ABSTRACT
BACKGROUND
Lowering hospital readmission rates has become a primary target for the Centers for Medicare & Medicaid Services, but studies of the relationship between adherence to the recommended hospital care processes and readmission rates have provided inconsistent and inconclusive results.
OBJECTIVE
To examine the association between hospital performance on Medicare’s Hospital Compare process quality measures and 30-day readmission rates for patients with acute myocardial infarction (AMI), heart failure and pneumonia, and for those undergoing major surgery.
DESIGN, SETTING AND PARTICIPANTS
We assessed hospital performance on process measures using the 2007 Hospital Inpatient Quality Reporting Program. The process measures for each condition were aggregated in two separate measures: Overall Measure (OM) and Appropriate Care Measure (ACM) scores. Readmission rates were calculated using Medicare claims.
MAIN OUTCOME MEASURE
Risk-standardized 30-day all-cause readmission rate was calculated as the ratio of predicted to expected rate standardized by the overall mean readmission rate. We calculated predicted readmission rate using hierarchical generalized linear models and adjusting for patient-level factors.
RESULTS
Among patients aged ≥ 66 years, the median OM score ranged from 79.4 % for abdominal surgery to 95.7 % for AMI, and the median ACM scores ranged from 45.8 % for abdominal surgery to 87.9 % for AMI. We observed a statistically significant, but weak, correlation between performance scores and readmission rates for pneumonia (correlation coefficient R = 0.07), AMI (R = 0.10), and orthopedic surgery (R = 0.06). The difference in the mean readmission rate between hospitals in the 1st and 4th quartiles of process measure performance was statistically significant only for AMI (0.25 percentage points) and pneumonia (0.31 percentage points). Performance on process measures explained less than 1 % of hospital-level variation in readmission rates.
CONCLUSIONS
Hospitals with greater adherence to recommended care processes did not achieve meaningfully better 30-day hospital readmission rates compared to those with lower levels of performance.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-012-2229-8) contains supplementary material, which is available to authorized users.
KEY WORDS: medicare, hospital readmission rates, process of care measurements, hospital compare
INTRODUCTION
Hospital readmissions are common, potentially harmful for patients, and enormously costly to the US health care system. Within 30 days of discharge, as many as one in four patients will return to the hospital,1–5 and it has been estimated that unplanned readmissions were responsible for $17.6 billion in Medicare spending in 2004.5,6 The large clinical impact, coupled with growing concerns about current levels of health care spending, has made reducing readmission rates a national priority and a central goal of health care reform legislation.
Existing literature on the association between hospital care processes and outcomes have provided inconsistent results. Earlier studies,7,8 as well as more recent single-institution analyses,9,10 have suggested that better quality of inpatient care is associated with a lower risk of readmission. Little is known, however, about whether greater adherence to the process of care quality measures reported on the Centers for Medicare & Medicaid Services (CMS) Hospital Compare website11 is associated with lower readmission risk. While previous studies have observed only a weak association between performance on these process measures and 30-day mortality rates,12–14 it is possible that these interventions have a greater effect on readmission than on mortality. These process measures focus on appropriate medications at the time of discharge, vaccination, and discharge instructions, and hospitals that are more successful at delivering such interventions might experience lower readmission rates.
We explored the relationship between hospital performance on Medicare’s Hospital Compare process quality measures and risk-standardized all-cause 30-day readmission rates for patients aged 66 or older, with a principal discharge diagnosis of acute myocardial infarction (AMI), heart failure (HF), or pneumonia, or undergoing abdominal, cardiac and vascular, or orthopedic surgery.
METHODS
Design and Data Sources
We performed a cross-sectional analysis using discharge and quality of care assessment records that were submitted by hospitals that participated in the Hospital Inpatient Quality Reporting (IQR) Program11,15 from January 1 through December 1, 2007. We used the Quality Improvement Organization (QIO) Clinical Data Warehouse (CDW), which is an electronic database currently being used by CMS for the Hospital IQR Program, The Joint Commission, and the Hospital Quality Alliance (HQA) initiative. It contains patient-level data, including quality of care assessments using uniform instructions, principal and secondary diagnoses, procedures performed, discharge disposition status, the patient’s ZIP code of residence, age, gender and reported race/ethnicity.15,16 Results from this database are made available to consumers on CMS’ Hospital Compare website, aggregated at the hospital level.11 The analysis was restricted to patients who were enrolled in fee-for-service Medicare, aged ≥ 66 years. Prior admissions and readmissions were assessed using the National Claims History (NCH) file. Characteristics of the participating hospitals, including the number of beds, teaching status, geographic region, and whether the hospital was located in an urban or rural area, were obtained from the CMS Online Survey, Certification and Reporting database (OSCAR) and from the CMS Historical Impact Files for fiscal year 2007.17
Study Population
Patients were included if they were 66 years or older, received a principal discharge diagnosis of AMI, HF, or pneumonia, or a principal procedure code indicative of abdominal surgery, cardiac and vascular surgery, or orthopedic surgery, and were discharged from an acute care hospital that reported data to the Hospital IQR Program in 2007. Approximately 95 % of the acute care hospitals participated in the reporting program in 2007.18 International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used in accordance with the Specifications Manual for National Hospital Quality Measures for 2007 hospital discharges16 (Available online: Appendix 1).
