ABSTRACT
BACKGROUND
Hospital discharge planning is required as a Medicare Condition of Participation (CoP), and is essential to the health and safety for all patients. However, there have been no studies examining specific hospital discharge processes, such as patient education and communication with primary care providers, in relation to hospital 30-day risk standardized mortality rates (RSMRs) for patients with acute myocardial infarction (AMI).
OBJECTIVE
To identify hospital discharge processes that may be associated with better performance in hospital AMI care as measured by RSMR.
DESIGN
We conducted a qualitative study of U.S. Hospitals, which were selected based on their RSMR reported by the Centers for Medicare & Medicaid Services (CMS) Hospital Compare website for the most recent data available (January 1, 2005 – December 31, 2007). We selected hospitals that ranked in the top 5 % and the bottom 5 % of RSMR for the two consecutive years. We focused on hospitals at the extreme ends of the range in RSMR, known as deviant case sampling. We excluded hospitals that did not have the ability to perform percutaneous coronary intervention in order to decrease the heterogeneity in our sample.
PARTICIPANTS
Participants included key hospital clinical and administrative staff most involved in discharge planning for patients admitted with AMI.
METHODS
We conducted 14 site visits and 57 in-depth interviews using a standard discussion guide. We employed a grounded theory approach and used the constant comparative method to generate recurrent and unifying themes.
KEY RESULTS
We identified five broad discharge processes that distinguished higher and lower performing hospitals: 1) initiating discharge planning upon patient admission; 2) using multidisciplinary case management services; 3) ensuring that a follow-up plan is in place prior to discharge; 4) providing focused education sessions for both the patient and family; and 5) contacting the primary care physician regarding the patient’s hospitalization and follow-up care plan.
CONCLUSION
Comprehensive and more intense discharge processes that start on admission continue during the patient’s hospital stay, and follow up with the primary care physician within 2 days post-discharge, may be critical in reducing hospital RSMR for patients with AMI.
KEY WORDS: discharge planning, acute myocardial infarction, risk standardized mortality rates, qualitative study
INTRODUCTION
Despite the national focus on improving quality of hospital care for patients with acute myocardial infarction (AMI), hospital variation in 30-day mortality rates for patients with AMI is substantial, even after adjusting for the patient’s clinical characteristics. Recent national data have shown a nearly two-fold difference in risk-standardized 30-day mortality rates (RSMRs) after AMI between the highest and lowest performing hospitals.1 Although hospital structural factors such as percutaneous coronary intervention (PCI) capability, teaching status, geographic location, and volume are modestly associated with RSMR, these factors leave much of the variation in RSMR unexplained.2,3
Although recent work 4 has indicated that hospitals with top performance in RSMR excelled in communication and coordination among departments and disciplines, previous studies have not investigated discharge processes that may contribute to RSMR. Because one-third of the deaths that contribute to RSMR occur after discharge from the hospital,5 effective discharge processes such as patient education and communication with primary care providers may be helpful in lowering hospital RSMRs. We hypothesized that if patients and family caregivers had an understanding of the patient’s plan of care, adverse events or outcomes might decrease, and hence, possibly reduce hospital RSMR rates. For example, effective discharge planning that includes patient and caregiver education, as well as early cardiology follow-up, may ensure adherence to and titration of important medications and prompt recognition of signs and symptoms, which may mitigate risks of acute illness or early mortality.
Accordingly, we sought to understand the role of discharge processes in RSMR for patients with AMI. We used a positive deviance approach6,7 to understand the role of discharge processes in RSMR for patients with AMI. We employed this approach in our earlier research, developing hypotheses in the area of what hospitals are doing to reduce RSMR for patients with AMI.4 Our initial work4 sought to broadly understand the features of hospitals’ organizational environment and care practices for patients with AMI. In the present study, we sought to examine in greater depth a core concept that emerged from the earlier work: the discharge process.
