Abstract
Muscle weakness may contribute to crouch gait in individuals with cerebral palsy, and some individuals participate in strength training programs to improve crouch gait. Unfortunately, improvements in muscle strength and gait are inconsistent after completing strength training programs. The purpose of this study was to examine changes in knee extensor strength and knee extension angle during walking after strength training in individuals with cerebral palsy who walk in crouch gait and to determine subject characteristics associated with these changes. A literature review was performed of studies published since January 2000 that included strength training, three-dimensional motion analysis, and knee extensor strength measurements for individuals with cerebral palsy. Three studies met these criteria and individual subject data was obtained from the authors for thirty crouch gait subjects. Univariate regression analyses were performed to determine which of ten physical examination and motor performance variables were associated with changes in strength and knee extension during gait. Change in knee extensor strength ranged from a 25% decrease to a 215% increase, and change in minimum knee flexion angle during gait ranged from an improvement of 9° more knee extension to 15° more knee flexion. Individuals without hamstring spasticity had greater improvement in knee extension after strength training. Hamstring spasticity was associated with an undesired increase in knee flexion during walking. Subject-specific factors such as hamstring spasticity may be useful for predicting which subjects will benefit from strength training to improve crouch gait.
Keywords: cerebral palsy, strength training, crouch gait, spasticity
1. Introduction
Crouch gait, a common movement pattern in individuals with cerebral palsy, is characterized by excessive knee flexion during the stance-phase of gait. There are several proposed causes of crouch gait, including contracted hamstrings, weak ankle plantarflexors, contracted hip flexors, impaired balance, general muscle weakness, and foot malalignment [1]. If left untreated, crouch gait can lead to joint pain [2], bone deformities [3], and walking limitations [4,5]. Treatment of crouch gait frequently involves orthopedic surgery. Surgery can be effective in reducing excessive knee flexion, correcting bony deformities, and improving walking ability [6]. However, surgery does not correct underlying muscle weakness.
Weakness of the extensor muscles in the lower extremity is present in many individuals with cerebral palsy [7,8]. Weakness in individuals with a crouch gait could compromise their ability to generate the muscle forces required to produce an upright gait pattern. Muscles such as the gluteus maximus, vasti, gastrocnemius, and soleus are major contributors to supporting body-weight during crouch gait [9]; therefore, strengthening these muscles could potentially improve an individual's ability to walk in a more upright posture.
There is conflicting evidence on the efficacy of strength training in cerebral palsy. Individuals with cerebral palsy can gain muscle strength after participation in strength training programs [10,11], but the functional changes after a strength training program are variable. Damiano et al. [12] observed improvement in knee extension at initial contact during walking and increased stride length after strength training, and Blundell et al. and Dodd et al. [13,14] demonstrated an improvement in functional tests after strength training. Other studies have not found significant changes in functional tests [15,16], or observed increased knee flexion during gait in some subjects after strength training [17]. There is a lack of consensus regarding the efficacy of strength training in individuals with cerebral palsy [18-21], and it is unclear which muscles should be strengthened in order to improve crouch gait.
It is challenging to characterize the efficacy of strength training programs in individuals with cerebral palsy because most studies include individuals with different gait patterns and levels of impairment. Furthermore, most studies only report average changes and do not document individual outcomes. This makes it difficult to understand the variability in outcomes between subjects and confounds efforts to determine which subjects benefit from strength training. Individuals with cerebral palsy represent a heterogeneous population. Strengthening may not be effective in all individuals with crouch gait, and a better understanding of the characteristics associated with improved strength and function following strength training is needed.
The goals of this study were to: (1) examine the variability in outcomes after progressive resistance strength training for individuals with cerebral palsy who walk in a crouch gait, and (2) identify the subject characteristics associated with gains in strength and improved knee extension during gait after strength training. To achieve this goal a literature search was performed for studies that combined three-dimensional motion analysis and a progressive resistance strength training program for subjects with crouch gait. Data from studies that met these criteria [17,22,23] were used to create a database of strength measurements and walking kinematics before and after strength training. Regression analyses were performed to identify characteristics associated with gains in strength and improvement in knee extension.
