributing not only to our scientific knowledge base, but also to their clinical practice armamentarium.
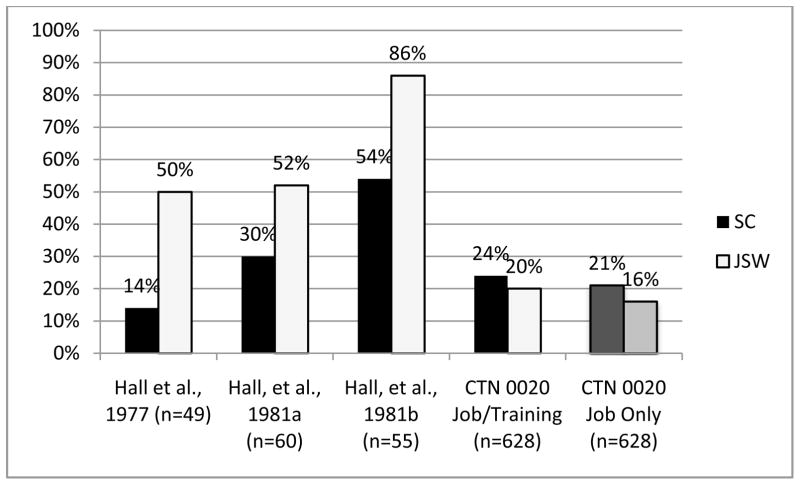
A review of the literature at that time identified only one empirically-tested intervention focused on skills needed to find and secure a job. The Job Seekers’ Workshop (JSW) was developed specifically for drug dependent individuals. JSW was tested in the late 1970’s and demonstrated efficacy in both heroin dependent parolees and probationers (Hall et al., 1981a) and unemployed methadone maintenance patients (Hall et al., 1981b). In a 1977 pilot study with 49 subjects, 50% of the JSW group as compared to 14% of controls obtained employment/training at follow-up (Hall et al., 1977). In another study (N=55 subjects), rates of employment were significantly higher for JSW vs control subjects (86% and 54%, respectively, at 3 month follow-up; p<.03) (Hall, et al., 1981a). In a third study (N=60 subjects), a similar pattern was observed. While not statistically significant, rates of employment were nearly 2 times higher for JSW (52%) as compared to control (30%) subjects (Hall et al, 1981b).
Through the NIDA CTN, the present study examined efficacy of JSW in a much larger and more heterogeneous treatment-based sample of persons with SUDs. In a multi-site randomized clinical trial, the present study compared employment outcomes in participants randomized to either JSW or Standard Care (SC). Both methadone maintenance and psychosocial outpatient modalities of treatment participated in the research. Based on earlier data, we hypothesized that time (days) to either a new taxed job or job-training program and total hours worked in a taxed job or spent in skills training would be higher for JSW as compared to SC control group members at 12-week follow-up.
2. Methods
2.1 Participants
Study participants were recruited nationally from 11 drug abuse treatment programs. All sites obtained approval from local institutional review boards prior to study launch. Both men and women of a wide range of racial and ethnic groups were invited to participate in the research if they met the following primary inclusion criteria: 1) 18 years of age or older; 2) fulfilled DSM-IV diagnostic criteria (lifetime) for Alcohol and/or Drug Abuse or Dependence; 3) had been enrolled in the substance abuse treatment program for a minimum of 30 days; 4) were unemployed (no taxed or non-taxed work in the four weeks prior to study enrollment) or underemployed (worked no more than 20 hrs/week in the past four weeks); and 5) reported interest in obtaining a job. Individuals who were unable to provide informed consent due to cognitive impairment, psychiatric instability or language barriers were excluded from study participation. Ability to provide informed consent required a score of 80% or above on a 10-item, true-false exam that assessed client understanding of the research design and study procedures.
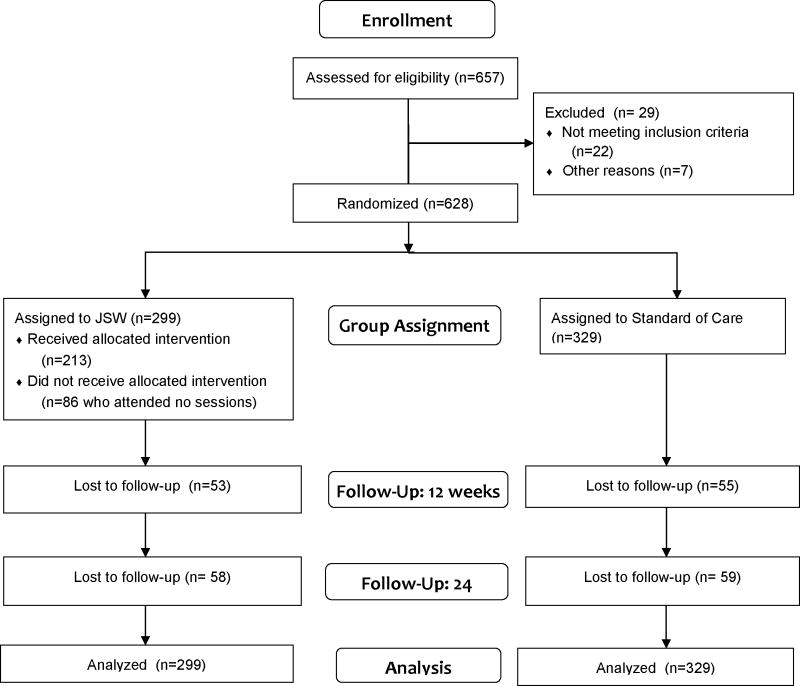
A total of 657 individuals were consented for study participation. Of those, 22 participants (3.3%) did not meet study inclusion criteria and 7 participants (1.1%) did not return for the baseline assessment. The remaining 628 participants (95.6%) were randomized into the clinical trial. (See Figure 1, CONSORT Diagram, for schematic of study components and participant flow from enrollment through data analysis (Schulz et al., 2010)).
Figure 1. CONSORT Flow Diagram.
The flow diagram for the 2-group randomized clinical trial is displayed. Participant screening, recruitment, randomization and follow-up rates at 12 and 24 weeks post-randomization are shown.
2.2 Study Sites
Participating treatment programs (n=11) were members of the NIDA Clinical Trials Network (CTN) who expressed interest in testing the Job Seekers’ Workshop. Both outpatient psychosocial counseling (n=6) and methadone maintenance (n=5) programs were represented. Outpatient psychosocial programs were located in Michigan, Virginia, Massachusetts, New Mexico, South Carolina and Oregon. Methadone maintenance programs were located in Michigan, Maryland (2), Massachusetts and California. Both rural and urban programs were represented.