METHODS
Study Design and Sample
We conducted a qualitative study of key hospital clinical and administrative staff most involved in the care of patients admitted with AMI. The qualitative approach is beneficial in contributing a deeper understanding of complex phenomena, such as discharge planning, from the perspective of many different disciplines.8 We selected hospitals based on their RSMR reported by the Centers for Medicare & Medicaid Services (CMS) Hospital Compare website for the most recent data available (January 1, 2005 – December 31, 2007) (CMS.gov., Hospital Compare). The outcome was calculated by dividing the actual number of deaths within 30 days of admission at each hospital by the expected number of deaths within 30 days of admission, and multiplying the ratio by the overall 30-day mortality rate of the cohort (e.g. patients with AMI).9,10
In order to gain an in-depth understanding about discharge processes, we used purposeful sampling;11 we sought hospitals that had both higher and lower RSMR performance. Hospitals were arrayed in the top 5 % of RSMR from lowest (e.g., higher performing) to highest RSMR. Hospitals in the bottom 5 % were arrayed from highest (e.g., lower performing) to lowest RSMR. We started at the beginning of each list and worked our way down. If a hospital declined to participate, we moved onto the next hospital on the list. Among the hospitals we selected, we paid particular attention to ensuring diversity in hospital characteristics, such as geographic location, size, socioeconomic status, and teaching status; as these are the factors that have been shown to be important correlates with AMI mortality rates.2 We excluded hospitals that did not have the capability to perform primary percutaneous coronary intervention in order to decrease the heterogeneity in our sample. We conducted site visits until we reached the point of theoretical saturation (i.e., when no new concepts were identified by additional interviews), which occurred after 14 hospital site visits. We retained 11 of the hospitals in the sample for analysis because their RSMR performance remained in the top 5 % or bottom 16 % during 2007–2008 (the performance data most proximal to the data collection period), as we were focusing on the hospitals at the most extreme ends of the range (extreme or deviant case sampling) in order to maximize the opportunity to learn from their experiences.11
Data Collection
Data collection was carried out by an interdisciplinary team of researchers from cardiology, public health, nursing, social work, emergency medicine and organizational psychology. Site visits were conducted from December 2008 to December 2009, and focused on the previous years of activity; three to four researchers from the team attended each site visit. Prior to the site visits, team members participated in a training session on conducting qualitative interviews that was presented by an expert member on the team in qualitative methodology.
Within each hospital, the first person contacted was most often the Director of Quality or Performance Improvement. Each hospital included an interview with at least one physician, nurse and administrative staff member and the remaining interviews varied by site, as the hospital contact person coordinating the visit selected staff with the greatest knowledge regarding care of AMI patients or hospital quality improvement efforts in the care of patients with AMI. We conducted 158 in-depth interviews;12,13 a total of 57 participants had roles specifically related to discharge planning. Site visit interviews were conducted over 1–2 days; each interview lasted approximately 1 h, followed a standard discussion guide, and was audio-taped and professionally transcribed.
Data Analysis
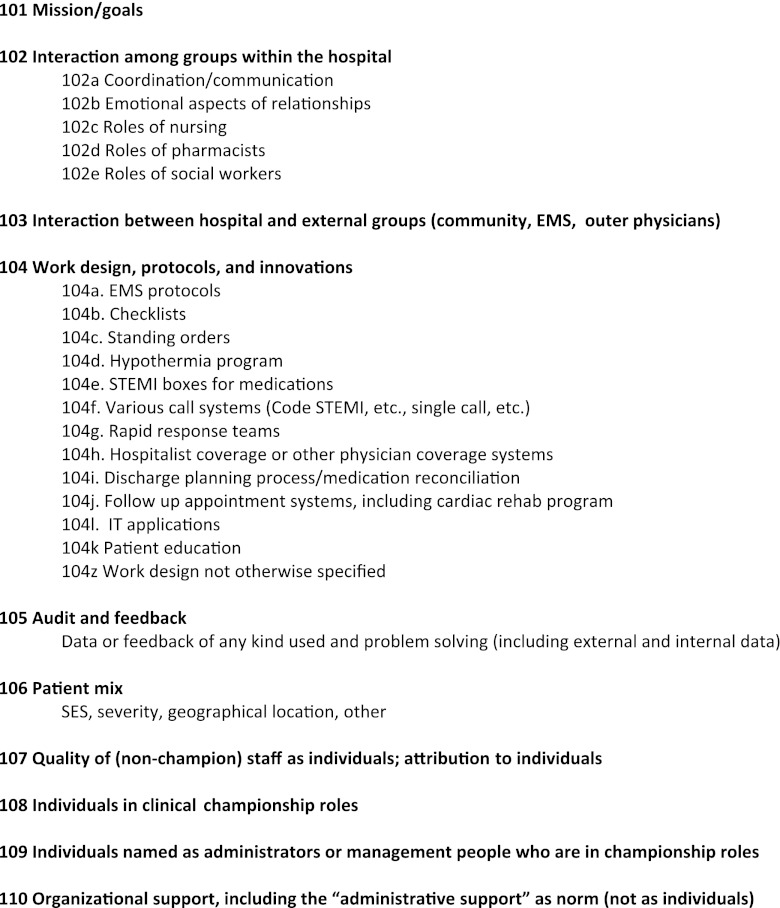