Patients were excluded if they did not survive the index admission. Cases where it was not possible to create a link between the QIO CDW and NCH File were also excluded. Consistent with the approach used by CMS for hospital outcomes reporting,19 patients transferred to another acute care hospital were assigned to the hospital that discharged the patient. Any admission within 30 days of discharge from an index admission was considered a readmission. (Patient selection flowchart available online: Appendix 2)
Process of Care Quality Measures
Individual-level process of care quality measures in the QIO CDW database for 2007 included eight measures to assess the quality of care provided for patients with AMI, four measures for HF, seven measures for pneumonia, and nine measures related to CMS’ Surgical Care Improvement Project (Table 1).
Table 1.
Condition-Specific Process of Care Performance Measures
| Acute Myocardial Infarction (AMI) | |
| AMI-1 | Aspirin use at arrival |
| AMI-2 | Aspirin prescribed at discharge |
| AMI-3 | Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker for left ventricular dysfunction |
| AMI-4 | Adult smoking cessation advice/counseling |
| AMI-5 | Beta blocker prescribed at discharge |
| AMI-6 | Beta blocker at arrival |
| AMI-7a | Thrombolytic agent received within 30 min of arrival |
| AMI-7b | Percutaneous coronary intervention received within 90 min of hospital arrival |
| Pneumonia (PN) | |
| PN-1 | Oxygenation assessment |
| PN −2 | Pneumococcal vaccination status |
| PN-3b | Blood culture performed in the emergency department prior to receiving antibiotic |
| PN-4 | Adult smoking cessation advice/counseling |
| PN-5b | Initial antibiotic received within 4 h of hospital arrival |
| PN-6 | Appropriate initial antibiotic selection |
| PN-7 | Influenza vaccination status |
| Heart Failure (HF) | |
| HF-1 | Discharge instruction |
| HF-2 | Left ventricular function assessment |
| HF-3 | Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker for left ventricular dysfunction |
| HF-4 | Adult smoking cessation advice/counseling |
| Surgical Care Improvement Project (SCIP) | |
| SCIP-Inf1 | Prophylactic antibiotic received within 1 h prior to surgical incision |
| SCIP-Inf2 | Prophylactic antibiotic selection |
| SCIP-Inf3 | Prophylactic antibiotic discontinued within 24 h after surgery end time |
| SCIP-Inf4 | Cardiac surgery patients with controlled 6 AM postoperative glucose |
| SCIP-Inf6 | Patients with appropriate hair removal |
| SCIP-Inf7 | Colorectal surgery patients with immediate postoperative normothermia |
| SCIP-VTE1 | Recommended venous thromboembolism prophylaxis ordered |
| SCIP-VTE2 | Recommended venous thromboembolism prophylaxis ordered and prophylaxis received |
| SCIP –Card2 | Surgery patients on beta-blocker therapy prior to admission who received a beta-blocker during perioperative period |
Hospital Performance on Process of Care Measures
We computed two standard composite measures of hospital performance for each condition: the “Overall Measure” (OM), also known as the “Opportunity Model” score, and the “Appropriate Care Measure” (ACM), also known as the “All-or-None” score. To obtain the OM score, we first calculated the hospital performance rate for each measure as the proportion of patients who received a specific process of care out of all the patients who were eligible for such care, using patient-level data. As an example for eligibility, a patient with AMI is not considered eligible for smoking cessation counseling if he is a non-smoker. We then computed the OM score by adding up the number of care events that met the recommendations and dividing this sum by the number of opportunities to provide the recommended care.20 With this approach to measurement, if a patient receives three of the four recommended care elements, the hospital gets credit for delivering 75 % of the elements. Using patient-level data again, the ACM score was calculated, as the proportion of patients who received all of the indicated processes of care for which they were eligible out of all the patients who were eligible for one or more of the indicated processes of care.21 With this option for calculating performance no partial credit is given; the patient either receives all the care elements or does not.
