ABSTRACT
BACKGROUND
Low health literacy is considered a potential barrier to improving health outcomes in people with diabetes and other chronic conditions, although the evidence has not been previously systematically reviewed.
OBJECTIVE
To identify, appraise, and synthesize research evidence on the relationships between health literacy (functional, interactive, and critical) or numeracy and health outcomes (i.e., knowledge, behavioral and clinical) in people with diabetes.
METHODS
English-language articles that addressed the relationship between health literacy or numeracy and at least one health outcome in people with diabetes were identified by two reviewers through searching six scientific databases, and hand-searching journals and reference lists.
FINDINGS
Seven hundred twenty-three citations were identified and screened, 196 were considered, and 34 publications reporting data from 24 studies met the inclusion criteria and were included in this review. Consistent and sufficient evidence showed a positive association between health literacy and diabetes knowledge (eight studies). There was a lack of consistent evidence on the relationship between health literacy or numeracy and clinical outcomes, e.g., A1C (13 studies), self-reported complications (two studies), and achievement of clinical goals (one study); behavioral outcomes, e.g., self-monitoring of blood glucose (one study), self-efficacy (five studies); or patient-provider interactions (i.e., patient-physician communication, information exchange, decision-making, and trust), and other outcomes. The majority of the studies were from US primary care setting (87.5 %), and there were no randomized or other trials to improve health literacy.
CONCLUSIONS
Low health literacy is consistently associated with poorer diabetes knowledge. However, there is little sufficient or consistent evidence suggesting that it is independently associated with processes or outcomes of diabetes-related care. Based on these findings, it may be premature to routinely screen for low health literacy as a means for improving diabetes-related health-related outcomes.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-012-2241-z) contains supplementary material, which is available to authorized users.
KEY WORDS: health literacy, numeracy, diabetes, health outcomes
INTRODUCTION
Health literacy is a set of skills that people need to function effectively in the healthcare environment.1 These include functional, interactive, critical and numeracy skills. Functional skills are the ability to read and understand written text, locate and interpret information in documents, and write or complete forms. Interactive skills are ability to speak and listen effectively and communicate about health-related information. Critical skills are the ability to navigate the healthcare system and make appropriate health decisions. Numeracy skills are ability to use numeric information for tasks, such as interpreting medication dosages and food labels.1,2
Low health literacy is recognized as a stronger predictor of a persons’ health than age, income, employment status, education level, or race,3 and is associated with a wide range of adverse effects on care processes and health outcomes.4,5 Low levels of health literacy are more prevalent in minority populations, among persons for whom English is a second language, people with low levels of income and education, and people with a compromised health status and elder communities—the very same populations that carry the greatest burden of chronic conditions.3,6–8
Diabetes is a prototypical chronic disease, characterized by a high level of complexity that requires extensive self-care education and management. The demands on individuals with diabetes are complicated by the fact that self-care often relies on printed educational materials and verbal instructions, and requires advanced health literacy skills.9 There is a growing body of literature that explores the relationship between health literacy and health outcomes in people with diabetes. Older studies of low health literacy reported adverse impacts on diabetes-related health outcomes;10–12 however, more recent studies showed no association between health literacy levels and intensity, frequency or incidence of outcomes,13,14 and thus the effect of health literacy on the health of people with diabetes is yet unclear.
To better understand the relationship between health literacy and numeracy and health outcomes in diabetes, we conducted a systematic review of the literature. Since health literacy and numeracy are measured as separate constructs, in synthesizing the literature, we considered the association between health literacy (functional, interactive, and critical components) and health outcomes, and between numeracy (computational component) and health outcomes separately in the diabetes population.
METHODS
Data Sources, Search strategy and Study selection
We conducted a systematic review of six databases: CINAHL, Embase, ERIC, Medline, psycINFO, and SCOPUS. The searches were not limited to any time period, language, or type of published paper. No Medical Subject Heading terms specifically identify health literacy-related articles, so we conducted the searches using different combinations of the following keywords: literacy, numeracy, health literacy, diabetes, diabetic, type 2 diabetes, type 1 diabetes, and the names of health literacy instruments. Keywords were matched to database-specific indexing terms (detailed information about the search strategy are available upon request from FAS). Electronic searches were supplemented by hand searches, review of the reference lists of the included articles, and contact with content experts. Additionally, authors were contacted when additional information to determine eligibility for inclusion was needed.
Two reviewers screened the identified records, reviewed the full text of the included articles, and performed data abstraction and assessment of quality and strength of evidence. Criteria for inclusion were studies that: addressed the relationship between health literacy or numeracy and health outcomes in people with type 1 or type 2 diabetes, involved the use of valid direct or indirect measure of health literacy or numeracy, addressed at least one health outcome, and were written in English. Cohen’s kappa was used to assess inter-rater reliability in selecting studies for inclusion. Initial discrepancies were addressed through consensus and, if necessary, resolved by the senior author (JAJ).