Using a grounded theory approach,12 we generated themes inductively from participant’s expressed perspectives rather than testing of predetermined hypotheses. All six coding team members independently reviewed two to three transcripts at a time, applying codes to text segments as concepts became apparent, and then convening on a regular basis to negotiate consensus over differences in code structure. We used the constant comparative method,11,12,14 iteratively comparing coded transcript segments to previously coded segments to identify novel concepts, ensure consistent identification of emerging themes, and expand or refine codes. The final code structure included ten main codes and 18 subcodes (Fig. 1). In this study, a focused analysis of these data was carried out to examine the discharge practices in depth. Three members of the research team [EJC, LAC, EHB] focused on four codes developed in our earlier study:4 role of social workers; discharge planning and medical reconciliation; follow-up appointment systems including cardiac rehab programs; and patient education. Applying the constant comparative method,11,12,14 we identified prominent differences in themes between higher and lower performing hospitals. The final code structure for this present study included five main codes (Fig. 2).
Figure 1.
Original code structure.
Figure 2.
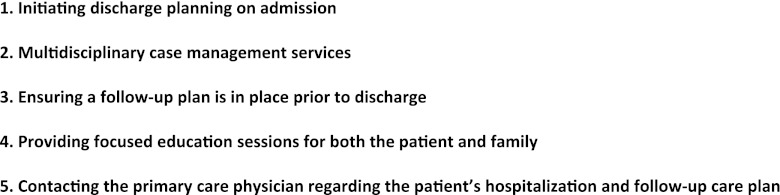
Discharge planning code structure.
We used ATLAS.TI Scientific Software, version 6.2 (ATLAS.ti. Berlin, Germany) in data analysis. All research procedures were approved by the Institutional Review Board at Yale University School of Medicine.
RESULTS
The sample of hospitals included a diverse set of hospitals based on RSMR, geographic location, and socioeconomic status15,16 of their patients with AMI (Table 1). To measure the socioeconomic profile of the hospital’s patient population, we used a ZIP code level socioeconomic status (SES) score developed by Claritas, Inc (Los Angeles, CA). We classified each patient according to the SES score assigned to their ZIP code. We identified quintiles of the SES scores and patients were coded 1 if they resided in a ZIP code whose SES score was in the lowest quintile of SES scores and 0 otherwise. For each hospital, we then calculated the percentage of Medicare AMI discharges that were categorized as residing in ZIP code areas with SES scores in the lowest quintile of SES scores. Interview participants (n = 57) included physicians, nurses, social workers, administration and quality improvement (QI) personnel (Table 2). Discharge processes at the higher versus lower performing hospitals were both more comprehensive in scope and more intense in nature. Furthermore, five broad features of discharge processes distinguished higher and lower performing hospitals; each theme was prominent in the higher performing hospitals and less apparent in the lower performing hospitals.
Table 1.
Description of Study Sample (Hospitals)
| Hospital ID | Region | % of Patients from Low Socioeconomic Zip codesa | RSMR %b | Ownership status | Teaching status | Performance statusc | |
|---|---|---|---|---|---|---|---|
| 05-06 06-07 | |||||||
| 1 | Pacific | 8.1 | 13.4 | 13.4 | Nonprofit | Yes | High |
| 2 | East North Central | 30.7 | 13.8 | 12.8 | Nonprofit | Yes | High |
| 3 | Middle Atlantic | 14.0 | 13.4 | 13.3 | Nonprofit | Yes | High |
| 4 | New England | 19.4 | 13.1 | 13.3 | Nonprofit | Yes | High |
| 5 | New England | 5.6 | 13.3 | 13.4 | Nonprofit | Yes | High |
| 6 | Middle Atlantic | 1.9 | 14.0 | 13.2 | Nonprofit | Yes | High |
| 7 | East North Central | 4.9 | 11.4 | 14.0 | Nonprofit | No | High |
| 8 | South Atlantic | 44.2 | 18.6 | 19.1 | Nonprofit | Yes | Low |
| 9 | South Atlantic | 25.3 | 17.9 | 18.7 | Nonprofit | No | Low |
| 10 | West South Central | 20.8 | 20.9 | 19.6 | Government | No | Low |
| 11 | East North Central | 0.0 | 20.6 | 19.9 | Nonprofit | No | Low |
a Percentage of patients with AMI in that hospital who were from ZIP codes rated in the lowest quintile of socioeconomic status, as measured by the Socioeconomic Status scale
bRSMR Risk-standardized mortality rate
cPerformance status: High performance status means low RSMR rates; Low performance means high RSMR rates
Table 2.