2. Methods
To investigate the effects of strength training in individuals with cerebral palsy who walk with a crouch gait, a literature search was performed for studies published since January 2000 that included (1) a progressive resistance strength training program, (2) a three-dimensional motion analysis before and after strength training, and (3) a goal of improved knee extension for individuals who walked in a crouch gait. The time period was chosen to increase the likelihood that individual data not included in the manuscript would be retrievable. PubMED was used as the search database in addition to scanning reference lists. A combination of the following search terms was used: cerebral palsy AND strength AND (training OR program). 58 articles were identified in the initial literature search that had been published since January 2000 (Supplementary Fig. 1). Of these articles, 32 were review articles, post-operative rehabilitation programs, or not strength training programs for individuals with cerebral palsy. Additionally, 23 articles were excluded that did not include three-dimensional motion analysis, knee extensor strength measurements, or a progressive resistance strength training protocol.
Three studies [17,22,23] were identified that met all criteria (Table 1). The first authors were contacted and agreed to collaborate in this study. Subject information, physical exam measures, muscle strength data, and gait kinematics were collected for all subjects in each study. All studies were performed according to the human subject research requirement at their respective institutions. All data shared as part of this analysis was de-identified.
Table 1.
Summary of crouch subjects and training programs for all studies
| Study | Number of crouch subjects | Age (yrs) | Height (cm) | Weight (kg) | Training Program |
|---|---|---|---|---|---|
| Damiano (2009) | 7 | 8.1 ± 2.6 | 118 ± 13 | 20.5 ± 4.8 | 8 weeks (3 times/week) Progressive resistance with weight machines & cuffs Targeted hip and knee extensors |
| Unger (2006) | 17 | 16.2 ± 1.4 | 158 ± 12 | 51.5 ± 9.5 | 8 weeks (1-3 times/week) Progressive resistance with weights & resistance bands Full body |
| Eek (2006) | 6 | 12.4 ± 1.6 | 145 ± 9 | 40.5 ± 9.2 | 8 weeks (3 times/week) Progressive resistance with weights & resistance bands Targeted 4 muscle groups per child |
| Total | 30 | 13.7 ± 3.8 | 147 ± 20 | 42.4 ± 15.2 | |
2.1 Subject Selection
Individuals who walked in a crouch gait pattern were selected from each study. Crouch gait was defined as a minimum knee flexion angle greater than 10° during stance. Thirty subjects met this criterion and were included in the study (Table 1). The subjects included 14 who had a mild crouch with a minimum knee flexion angle less than 20°, 12 who had a moderate crouch gait with a minimum knee flexion angle between 20° and 30°, and 3 who had a minimum knee flexion angle greater than 30°. The average minimum knee flexion angle during stance was 20°. GMFCS levels were available for two of the studies [17,22] and the crouch gait subjects included 3 GMFCS Level I, 6 GMFCS Level II, and 4 GMFCS Level III. All studies excluded subjects that had surgery within 12 months prior to the study.
2.2 Strength Training Programs
The studies consisted of 8-week progressive resistance strength training programs, including both home and therapist-supervised training sessions, and targeted a range of muscle groups. The subjects in the program reported by Damiano et al. [17] were younger than the other two studies and participated in a program targeting the hip and knee extensors in therapist-supervised sessions three times per week. Unger et al. [23] organized a school-based circuit strength training program that subjects completed one to three times per week. Eek et al. [22] designed individualized strength training programs that targeted four lower-extremity muscle groups that subjects completed three times per week (twice at home and once at a physiotherapy clinic). Detailed information on each study is provided in the original publications.
2.3 Outcomes Measures
Since the focus of this study was on individuals with a crouch gait, change in knee extensor strength and change in minimum knee flexion angle during stance after strength training were examined. Knee extensor strength was measured using an isokinetic strength assessment at 30°/s [17] or an isometric strength assessment using a dynamometer [22,23]. Change in knee extensor strength was calculated as the percent change in maximum knee extensor torque after strength training. Change in minimum knee flexion angle was calculated from kinematics obtained from three-dimensional motion analysis.