2.3 Study Recruitment and Randomization
Potential study participants were identified through both self- and counselor-based referrals. Flyers describing the study were posted in public areas (e.g., waiting rooms, bulletin boards) at each treatment program to encourage self-referrals. Research staff also periodically attended treatment team meetings to remind therapists about the study and encourage patient referrals. Once identified, potential participants would meet briefly with research assistants (RAs) to learn more about the study. Those with continued interest completed informed consent procedures and baseline assessment. RAs then contacted the Data Management Center (DMC) for the protocol. The DMC verified participant eligibility and used urn randomization procedures to randomly assign individuals to either the Job Seekers’ Workshop (JSW) or Treatment as Usual (Standard Care, SC), with stratification on the basis of employment history (yes or no response to the question “Were you employed at all in the past 5 years?”) and current employment status (unemployed or underemployed in the 4 weeks prior to study enrollment).
2.4 Baseline Assessment
Baseline assessment focused on participant demographics, alcohol and drug use severity, employment/work history and psychosocial functioning. Measures included the CTN Common Assessment Battery (CAB) as well as protocol-specific measures. The majority of baseline assessments were administered in interview format and required approximately 2 hours to complete. Urine samples were also collected in drug test cups with temperature-controlled monitoring. On-site assays were done using On-Track Test cups and other supplies provided by NIDA approved supplier (Roche Diagnostics, Basel, Switzerland). Urine toxicology tested for the presence of: cocaine, opiates, methadone, THC, PCP, amphetamines, barbiturates, methamphetamines and benzodiazepines. Participants received a $25 gift certificate as compensation for their time and effort.
2.5 Assessment Measures
The present study used data from two CAB measures: Addiction Severity Index-Lite (ASI-Lite) and the Alcohol and Drug Modules of the Composite International Diagnostic Interview (CIDI-2.1) (World Health Organization, 1990). The ASI (McLellan et al., 1980, 1999) has a high level of psychometric support (McLellan et al., 1980, 1999; Alterman et al., 1994, 2001). The ASI-Lite, used in the CTN, eliminated some questions which were collected elsewhere in the assessment battery and/or were not used in the calculation of composite scores.
In addition, the following protocol-specific assessments were collected: Wide Range Achievement Test (WRAT-3) (Wilkinson, 1993), Addiction Severity Index-Addendum for Women (assesses domains germane to women) (Comfort and Kaltenbach, 1996; Comfort et al., 1999); Vocational Survey (VS) and the Timeline Follow Back Interview for Employment (TLFB-E). Of the protocol-specific measures, only the TLFB-E and one item (job type) from the Vocational Survey were used in the present study.
Timeline Follow Back Interview for Employment (TLFB-E)
The TLFB-E uses procedures originally developed to measure alcohol consumption in problem drinkers (Sobell et al., 1996). The original TLFB was found to collect reliable and valid retrospective estimates of drinking behavior (Sobell et al., 1996). TLFB methods have subsequently been used to accurately track other behaviors (e.g., episodes of violence and gambling behavior) (e.g., Caetano et al., 2001). For the present study, TLFB procedures were used to collect employment-related measures (e.g., days worked, number of hours worked per day). The TLFB-E uses a calendar to assist participants in providing retrospective estimates of vocational activity. At baseline, the TLFB-E was used to confirm that each participant met study criteria for unemployment or underemployment. At follow-up, it was used to document onset of employment and hours worked during the period of assessment as well as enrollment and hours spent in formal job training.
2.6 Study Conditions
Job Seekers’ Workshop (JSW)
JSW is based on the premise that information and practice in job acquisition skills will facilitate job placement (Hall et al., 1977), and preliminary studies demonstrated its effectiveness (Hall et al., 1981; Hall et al., 1981 a, b; Sorensen et al., 1988). The intervention seeks to improve job-seeking skills and job interview behaviors. Administered in three 4-hour, small group sessions, JSW focuses on locating available jobs, making “cold calls” to potential employers, and rehearsing job interview skills. Individualized videotape feedback is a primary component and allows participants to practice and gradually improve their job interview skills.
The three JSW sessions were offered consecutively, one session per week, for the first three weeks of every month, with make-up sessions scheduled as needed. Make-up sessions occurred primarily in week 4 of every month, but additional sessions could be scheduled to facilitate attendance. Participants recruited in the prior month were invited to start at the beginning of the next workshop series. Snacks and beverages were provided to ensure participant comfort and minimize early departure from a JSW session.
Standard care (SC)
Procedures for the control group were designed to represent “standard care” as it existed within each participating treatment program. Thus, each program was free to offer vocational groups or make community referrals according to their usual care practices. The one SC element that was standardized across all participating programs was a Community Job Resources Brochure (CJRB). Each treatment program tailored the CJRB to provide information about job placement and vocational training resources specific to their local communities. The CJRB included names, addresses and telephone numbers for local employment service providers. In most cases, this was the only service offered by the agency. JSW research staff provided guidance and consultation during brochure development. Since CJRB was integrated with SC at each site, all participants (JSW and SC) received the CJRB following randomization.
2.7 JSW Training and Fidelity Monitoring
At each site, at least two individuals were trained to administer the JSW intervention. Training was provided by two JSW intervention experts, one of whom had been a member of the original research team that developed and empirically tested JSW (P.L, co-author). For the current protocol, JSW training consisted of two full-days of didactic and experiential learning including role-play exercises. Facilitators then returned home where they practiced the intervention with at least one group of pilot drug dependent persons, submitted tapes of these sessions and obtained feedback and guidance from supervisors and JSW experts. Certification of JSW facilitators was completed based on performance during training and review of taped pilot sessions.
Thereafter, all certified JSW facilitators participated in monthly phone calls with the training experts to review ongoing JSW session experiences, provide feedback and monitor adherence to workshop implementation guidelines. In addition, study coordinators or clinical supervisors in each CTN Node, trained in the JSW intervention, regularly monitored JSW facilitator sessions either in-person or via audio taping using Likert rating scales developed by the training experts. Rating forms were used to provide feedback to JSW facilitators with a constant effort to maximize fidelity of intervention delivery.