For each composite measure, hospitals with fewer than 25 eligible patients in the denominator were excluded.
Outcome Measures
Each hospital’s condition-specific 30-day risk standardized readmission rate was estimated from patient level-data, only for those individuals included in the process of care performance scores. We used the statistical modeling techniques employed by CMS for reported readmission rates on the Hospital Compare website.19 Using hierarchical generalized linear models accounting for clustering of patients within hospitals, for each condition we modeled the patient’s probability of readmission based on age, gender, race/ethnicity, the median income level in the patient’s ZIP code of residence, comorbidities, discharge disposition, number of admissions in the prior year, and length of stay relative to the hospital median length of stay for that condition. From the models, the predicted readmission rate for each hospital and each condition was calculated as the rate of readmission that would be anticipated in the particular hospital, using the hospital random effect, given the patient case-mix. Then, the expected readmission rate was calculated as the rate of readmissions that would be expected if the same patient mix had been treated at the “average” hospital, using the average hospital effect. Finally, each hospital’s condition-specific risk-standardized readmission rate was calculated as the ratio of the predicted to expected readmission rates standardized by the overall unadjusted mean readmission rate for all included cases. Bootstrapping methods were used to derive confidence intervals. Comorbidities were assessed using software made available by the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality.22 This software, based on the work reported by Elixhauser et al.,23 assigns variables that identify comorbidities in hospital discharge records using the diagnosis coding of ICD-9-CM.
Analysis
We examined the association between hospital performance on the process of care measures and risk-standardized readmission rates via Spearman rank correlations. Additionally, we stratified hospitals into quartiles based on their performance scores for each of the conditions, and calculated the absolute difference in mean risk-standardized readmission rates of hospitals in the highest and lowest quartiles of performance.
We developed two multivariable linear models to evaluate the association of performance measure scores with risk-standardized readmission rates, with and without adjustment for the hospital characteristics (number of beds, teaching status, geographic region, and whether the hospital was located in an urban or rural area). We assessed the first model with the performance scores grouped in quartiles and the second model with the performance scores as a continuous variable. Separate models were developed for each medical and surgical condition.
For conditions that showed a significant correlation between the performance score and the readmission rate, we calculated the number of potentially avoidable readmissions/100,000 discharges if all patients would have been treated at hospitals with readmission rates at the mean level of the highest quartile of performance.
All analyses were conducted using SAS 9.2 (SAS Institute, North Carolina).
The study protocol and procedures were reviewed and approved by the Institutional Review Board at Baystate Medical Center.
RESULTS
The number of hospitals included for each condition ranged from 972 for cardiac and vascular surgery to 2,940 for heart failure. The number of patients included in the analyses varied from 328,830 for pneumonia to 48,281 for abdominal surgery (Table 2).
Table 2.
Median Hospital Performance on Overall Measure Score and Appropriate Care Measure Score, 2007
| Condition | Number of hospitals | Number of patients | Overall Measure (OM) Score (%) | Appropriate Care (ACM) Measure Score (%) |
|---|---|---|---|---|
| Median (IQR*) | Median (IQR*) | |||
| Pneumonia | 2,940 | 328,830 | 89.6 (84.6–93.2) | 66.7 (54.8–77.2) |
| Heart Failure | 2,773 | 322,668 | 89.0 (81.9–94.3) | 78.8 (66.2–88.8) |
| Acute Myocardial Infarction | 1,477 | 117,514 | 95.7 (93.1–97.8) | 87.9 (80.8–93.7) |
| Abdominal Surgery | 1,106 | 48,281 | 79.4 (71.1–86.6) | 45.8 (32.1–59.7) |
| Cardiac and Vascular Surgery | 972 | 73,573 | 91.7 (86.5–94.7) | 73.0 (59.3–82.7) |
| Orthopedic Surgery | 2,270 | 205,526 | 92.9 (88.3–95.9) | 71.1 (55.8–82.6) |
*IQR Interquartile range
Hospital Process Measures Scores
Across the six conditions, the median OM score ranged from 79.4 % for abdominal surgery to 95.7 % for AMI, and the median ACM score ranged from 45.8 % for abdominal surgery to 87.9 % for AMI (Table 2). Individual item process compliance on the hospital performance measures ranged from as low as 67.4 % for recommended venous thromboembolism prophylaxis received within 24 h after abdominal surgery to 98 % for smoking cessation counseling.