2.4 Subject-Specific Characteristics
Ten subject characteristics were selected based upon literature and clinical experience that could be associated with changes in knee extensor strength and knee extension during gait. These included: (1) hamstring spasticity, (2) popliteal angle, (3) knee flexion at initial contact, (4) minimum knee flexion angle during stance, (5) quadriceps strength, (6) age, (7) height, (8) weight, (9) walking speed, and (10) Gross Motor Function Classification System (GMFCS) level. All characteristics were measured before the strength training program.
Hamstring spasticity, popliteal angle, and GMFCS level were only available for the subjects in studies by Damiano et al. [17] and Eek et al. [22]. Hamstring spasticity was included as a binary variable with an Ashworth score ≥ 2 indicating hamstring spasticity.
2.5 Regression Analyses
Univariate linear regression analyses were performed between each of the 10 subject-specific characteristics and the two outcome measures, (1) change in knee extensor strength and (2) change in minimum knee flexion angle during stance, to determine which characteristics had the strongest association with each outcome measure. A random effect term for “study” was also included in each model to account for between-study variation [24]. No corrections were made for multiple comparisons [25]. To compare the relative effects of the characteristics, we performed a multivariate linear regression analysis that included all the characteristics with a significant association for each outcome measure (p < 0.05). Significant associations were also checked for confounding effects of age, height, and weight. All statistics were performed using R, a statistical analysis package (www.r-project.org/index.html).
3. Results
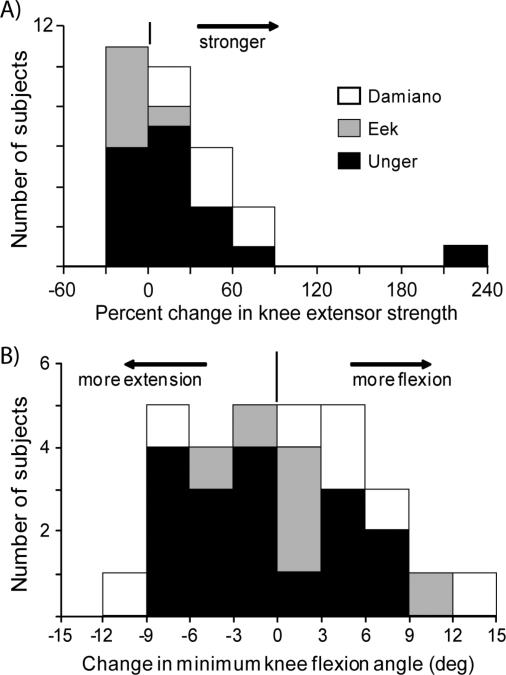
The 30 crouch gait subjects had variable changes in knee extensor strength and minimum knee flexion angle during gait after completing a strength training program. The average change in knee extensor strength was a 23% increase; however, the range varied from a 25% decrease to a 215% increase (Fig. 1A). The average change in minimum knee flexion angle after strength training for the group was 0°; however, the range varied from an improvement of 9° more knee extension to a deterioration of 15° more knee flexion (Fig. 1B).
Figure 1.
Histograms of (A) percent change in knee extensor strength and (B) change in minimum knee flexion angle during gait after completing a strength training program. Subjects from each of the three studies are shown separately – Damiano (white), Eek (gray), and Unger (black). A negative change in minimum knee flexion angle indicates a more upright posture, or a positive outcome, after strength training. Note that in all three studies the outcomes were variable between subjects.