2.8 Study Follow-Up
Follow-up assessments were conducted at 4, 12 and 24 weeks post-randomization. Follow-up assessments included the ASI-Lite, Vocational Survey and the TLFB-E. Each assessment focused on the time that had elapsed since the previous assessment. All participants were compensated using gift certificates for their time and effort. Specifically, they received $20 for 4-week follow-up, $30 for 12-week follow-up, and $40 for 24-week follow-up. In addition, a $40 bonus was awarded to participants who completed all 3 follow-up assessments. Taken together, all participants could earn up to $155 in gift certificates for full participation in baseline and follow-up assessments.
2.9 Data Analysis
Baseline comparisons between those randomized to JSW and SC were performed using chi-square analyses for categorical and t-tests for continuous variables. Primary analyses compared JSW and SC groups with regard to two employment outcomes at 12-week follow-up: 1) Time (number of days) to either a new taxed job or enrollment in a job-training program during 12-week follow-up; and 2) total hours worked in a taxed income job and/or hours accumulated in job skills training during 12-week follow-up. The 12-week timeframe was selected because that is the period most likely to be influenced by the workshop intervention. For secondary analyses, non-taxed employment was included and outcomes were expanded to include the full 24-week follow-up period. An additional outcome measure, job acquisition alone (excluding job training), was also created and analyzed comparing JSW and SC groups using procedures summarized below.
To compare treatment groups for all time to event variables (i.e., time to a new taxed job/training enrollment and time to a new taxed or non-taxed job/training enrollment within 12 weeks and within 24 weeks), Cox proportional hazards regression was used. For time to a job/training within 12 weeks, we censored individuals who failed to obtain employment or job training within by the end of the 12 week follow-up at 84 days. For the 12 week follow-up, we were unable to determine job/training status at the three month follow-up for 43 (6.85%) subjects. These subjects were censored to 84 days. For the 24 week follow-up, we were unable to determine job/training status at that time for 42 (6.69%) subjects. These individuals were censored to 168 days. Similarly, we censored those not obtaining a job or job training within the 24 week period to 168 days. These analyses were repeated but with the addition of a study site term. To compare JSW and SC groups for total hours worked and/or in training, t-tests were used. As before, the analysis was repeated including a site term and using ANOVA. We were able to obtain the number of hours worked or in training for all subjects who had obtained a job or training. For subjects that were missing at follow-up (12 or 24 weeks), subjects were assigned to zero hours.
We subsequently examined whether the relationships between treatment and outcomes were differentially affected by several covariates. Based on the literature, initial discussions with protocol planning group, and input from counselors and JSW facilitators at participating sites, five covariates were chosen: gender, modality (psychosocial vs. methadone maintenance), days in treatment prior to baseline assessment (1–6 months vs. >6 months); working in the four weeks prior to baseline assessment (yes/no); and recent drug use (positive or negative drug screen at baseline).
For time to event variables, Cox regressions were repeated with main effects for treatment and the covariate of interest plus a treatment X covariate interaction term. If the interaction term was significant, stratified models (stratifying by the covariate) were planned. For the outcome of total hours worked, ordinary least squares regression was used. Separate regression analysis for each covariate was run by entering a main effect for treatment group and the covariate along with a treatment X covariate interaction term. If the interaction term was significant, stratified models were to be run, examining total hours worked/training hours by treatment group, stratifying by each level of the covariate.
3. Results
3.1 Baseline Demographic and Drug Use Histories
Demographic and substance use characteristics for participants randomized to JSW and SC conditions are summarized in Table 1. No baseline differences were found between JSW and SC group participants for the variables summarized in the table. Participants were primarily Caucasian (40.9%) or African American (38.8%). They had less than a high school education (mean 11.98 (SE=0.09) years), and were approximately 41.12 (SE=0.43) years old. Average time in treatment at study enrollment was almost 1 ½ years (mean 505.39 days (SE=35.62)). Stratification variables are also summarized in Table 1. JSW and SC groups did not differ on either measure, with approximately 84% of both groups reporting no work in the 4 weeks prior to study enrollment (unemployed) and approximately 80% of both groups indicating having worked at some point during the preceding 5 years.
Table 1.
Comparison of demographic and baseline characteristics of individuals randomized to JSW and SC conditions
| N | JSW (n=299) | SC (n=329) | p-value |
|---|---|---|---|
| Age group | |||
| 18–29 | 46 (15.4) | 72 (21.9) | χ2=4.640, p=0.200 |
| 30–39 | 64 (21.4) | 70 (21.3) | |
| 40–49 | 113 (37.8) | 114 (34.7) | |
| 50+ | 76 (25.4) | 73 (22.2) | |
| Education (%) | |||
| 0–11 years | 90 (30.1) | 109 (33.1) | χ2=2.892, p=0.236 |
| 12 years | 127 (42.5) | 118 (35.9) | |
| 13+ years | 82 (27.4) | 102 (31.0) | |
| Time in treatment at study enrollment | |||
| 1–6 months | 171(57.2) | 199 (60.5) | χ2=0.703, p=0.402 |
| > 6 months | 128 (42.8) | 130 (39.5) | |
| Race (%) | |||
| Caucasian | 120 (40.1) | 137 (41.6) | χ2=1.483, p=0.476 |
| African American | 123 (41.1) | 121 (36.8) | |
| Other (incl multi-racial) | 56 (18.7) | 71 (21.6) | |
| Gender (%) | |||
| Male | 144 (48.2) | 150 (45.6) | χ2=0.415, p=0.520 |
| Female | 155 (51.8) | 179 (54.4) | |
| Recent Employment (past 4 weeks) (%) | |||
| Unemployed | 247 (82.6) | 280 (85.1) | χ2=0.724, p-=0.395 |
| Underemployed | 52 (17.4) | 49 (14.9) | |
| Employed at all in past 5 years (%) | |||
| Yes | 234 (78.3) | 270 (82.1) | χ2=1.432, p=0.232 |
| No | 65 (21.7) | 59 (17.9) | |
| Modality of Treatment (%) | |||
| Methadone Maintenance | 142 (52.5) | 159(51.7) | χ2=0.044, p=0.834 |
| Psychosocial Outpatient | 157 (47.5) | 170 (48.3) | |
| Lifetime Abuse/Dependence (%)a | |||
| Alcohol | 202 (67.8) | 236 (71.7) | χ2=1.157, p=0.282 |
| Cocaine/Other Stimulants | 206 (68.9) | 224 (68.1) | χ2=0.048, p=0.827 |
| Opioids | 189 (63.2) | 230 (69.1) | χ2=3.165, p=0.075 |
| Marijuana | 159 (53.2) | 176 (53.5) | χ2=0.006, p=0.936 |
| Drug screen on intake (%)b | |||
| Positive | 158 (52.8) | 171 (52.0) | χ2=0.047, p=0.828 |
| Negative | 141 (47.2) | 158 (48.0) | |
Based on DSM-IV diagnoses
Excluding methadone.