Hospital-Level Risk-Standardized Readmission Rates
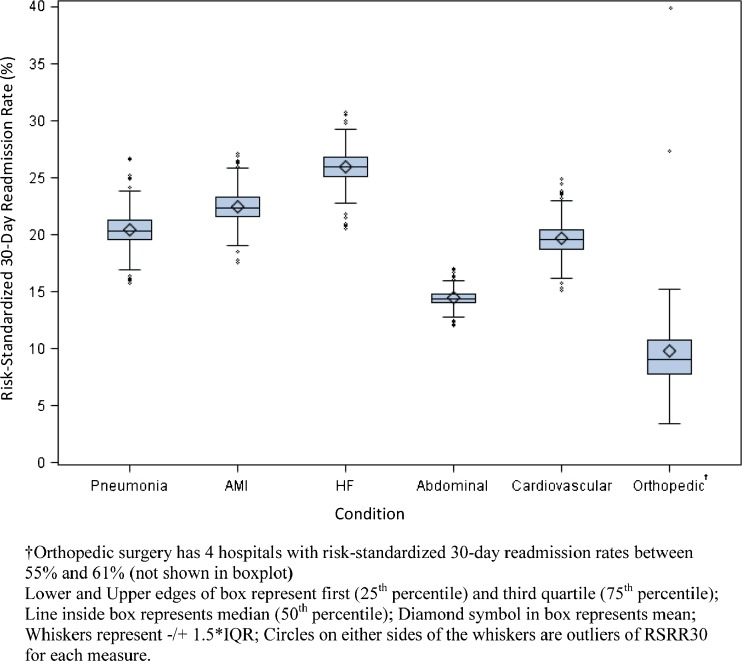
Median risk-standardized readmission rates ranged from 9.1 % for orthopedic surgery to 25.9 % for HF (Fig. 1). Across the 10th to 90th percentiles, the readmission rate ranged from 24.3 to 27.6 % for HF; 20.7 to 24.1 % for AMI; 18.8 to 22.2 % for pneumonia; 13.7 to 15.2 % for abdominal surgery; 18.1 to 21.4 % for cardiac and vascular surgeries; and 6.9 to 12.7 % for orthopedic surgeries.
Figure 1.
Condition-specific risk-standardized 30-day readmission rates across hospitals.
Relationship Between Process Measure Performance and Risk-Standardized Readmission Rates
Higher performance scores were significantly associated with lower readmission rates for pneumonia, AMI, and orthopedic surgery, but the R correlation coefficients were low, ranging from 0.06 to 0.10. There was no statistically significant correlation between process measures and hospital readmission rates for HF, abdominal surgery, or cardiac/vascular surgery (Table 3).
Table 3.
Spearman Correlations for Performance Scores and Risk-Standardized All-Cause 30-day Readmission Rates
| Condition | Overall Measure (OM) Score | Appropriate Care Measure (ACM) Score | ||
|---|---|---|---|---|
| Spearman Correlation | p-value | Spearman Correlation | p-value | |
| Pneumonia | −0.07 | < 0.001 | −0.06 | 0.001 |
| Heart Failure | −0.02 | 0.22 | −0.03 | 0.19 |
| Acute Myocardial Infarction | −0.10 | < 0.001 | −0.10 | < 0.001 |
| Abdominal Surgery | 0.04 | 0.19 | 0.06 | 0.05 |
| Cardiac and Vascular Surgery | 0.05 | 0.16 | 0.04 | 0.26 |
| Orthopedic Surgery | −0.06 | 0.003 | −0.05 | 0.03 |
There was little variation in risk-standardized readmission rates across the four quartiles of process measure performance score. The difference in mean risk-standardized readmission rates between hospitals in the 1st and 4th quartiles of process measure performance was statistically significant only for AMI and pneumonia; however, in these cases, the difference in readmission rates was small (0.3 percentage points) (Table 4 and Fig. 2).
Table 4.