Data Abstraction and Quality Assessment
Data on the general characteristics of the studies, including aim, design, methods, sample size and characteristics, health literacy measurement, outcomes measurement, analysis, results and conclusions, were extracted (Appendices 1 and 2; Available online). Data abstraction was done by one reviewer, and confirmed by the second reviewer. We were interested in summarizing evidence on the following outcomes: 1) clinical, 2) behavioral, 3) patient-provider relationship, and 4) other outcomes. If a study produced multiple publications on the relationship between a particular outcome and health literacy, estimates from only the most recent publication were considered in the assessment of the strength of evidence.
Since all the identified studies were observational, with no intervention intended to affect the outcome, each article was rated based on the criteria in the quality rating for observational studies by the Agency for Healthcare Research (AHRQ).15 Quality ratings are presented in Appendices 1 and 2 (Available online). Two reviewers independently rated the quality of studies as good, fair, or poor, based on the criteria that focuses on detecting bias in an observational study and precision of measurement. Because analysis techniques differed among multiple publications of the same study, overall quality was assessed for each publication, not each study. Only studies that were of fair to good quality were included in this review. Cohen’s kappa was used to assess inter-rater reliability in quality rating between the two reviewers.
Strength of Evidence Assessment
The strength of the evidence for each outcome was determined using the AHRQ guidelines16 for publications measuring health literacy and numeracy. Two reviewers independently graded the strength of evidence as high, moderate, low or insufficient on the basis of potential risk of bias of the included publications, consistency of effect across publications, directness of evidence, and precision of the estimate (Table 1). Cohen’s kappa was used to assess inter-rater reliability in rating the strength of evidence between the two reviewers.
Table 1.
Strength of Evidence Grades and Definitions16
| Grade | Definition |
|---|---|
| High | High confidence that the evidence reflects the true effect. Further research is very unlikely to change our confidence in the estimate of the effect. |
| Moderate | Moderate confidence that the evidence reflects the true effect. Further research may change our confidence in the estimate of the effect and may change the estimate. |
| Low | Low confidence that the evidence reflects the true effect. Further research is likely to change our confidence in the estimate of the effect and is likely to change the estimate. The evidence was graded as low if findings were limited to only one or a few studies that controlled for potential confounding, or if the preponderance of evidence was based on studies that did not control for potential confounding. |
| Insufficient | Evidence is unavailable or does not permit estimation of an effect. Inconsistent findings across studies were generally graded as insufficient, as was evidence limited to one study that did not control for potential confounding. |
We attempted to perform a meta-analysis to quantitatively summarize the evidence for each outcome. In both fixed and random effects models, heterogeneity was large (I2 = 80–90 %), which meant that a meta-analysis was not feasible, and pooled estimates of effects were not reported. In comparing the general characteristics of the studies, we noticed methodological variations between studies with respect to sample size, sample characteristics, health literacy measurement, and in the adjustment of potential confounders. These factors might have contributed to the observed heterogeneity. For these reasons, the evidence from included studies was summarized qualitatively in this review.
RESULTS
Literature Search
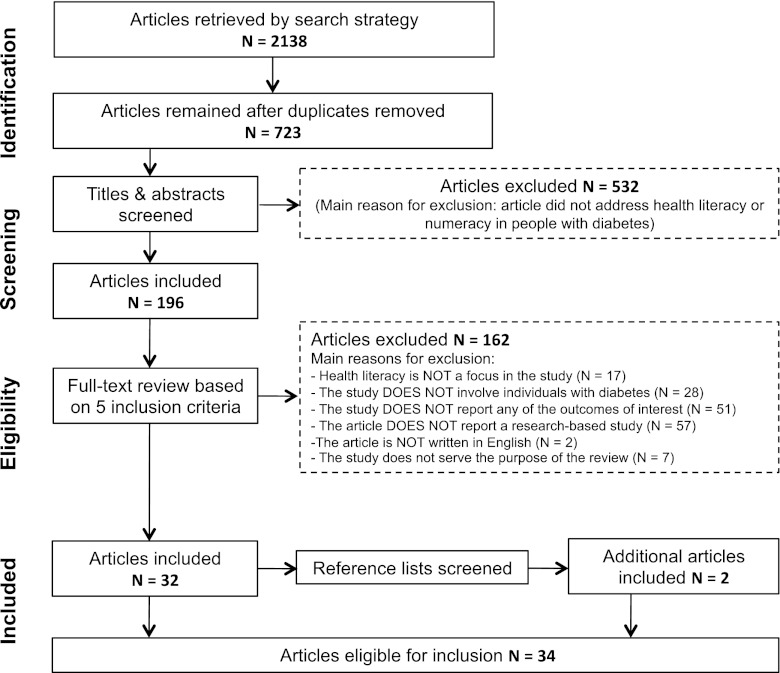
Across all databases, the search yielded 2,138 citations (Fig. 1). After removal of duplicates, 723 remained. Titles and abstracts were screened for relevance, and based on that, 196 publications were included for full-text review. Of these, 32 publications met our eligibility criteria and were included. The most common reasons for exclusion were: review and conceptual articles (35.2 %), studies that did not address any of the outcomes of interest (31.5 %), and studies that did not involve individuals with diabetes (17.3 %). Studies that addressed health literacy in caregivers of individuals with diabetes (N = 4), and in women with gestational diabetes (N = 1) were also excluded. The hand search of reference lists of included studies resulted in the inclusion of two additional publications. Thus, the total number of eligible publications was 34. Inter-rater agreement was 88 % and Cohen’s kappa was 0.70 (95 % CI: 0.59–0.84). The 34 articles were multiple publications from 24 studies. We reported the findings of this review based on the 24 studies, and evaluated the evidence based on estimates from the most recent publication of each study to avoid bias due to multiple publications.