3.2 Study and Intervention Participation
Review of JSW session attendance records found considerable variability, with nearly half of participants randomized to JSW (48.5%) attending all three workshop sessions and approximately one-fourth (28.7%) attending no scheduled sessions. The remaining 22.7% of the JSW sample attended an intermediate number (1 or 2) of sessions. The size of JSW groups ranged from 1 to 4 participants, with an average of 1.5 persons per session and the average session lasted approximately 2 hours.
Rates of follow-up interview participation for those randomized to JSW and SC were 82.3% and 83.3%, respectively, at 12 week assessment and 80.6% and 82.1% at 24 week assessment. Follow-up rates did not differ for the two groups.
3.3 Employment Outcomes for JSW and SC Participants
3.3.1 Rates of New Job/Training Acquisition
Rates of new job/training acquisition are summarized in Table 2 (top panel). Two time intervals were examined: 1–12 and 1–24 weeks post randomization. Also, employment was defined in two ways: a) new taxed job or enrollment in a job training program; and b) new taxed or non-taxed job or job training program. Rates of employment/training did not differ for JSW and SC groups. Specifically, less than one-fourth of participants in both the JSW (20.1%) and SC (24.3%) groups obtained a taxed job/training during weeks 1–12. For weeks 1–24, rates of new taxed job acquisition or training rose to nearly one third. Again, rates did not differ for JSW and SC groups.
Table 2.
Employment outcomes: Days to employment and number employed, (weeks 1–12 and 1–24) by treatment condition
| Variable Number employed | Standard Care (n=329) | Job Seekers Workshop (n=299) | Unadjusted Hazard ratio (95% CI) | Chi-square p-value | ||
|---|---|---|---|---|---|---|
|
| ||||||
| # | % | # | % | |||
|
| ||||||
| Employed in new taxed job or enrolled in a job training program (weeks 1–12) | 80 | 24.3 | 60 | 20.1 | 0.80 (0.57–1.11) | χ2=1.80, df=1 p=0.179 |
| Employed in new taxed/non- taxed job or enrolled in job training (weeks 1–12) | 115 | 35.0 | 100 | 33.4 | 0.93 (0.70–1.23) | χ2=0.29, df=1, p=0.593 |
| Employed in new taxed job or enrolled in a job training program (weeks 1–24) | 105 | 31.9 | 94 | 31.4 | 0.95 (0.72–1.26) | χ2= 0.12, df=1, p=0.726 |
| Employed in new taxed/non- taxed job or enrolled in job training (weeks 1–24) | 143 | 43.5 | 149 | 49.8 | 1.41 (0.91–1.44) | χ2=1.27, df=1, p=0.26 |
| Variable Number of Days | Standard Care | Job Seekers Workshop | T-Test | ||
|---|---|---|---|---|---|
|
| |||||
| Mean | SE | Mean | SE | ||
|
| |||||
| Number of days to new taxed job or training program (weeks 1–12) | 34.05 (n=80) | 2.72 | 38.28 (n=60) | 3.17 | t=1.01, df, 138, p=.312 |
| Number of days to new taxed/non-taxed job or training program (weeks 1–12) | 34.60 (n=115) | 2.41 | 36.90 (n=100) | 2.40 | t=0.67, df=213, p=.502 |
| Number of days to new taxed job or job training program (weeks 1–24) | 55.60 (n=105) | 4.42 | 69.14 (n=94) | 4.89 | t=2.06, df=197, p=.041 |
| Number of days to new taxed/non-taxed job or job training program (weeks 1–24) | 52.82 (n=143) | 3.73 | 66.40 (n=149) | 3.99 | t=2.48, df=290, p=.014 |
Since two previous JSW studies did not include formal job training in their outcome investigations (Hall et al., 1981 a, b), analyses were repeated using only job acquisition as the criterion (i.e., enrollment in job training was no longer classified as a favorable outcome). For Weeks 1–12, n=140 participants (of 628) obtained a job and/or enrolled in job training. Of this sample, n=117 (83.6%) obtained a taxed job while n=30 (21.4%) enrolled in formal job training. Of the 30 enrolling in training, 7 also obtained a new taxed job. Thus, enrolling in training contributed an additional 23 subjects to the primary outcome. Over the 12 week follow-up period, 18.6% (n=117) of the total sample acquired taxed employment. For Weeks 1–24, n=199 participants obtained a job/enrolled in training. Of these, n=172 (86.4%) obtained a taxed job, with n=27 in training alone. A total of 45 subjects enrolled in training with 18 of those also obtaining a new taxed job. In this case, 27.4% of the total sample obtained taxed employment over the full 24 week follow-up. Chi-square analyses comparing rates of new taxed employment (omitting training) for JSW and SC groups demonstrated no significant differences at either Weeks 1–12 (χ2=1.894, df = 1, p=0.169) or Weeks 1–24 (χ2=0.115, df=1, p=0.735). (Cox regression analyses were nearly identical and are not reported.)
Since many consider full-time (35+ hours/week) employment to be the “gold standard” in a clinical trial of job acquisition, rates of Full Time employment (taxed and untaxed), excluding part time work, for SC and JSW groups, were also compared at Weeks 12 and 24. Rates of full-time employment (taxed or untaxed) for SC and JSW participants did not differ at either end of week 12 (6.1% vs. 6.7%, respectively) (χ2 = 0.098, df=1, p=0.755) or week 24 (5.2% vs. 6.0%, respectively) (χ2=0.217, df=1, p=0.642).
3.3.2 Types of Jobs Acquired by Study Participants
For participants who attained employment during the 1–24 week follow-up, we also reviewed the types of jobs they acquired. At 24 weeks post-randomization, almost one quarter of jobs (27.0%) were classified as unskilled labor, with an additional 13.7% labeled “some type of manual labor” (e.g., construction, warehouse work, landscaping). An additional 15.5% of acquired jobs were categorized as clerical or sales (e.g., secretary, retail sales, cashier). Additional job categories included: child or geriatric care (7.8%), restaurant work (11.9%), janitorial or cleaning services (7.4%) and other skilled labor (10.4%). Finally, a smaller percentage of jobs were classified as managerial positions (3.3%), driving/delivery services (2.2%) and temp services (2.2%).