Mean Risk-Standardized All-Cause 30-day Readmission Rates, by Performance Score Quartiles, and Difference in Mean Readmission Rate Between Lowest and Highest Quartiles of Performance
| Mean (SE) Risk-Standardized All-Cause 30-Day Readmission Rate | ||||||
|---|---|---|---|---|---|---|
| Pneumonia | Heart Failure | Acute Myocardial Infarction | Abdominal Surgery | Cardiac and Vascular Surgery | Orthopedic Surgery | |
| Quartiles of Overall Measure (OM) Score | ||||||
| 1st quartile | 19.42 % (0.2) | 25.34 % (0.2) | 21.49 % (0.2) | 14.23 % (0.1) | 19.18 % (0.3) | 9.70 % (0.5) |
| 2nd quartile | 19.10 % (0.2) | 25.27 % (0.2) | 21.42 % (0.2) | 14.23 % (0.1) | 19.08 % (0.3) | 9.70 % (0.5) |
| 3rd quartile | 19.15 % (0.2) | 25.26 % (0.2) | 21.29 % (0.2) | 14.25 % (0.1) | 19.36 % (0.3) | 9.27 % (0.5) |
| 4th quartile | 19.11 % (0.2) | 25.29 % (0.2) | 21.24 % (0.2) | 14.29 % (0.1) | 19.27 % (0.3) | 9.61 % (0.5) |
| Difference in mean readmission rate between lowest and highest quartile (SE) | 0.31 (0.1) | 0.05 (0.1) | 0.25 (0.1) | −0.06 (0.06) | −0.09 (0.1) | 0.09 (0.2) |
| p-value* | <0.0001 | 0.5226 | 0.0148 | 0.3104 | 0.4735 | 0.7257 |
| Quartiles of Appropriate Care Measure (ACM) Score | ||||||
| 1st quartile | 19.38 % (0.2) | 25.35 % (0.2) | 21.56 % (0.2) | 14.21 % (0.1) | 19.23 % (0.3) | 9.67 % (0.5) |
| 2nd quartile | 19.13 % (0.2) | 25.25 % (0.2) | 21.39 % (0.2) | 14.19 % (0.1) | 19.06 % (0.3) | 9.63 % (0.5) |
| 3rd quartile | 19.11 % (0.2) | 25.27 % (0.2) | 21.29 % (0.2) | 14.27 % (0.1) | 19.39 % (0.3) | 9.44 % (0.5) |
| 4th quartile | 19.15 % (0.2) | 25.28 % (0.2) | 21.25 % (0.2) | 14.29 % (0.1) | 19.28 % (0.3) | 9.55 % (0.5) |
| Difference in mean readmission rate between lowest and highest quartile (SE) | 0.23 (0.1) | 0.07 (0.1) | 0.31 (0.1) | −0.08 (0.06) | −0.05 (0.1) | 0.12 (0.2) |
| p-value* | 0.0019 | 0.3432 | 0.0022 | 0.1293 | 0.6587 | 0.6265 |
Adjusted for hospital bed size, rural–urban status, region, ownership, teaching status, hospital mortality rate
*t-test for difference between lowest and highest quartile mean readmission rate
Figure 2.
Risk-standardized 30-day readmission rates and hospital performance.
In the sensitivity analyses, which modeled the risk standardized readmission rate adjusting for hospital characteristics and performance scores, the results did not change meaningfully (data not shown).
Multivariable models that included process measure compliance scores along with hospital characteristics explained only a small amount of the variation in risk-standardized, readmission rates. For example, for pneumonia, only 4.3 % of the total variation in hospital-level readmission rates was explained by the model, and the OM score alone accounted for only 0.64 % of the variation observed.
For conditions where higher performance was associated with lower readmission rates, the potential number of readmissions avoided per 100,000 discharges was 226 (95 % CI, 83–368) for pneumonia and 308 (95 % CI, 111–505) for AMI.
DISCUSSION
In this large study of approximately 2,700 US hospitals, we found little association between hospital performance on the process of care quality measures and hospital risk-standardized, 30-day all-cause readmission rates across a spectrum of medical and surgical conditions. Even when the associations were statistically significant, the differences in the readmission rates of high and low-performing hospitals were small. Moreover, our analysis showed that performance on process measures explained less than 1 % of the observed variation in risk-standardized readmission rates across hospitals. Based on these results, it does not appear that efforts to reduce readmission rates are likely to benefit from further focus on collecting and publicly reporting data on these process measures.
How can we account for the weak associations observed in this study? One possibility is that these measures may have little impact on the risk of readmission. For example, antibiotic discontinuation after 24 h among patients undergoing surgery was intended to prevent unnecessary antibiotic therapy, and as such is unlikely to affect 30-day readmission, except through decreasing the risk of C difficile colitis. Also, the benefit of smoking cessation counseling is achieved over the long-term. In contrast to existing process measures, initiatives such as improving the quality of care coordination at the time of discharge, early follow-up with one’s primary care physician, and patient adherence to prescribed medication regimens have demonstrated to reduce readmission rates.24–30 Second, even if some of the processes measures do play a role in determining the risk of readmission, the way they are defined may make them insensitive to subtle differences in the quality of the process they are attempting to measure. For example, documentation in the chart that discharge instructions were provided to patients does not accurately reflect the intensity of the intervention. Further, the number of care processes reflected by current measures represents just a fraction of the entire spectrum of care provided to patients during hospitalization. Finally, there was relatively little variation across hospitals in some of the processes of care, thereby reducing the range of performance that could be sufficiently examined.