Figure 1.
PRISMA diagram of the search and retrieval process.
Characteristics of the Included Studies
The 34 identified publications of the 24 studies were of fair to good quality (Appendices 1 and 2; Available online), and thus they were all included in this review. Inter-rater agreement on quality rating was 97 % and Cohen’s kappa was 0.91 (95%CI: 0.76–0.98). The majority of publications (29 from 21 studies) addressed only health literacy and health outcomes, while only five publications (from four studies) addressed health numeracy. All studies were observational; only two performed longitudinal data analysis (one using data from a randomized controlled trial and one from a prospective cohort study). There were no experimental studies that addressed the effect of health literacy and/or numeracy on health outcomes in this population. Half of the studies included only individuals with type 2 diabetes (12 studies) and 12 included individuals with type 1 or type 2 diabetes; no studies focused solely on type 1 diabetes. The majority of the identified studies were conducted in the United States, primarily on minority or vulnerable populations.
Health Literacy Measures
Several instruments were used to measure health literacy and numeracy in these studies. The most commonly used measure of health literacy was the Test of Functional Health Literacy in Adults–short form (s-TOFHLA) (ten studies), followed by the Rapid Estimate of Adult Literacy in Medicine (REALM) (seven studies), three brief screening questions (three studies), the original long form of the TOFHLA (two studies), the revised REALM-R (one study), and the self-rated Health Literacy 3-item scale (one study). Diabetes Numeracy Test was used to measure diabetes numeracy (three studies), and the Wide Range Achievement Test (three studies) and Subjective Numeracy Scale (one study) were used to measure general numeracy.
The included studies differed in how investigators distinguished between levels or thresholds of health literacy, either as a continuous measure or categories (e.g., inadequate, marginal, adequate; or high versus low). When categorized, the majority of the studies focused on the differences between the lowest and highest groups. Additionally, studies differed in which domain of health literacy they addressed, where most used measures of functional health literacy (23 studies), and only one study addressed all components (functional, interactive, and critical).
Health Literacy and Health Outcomes
Overall, inter-rater agreement for strength of evidence ratings for health literacy and health outcomes was 92 % and Cohen’s kappa was 0.85 (95%CI: 0.71–0.98). For health literacy, there were 23 outcomes grouped into four categories: Clinical, behavioral, patient-provider communication, and other outcomes (Table 2).
Table 2.
Health Literacy and Outcomes in Diabetes: Strength of Evidence and Summary of Findings
| Category | Outcome | Total # of studies by study design = N (# of studies NOT controlling for confounding = n1; # of studies controlling for confounding = n2) | Summary of results | Strength of evidence | ||||
|---|---|---|---|---|---|---|---|---|
| Studies NOT controlling for confounding (n1) | Studies controlling for confounding (n2) | |||||||
| Design | N (n1; n2) | Positive results* | Negative results† | Positive results* | Negative results† | |||
| Clinical outcomes | A1c | Cross-sectional | 12 (4; 8) | 1 | 3 | 4 | 4 | Insufficient |
| Longitudinal | 1 (0; 1) | – | – | – | 1 | |||
| Low-density lipoprotein (LDL) | Cross-sectional | 1 (0; 1) | – | – | – | 1 | Low | |
| Blood pressure | Cross-sectional | 2 (1; 1) | – | 1 | – | 1 | Low | |
| Self-reported significant hypoglycemia | Cross-sectional | 1 (0; 1) | – | – | 1 | – | Low | |
| Self-reported complications | Cross-sectional | 2 (0; 2) | 1 | – | – | 1 | Insufficient | |
| Achievement of clinical outcome goals for A1c | Longitudinal | 1 (0; 1) | – | – | 1 | – | Low | |
| Behavioral outcomes | Self-care | Cross-sectional | 4 (0; 4) | – | – | 4 | – | Moderate |
| Self-monitoring of blood glucose | Cross-sectional | 1 (0; 1) | – | – | – | 1 | Low | |
| Self-efficacy | Cross-sectional | 5 (1; 4) | 1 | – | 1 | 3 | Insufficient | |
| Self-management support | Cross-sectional | 1 (0; 1) | – | – | 1 | – | Low | |
| Medication adherence | Cross-sectional | 1 (0; 1) | – | – | – | 1 | Low | |
| Diabetes knowledge | Cross-sectional | 8 (3; 5) | 3 | – | 5 | – | High | |
| Longitudinal | 1 (0; 1) | – | – | 1 | – | |||
| Patient-provider interaction | Patient–physician communication | Cross-sectional | 2 (1; 1) | 1 | – | 1 | – | Low |
| Information exchange | Cross-sectional | 1 (0; 1) | – | – | 1 | – | Low | |
| Involvement in decision making | Cross-sectional | 1 (1: 0) | 1 | – | – | – | Insufficient | |
| Trust | Cross-sectional | 2 (1; 1) | – | 1 | 1 | – | Insufficient | |
| Other outcomes | Prevalence of heart failure | Cross-sectional | 1 (0; 1) | – | – | – | 1 | Low |
| Prevalence of depressive symptoms | Cross-sectional | 1 (0; 1) | – | – | – | 1 | Low | |