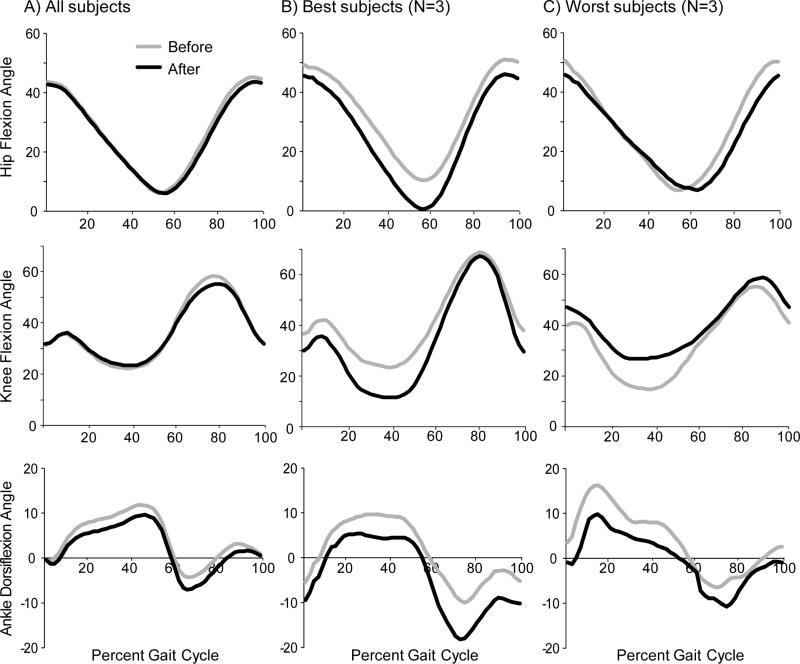
Although the average knee kinematics of the group suggest that the strength training program had no effect on knee kinematics (Fig. 2A), examining the changes in knee flexion for the subjects with the best and worst outcomes demonstrates that some subjects had substantial improvements (Fig. 2B), while others had deterioration after completing the strength training program (Fig. 2C). For example, the top ten percent of subjects had an average improvement of 9° more knee extension during stance, whereas the bottom ten percent of subjects, with the greatest increase in minimum knee flexion, had an average change of 10° more knee flexion. After the strength training program, the subjects with the best outcomes achieved knee extension within normal limits in late stance.
Figure 2.
Average hip, knee, and ankle flexion angles for (A) all subjects, (B) the three subjects with the largest increase in knee extension (best outcomes), and (C) the three subjects with the largest increase in knee flexion (worst outcomes) before and after completing strength training program. Note that although there was no significant change in knee flexion for the group as a whole, there were subsets of subjects with significant positive and negative changes.
There was a significant association between change in minimum knee flexion angle and change in minimum hip flexion angle (slope = 0.59, p = 0.001), suggesting that individuals with improved knee extension also had improved hip extension after strength training. There was no association between change in knee flexion angle and change in maximum dorsiflexion angle during stance. Average hip flexion angle and ankle dorsiflexion angle did not change significantly after strength training for the group (Fig. 2A), but the inter-subject variability was similar to the variability in change in knee flexion angle.
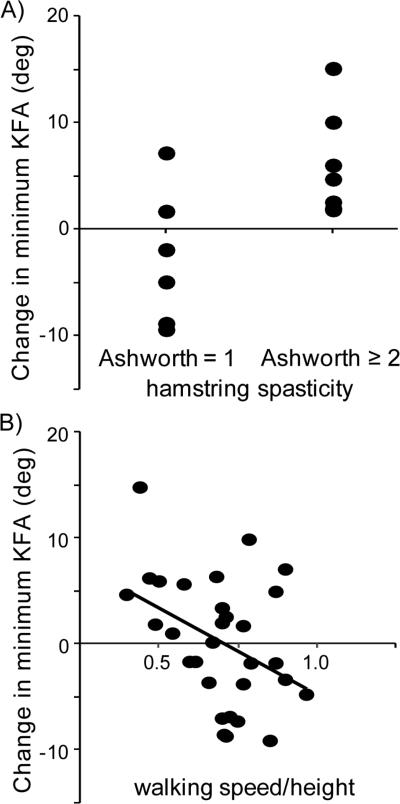
Hamstring spasticity was associated with change in minimum knee flexion angle after strength training (Table 2). No subject with an Ashworth Score ≥ 2 had an improvement in knee flexion angle after strength training (Fig. 3A). Individuals with a hamstring Ashworth score of 1 had an average improvement of 3° more knee extension, and 4 out of 6 of these subjects showed improved knee extension after the strength training program. The association between hamstring spasticity and change in knee flexion angle was maintained after controlling for age, height, and weight. Walking speed recorded before the strength training program was also associated with change in minimum knee flexion angle (p = 0.03); individuals who walked faster were more likely to have improved knee extension after the strength training program (Fig. 3B). However, when included in a multi-regression analysis with hamstring spasticity, walking speed did not add additional information to the model and was no longer significant. Walking speed was correlated with hamstring spasticity (r2 = -0.55), indicating that individuals with hamstring spasticity tended to walk slower.