Given our results, some will inevitably question the appropriateness of continuing to promote these process measures as tools for consumers to identify high-performing hospitals, or for pay-for-performance programs. However, in the face of limited evidence about effective treatment strategies for most acute care conditions, it is important to recognize the generally strong evidence for most of CMS’ reported hospital quality of care measures. For example, there is little controversy that patients with AMI should receive beta blockers at discharge,31 or that all eligible patients with HF should receive an angiotensin-converting enzyme inhibitor.32,33 Furthermore, although performance on the measures may not predict hospital-level outcomes, the Hospital Inpatient Quality Reporting program has stimulated measurement and reporting activities that are now routine in the majority of hospitals.34,35 While there are many enhancements that can be made to the selected processes of care measured, the measures publicly reported on Hospital Compare should be viewed as providing information complementary to that provided by outcome measures such as readmission rates, and should be reported together as both reflect quality of care.34
The results of this study extend the findings of previous research, which found that Hospital Compare performance measures had a modest association with all-cause mortality. For example, in a study of Medicare patients admitted at 3,657 acute care hospitals, Werner and colleagues12 found that differences in performance on the process measures explained little of the variation in risk-standardized mortality for AMI or pneumonia. The existing research on the association between process measures and readmission rates has provided inconsistent results. A small cohort study showed that adherence to a composite process of care measurements was related to a reduction in all-cause readmission in patients with HF.8 A more recent single center study found that adherence to recommended AMI and pneumonia care processes was associated with improved long-term outcomes, whereas the results for HF measures were inconsistent.9 Our results confirm and build upon the findings from another study that found no association between discharge instructions and readmission rates in patients with HF.36 A significant methodological strength of our study is that we relied on patient-level data and hospital readmission rates were estimated for those individuals included in the process of care performance scores. Several of the earlier studies assessed the association between hospitals performance and readmission rates based on the results reported on Hospital Compare; because they used performance on the process of care measures assessed at the hospital level, the estimated readmission and mortality rates did not exclude patients who were considered ineligible for the recommended interventions. Another important strength of our study is that in 2007, nearly 95 % of acute care hospitals participated successfully in the reporting program, demonstrating that our results can be generalized.18
Our study has several limitations. First, we analyzed patients enrolled in traditional fee-for-service Medicare and the results may not be generalizable to other patient populations, particularly to younger patients. Second, our approach to risk adjustment relied on administrative claims, and may have failed to account for important unmeasured factors, resulting in residual confounding. However, these methods have been found to achieve similar results to those obtained by chart review.37,38 Third, there are important limitations to some of the process measures we relied upon. For example, while providing a prescription for a beta blocker at the time of discharge to a patient with AMI represents good care, it does not ensure medication adherence after the patient returns home. Additionally, a large proportion of patients are not included in the publicly reported process of care measures data. The exclusion rates vary by measure, and the reported rates of performance on Hospital Compare only reflect care that was given to patients who were eligible for the measures.39,40 Patients excluded from the measures might have higher rates of adverse outcomes.41 More detailed information on the portion and characteristics of included patients should be reported for currently reported process measures. Finally, our findings are valid only over the 2007 study period and our data predates the public reporting of readmission rates. As hospital performance on the process measures improves and hospitals focus on reducing readmission rates, more recent data could produce different results than those reported in this study.
CONCLUSION
Hospitals that achieved greater adherence to recommended care processes did not achieve meaningfully lower 30-day risk-standardized hospital readmission rates compared to those with lower levels of performance. Based on these results, it does not appear that efforts to reduce readmission rates are likely to benefit from further focus on collecting and publicly reporting data on these process measures.
Electronic supplementary material
(DOC 197 kb)
Acknowledgements
Dr. Stefan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Stefan, Lindenauer, Bratzler, Nsa, Pekow, Rothberg
Analysis and interpretation of the data: Miller, Nsa, Priya, Pekow, Stefan, Lindenauer
Drafting of the manuscript: Stefan
Critical revision of the manuscript for important intellectual content: Stefan, Lindenauer, Pekow, Nsa, Rothberg, Bratzler, Goldberg, Baus
We thank Ms. Dana Auden MS for her contribution to the statistical analysis of this study. Ms Auden was employed by Oklahoma Foundation for Medical Quality during the project, which led to this publication. Ms. Auden was not compensated for this work.