| Health-related quality of life | Cross-sectional | 1 (1; 0) | – | 1 | – | – | Insufficient | |
| Diabetes health-related beliefs | Cross-sectional | 1 (0; 1) | – | – | – | 1 | Low | |
| Medication beliefs | Cross-sectional | 1 (0; 1) | – | – | 1 | – | Low | |
| Healthcare and general discrimination | Cross-sectional | 1 (0; 1) | – | – | 1 | – | Low | |
| Use of computers and internet | Cross-sectional | 2 (1; 1) | 1 | – | 1 | – | Low | |
*Indicates that the study found a significant association between health literacy level and the outcomes
†Indicates that the study did not find a significant association between health literacy level and the outcomes
Health Literacy and Clinical Outcomes
Glycemic Control
The relationship between health literacy and A1c was explored in 13 studies; 12 of which were cross-sectional and one longitudinal. Some of the identified studies showed that higher levels of health literacy were associated with better glycemic control,10,12,17,18 and this relationship was mostly observed in studies that adjusted for age, sex, race, education, and treatment regimen. Moreover, few studies reported that health literacy has indirect effect on glycemic control, but did not show any direct associations.19 Overall, evidence on the relationship between health literacy and glycemic control was inconsistent across studies, and the heterogeneity did not permit the estimation of an overall effect. Therefore, this evidence was rated insufficient.
We were able to observe a trend between confounders controlled for and reported estimates in studies that explored the relationship between health literacy and A1c. The association between health literacy and A1c was significant in studies that did not adjust for diabetes knowledge;10,12,17 however, that association was not observed in studies that controlled for diabetes knowledge.13,14 Similar trends were not observed for other outcomes because of the small number of available studies.
Hypoglycemia
Two studies explored the relationships between low health literacy and self-reported hypoglycemia, and one of these studies reported that lower health literacy was associated with higher frequency of self-reported hypoglycemia.11 The quality of evidence from these two studies was rated low.
Blood Pressure
Two studies explored the relationship between health literacy and blood pressure in people with diabetes,20,24 although only one adjusted for potential confounders.20 Both studies reported that lower health literacy was associated with better control of blood pressure. This evidence was rated low.
Diabetes Complications
The relationship between health literacy and self-reported complications was explored in two studies, both adjusted for potential confounders.10,20 One study reported that lower health literacy was associated with retinopathy and stroke, but not with nephropathy, lower extremity amputation or ischemic heart disease.10 The other study showed no association between health literacy and self-reported complications.20 The evidence from these studies was inconsistent and rated insufficient.
Low-Density Lipoprotein (LDL)
One study that adjusted for potential confounders explored the relationship between health literacy and low-density lipoprotein (LDL), and showed that health literacy was not associated with LDL levels.20
Health literacy and Behavioral Indicators and Patient-Reported Outcomes
Diabetes Knowledge
Nine studies, six of which adjusted for potential confounders12–14,21–23 and three of which did not,24–26 provided high evidence that higher health literacy levels were associated with better diabetes knowledge.
Self-Efficacy
Five studies provided evidence on the relationship between health literacy and self-efficacy. Three studies reported adjusted results and showed no association between health literacy levels and self-efficacy.18,22,24 One study that adjusted for confounders27 showed no association between health literacy and self-efficacy, and the unadjusted study28 showed that higher health literacy levels were associated with higher self-efficacy scores. The evidence was inconsistent and rated insufficient.
Self-Care
Four studies that reported adjusted results showed no association between health literacy and self-care behaviors, namely diet, exercise, blood sugar testing, foot care, smoking cessation, and medication adherence.13,14,23,24 Since the evidence on this relationship was consistent, it was rated moderate.
Self-Monitoring of Blood Glucose (SMBG) and Other Self-Management
Three studies explored the relationship between health literacy and self-monitoring of blood glucose (SMBG) and self-management support, and all adjusted for potential confounders. One study did not show an association between health literacy and the frequency of SMBG,29 and another study did not show an association with medication adherence.13 The third study showed that higher health literacy levels were associated with higher self-management support ratings.30 The evidence from each of these studies was rated low.