Table 2.
Results of regression analyses
|
Kinematics: Change in min knee flexion angle (KFA) |
Strength: Change in knee extensor strength |
||||||
|---|---|---|---|---|---|---|---|
| Coeff | S.E. | p-value | p-adj** | Coeff | S.E. | p-value | |
| Hamstring spasticity* | 8.51 | 3.06 | 0.02 | 0.006 | 0.13 | 0.1 | 0.21 |
| Popliteal angle* (deg) | -0.14 | 0.15 | 0.36 | -0.01 | 0.005 | 0.11 | |
| KFA at initial contact (deg) | 0.12 | 0.08 | 0.12 | 0.005 | 0.006 | 0.43 | |
| Min KFA (deg) | -0.05 | 0.12 | 0.66 | -0.002 | 0.01 | 0.77 | |
| Knee extensor strength (Nm/kg) | 6.43 | 21.2 | 0.76 | -2.83 | 0.79 | 0.11 | |
| Age (yr) | -0.35 | 0.28 | 0.22 | -0.02 | 0.03 | 0.45 | |
| Height (cm) | -0.08 | 0.05 | 0.13 | < 0.001 | < 0.001 | 0.99 | |
| Weight (kg) | -0.07 | 0.07 | 0.35 | < 0.002 | 0.01 | 0.52 | |
| Walking speed/height (s-1) | -16.7 | 6.95 | 0.02 | 0.02 | 0.01 | 0.57 | 0.99 |
| GMFCS level* | 2.51 | 2.62 | 0.36 | 0.03 | 0.13 | 0.79 | |
p < 0.05
Each regression analysis included a random effects term, “study,” as a covariate.
Coeff, Regression coefficient; S.E., Standard Error; GMFCS, Gross Motor Function Classification System
Data available for subjects from studies by Damiano and Eek
Adjusted for age, height, and weight
Figure 3.
Hamstring spasticity (A) and walking speed (B) were associated with change in minimum knee flexion angle (KFA) during stance with a p-value < 0.05.
There were no significant associations between the subject characteristics and percent change in knee extensor strength (Table 2). There was also no relationship between the change in minimum knee flexion angle and change in knee extensor strength (R2 = 0.0).
4. Discussion
Individuals with cerebral palsy who walk in a crouch gait have inconsistent outcomes after strength training. Although the majority of subjects had an increase in knee extensor strength, the change in knee extension during gait was variable. Some individuals had an improvement in knee extension during gait that was comparable to outcomes after orthopedic surgery [26]; however, other subjects with crouch gait walked with greater knee flexion after strength training. Determining which subjects will improve knee extension after strength training is necessary to determine who should participate in these programs.
Hamstring spasticity was associated with more knee flexion after strength training. Strength training in subjects with hamstring spasticity to improve crouch gait is not supported by this analysis. However, from the small sample included in this study, it does not appear that strength training exacerbated spasticity. The Ashworth score for the hamstrings changed for only two subjects after strength training; one subject had a lower Ashworth score and another had a higher Ashworth score. The association between hamstring spasticity and increased knee flexion after strength training may be a result of increased muscle strength amplifying the effects of excessive muscle activity during gait. Future studies should incorporate more quantitative spasticity measurements and evaluate spasticity of multiple muscle groups before and after strength training.
No significant associations were found between the subject characteristics and change in quadriceps strength. The lack of associations may be confounded by the different methods used for measuring knee extensor strength between studies. Not all subjects included in this analysis increased quadriceps strength after completing a strength training program; therefore, future studies to explain the variability in changes in strength between subjects would be valuable. Other factors such as selective motor control, hip range of motion, or rotational deformities may contribute to variability in change in knee extensor strength.