3.3.3 Time to New Job/Training Acquisition
Table 2 (bottom panel) uses t-tests to compare days to new job or training program for JSW and SC group members. Only those participants who obtained a job/enrolled in training during either the 1–12 or 1–24 week follow-up periods were included in the analyses. Separate comparisons were made for taxed work/job training (taxed only) and work/job training (taxed and non-taxed combined). For weeks 1–12, days to new job/training were comparable for the 2 groups. For weeks 1–24, however, significant differences were found. Specifically, mean days to new taxed job/training for SC participants was significantly shorter (55.6 days) than that for JSW participants (69.1 days (t=2.06, df=197, p<.05). The same pattern was seen for taxed or non-taxed job/training, with SC participants acquiring a job sooner than JSW participants (52.8 and 66.4 days, respectively; t=2.48, df=290, p<.05).
3.3.4 Hours worked in new job/training program
Average hours worked in a new job or training program by JSW and SC group participants over the 12- and 24-week time periods are shown in Table 3. Separate comparisons were made for taxed work/job training alone and taxed or non-taxed work/job training. T-test analyses found no significant between-group differences regardless of how employment was defined or the time interval.
Table 3.
Employment outcomes: Hours worked (weeks 1–12 and 1–24) by treatment group
| Variable | Standard care (n=329) | Job Seekers Workshop (n=299) | T-test | ||
|---|---|---|---|---|---|
|
| |||||
| Mean | SE | Mean | SE | ||
| Total hours worked new taxed job or enrolled in job training program (weeks 1–12) | 20.6 | 3.0 | 15.8 | 2.8 | t=1.19, df, 625.7, p=0.233 |
| Total hours worked in new taxed/non- taxed job or training program (weeks 1–12) | 45.5 | 5.4 | 47.9 | 6.1 | t=0.30, df=626, p=0.765 |
| Total hours worked in new taxed job or job training program (weeks 1–24) | 43.8 | 5.4 | 47.4 | 6.6 | t=0.43, df=590.4, p=0.669 |
| Total hours worked in new taxed/non- taxed job or job training program (weeks 1–24) | 119.6 | 12.0 | 131.9 | 13.3 | t=0.69, df=626, p=0.490 |
Since the majority of participants were not employed during either follow-up period, the analyses in Table 3 included many zero values, resulting in a non-normal distribution. While there is no ideal solution for analyzing such data (e.g., various transformations will not normalize the distribution), we also selected only those who obtained a job or training in the 12- and 24-week follow-up periods and compared JSW and SC groups on total hours worked or in training. Our rationale is that while the rates of obtaining a job/training did not differ, we might observe a difference in hours worked when only those who obtained a job/training were included in the analyses.
Using t-tests, we again observed no significant group differences. For example, the mean number of hours worked or in training was 78.7 (SE=10.41) for the 60 subjects in the JSW group who obtained a new taxed job or training during weeks 1–12. This was not significantly different from the mean of 84.9 hours (SE=8.99) for the 80 subjects in the SC group who obtained a new taxed job/training within the same follow-up period (t=−0.45, df=138, p=0.655). Similarly, no differences were found between JSW and SC groups when the definition of employment was broadened to include both taxed and non-taxed jobs. During the first 12 weeks of follow-up, individuals who obtained a new taxed or non-taxed job during that time, JSW participants (n=100) worked a mean of 143.1 (SE=14.01) total hours and SC participants (n=115) worked a mean of 130.0 (SE=11.94) total hours (t=0.72, df=213, p=0.474). Further, no between-group differences were noted in weeks 1–24 with regard total hours worked in a new taxed job or job training (t=0.66, df=197, p=0.509), or total hours worked in a new taxed or non-taxed job or job training (t=−0.34, df=290, p=0.734).
3.4 Potential interactions: Subgroup comparisons of employment outcomes
While there were no significant JSW and SC differences in primary and secondary outcomes, it is possible that the intervention was effective for certain subgroups. For the present study, 5 variables were selected. Some were identified during protocol development, while others were selected based on protocol workgroup feedback during study development and implementation. The 5 variables selected for subgroup comparisons were: gender (male and female); treatment modality (methadone maintenance and abstinence-focused outpatient); time in treatment at study enrollment (1–6 months and > 6 months at baseline assessment); employment during the 4 weeks prior to baseline assessment (unemployed (no work whatsoever) and underemployed (0<x<20 hrs/week)) and drug use (positive and negative drug urinalysis assay at baseline).
For time to event variables, Cox regressions were run, entering each of the 5 variables above as main effects and including an interaction term of the covariate X treatment group. While three of the covariates showed significance as main effects for both the 1–12 and 1–24 week time periods (days in treatment prior to baseline, treatment modality and recent drug use (urine drug assay), no significant interaction terms were observed. Thus, we did not proceed to testing stratified models.
For the hours worked/training, ordinary least squares regression models were run (with a treatment group main effect, a covariate main effect and an interaction term of treatment X covariate). Again, significant main effects were found for several of the covariates for weeks 1–12 (days in treatment prior to baseline and treatment modality) and weeks 1–24 (days in treatment prior to baseline, treatment modality and recent drug use). However, interaction terms were not significant.
4. Discussion
Early studies of the Job Seekers’ Workshop found higher rates of employment (Hall et al., 1981a, b) and employment/training (Hall et al., 1977) at 3 month follow-up for JSW versus control group participants. In contrast the present study found no group differences for the same outcome measures (see Figure 2). It is notable that absolute rates of job/training program enrollment at 12 week follow-up for current study JSW participants were much lower than those found in studies conducted more than 20 years earlier (Hall et al., 1977, 1981a, b). In fact, both JSW and SC participants in the present study had outcomes comparable to those of earlier control groups. Specifically, only one-fifth (at 12 Weeks) and one-third (at 24 Weeks) of JSW and SC participants were employed (taxed job) or enrolled in training at some point during each period of review. Several study design factors may have contributed to these findings of similar overall low rates of employment in JSW and SC group members.
Figure 2. Employment Outcomes in Three Clinical Trials of Job Seekers’ Workshop.
The figure compares present study (CTN0020) findings to those of three previous studies completed in the 1970s/80s (Hall et al., 1977; Hall et al., 1981a, b).
The x-axis shows each of the 3 earlier studies, followed by the present study. The y-axis denotes percentage of participants achieving specific outcomes. Outcomes varied across studies, with some focused on taxed job/enrollment in job training and others targeting only employment. Solid black bars represent clients in the standard of care (SC, control) group who obtained a taxed job/enrolled in a job training program at 3 mo. follow-up. Solid white bars represent clients in the JSW group who achieved the same criterion.