Health Literacy and Patient–Provider Interaction Indicators
Patient–Provider Communication
Two studies,31,32 where only one reported adjusted results, showed that higher health literacy levels were associated with better patient–physician communication.32 The evidence from these studies was rated low.
Patient Trust
Two studies explored the relationship between health literacy and patient trust, where only one reported adjusted results and showed that higher health literacy levels were associated with higher scores on patient trust scores.14 The other study did not show an association between health literacy and patient trust.28 The evidence from the two studies was rated insufficient.
Information Exchange and Involvement in Decision-Making
One study reported adjusted results and showed that higher health literacy was associated with better information exchange between patients and their physicians.32 The evidence from this study was rated low. Another study that did not adjust for confounders showed no association between health literacy and patient’s involvement in decision making with their physicians.28 The evidence from this study was rated insufficient.
Use of Computers and Internet
Two studies, where only one reported adjusted results,33 explored the relationship between health literacy and patient’s use of computers and Internet for health-related learning. These studies provided low evidence that higher health literacy was associated with more frequent use of computers and Internet.33,34
Other Outcomes
Six studies explored the relationship between health literacy and prevalence of heart failure, prevalence of depressive symptoms, health-related quality of life (HRQL), diabetes health-related beliefs, medication beliefs, and healthcare discrimination respectively, where all but one reported adjusted findings. In these studies, there was no association between health literacy and prevalence of heart failure,35 prevalence of depressive symptoms,14 HRQL,28 or diabetes health-related beliefs.12 One study showed that lower health literacy was associated with medication beliefs, particularly with more concern about the harmfulness of medications,36 and another showed that lower health literacy was associated with higher reporting of healthcare discrimination.37 The evidence on these relationships was rated low, except for HRQL, which was rated insufficient.
Numeracy and Health Outcomes
Overall, inter-rater agreement for strength of evidence ratings for numeracy and health outcomes was 94 % and Cohen’s kappa was 0.86 (95 % CI: 0.73–0.99). There were four outcomes grouped into three categories: Clinical, behavioral, and other outcomes (Table 3).
Table 3.
Numeracy and Outcomes in Diabetes: Strength of Evidence and Summary of Findings
| Category | Outcome | Total # of studies by study design = N (# of studies NOT controlling for confounding = n1; # of studies controlling for confounding = n2) | Summary of results | Strength of evidence | ||||
|---|---|---|---|---|---|---|---|---|
| Studies NOT controlling for confounding (n1) | Studies controlling for confounding (n2) | |||||||
| Design | N (n1; n2) | Positive results* | Negative results† | Positive results* | Negative results† | |||
| Clinical outcomes | A1c | Cross-sectional | 4 (1; 3) | – | 1 | 2 | 1 | Insufficient |
| Behavioral outcomes | Self-care | Cross-sectional | 1 (1; 0) | – | 1 | – | – | Insufficient |
| Self-efficacy | Cross-sectional | 2 (1; 1) | – | 1 | 1 | – | Insufficient | |
| Other outcomes | Use of computers and internet | Cross-sectional | 1 (1; 0) | 1 | – | – | – | Insufficient |
*Indicates that the study found a significant association between health literacy level and the outcomes
†Indicates that the study did not find a significant association between health literacy level and the outcomes
Numeracy and Clinical Outcomes
Glycemic Control
The relationship between numeracy and A1c was explored in four studies. Two studies adjusted for potential confounders; one showed that higher numeracy was directly associated with better A1c38 and the other showed indirect effect of numeracy on A1c.39 The two other studies that reported unadjusted results did not show an association between numeracy and A1c levels.34,40 The evidence was rated insufficient.
Numeracy and Behavioral Indicators and Patient-Reported Outcomes
Self-Efficacy
Two studies explored the relationship between numeracy and self-efficacy. One study reported adjusted results and showed that higher numeracy was associated with better self-efficacy,27 and the other study reported unadjusted results and showed no association between numeracy and self-efficacy.40 This evidence was rated insufficient.
Self-Care
One study that did not adjust for confounders reported no association between numeracy and self-care.40 This evidence was rated insufficient.
Other Outcomes
One unadjusted study explored that relationship between numeracy and the use of computers and internet, and reported that higher numeracy was associated with more frequent use of computers and Internet for health-related learning.34 This evidence was rated insufficient.
Discussion
Our systematic review showed a discrepancy among studies regarding the relationship between health literacy or numeracy and several health outcomes in people with diabetes. Consistent evidence suggested a positive association between health literacy and diabetes knowledge, but even this evidence was only rated sufficient. Likewise, there is likely sufficient evidence to support a positive relationship between health literacy and self-care activities. On the other hand, the evidence for an association between health literacy and clinical indicators was weak. We found little evidence to support (or refute) an association between health literacy and important clinical events (such as mortality, cardiovascular disease), other than self-reported hypoglycemia and presence of diabetic complications. The majority of this evidence comes from cross-sectional studies, however, limiting causal inference.