The change in knee flexion angle after strength training was significantly correlated with change in hip flexion angle but not with change in ankle dorsiflexion angle. The individuals included in this study walked with varying degrees of ankle dorsiflexion during stance, which likely contributed to the lack of correlation between change in knee and ankle angle. Eight of the thirty individuals included in this study had a maximum ankle dorsiflexion angle during stance of less than 5 degrees. Testing to see if the outcomes or regression models were different for those individuals who walked with reduced dorsiflexion during stance showed no significant differences. Future studies that examine differences between subgroups of crouch gait could further improve the ability of clinicians to determine optimal treatment for each subject.
Strength training programs designed for individuals who walk in a crouch gait, including those in this analysis, have focused on strengthening the hip and knee extensors. However, weakness of these muscle groups may not be a primary cause of crouch gait. During normal gait, the vasti and gluteus maximus support the body weight in early stance and the ankle plantarflexors support the body weight in terminal stance [27]. In crouch gait, the knee extensor moment during stance is larger, which requires higher forces to be generated by the knee extensors. These larger loads may lead to patellar fracture or patella alta [28-30]. Since walking in an erect gait requires less strength than walking in crouch gait, strengthening of the knee extensors may not correct crouch gait in some subjects.
In contrast, ankle plantarflexor weakness is commonly cited as a potential cause of crouch gait [1]. Engsberg et al. (2006) examined the effects of strengthening the ankle plantarflexors and reported an improvement in knee flexion during stance, although the study was not specific to individuals with crouch gait [31]. Identifying the primary cause of crouch gait in each individual would improve the ability of clinicians to target the correct muscles for strength training programs or other treatment strategies.
The limited number of subjects and combination of outcomes from three centers limits the power of this analysis. No corrections were made for multiple comparisons, which increases the probability of Type I errors in this statistical analysis. This analysis also combined data from three independent studies performed according to different protocols at different institutions. The change in knee flexion angle and percent change in knee extensor strength were similar in magnitude at all three institutions, and all three studies had variable outcomes between subjects. The limited number of subjects also limited the number of subject characteristics that could be included in this analysis. Additionally, other factors that were not included in the original studies, such as selective motor control, range of motion, and spasticity in other muscle groups, could be important predictors of outcomes after strength training. There may also be benefits of strength training programs that are not captured by the outcome measures included in this analysis, such as increased physical activity, improved cardiovascular health, and enhanced self-image [32]. The Ashworth score was used by the studies included in this analysis to measure hamstring spasticity; however, more quantitative measures of spasticity are desirable. Due to these limitations, future studies are required to test the generalizability of the results.
The goal of strength training studies in individuals with cerebral palsy should be to identify those subjects with the greatest likelihood for a positive outcome. Some subjects benefit from progressive resistance strength training, but it is unlikely that strengthening is the ideal therapy for all subjects. Methods that determine which subjects are unlikely to respond well can save resources of patients, clinicians, and caregivers. Understanding how characteristics such as spasticity and changes in muscle strength affect functional outcomes are important areas for future research to inform the design of optimal, subject-specific treatments.
Supplementary Material
Acknowledgements
This work was supported by NIH grant R01 HD033929, NIH grant U54GM072970, the NIH National Center for Simulation in Rehabilitation Research (NCSRR) R24 HD065690, the intramural research program of the NIH Clinical Center, and an NSF Graduate Research Fellowship.
Footnotes
Conflict of interest statement
None of the authors had any financial or personal conflict of interest with regard to this study.