Description of Study Sample (Participants)
| Participants | No. in Sample (n = 57) |
|---|---|
| Physicians | |
| Emergency medicine physicians | 1 |
| Interventional cardiologists | 1 |
| Cardiac fellow | 2 |
| Hospitalist | 2 |
| Nurses | |
| Nurse managers | 7 |
| Case managers | 7 |
| Cardiac services | 1 |
| Emergency department nurses | 1 |
| Catheterization laboratory nurses | 1 |
| Critical care nurses | 2 |
| Clinical nurse specialist (CNS) | 1 |
| Cardiac research coordinator | 3 |
| Nursing educator | 2 |
| Nurse practitioner | 1 |
| Administration | |
| Chief medical officers | 3 |
| Chief executive officer | 1 |
| Chief quality officer | 1 |
| Chief of emergency medicine | 3 |
| Chief of cardiology services | 1 |
| Director of cardiac rehabilitation | 1 |
| Director of critical care | 1 |
| Director of catheterization laboratory | 1 |
| Director of pharmocotherapy | 1 |
| Director of quality management | 1 |
| Chairman of cardiology | 1 |
| Chairman of emergency medicine | 2 |
| Vice presidents and presidents | 2 |
| Administrative director of patient care | 1 |
| Administrative director of nursing operations | 1 |
| Clinical staff | |
| Quality management staff | 2 |
| Social workers | 2 |
| Total | 57 |
Theme 1: Initiating Discharge Planning Upon Patient Admission
Participants in the higher performing hospitals described discharge planning efforts that began very early in a patient’s stay. Some hospitals had care managers focused specifically on patients with AMI from the moment they came into the hospital:
“From the minute they come in they [care managers] are focusing on what is to be done and to get the patient out and what is the discharge plan.” (Chief Medical Officer, ID#3)
In addition, participants from the higher performing hospitals indicated that it was important to be proactive from the beginning of a patient’s admission in order to prepare for a patient’s discharge. For nurses, who often initiated the discharge process, early preparation for discharge meant getting other staff (e.g., social work, discharge planners) involved early on, to learn as much as possible about the patient’s post-discharge situation and supports:
“I would say from a nursing point of view, what we do initially on admission is to ask the key question, ‘Do you live alone?’ So we ask key questions and start looking at the possible discharge needs from the start. And so, probably from that point on, we’ll put in a referral to discharge planning or social work.” (Nurse Manager, ID #5)
Participants from the lower performing hospitals did not describe initiating discharge planning early on in the patient’s hospital stay. Rather, planning occurred at the end of the patient’s hospital stay, and focused on compliance with guidelines in contrast to a more comprehensive assessment of individual patient circumstances and needs:
“Right before we’re ready to discharge them, [we] do all their education. And they do a good job of that I think…I know the nurses are supposed to fill out some more education forms and we go over them with the patient to comply with the guidelines.” (Hospitalist, ID#9)
Theme 2: Multidisciplinary Case Management Services
Case management services varied among all the hospitals. In the higher performing hospitals, case management was carried out by multidisciplinary teams in which nurses reviewed medications, social workers managed the more complicated cases, and ancillary staff (e.g., pharmacists, nutritionists) counseled patients about medication instructions and dietary needs. A case manager from one higher performing hospital described the thoroughness of case management that was also evident in other higher performers:
“We look to see what happened to the patient, why he was admitted, what procedures were done on him, and what tests are currently being ordered. We would then go in and talk with the patient, find out his living situation. If he was living alone, if he had a family, what kind of support system, how independent he was. If it’s someone that’s elderly, we might need physical therapy and if the doctor hasn’t ordered it, we’ll call and try to get an order and we also have a program here called cardiac rehab.” (RN Case Manager, ID #1)
While we found evidence of coordination between disciplines to balance patient needs at higher performing hospitals, especially between nursing and social work, the discharge planning activities at the lower performing hospitals were less coordinated between disciplines. In one of the lower performing hospitals, a nurse indicated that the social workers were all replaced with RN case managers. In contrast to evaluating the patient’s needs post-discharge, discharge planning in the lower performing hospitals focused on meeting the requirements to get the patient out of the hospital:
“That really comes down to resources and our case management social work department is very much hospital-based. Sort of like a typical hospital-based program. They do all the utilization review, getting all the authorizations and coordinating the discharge planning, and you know, then their work ends there.” (Director, Quality Improvement, ID#8)
Theme 3: Ensuring a Follow-up Plan is in Place Prior to Discharge
Participants at higher performing hospitals uniformly discussed the importance of follow up after the patient was discharged. In higher performing hospitals, the staff indicated that patients were not discharged unless a plan was in place:
“We do not let anyone out the door unless we know they’re going to have some follow-up and that they’re able to pay for Plavix, which they need.” (Case Manager, ID#5).