It is important to note that substantial discrepancies exist in the literature, which could be due to methodological issues and challenges in the identified studies. One potential source of discrepancy could be the different tools used to measure health literacy41 and differences in thresholds used to distinguish between health literacy levels.42 This variation in estimates and thresholds, in addition to the fact that these instruments measure different aspects of health literacy and thus reflect different skills,43 could have influenced the magnitude and the precision of the observed estimates in these studies.
Another potential reason for discrepancy could be adjustment for confounders. Most studies adjusted for age, sex, race, and educational level in the analyses; however, few studies also adjusted for other factors such as diabetes duration, diabetes knowledge, self-care, self-efficacy, health status, treatment regimen, and many others, where some of these were included as mediators in the pathway between health literacy and outcomes.27 Adjusting for these confounders that are possibly intermediate variables could have induced over-adjustment bias in estimating direct effects of health literacy on outcomes.44
Another equally interesting observation in this review was from recent studies that explored factors that mediate the relationship between health literacy and diabetes-related health outcomes. Osborn and colleagues39 found that health literacy was not directly associated with self-care and A1c; however, it was indirectly associated with these outcomes through social support. The same investigators in subsequent analysis of the same study found that health literacy was indirectly associated with A1c through self-efficacy.27 Future research should further investigate these mediators and others to better understand the relationship between health literacy and health outcomes and what factors should be the target of intervention, health literacy or the mediators.
Other methodological issues that might have introduced the inconsistent results include the lack of power in some studies, or heterogeneity of participants across studies. This could indicate that health literacy might be related to certain outcomes in particular diabetes populations, but not in others. These speculations are difficult to examine, however, with the limited data and available studies.
A recent review by Berkman and colleagues explored the relationship between health literacy and health outcomes in patients of all ages and was not limited to any patient groups.4 Their findings were similar to ours, particularly on the relationship between health literacy and disease knowledge, and they reported inconsistent results regarding other outcomes that were not addressed in our review, such as healthcare utilization and costs. Other reviews focused on specific populations such as emergency room patients,45 working-age adults,46 children,47,48 and ambulatory care patients.49 These reviews also had similar results to ours with respect to disease knowledge; most were not able to provide firm conclusions on other outcomes due to insufficient evidence.
This review, as any other systematic review, reflects the quality of the published literature. Although the quality of the included studies ranged from fair to good, these ratings did not reflect the limitations imposed by the cross-sectional design of the majority of the studies, using different measures of health literacy across studies, choosing different cut-points for analysis, the inconsistent and potentially inappropriate control for confounders, and poor reporting, which made comparisons between studies difficult. In addition to methodological limitations, the majority of the studies were conducted in primary care clinics in the US; only a few were population-based and very few were conducted outside of the US (Japan, China, and Ireland).
CONCLUSION
Our review indicates that the current understanding of the effect of low health literacy on the health of people with diabetes is limited. We found that low health literacy is consistently associated with poorer diabetes knowledge. However, there is little sufficient or consistent evidence suggesting that it is independently associated with processes or outcomes of diabetes-related care. Given how important the topic is, we were surprised by the paucity of high-quality evidence.
Certainly, our findings suggest that it might be premature to embark on randomized trials or controlled interventions to improve health literacy in those with diabetes, given how little we actually know. Until better evidence is available, we believe that, outside of the study setting, it might be premature to routinely screen for health literacy or to try to improve health literacy for the purposes of improving patient-related outcomes in diabetes—although there may be other reasons to do so.
Electronic supplementary material
(PDF 190 kb)
Acknowledgements
Contributors
Not applicable
Funding
This work was supported in part by an Emerging Team Grant to the Alliance for Canadian Health Outcomes Research in Diabetes (ACHORD) (reference #: OTG-88588), sponsored by the Canadian Institute for Health Research, Institute of Nutrition, Metabolism and Diabetes.