References
- 1.Gage JR. Surgical treatment of knee dysfunction in cerebral palsy. Clin Orthop Relat Res. 1990;253:45–54. [PubMed] [Google Scholar]
- 2.Jahnsen R, Villien L, Aamodt G, Stanghelle JK, Holm I. Musculoskeletal pain in adults with cerebral palsy compared with the general population. J Rehabil Med. 2004;36(2):78–84. doi: 10.1080/16501970310018305. [DOI] [PubMed] [Google Scholar]
- 3.Graham H, Selber P. Musculoskeletal aspects of cerebral palsy. Journal of Bone & Joint Surgery, British Volume. 2003;85(2):157–166. doi: 10.1302/0301-620x.85b2.14066. [DOI] [PubMed] [Google Scholar]
- 4.Johnson DC, Damiano DL, Abel MF. The evolution of gait in childhood and adolescent cerebral palsy. J Pediatr Orthop. 1997;17(3):392–396. [PubMed] [Google Scholar]
- 5.Opheim A, Jahnsen R, Olsson E, Stanghelle JK. Walking function, pain, and fatigue in adults with cerebral palsy: a 7-year follow-up study. Dev Med Child Neurol. 2009;51(5):381–388. doi: 10.1111/j.1469-8749.2008.03250.x. [DOI] [PubMed] [Google Scholar]
- 6.Rodda JM, Graham HK, Nattrass GR, Galea MP, Baker R, Wolfe R. Correction of severe crouch gait in patients with spastic diplegia with use of multilevel orthopaedic surgery. J Bone Joint Surg Am. 2006;88(12):2653–2664. doi: 10.2106/JBJS.E.00993. [DOI] [PubMed] [Google Scholar]
- 7.Damiano DL, Vaughan CL, Abel MF. Muscle response to heavy resistance exercise in children with spastic cerebral palsy. Dev Med Child Neurol. 1995;37(8):731–739. doi: 10.1111/j.1469-8749.1995.tb15019.x. [DOI] [PubMed] [Google Scholar]
- 8.Wiley ME, Damiano DL. Lower-extremity strength profiles in spastic cerebral palsy. Dev Med Child Neurol. 1998;40(2):100–107. doi: 10.1111/j.1469-8749.1998.tb15369.x. [DOI] [PubMed] [Google Scholar]
- 9.Steele KM, Seth A, Hicks JL, Schwartz MS, Delp SL. Muscle contributions to support and progression during single-limb stance in crouch gait. J Biomech. 2010;43(11):2099–2105. doi: 10.1016/j.jbiomech.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Healy A. 2 Methods of Weight-Training for Children with Spastic Type of Cerebral-Palsy. Research Quarterly. 1958;29(4):389–395. [Google Scholar]
- 11.McCubbin J, Shasby G. Effects of isokinetic exercise on adolescents with cerebral palsy. Adapted Physical Activity Quarterly. 1985;2:56–64. [Google Scholar]
- 12.Damiano DL, Kelly LE, Vaughn CL. Effects of quadriceps femoris muscle strengthening on crouch gait in children with spastic diplegia. Physical therapy. 1995;75(8):658–667. doi: 10.1093/ptj/75.8.658. discussion 668-671. [DOI] [PubMed] [Google Scholar]
- 13.Blundell SW, Shepherd RB, Dean CM, Adams RD, Cahill BM. Functional strength training in cerebral palsy: a pilot study of a group circuit training class for children aged 4-8 years. Clin Rehabil. 2003;17(1):48–57. doi: 10.1191/0269215503cr584oa. [DOI] [PubMed] [Google Scholar]
- 14.Dodd KJ, Taylor NF, Graham HK. A randomized clinical trial of strength training in young people with cerebral palsy. Dev Med Child Neurol. 2003;45(10):652–657. doi: 10.1017/s0012162203001221. [DOI] [PubMed] [Google Scholar]
- 15.Kerr C, McDowell B, Cosgrove A, Walsh D, Bradbury I, McDonough S. Electrical stimulation in cerebral palsy: a randomized controlled trial. Dev Med Child Neurol. 2006;48(11):870–876. doi: 10.1017/S0012162206001915. [DOI] [PubMed] [Google Scholar]
- 16.Liao HF, Liu YC, Liu WY, Lin YT. Effectiveness of loaded sit-to-stand resistance exercise for children with mild spastic diplegia: a randomized clinical trial. Arch Phys Med Rehabil. 2007;88(1):25–31. doi: 10.1016/j.apmr.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Damiano DL, Arnold AS, Steele KM, Delp SL. Can strength training predictably improve gait kinematics? A pilot study on the effects of hip and knee extensor strengthening on lower-extremity alignment in cerebral palsy. Physical therapy. 2010;90(2):269–279. doi: 10.2522/ptj.20090062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dodd KJ, Taylor NF, Damiano DL. A systematic review of the effectiveness of strength-training programs for people with cerebral palsy. Arch Phys Med Rehabil. 2002;83(8):1157–1164. doi: 10.1053/apmr.2002.34286. [DOI] [PubMed] [Google Scholar]