Additionally, in higher-performing hospitals, staff expressed a shared recognition of the importance of follow-up, calling patients after discharge to address questions about their care and medications, and ensuring that patients were aware and understood what was expected post-discharge.
“You sit down with a patient and say ‘who’s your follow-up cardiologist going to be?’ Well, it’s going to be this person —and we talk to that person. We give them a discharge summary. We make sure that the patient knows that there is a follow-up for cardiology. What to expect when they see them in a week or two. What to expect from rehab. Rehab ingrains in them what’s going to happen when they get involved with the rehab program…So, it really requires a culture of working together pointed towards what’s best for the patient.” (Interventional Cardiologist, ID#4).
Although participants at lower performing hospitals indicated an obligation to educate patient about their medications and the importance of following up with their physicians after discharge, it was apparent that this was not uniformly accomplished:
“We have a rule you’re supposed to call your consultant, primary care or anybody but people were really not doing it. So we have tried to make on our order form, you know, a box on the top …consult Dr. So and so and the rule is if you want the doctor to see the patient that day, you have to call the doctor yourself. If it’s a routine consult, the secretary can call. And then the doctor can come and see the patient next day. So that’s basically the rules. Some people follow. Others don’t” (Cardiologist, ID#9)
Theme 4: Providing Focused Education Sessions for Both the Patient and Family
A strong focus on education for both patient and family members was apparent across disciplines at higher performing hospitals. Staff repeatedly emphasized the completeness of the education, covering all aspects to meet patient’s needs:
“They’ll get multiple sessions where they’re [the patient] inquired about what their experience is, what their needs are, and what other reinforcements they might like, what other assistance we can give them. We’re very thorough about our instructions…exercise, diet, risk factor modification, the impact of diabetes. We try to make connections all the time with how everything works together and how improvement in one area will definitely make improvements in others.” (Nurse Practitioner, ID#3)
Similarly, physicians focused on extending education more broadly to families, so that they understand what happened and the course of action once the patient returns home, emphasizing the families’ pivotal role post-discharge:
“I try to talk to the spouses several times before they leave. Educate them as to what happened…there is a whole culture…Get the family involved and they will support the compliance with medication and smoking cessation and diet. Find out who cooks at home. And have the rehab talk with the person that actually cooks at home. If we don’t arrange good follow-up, then the patient is sometimes left out to the wind.” (Interventional Cardiologist, ID#4)
The shared focus across disciplines in providing education to patients and families was not apparent in the lower performing hospitals. Rather than providing multiple educational sessions throughout the patients’ stays, staff described patient education taking place just prior to discharge:
“There are special nurse educators for MIs (myocardial infarctions) and CHF (congestive heart failure) and things like that. So they always get to the patients you know, right before we’re ready to discharge them and do all their education.” (Hospitalist, ID#9)
Theme 5: Contacting the Primary Care Physician Regarding the Patient’s Hospitalization and Follow-up Care Plan
Follow-up with patients post-discharge was commonly described in the higher performing hospitals as ensuring that the primary care physician was contacted after discharge regarding the patient’s experience while in the hospital, often within 1–2 days after discharge. This was described for patients who lived both close to and farther from the hospital:
“We do have a high volume of patients from outside the area, there is always…almost always a discharge letter that the attending cardiologist here will send to the patient’s home physician, and I think that’s really important because that kind of summarizes what happened here. So that physician knows maybe what problems were encountered, what was done here, and of course the medication list. I think that helps reconnect them with their home physician and that’s real important when they are not from this area.” (Cardiovascular Manager, ID#3)
Although passing discharge information to the primary care physician was reported by staff at the lower performing hospitals, the onus was on the patient for providing such information to the primary care physician:
“That’s something we are trying to change. We have been trying to set up a process where the discharge summaries are actually going to the doctor directly; we have never done that before. Basically, we were telling the patient that they would get a discharge summary that was transcribed by the nurse, based on the physician’s summary, and we would tell them to bring that to their physician, and they could call us if they need us.” (Hospitalist, ID#11)
DISCUSSION
We found distinct differences in discharge processes between the higher and lower performers. These included initiating discharge planning on admission, multidisciplinary case management services, ensuring a follow-up plan prior to discharge, education for patients and families, and contacting the primary care physician regarding the patient’s hospitalization and follow-up plan. Although previous research has identified factors that limit the quality of discharge practices,17 to our knowledge, no study has explored discharge practices in relation to 30-day mortality rates. Our study extends this research by suggesting that staff at the high performing hospitals effectively leveraged multidisciplinary teams and viewed discharge processes as broad and inclusive, beginning from the moment they met the patient and continuing after the patient was discharged from the hospital.