Presentations
This work was presented at the “Alliance for Canadian Health Outcomes Research in Diabetes” annual research retreat in Banff, Canada, March 2012.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Berkman N, Terry D, McCormack L. Health literacy: What is it? J Health Comm. 2010;15:9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- 2.Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67:2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 3.Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. Health Literacy: Report of the Council on Scientific Affairs. JAMA. 1999;282:526–7. [PubMed]
- 4.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 5.DeWalt DA, Berkman N, Sheridan S, Lohr KN, Pignone MP. Literacy and Health Outcomes: A Systematic Review of the Literature. J Gen Intern Med. 2004;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolf M, Gazmararian J, Baker D. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 7.Sudore R, Mehta K, Simonsick A ea, Harris TB, Newman AB, Satterfield S, et al. Limited literacy in older people and disparities in health and healthcare access. Journal of the American Geriatrics Society. 2006;54:770-6. [DOI] [PubMed]
- 8.Schultz S, Kopec J. Impact of chronic conditions. Health Reports. Statistics Canada catalogue no. 82-003-XIE. 2003;14:41-56. [PubMed]
- 9.White R, Wolff K, Cavanaugh K, Rothman R. Addressing Health Literacy and Numeracy to Improve Diabetes Education and Care. Diabetes Spectrum. 2010;23:238–243. doi: 10.2337/diaspect.23.4.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 11.Sarkar U, Karter A, Liu J, Moffet HH, Adler NE, Schillinger D. Hypoglycemia is more common among type 2 diabetes patients with limited health literacy: The diabetes Study of Northern California (DISTANCE) J Gen Intern Med. 2010;25:962–967. doi: 10.1007/s11606-010-1389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educat. 2007;33:144–151. doi: 10.1177/0145721706297452. [DOI] [PubMed] [Google Scholar]
- 13.Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Tech Therapeut. 2011;13:335–341. doi: 10.1089/dia.2010.0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mancuso JM. Impact of health literacy and patient trust on glycemic control in an urban USA population. Nurs Health Sci. 2010;12:94–104. doi: 10.1111/j.1442-2018.2009.00506.x. [DOI] [PubMed] [Google Scholar]
- 15.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K, et al. Health literacy interventions and outcomes: an update of the literacy and health outcomes systematic review of the literature. Evidence Report/Technology Assessment no.199. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
- 16.Owens DK, Lohr KN, Atkins D, Treadwell JR, Reston JT, Bass EB, et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions—agency for healthcare research and quality and the effective health-care programs. J Clin Epidemiol. 2010;63:513–523. doi: 10.1016/j.jclinepi.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 17.Tang YH, Pang SM, Chan MF, Yeung GS, Yeung VT. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. AJAN. 2008;62:74–83. doi: 10.1111/j.1365-2648.2007.04526.x. [DOI] [PubMed] [Google Scholar]
- 18.Ishikawa H, Yano E. The relationship of patient participation and diabetes outcomes for patients with high vs. low health literacy. Patient Educ Counsel. 2011;84(3):393–7. [DOI] [PubMed]
- 19.Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy: An overlooked factor in understanding racial disparities in glycemic control. Diabetes Care 2009;32(9):1614–9. [DOI] [PMC free article] [PubMed]
- 20.Morris NS, MacLean CD, Chew LD, Littenberg B. The Single Item Literacy Screener: evaluation of a brief instrument to identify limited reading ability. BMC Family Practice 2006;7:21. [DOI] [PMC free article] [PubMed]
- 21.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Counsel. 2003;51:267–275. doi: 10.1016/S0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 22.Gerber BS, Pagcatipunan M, Smith EV, Jr, Basu SS, Lawless KA, Smolin LI, et al. The assessment of diabetes knowledge and self-efficacy in diverse population using Rasch Measurmeent. J Appl Meas. 2006;7(1):55–73. [PubMed] [Google Scholar]
- 23.Kim S, Love F, Questberg D, Shea JA. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care. 2004;27:2980–2982. doi: 10.2337/diacare.27.12.2980. [DOI] [PubMed] [Google Scholar]
- 24.McCleary-Jones V. Health literacy and its association with diabetes knowledge, self efficacy and diabetes self-management among African Americans with Diabetes Mellitus. The ABNF Journal. 2011;22(2):25–32. [PubMed] [Google Scholar]
- 25.Ishikawa H, Takeuchi T, Yano E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care. 2008;31:874–879. doi: 10.2337/dc07-1932. [DOI] [PubMed] [Google Scholar]
- 26.Williams M, Baker D, Parkes R, Nurss R. Relationship of functional health literacy to patients’ knowledge of chronic disease: A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 27.Osborn C, Cavanaugh K, Wallston K, Rothman R. Self-Efficacy Links Health Literacy and Numeracy to Glycemic Control. J Health Comm. 2010;15:146–158. doi: 10.1080/10810730.2010.499980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DeWalt DA, Boone RS, Pignone MP. Literacy and Its Relationship With Self-efficacy, Trust, and Participation in Medical Decision Making. Am J Health Behav. 2007;31(Suppl 1):S27–S35. doi: 10.5993/AJHB.31.s1.5. [DOI] [PubMed] [Google Scholar]