The analyses upon which this publication is based were performed under Contract Number HHSM-500-2008-OK9THC, entitled “Utilization and Quality Control Peer Review Organization for the State Oklahoma,” sponsored by the Centers for Medicare & Medicaid Services, an agency of the Department of Health & Human Services. The contents of this publication does not necessarily reflect the views or policies of the Department of Health & Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government. The authors assume full responsibility of the accuracy and completeness of the ideas presented. 4-1399-OK-0212
This study was also supported by a Baystate Health Incubator fund and internal Center for Quality of Care departmental funds.
Dr. Stefan is supported by KM1 CA156726 from the National Cancer Institute (NCI) and by the National Center for Research Resources (UL1 RR025752). The content of this publication is solely the responsibility of the authors and does not represent the official views of NIH, NCRR or NCI.
The sponsors did not have any role in the design and conduct of the study, in the collection, management, analysis and interpretation of the data, or in the preparation, review or approval of the manuscript
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Bernheim SM, Grady JN, Lin Z, et al. National patterns of risk-standardized mortality and readmission for acute myocardial infarction and heart failure. Update on publicly reported outcomes measures based on the 2010 release. Circ Cardiovasc Qual Outcomes. 2010;3(5):459–467. doi: 10.1161/CIRCOUTCOMES.110.957613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303(21):2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Epstein AM. Revisiting readmissions–changing the incentives for shared accountability. N Engl J Med. 2009;360(14):1457–1459. doi: 10.1056/NEJMe0901006. [DOI] [PubMed] [Google Scholar]
- 4.Ross JS, Chen J, Lin Z, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. Jan;3(1):97–103. [DOI] [PMC free article] [PubMed]
- 5.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 6.Report to the congress: Promoting greater efficiency in Medicare. Washington, DC: MedPAC; 2007. [Google Scholar]
- 7.Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care. 1997;35(10):1044–1059. doi: 10.1097/00005650-199710000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Chung ES, Lin G, Casey DE, Jr, et al. Relationship of a quality measure composite to clinical outcomes for patients with heart failure. Am J Med Qual. 2008;23(3):168–175. doi: 10.1177/1062860608315337. [DOI] [PubMed] [Google Scholar]
- 9.Shahian DM, Meyer GS, Mort E, et al. Association of national hospital quality measure adherence with long-term mortality and readmissions. BMJ Qual Saf. 2012;21(4):325–336. doi: 10.1136/bmjqs-2011-000615. [DOI] [PubMed] [Google Scholar]
- 10.Polanczyk CA, Newton C, Dec GW, Di Salvo TG. Quality of care and hospital readmission in congestive heart failure: an explicit review process. J Card Fail. 2001;7(4):289–298. doi: 10.1054/jcaf.2001.28931. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Medicare and Medicaid. Hospital Compare. http://www.hospitalcompare.hhs.gov/. Accessed September 13, 2012.
- 12.Werner RM, Bradlow ET. Relationship between Medicare’s hospital compare performance measures and mortality rates. JAMA. 2006;296(22):2694–2702. doi: 10.1001/jama.296.22.2694. [DOI] [PubMed] [Google Scholar]
- 13.Jha AK OE, Li Z, Epstein AM. The inverse relationship between mortality rates and performance in the hospital quality alliance measures. Health Aff (Millwood) 2007;26(4):1104–1110. doi: 10.1377/hlthaff.26.4.1104. [DOI] [PubMed] [Google Scholar]
- 14.Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007;297(1):61–70. doi: 10.1001/jama.297.1.61. [DOI] [PubMed] [Google Scholar]
- 15.Hospital Inpatient Quality Reporting Program. www.qualitynet.org/. Accessed September 13, 2012.
- 16.Specifications Manual for National Hospital Quality Measures, version 1.04a, Apendix A. http://www.jointcommission.org/specifications_manual_for_national_hospital_inpatient_quality_measures.aspx. Accessed September 13, 2012.
- 17.CMS Historical Impact Files. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Historical-Impact-Files-for-FY-1994-through-Present.html. Accessed September 13, 2012.
- 18.Hospital Inpatient Quality Reporting Program http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalRHQDAPU.html. Accessed September 13, 2012.
- 19.Statistical methods to calculate 30-day risk standardized rates of readmission. http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1219069855841. Accessed September 13, 2012.