- 19.Mockford M, Caulton JM. Systematic review of progressive strength training in children and adolescents with cerebral palsy who are ambulatory. Pediatr Phys Ther. 2008;20(4):318–333. doi: 10.1097/PEP.0b013e31818b7ccd. [DOI] [PubMed] [Google Scholar]
- 20.Scianni A, Butler JM, Ada L, Teixeira-Salmela LF. Muscle strengthening is not effective in children and adolescents with cerebral palsy: a systematic review. Aust J Physiother. 2009;55(2):81–87. doi: 10.1016/s0004-9514(09)70037-6. [DOI] [PubMed] [Google Scholar]
- 21.Scholtes VA, Dallmeijer AJ, Rameckers EA, Verschuren O, Tempelaars E, Hensen M, Becher JG. Lower limb strength training in children with cerebral palsy--a randomized controlled trial protocol for functional strength training based on progressive resistance exercise principles. BMC Pediatr. 2008;8(41) doi: 10.1186/1471-2431-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eek MN, Tranberg R, Zugner R, Alkema K, Beckung E. Muscle strength training to improve gait function in children with cerebral palsy. Dev Med Child Neurol. 2008;50(10):759–764. doi: 10.1111/j.1469-8749.2008.03045.x. [DOI] [PubMed] [Google Scholar]
- 23.Unger M, Faure M, Frieg A. Strength training in adolescent learners with cerebral palsy: a randomized controlled trial. Clin Rehabil. 2006;20(6):469–477. doi: 10.1191/0269215506cr961oa. [DOI] [PubMed] [Google Scholar]
- 24.Pinheiro JC, Bates DM. Mixed-effects models in S and S-PLUS. Springer Verlag; 2009. [Google Scholar]
- 25.Rothman KJ. No adjustments are needed for multiple testing. Epidemiology. 1990;1(1):43–46. [PubMed] [Google Scholar]
- 26.Adolfsen SE, Ounpuu S, Bell KJ, DeLuca PA. Kinematic and kinetic outcomes after identical multilevel soft tissue surgery in children with cerebral palsy. J Pediatr Orthop. 2007;27(6):658–667. doi: 10.1097/BPO.0b013e3180dca114. [DOI] [PubMed] [Google Scholar]
- 27.Liu MQ, Anderson FC, Schwartz MH, Delp SL. Muscle contributions to support and progression over a range of walking speeds. J Biomech. 2008;41(15):3243–3252. doi: 10.1016/j.jbiomech.2008.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murphy KP. Cerebral palsy lifetime care - four musculoskeletal conditions. Dev Med Child Neurol. 2009;51(Suppl 4):30–37. doi: 10.1111/j.1469-8749.2009.03431.x. [DOI] [PubMed] [Google Scholar]
- 29.O'Sullivan R, Walsh M, Kiernan D, O'Brien T. The knee kinematic pattern associated with disruption of the knee extensor mechanism in ambulant patients with diplegic cerebral palsy. Clin Anat. 23(5):586–592. doi: 10.1002/ca.20976. [DOI] [PubMed] [Google Scholar]
- 30.Rosenthal RK, Levine DB. Fragmentation of the distal pole of the patella in spastic cerebral palsy. J Bone Joint Surg Am. 1977;59(7):934–939. [PubMed] [Google Scholar]
- 31.Engsberg JR, Ross SA, Collins DR. Increasing ankle strength to improve gait and function in children with cerebral palsy: a pilot study. Pediatr Phys Ther. 2006;18(4):266–275. doi: 10.1097/01.pep.0000233023.33383.2b. [DOI] [PubMed] [Google Scholar]
- 32.Faigenbaum AD, Kraemer WJ, Blimkie CJ, Jeffreys I, Micheli LJ, Nitka M, Rowland TW. Youth resistance training: updated position statement paper from the national strength and conditioning association. J Strength Cond Res. 2009;23(5 Suppl):S60–79. doi: 10.1519/JSC.0b013e31819df407. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.