- 29.Mbaezue N, Mayberry R, Gazmararian J, Quarshie A, Ivonye C, Heisler M. The impact of health literacy on self-monitoring of blood glucose in patients with diabetes receiving care in an inner-city hospital. J Natl Med Assoc. 2010;102:5–9. doi: 10.1016/s0027-9684(15)30469-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wallace AS, Carlson JR, Malone RM, Joyner J, DeWalt DA. The influence of literacy on patient-reported experiences of diabetes self-management support. Nursing Research. 2010;59:356–363. doi: 10.1097/NNR.0b013e3181ef3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arthur SA, Geiser HR, Arriola KR, Kripalani S. Health literacy and control in the medical encounter: A mixed-methods analysis. J National Med Assoc. 2009;101:677–683. doi: 10.1016/s0027-9684(15)30976-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ishikawa H, Yano E, Fujimori S, Kinoshitac M, Yamanouchic T, Yoshikawad T, et al. Patient health literacy and patient-physician information exchange during a visit. Family Practice. 2009;26:517–523. doi: 10.1093/fampra/cmp060. [DOI] [PubMed] [Google Scholar]
- 33.Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, Lopez A, et al. The literacy divide: Health literacy and the use of an internet-based patient portal in an integrated health system-results from the diabetes study of northern California (DISTANCE) J Health Comm. 2010;15(Suppl 2):183–196. doi: 10.1080/10810730.2010.499988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mayberry LS, Kripalani S, Rothman RL, Osborn CY. Bridging the digital divide in diabetes: Family support and implications for health literacy Diabetes Tech Therapeut. 2011;13(10):1005–12. [DOI] [PMC free article] [PubMed]
- 35.Laramee AS, Morris N, Littenberg B. Relationship of literacy and heart failure in adults with diabetes. BMC Health Serv Res. 2007;7:98. [DOI] [PMC free article] [PubMed]
- 36.Aikens J, Piette J. Diabetic patients’ medication underuse, illness outcomes, and beliefs about antihyperglycemic and antihypertensive treatments. Diabetes Care. 2009;32:19–24. doi: 10.2337/dc08-1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lyles C, Karter AJ, Young BA, Spigner C, Grembowski D, Schillinger D, et al. Correlates of patient-reported racial/ethnic health care discrimination in the diabetes study of northern California (DISTANCE) J Health Care Poor Underserved. 2011;22:211–225. doi: 10.1353/hpu.2011.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cavanaugh K, Wallston KA, Gebretsadik T, Shintani A, Huizinga MM, Davis D, et al. Addressing literacy and numeracy to improve diabetes care: Two randomized controlled trials. Diabetes Care. 2009;32:2149–2155. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Osborn CY, Bains SS, Egede LE. Health literacy, diabetes self-care, and glycemic control in adults with type 2 diabetes. Diabetes Tech Therapeut. 2010;12:913–919. doi: 10.1089/dia.2010.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.White RO, Osborn CY, Gebretsadik T, Kripalani S, Rothman RL. Development and validation of a Spanish diabetes-specific numeracy measure: DNT-15 Latino Diabetes Tech Therapeut. 2011;13(9):893–8. [DOI] [PMC free article] [PubMed]
- 41.Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Saha S, Snyder A, et al. Variation in Estimates of Limited Health Literacy by Assessment Instruments and Non-Response Bias. J Gen Intern Med. 2010;25(7):675–681. doi: 10.1007/s11606-010-1304-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wolf MS, Feinglass J, Thompson J, Baker DW. In search of ‘low health literacy’: threshold vs. gradient effect of literacy on health status and mortality. Soc Sci Med. 2010;70(9):1335–1341. doi: 10.1016/j.socscimed.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 43.Al Sayah F, Williams B, Johnson JA. Are we failing at measuring health literacy in individuals with diabetes? A review and appraisal of available measures Health Behavior and Education. In press. [DOI] [PubMed]
- 44.Schisterman EF, Cole SR, Platt RW. Overadjustment Bias and Unnecessary Adjustment in Epidemiologic Studies. Epidemiology. 2009;20(4):488–495. doi: 10.1097/EDE.0b013e3181a819a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Herndon JB, Chaney M, Carden D. Health literacy and emergency department outcomes: a systematic review. Ann Emerg Med. 2011;57(4):334–345. doi: 10.1016/j.annemergmed.2010.08.035. [DOI] [PubMed] [Google Scholar]
- 46.Easton P, Entwistle VA, Williams B. Health in the ‘hidden population’ of people with low literacy. A systematic review of the literature. BMC Public Health. 2010;5(10):459. [DOI] [PMC free article] [PubMed]
- 47.Sanders LM, Federico S, Klass P, Abrams MA, Dreyer B. Literacy and child health: a systematic review. Arch Pediatr Adolesc Med. 2009;163(2):131–140. doi: 10.1001/archpediatrics.2008.539. [DOI] [PubMed] [Google Scholar]
- 48.DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124(Suppl 3):S265–S274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 49.Keller DL, Wright J, Pace HA. Impact of health literacy on health outcomes in ambulatory care patients: a systematic review. Ann Pharmacother. 2008;42(9):1272–1281. doi: 10.1345/aph.1L093. [DOI] [PubMed] [Google Scholar]
- 50.Rothman R, DeWalt D, Malone B, Bryant B, Shintani A, Crigler B, et al. Influence of patient literacy in the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292:1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 51.Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, et al. Closing the loop: Physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 52.Schillinger D, Bindman A, Wang F, Stewart F, Stewart A, Piette J. Functional health literacy and the quality of physician–patient communication among diabetes patients. patient. Patient Educ Couns. 2004;52:315–323. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 53.Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121:245–254. doi: 10.1177/003335490612100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thabit H, Shah S, Nash M, Brema I, Nolan JJ, Martin G. Globalization, immigration and diabetes self-management: an empirical study amongst immigrants with type 2 diabetes mellitus in Ireland QJM. Int J Med Publ Health. 2009;102(10):713–720. doi: 10.1093/qjmed/hcp113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 190 kb)