The multidisciplinary nature of case management found in the higher performing hospitals is consistent with our earlier research that indicated communication and coordination across disciplines was evident in the higher performing hospitals.4 In the present study, it was evident in the higher performing hospitals that coordination among varying disciplines within the hospital was viewed as important for smooth transitions in care for patients with AMI. Previous studies have indicated that collaborative teams are important in the quality and safety of patient care—including the presence of physicians on the team.4,18–20 Although discharge planning activities are frequently thought to be assigned to the social work department in hospitals, we found that at higher performing hospitals other hospital staff, including nurses and cardiologists, were reported to be involved in making sure patients understood the importance of follow-up care. Multidisciplinary involvement has also been linked to quality improvement for patients with chronic illness,20 increased patient satisfaction,21 and improvement in core measure performance for congestive heart failure (CHF), pneumonia, and AMI,22 and improved adherence to evidence-based guidelines.23 Furthering this work, we suggest that effective discharge processes may also be related to improved post-hospital survival rates.
The Medicare Conditions of Participation (CoP) provide guidance for hospital discharge planning processes,24 although the requirements are general in nature. For instance, hospitals must identify patients in need of discharge planning at an early stage of hospitalization and provide a discharge plan if indicated. Our findings suggest that specific processes may be important to patients’ 30-day survival after AMI, such as involving a multidisciplinary team in discharge planning, calling patients post-discharge, ensuring primary care physicians have the discharge summary, and focusing on families’ educational needs so they understand what is needed to assist or manage the patient’s care post-discharge. For example, having a process in place to call patients within 72 h after discharge and assess if they understand the discharge instructions (e.g., dietary restrictions) may avert complications.
The study has several limitations. First, we visited hospitals at a single point in time. It is possible that the low performing hospitals were on a trajectory towards improvement that was not captured in our data. However, we did compute RSMRs over a three-year period among selected hospitals and found little movement in rank among them. Second, social desirability response bias,25 in which participants may have misrepresented their improvement efforts in order to provide desirable answers, may have occurred. Third, hospitals were unable to be ‘blinded’ as to the reason for selection, potentially resulting in response bias, such as lower performing hospitals highlighting more negative aspects of care. Fourth, we used purposeful sampling,11 which does not allow for generalizability and assurance that the same types of hospital representatives were interviewed. However, we interviewed multiple staff in each hospital, using scripted probes to encourage the disclosure of details that would be difficult to misrepresent, and instructed respondents to share both positive and negative experiences. Fifth, while we identified discharge processes in higher performing hospitals that were not present in lower performing hospitals, we were not able to identify how hospitals are able to sustain consistency in their discharge planning process in this qualitative study. Last, it is plausible that the distinguishing features we identified between the high and lower performing hospitals resulted from factors we were not able to explore in the current study. However, our sample included hospitals that were diverse in characteristics such as RSMR, geographic location, socioeconomic status15,16 of their patients with AMI, and teaching status (Table 1).