The dark gray bar denotes clients in SC who obtained a taxed job at 3 mos., and light gray bar denotes this same outcome for JSW group members.
For example, community employment/training agencies will typically not serve persons with less than 6 months of SA treatment in order to ensure their stability and motivation for recovery. In contrast, the present study required that clients have only 30 days in SA treatment prior to enrollment in the clinical trial, and two-thirds of our sample did report < 6 months in SA treatment at enrollment). It is possible that this early treatment group may lack the stability and resources necessary to get and keep a job.
Recent drug use was assessed at baseline but the results were not used to determine study eligibility. Thus, it was notable that over half of participants screened positive for one or more drugs (excluding methadone) at baseline (see Table 1). These data suggest many participants may have been too early in their recovery, with a premature focus on employment and job training. This could explain both lower overall rates of taxed job/training at 12- and 24-Week follow-up, as well as the comparable rates of job acquisition for JSW and SC participants.
A second factor that may have impacted our results was client motivation to a get a new job. During protocol development, counseling staff from participating programs advocated strongly for the inclusion of underemployed patients (those working less than 20 hrs in any week during the 4 weeks prior to study enrollment) in the clinical trial. They stated this was a significant segment of their client base and it was an overlooked group that could benefit from the JSW intervention. Such persons were generally not enrolled in previous JSW studies. Thus, little is known about their motivation to obtain a new or better job and how it might compare with the more traditional unemployed target group. Since the under-employed represented nearly 1/5th of the sample (see Table 1), this could also have reduced rates of new/better job acquisition for both JSW and SC participants.
Moving to study participants unemployed at baseline, “interest in getting a job” was one criterion for study enrollment. Previous studies showed client motivation to work was a significant predictor of employment status at 3-month follow-up (Zanis et al., 2001). Motivation and interest in getting a job is difficult to measure in a reliable and valid way. For the present study, research coordinators encouraged RAs to query clients about their interest and motivation to find work. However, no systematic screening procedures were put in place. In addition, it was stressed to RAs that an adequate recruitment rate must be maintained during the trial. These two methodological challenges may have contributed to less motivated clients entering the study. Further, through study flyers posted at participating treatment sites, clients were aware that monetary compensation was available for research participation. Thus, in some instances, clients may have been motivated to join the study by this immediate earning potential rather than by actually wanting to get a job.
Several of the aforementioned concerns about client motivation to obtain employment are specific to the conduct of a clinical research trial (e.g., payment for study assessments), and would not play a substantive role in clinical practice. Others are relevant to both domains, and suggest promising directions for future research. For example, a reliable and valid measure of client motivation and readiness for work or job training is sorely needed. Dennis and colleagues (1993) developed such a tool for use with methadone maintenance programs. If such a screener could identify clients most likely to benefit from further services (e.g., referral to vocational rehabilitation specialist), it is likely to have both clinical and economic benefits.
In addition, strategies to improve motivation and interest in employment are also needed. It appears some clients feel ambivalent about getting a job, while others may lack confidence or self-efficacy in their ability to find employment. To strengthen client motivation and promote self-efficacy, vocational counselors may benefit from training in Motivational Interviewing (MI). As an evidence-based practice (EBP), MI is well-suited to this goal (Miller and Rollnick, 2001) and is likely to inform future research on barriers to employment as well as ways to address them. Other EBPs, (e.g., Contingency Management (CM) or Motivational Incentives) warrant study as well. Studies of the Therapeutic Workplace (e.g., Silverman et al., 2001) have shown incentives can promote acquisition of job skills while encouraging drug abstinence. Use of incentives to reinforce client attendance of job-focused treatment groups or vocational counseling sessions may also promote self-confidence and strengthen motivation to get a job.
While less likely, it is also possible that enrollment of employment-motivated clients into the control group for the present study could have contributed to our failure to find a difference in employment rates for JSW and SC group members. For example, SC control group participants may have made full use of whatever vocational services were available as part of usual care at their treatment sites. Resources ranged from the vocational brochure handed out as part of the study to availability of a part-time (typically 4–8 hrs/week) on-site vocational case manager. Also, monitoring of job seeking behavior in and of itself may have impacted outcomes for the control group through enhanced awareness and motivation to find work (Clifford et al., 2007; Kyprik, 2007). Finally, some patients faced sanctions if they were unable to get a job through Drug Courts and similar programs, clearly an extraneous motivating influence.
Other factors may have contributed to the lower absolute rates of employment for both JSW and SC group members. First, treatment exposure varied across participants with only 50% completing all 3 JSW sessions and an additional 20% attending 1 or 2 sessions. It will be important in secondary analyses to examine potential relationships between intervention exposure and primary outcomes.
Our national economy can also not be ignored, and may have contributed to study outcomes in several ways. Less favorable economic conditions in the United States, with fewer job opportunities, may have added to the barriers faced by persons with SUDs when seeking employment. Stigma about persons with drug dependence may also have contributed, creating greater reluctance among potential employers to hire those with SUDs. In addition, rates of co-morbid psychopathology in drug dependent persons have increased over time (Hall et al., 2009) and could further limit a participant’s ability to locate and obtain a job.
Strengths of the study, conducted under auspices of the NIDA Clinical Trials Network, included random assignment, rigorous, standardized procedures for research staff training with ongoing quality assurance and involvement of the same workshop facilitators who conducted the original research more than 2 decades ago. Close involvement of the clinical sites in design and implementation of the study was another strength, as it was integral to successful integration of the protocol with ongoing SA treatment. It also guided protocol development, never losing focus on the relevance of study findings to “real life” SA clients.
Despite such strengths, the study also had several weaknesses. For example, a strong focus on clinical relevance and translatability of study findings may have limited other facets of study methods. For example, the decision not to pay study participants for JSW session attendance made it necessary for RAs to focus considerable time and effort on group attendance. Failure to do so could have yielded no JSW-SC differences because too few participants received the minimal dose of JSW necessary for a therapeutic effect.