- 20.Joint Commision on Accreditation of Healthcare Organizations. Quality report user guide. http://www.jointcommission.org/. Accessed September 13, 2012.
- 21.Nolan T, Berwick DM. All-or-none measurement raises the bar on performance. JAMA. 2006;295(10):1168–1170. doi: 10.1001/jama.295.10.1168. [DOI] [PubMed] [Google Scholar]
- 22.Healthcare Cost and Utilization Project (HCUP). Comorbidity Software, version 3.6. Rockville, MD: Agency for Healthcare Research and Quality. http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed September 13, 2012.
- 23.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Shepperd S, Parkes J, McClaren J, Phillips C. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2004;1:CD000313. doi: 10.1002/14651858.CD000313.pub2. [DOI] [PubMed] [Google Scholar]
- 25.van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192. doi: 10.1046/j.1525-1497.2002.10741.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parrish MM, O’Malley K, Adams RI, Adams SR, Coleman EA. Implementation of the care transitions intervention: sustainability and lessons learned. Prof Case Manag. 2009;14(6):282–293. doi: 10.1097/NCM.0b013e3181c3d380. [DOI] [PubMed] [Google Scholar]
- 28.Parry C, Min SJ, Chugh A, Chalmers S, Coleman EA. Further application of the care transitions intervention: results of a randomized controlled trial conducted in a fee-for-service setting. Home Health Care Serv Q. 2009;28(2–3):84–99. doi: 10.1080/01621420903155924. [DOI] [PubMed] [Google Scholar]
- 29.Coleman EA, Smith JD, Frank JC, Min SJ, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention. J Am Geriatr Soc. 2004;52(11):1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- 30.Daly BJ, Douglas SL, Kelley CG, O’Toole E, Montenegro H. Trial of a disease management program to reduce hospital readmissions of the chronically critically ill. Chest. 2005;128(2):507–517. doi: 10.1378/chest.128.2.507. [DOI] [PubMed] [Google Scholar]
- 31.Timolol-induced reduction in mortality and reinfarction in patients surviving acute myocardial infarction. N Engl J Med. Apr 2 1981;304(14):801–7. [DOI] [PubMed]
- 32.Pfeffer MA, Lamas GA, Vaughan DE, Parisi AF, Braunwald E. Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction. N Engl J Med. 1988;319(2):80–86. doi: 10.1056/NEJM198807143190204. [DOI] [PubMed] [Google Scholar]
- 33.Pfeffer MA, McMurray JJ, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003;349(20):1893–1906. doi: 10.1056/NEJMoa032292. [DOI] [PubMed] [Google Scholar]
- 34.Fung CH, Lim YW, Mattke S, Damberg C, Shekelle PG. Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med. 2008;148(2):111–123. doi: 10.7326/0003-4819-148-2-200801150-00006. [DOI] [PubMed] [Google Scholar]
- 35.Hibbard JH, Stockard J, Tusler M. Does publicizing hospital performance stimulate quality improvement efforts? Health Aff (Millwood) 2003;22(2):84–94. doi: 10.1377/hlthaff.22.2.84. [DOI] [PubMed] [Google Scholar]
- 36.Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361(27):2637–2645. doi: 10.1056/NEJMsa0904859. [DOI] [PubMed] [Google Scholar]
- 37.Lindenauer PK, Bernheim SM, Grady JN, et al. The performance of US hospitals as reflected in risk-standardized 30-day mortality and readmission rates for medicare beneficiaries with pneumonia. J Hosp Med. 2010;5(6):E12–18. doi: 10.1002/jhm.822. [DOI] [PubMed] [Google Scholar]
- 38.Keenan PS, Normand SL, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1(1):29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 39.Bernheim SM, Wang Y, Bradley EH, et al. Who is missing from the measures? Trends in the proportion and treatment of patients potentially excluded from publicly reported quality measures. Am Heart J. 2010;160(5):943–950. doi: 10.1016/j.ahj.2010.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rathore SS, Wang Y, Radford MJ, Ordin DL, Krumholz HM. Quality of care of Medicare beneficiaries with acute myocardial infarction: who is included in quality improvement measurement? J Am Geriatr Soc. 2003;51(4):466–475. doi: 10.1046/j.1532-5415.2003.51154.x. [DOI] [PubMed] [Google Scholar]
- 41.Bratzler DW, Ma A, Nsa W, Fleisher L. Performance on SCIP Measures and Risk of Surgical Site Infection IDSA. Boston; 2011.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 197 kb)