Understanding key discharge planning processes is important to improving the care patients receive in the hospital as well as their transition out of the hospital. As hospitals staff are facing increased accountability in improving outcomes such as mortality and readmission rates, exploring features of higher performing hospitals provides insight into effective practices. Consistent with our previous work,4,9 changes in hospital discharge processes will require substantial investment in improving communication among different departments and creating an organization culture that focuses on creative problem-solving. These investments will likely take time to be effective for hospitals to improve discharge processes and reduce RSMR.
In the last decade, we have generated evidence to improving hospital performance in beta-blocker use,26,27 door-to-balloon (D2B) time18,28 and AMI care.4,9 This evidence has been generated using a positive deviance, mixed methods approach.6,7 The next logical step to improving discharge planning performance would be to quantitatively examine the five broad features we identified and hospital RSMR. Further, to address the variation in hospital discharge planning, future research might include the utilization of measures of organizational culture29 and organizational readiness.30
Acknowledgements
Funding and support were provided by the Agency for Healthcare Research and Quality (AHRQ RO1-HS0-16929-1), the United Health Foundation, and the Commonwealth Fund. Dr. Krumholz was supported by grant U01 HL105270-02 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. We thank Yongfei Wang and the Multidisciplinary Team for their research contributions.
Conflict of Interest
Dr. Krumholz discloses that he is the recipient of a research grant from Medtronic, Inc. through Yale University and is chair of a cardiac scientific advisory board for UnitedHealth. All other authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, Wang Y, Wang Y, Lin Z, Straube BM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circulation: Cardiovasc Qual Outcomes. 2009;5:407–413. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 2.Bradley EH, Herrin J, Curry L, Cherlin EJ, Wang Y, Webster TR, Drye EE, Normand SL, Krumholz HM. Variation in hospital mortality rates for patients with acute myocardial infarction. Am J Cardiol. 2010;106:1108–1112. doi: 10.1016/j.amjcard.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 3.Chen J, Krumholz HM, Wang Y, Curtis JP, Rathore SS, Ross JS, Normand SL, Schreiner GC, Mulvey G, Nallamothu BK. Differences in patient survival after acute myocardial infarction by hospital capability of performing percutaneous coronary intervention: implications for regionalization. Arch Intern Med. 2010;170:433–439. doi: 10.1001/archinternmed.2009.538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Curry LA, Spatz E, Cherlin E, Thompson JW, Berg D, Ting HH, Decker C, Krumholz HM, Bradley EH. What distinguishes top-performing hospitals in acute myocardial infarction mortality rates? A qualitative study. Ann Intern Med. 2011;154:384–390. doi: 10.7326/0003-4819-154-6-201103150-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drye EE, Normand SL, Wang Y, Ross JS, Schreiner GC, Han L, Rapp M, Krumholz HM. Comparison of hospital risk-standardized mortality rates calculated by using in-hospital and 30-day models: an observational study with implications for hospital profiling. Ann Intern Med. 2012;156:19–26. doi: 10.1059/0003-4819-156-1-201201030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradley EH, Curry LA, Ramanadhan S, Rowe L, Nembhard IM, Krumholz HM. Research in action: using positive deviance to improve quality of health care. Implement Sci. 2009;4:25. doi: 10.1186/1748-5908-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krumholz HM, Curry LA, Bradley EH. Survival after acute myocardial infarction (SAMI) study: the design and implementation of a positive deviance study. Am Heart J. 2011;162:981–987. doi: 10.1016/j.ahj.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119:1442–1452. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 9.Bradley EH, Curry L, Spatz ES, Herrin J, Cherlin EJ, Curtis JP, Thompson JW, Ting HH, Wang Y, Krumholz HM. Hospital strategies for reducing risk-standardized mortality rates in acute myocardial infarction. Ann Intern Med. 2012;156:618–626. doi: 10.1059/0003-4819-156-9-201205010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krumholz HM, Wang Y, Mattera JA, Han LF, Ingber MJ, Roman S, Normand SL. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113:1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 11.Patton M. Qualitative research and evaluation methods. 3. Thousand Oaks: Sage Publications; 2002. [Google Scholar]
- 12.Glaser B, Strauss A. The discovery of grounded theory: Strategies for qualitative research. Chicago: Aldine Publishing Company; 1967. [Google Scholar]
- 13.McCracken G. The long interview. Newbury Park: Sage Publications; 1988. [Google Scholar]
- 14.Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2. Thousand Oaks: Sage Publications; 1994. [Google Scholar]
- 15.Nielson Claritas Inc. Population Facts 2009. Los Angeles: Nielson Claritas; 2009.