Other limitations included enrollment of a heterogeneous array of drug abuse clientele who may or may not have been motivated and ready to gain employment, incomplete exposure to the intervention and a primary outcome (obtaining a taxed job) measure that required participants to utilize a number of specific skill sets and behaviors in a coordinated manner. It is possible that JSW, when offered to persons currently in drug abuse treatment and early in their recovery, lacked sufficient potency to achieve JSW and SC differences. It would be important in future studies to test other outcomes such as objective ratings of participant interview skills by mock interviewers blind to participant group assignment. It will also be of considerable interest to examine the data set for subgroups that may have fared particularly well (e.g., those with higher education or a history of employment) or poorly (e.g., those with medical or psychiatric disabilities, criminal histories or social instability) in their job seeking efforts.
In summary, despite a strong focus on intervention fidelity and robust rates of participation in JSW, no intervention-specific effects were found in this contemporary study of the Job Seekers Workshop. Secondary analyses of present study findings will examine potential mediators and moderators of study outcomes, with a focus on barriers to employment and other variables. Also, it is important that we examine the extent to which skill sets of drug users match those advertised in the current job market. In the present study, the majority of jobs obtained during follow-up appeared to fall into the categories of unskilled and semi-skilled. It is important that we gain a better understanding of factors that contributed to the discrepancy between significant positive employment/training outcomes in the 1970s–80s and the lack of JSW and SC group differences in the current. In addition, findings suggest a need to revise study inclusion criteria, concentrating on both client “employability” and a period of success in maintaining drug abstinence prior to study enrollment. Finally, outcome measures in future research should be broadened to include variables that capture progress and improvement in job interview skills and recommended employment seeking behaviors among JSW group participants.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alterman AI, Bovasso GB, Cacciola JS, Mcdermott PA. A comparison of the predictive validity of four sets of baseline ASI summary indices. Psychol Addict. 2001;15:159–162. doi: 10.1037//0893-164x.15.2.159. [DOI] [PubMed] [Google Scholar]
- Alterman AI, Brown LS, Zaballero A, Mckay JR. Interviewer severity ratings and composite scores of the ASI: a further look. Drug Alcohol Depend. 1994;34:201–209. doi: 10.1016/0376-8716(94)90157-0. [DOI] [PubMed] [Google Scholar]
- Caetano R, Schafer J, Cunradi CB. Alcohol-related intimate partner violence among white, black, and Hispanic couples in the United States. Alcohol Res Health. 2001;25:58–65. [PMC free article] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA, Davis CM. Alcohol treatment research assessment exposure subject reactivity effects: part I treatment engagement and involvement. J Stud Alcohol. 2007;68:519–528. doi: 10.15288/jsad.2007.68.519. [DOI] [PubMed] [Google Scholar]
- Comfort M, Kaltenbach K. The psychosocial history: an interview for pregnant and parenting women in substance abuse treatment and research. In: Rahdert ER, editor. Treatment For Drug-Exposed Women And Their Children: Advances In Research Methodology. NIDA Research Monograph 166. NIH Publication No. 96-3632. National Institute on Drug Abuse; Rockville, Maryland: 1996. pp. 133–142. [PubMed] [Google Scholar]
- Comfort M, Zanis DA, Whiteley MJ, Kelly-Tyler A, Kaltenbach KA. Assessing the needs of substance abusing women: psychometric data on the psychosocial history. J Subst Abuse Treat. 1999;17:79–83. doi: 10.1016/s0740-5472(98)00048-8. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Karuntzos GT, McDougal GL, French MT, Hubbard RL. Developing training and employment programs to meet the needs of methadone treatment clients. Eval Program Plann. 1993;16:73–86. doi: 10.1016/0740-5472(92)90022-g. [DOI] [PubMed] [Google Scholar]
- Deren S, Randell J. The vocational rehabilitation of substance abusers. J Appl Rehabil Counsel. 1990;21:4–6. [Google Scholar]
- Dunlap LJ, Zarkin GA, Lennox R, Bray JW. Do treatment services for drug users in outpatient drug free treatment programs affect employment and crime? Subst Use Misuse. 2007;42:1161–1185. doi: 10.1080/10826080701409925. [DOI] [PubMed] [Google Scholar]
- Etheridge RM, Craddock SG, Dunteman GH, Hubbard RL. Treatment services in two national studies of community-based drug abuse treatment programs. J Subst Abuse Treat. 1995;7:9–26. doi: 10.1016/0899-3289(95)90303-8. [DOI] [PubMed] [Google Scholar]
- French MT, Dennis ML, McDougal GL, Karuntzos GT, Hubbard RL. Training and employment programs in methadone treatment. J Subst Abuse Treat. 1992;9:293–303. doi: 10.1016/0740-5472(92)90022-g. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, D’Aunnuo TA, Jin L, Alexander JA. Medical and psychosocial services in drug abuse treatment: do stronger linkages promote client utilization? Health Serv Res. 2000;35:443–465. [PMC free article] [PubMed] [Google Scholar]
- Hall SM, Loeb P, Coyne K, Cooper J. Increasing employment in ex-heroin addicts in criminal justice sample. Behav Ther. 1981a;12:443–452. [Google Scholar]
- Hall SM, Loeb P, LeVois M, Cooper J. Increasing employment in ex-heroin addicts II: methadone maintenance sample. Behav Ther. 1981b;12:453–460. [Google Scholar]
- Hall SM, Loeb P, Norton J. Improving vocational placement in drug treatment clients: a pilot study. Addict Behav. 1977;2:227–234. doi: 10.1016/0306-4603(77)90021-1. [DOI] [PubMed] [Google Scholar]
- Hall W, Degenhardt L, Teeson M. Understanding comorbidity between substance use, anxiety and affective disorders: broadening the research base. Addict Behav. 2009;24:526–530. doi: 10.1016/j.addbeh.2009.03.010. [DOI] [PubMed] [Google Scholar]
- Henderson L, Evans C, Hurley P. Uniform Facility Data Set (UFDS 1997) Office of Applied Studies, Substance Abuse and Mental Health Administration; Rockville, Maryland: 1999. [Google Scholar]
- Jenner M. Harm minimization outcomes for methadone recipients: role of employment. J Subst Misuse. 1998;3:114–118. [Google Scholar]