- 16.Rathore SS, Masoudi FA, Wang Y, Curtis JP, Foody JM, Havranek EP, Krumholz HM. Socioeconomic status, treatment, and outcomes among elderly patients hospitalized with heart failure: findings from the National Heart Failure Project. Am Heart J. 2006;152:371–378. doi: 10.1016/j.ahj.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greysen SR, Schiliro D, Horwitz LI, Curry L, Bradley EH. ‘Out of sight, out of mind’: housestaff perceptions of quality-limited factors in discharge teaching hospitals. J Hosp Med. 2012;7:376–381. doi: 10.1002/jhm.1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bradley EH, Curry LA, Webster TR, Mattera JA, Roumanis SA, Radford MJ, McNamara RL, Barton BA, Berg DN, Krumholz HM. Achieving rapid door-to-balloon times: how top hospitals improve complex clinical systems. Circulation. 2006;113:1079–1085. doi: 10.1161/CIRCULATIONAHA.105.590133. [DOI] [PubMed] [Google Scholar]
- 19.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004;13(Suppl 1):i85–i90. doi: 10.1136/qshc.2004.010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shortell SM, Marsteller JA, Lin M, Pearson ML, Wu SY, Mendel P, Cretin S, Rosen M. The role of perceived team effectiveness in improving chronic illness care. Med Care. 2004;42:1040–1048. doi: 10.1097/00005650-200411000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Meterko M, Mohr DC, Young GJ. Teamwork culture and patient satisfaction in hospitals. Med Care. 2004;42:492–498. doi: 10.1097/01.mlr.0000124389.58422.b2. [DOI] [PubMed] [Google Scholar]
- 22.O’Mahony S, Mazur E, Charney P, Wang Y, Fine J. Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay. J Gen Intern Med. 2007;22:1073–1079. doi: 10.1007/s11606-007-0225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ellrodt G, Glasener R, Cadorette B, Kradel K, Bercury C, Ferrarin A, Jewell D, Frechette C, Seckler P, Reed J, et al. Multidisciplinary rounds (MDR): an implementation system for sustained improvement in the American Heart Association’s Get With The Guidelines program. Crit Pathw Cardiol. 2007;6:106–116. doi: 10.1097/HPC.0b013e318073bd3c. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Government Printing Office: Conditions of Participation: Discharge Planning. Conditions of Federal Regulations Title 42, Pt. 482.43. In Book Conditions of Participation: Discharge Planning. Conditions of Federal Regulations Title 42, Pt. 482.43 (Editor ed.^eds.). City; 2009.
- 25.Sudman S, Bradburn NM, Schwarz N. Thinking about answers: The application of cognitive processes to survey methodology. San Francisco: Jossey-Bass Publishers; 1996. [Google Scholar]
- 26.Bradley EH, Holmboe ES, Mattera JA, Roumanis SA, Radford MJ, Krumholz HM. A qualitative study of increasing beta-blocker use after myocardial infarction: why do some hospitals succeed? JAMA. 2001;285:2604–2611. doi: 10.1001/jama.285.20.2604. [DOI] [PubMed] [Google Scholar]
- 27.Bradley EH, Herrin J, Mattera JA, Holmboe ES, Wang Y, Frederick P, Roumanis SA, Radford MJ, Krumholz HM. Quality improvement efforts and hospital performance: rates of beta-blocker prescription after acute myocardial infarction. Med Care. 2005;43:282–292. doi: 10.1097/00005650-200503000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Bradley EH, Nallamothu BK, Herrin J, Ting HH, Stern AF, Nembhard IM, Yuan CT, Green JC, Kline-Rogers E, Wang Y, et al. National efforts to improve door-to-balloon time results from the Door-to-Balloon Alliance. J Am Coll Cardiol. 2009;54:2423–2429. doi: 10.1016/j.jacc.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Glaser SR, Zamanou S. Measuring and interpreting organizational culture. Manag Commun Q. 1987;1:173–198. doi: 10.1177/0893318987001002003. [DOI] [Google Scholar]
- 30.Helfrich CD, Li YF, Sharp ND, Sales AE. Organizational readiness to change assessment (ORCA): development of an instrument based on the Promoting Action on Research in Health Services (PARIHS) framework. Implement Sci. 2009;4:38. doi: 10.1186/1748-5908-4-38. [DOI] [PMC free article] [PubMed] [Google Scholar]