- Kemp K, Savitz B, Thompson W, Zanis DA. Developing employment services for criminal justice clients enrolled in drug treatment programs. Subst Use Misuse. 2004;39:2491–2511. doi: 10.1081/ja-200034691. [DOI] [PubMed] [Google Scholar]
- Kerrigan AJ, Kaugh JE, Wilson BL, Wilson JV, Boering JA, Monger TN. Vocational rehabilitation outcomes of veterans with substance use disorders in a partial hospitalization program. Psychiatr Serv. 2000;51:1570–1572. doi: 10.1176/appi.ps.51.12.1570. [DOI] [PubMed] [Google Scholar]
- Kidorf M, Neufeld K, Brooner RK. Combining stepped-care approaches with behavioral reinforcement to motivate employment in opioid-dependent outpatients. Subst Use Misuse. 2004;39:2215–2238. doi: 10.1081/ja-200034591. [DOI] [PubMed] [Google Scholar]
- Kidorf M, Stitzer ML, Brooner RK. Characteristics of methadone patients responding to take-home incentives. Behav Ther. 1994;25:109–121. [Google Scholar]
- Kingree JB. The role of vocational behaviors preceding and during 12-step oriented treatment. J Subst Abuse Treat. 1997;14:575–580. doi: 10.1016/s0740-5472(97)00177-3. [DOI] [PubMed] [Google Scholar]
- Koo DJ, Chitwood DD, Sanchez J. Factors for employment: a case control study of fully employed and unemployed heroin users. Subst Use Misuse. 2007;42:1035–1054. doi: 10.1080/10826080701409404. [DOI] [PubMed] [Google Scholar]
- Kyprik K. Methodological issues in alcohol screening and brief intervention research, Subst. Abuse. 2007;28:31–42. doi: 10.1300/J465v28n03_04. [DOI] [PubMed] [Google Scholar]
- Lee MT, Reif S, Ritter GA, Levine HJ, Horgan CM. Access to services in the substance abuse treatment system: variations by facility characteristics. In: Galanter M, editor. Recent Developments in Alcoholism, Services Research in the Era of Managed Care. Vol. 15. Plenum Publishing; New York: 2001. pp. 137–156. [DOI] [PubMed] [Google Scholar]
- McCoy CB, Comerford M, Metsch LR. Employment among chronic drug users at baseline and 6 month follow-up. Subst Use Misuse. 2007;42:1055–1067. doi: 10.1080/10826080701409982. [DOI] [PubMed] [Google Scholar]
- McLellan AT. DHHS Publication No ADM 87-1281. US Government Printing Office; Washington, D.C: 1983. Patient Characteristics Associated with Outcome. Research on the Treatment of Narcotic Addiction; pp. 500–540. [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients. The Addiction Severity Index. J Nerv Ment Dis. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Cacciola J, Carise D, Coyne TH. Clinical Training Version. Treatment Research Institute; Philadelphia: 1999. Addiction Severity Index-Lite. [Google Scholar]
- Miller WR, Rollnick SP. Motivational Interviewing: Preparing people for change. 2. The Guilford Press; New York, NY: 2001. [Google Scholar]
- Platt JJ. Vocational rehabilitation of drug abusers. Psychol Bull. 1995;117:416–433. doi: 10.1037/0033-2909.117.3.416. [DOI] [PubMed] [Google Scholar]
- Reif S, Horgan CM, Ritter GA, Tompkins CP. The impact of employment counseling on substance user treatment participation and outcomes. Subst Use Misuse. 2004;39:2391–2424. doi: 10.1081/ja-200034661. [DOI] [PubMed] [Google Scholar]
- Rosenheck R, Seibyl CL. Effectiveness of treatment elements in a residential-work therapy program for veterans with severe substance abuse. Psychiatr Serv. 1997;48:928–935. doi: 10.1176/ps.48.7.928. [DOI] [PubMed] [Google Scholar]
- Schulz KF, Altman DG, Moher D for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010:152. [PMC free article] [PubMed] [Google Scholar]
- Shepard DS, Reif S. The value of vocational rehabilitation in substance user treatment: a cost-effectiveness framework. Subst Use Misuse. 2004;39:2581–2609. doi: 10.1081/ja-200034732. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Rowan-Szal GA, Greener JM. Drug abuse treatment process components that improve retention. J Subst Abuse Treat. 1997;14:565–572. doi: 10.1016/s0740-5472(97)00181-5. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Brown J, Leo GI, Sobell MB. The reliability of the alcohol Timeline Follow Back when administered by telephone and by computer. Drug Alcohol Depend. 1996;42:49–54. doi: 10.1016/0376-8716(96)01263-x. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow Back: A Calendar Method for Assessing Alcohol and Drug Use (User’s Guide) Addiction Research Foundation; Toronto, Canada: 1996. [Google Scholar]
- Sorensen JL, Hall SM, Loeb P, Allen T, Glaser EM, Greenberg PD. Dissemination of a job seekers’ workshop to drug treatment programs. Behav Ther. 1988;19:143–155. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The DASIS Report: Employment Status and Substance Abuse Treatment Admissions: 2006. Office of Applied Studies; Rockville, MD: 2008. [Google Scholar]
- TOPPS II. Drug treatment completion and post-discharge employment in the TOPPS-II Interstate Cooperative Study. J Subst Abuse Treat. 2003;25:9–18. doi: 10.1016/s0740-5472(03)00050-3. [DOI] [PubMed] [Google Scholar]
- Valliant GE. What can long-term follow-up teach us about relapse and prevention of relapse in addiction? Br J Addict. 1988;83:1147–1157. doi: 10.1111/j.1360-0443.1988.tb03021.x. [DOI] [PubMed] [Google Scholar]
- Wilkinson GS. The Wide Range Achievement Test: Manual. 3. Wide Range; Wilmington, Delaware: 1993. [Google Scholar]
- Wong CJ, Silverman K. Establishing and maintaining job skills and professional behaviors in chronically unemployed drug users. Subst Use Misuse. 2007;34:1127–1140. doi: 10.1080/10826080701407952. [DOI] [PubMed] [Google Scholar]
- World Health Organization. International Classification of Diseases. 10. Geneva, Switzerland: 1992. rev. [Google Scholar]
- Young NK. DHHS publication No (SMA) 00-3470. US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Centers for Substance Abuse Treatment; Rockville, Maryland: 2000. TIP 38: Integrating Substance Abuse Treatment and Vocational Services. [PubMed] [Google Scholar]
- Zanis DA, Metzger DS, McLellan AT. Factors associated with employment among methadone patients. Subst Abuse Treat. 1994;11:443–447. doi: 10.1016/0740-5472(94)90097-3. [DOI] [PubMed] [Google Scholar]
- Zanis DA, Coviello D, Alterman AI, Appling SE. A community-based trial of problem-solving to increase employment among methadone patients. J Subst Abuse Treat. 2001;21:19–26. doi: 10.1016/s0740-5472(01)00177-5. [DOI] [PubMed] [Google Scholar]