Abstract
Purpose
To describe the Intrauterine Contraception (IUC) adoption process among nulliparous adolescents and to identify the role of the medical provider in this trajectory.
Methods
We conducted semi-structured interviews with a clinic-based sample of twenty nulliparous adolescents (ages 15-24 years) with a history of IUC use. Interviews were analyzed using modified grounded theory and cross-case analysis to reveal a process model for IUC adoption with a focus on the role of the medical provider.
Results
The model includes the following stages: awareness, initial reaction, information gathering, adoption, and adjustment and reassessment. It is influenced by personal preferences and experiences, friends, family, sexual partner(s), and medical providers. Interactions with medical providers that study participants found helpful in navigating the adoption process included the use of visuals; tailored counseling to address specific contraceptive needs; assurance that IUC discontinuation was an option; information on a wide range of side effects; medical provider self-disclosure regarding use of IUC; and addressing and validating concerns both before and after IUC insertion.
Conclusions
Nulliparous adolescents in this study described a complex IUC adoption process in which the medical provider plays a substantial supportive role. Findings from this study may be used to counsel and support future nulliparous adolescents regarding IUC use.
Implications and Contribution Summary
Little is known about nulliparous adolescent use of IUC and the counseling needs of this population. This study offers counseling suggestions for medical providers that they may use to support nulliparous adolescents as they make decisions about IUC use.
Keywords: Intrauterine contraception, long-acting reversible contraception, nulliparous, adolescent, young adults, family planning counseling, provider self-disclosure
Unintended pregnancy disproportionately impacts adolescents—particularly those from racial/ethnic minority backgrounds—and is a major public health problem in the United States (1, 2). A significant contributor to unintended pregnancy in this age group is the incorrect or inconsistent use of contraception (3). Therefore, long-acting reversible contraceptives, such as intrauterine contraception (IUC), may play an important role in meeting the public health imperative to reduce unintended pregnancy among adolescents, as they are highly effective and have a low risk of user misuse (4).
Two forms of IUC are available for use in the United States: the hormonal levonorgestrel intrauterine system (LNG-IUS), which offers up to five years of pregnancy prevention, and the non-hormonal Copper T380 (Copper-T), which offers up to ten. However, only 1% of 15-19 year olds and 3.2% of 20-24 year olds use IUC (5). This is likely due to unsubstantiated concerns about infertility associated with IUC (6), adolescent lack of awareness regarding the method’s availability (7, 8), and provider hesitancy to insert IUC based on inaccurate knowledge of the method (9-12). Many of these issues are amplified for nulliparous adolescents despite the fact that the World Health Organization and American College of Obstetrics and Gynecologists recommends IUC for both adolescents and nulliparous women (13-15).
Professional organizations and researchers agree that counseling by medical providers can play a role in supporting the use of IUC, when appropriate, among nulliparous adolescents (7, 14, 16). However, little is known about the type of information and interactions nulliparous adolescents value from their medical providers when making decisions about IUC use. Because the healthcare provider is just one of many influences on adolescent contraceptive decision-making (17), counseling efforts may be more effective if providers are informed regarding the role they can play in adolescents’ decision to adopt IUC. Nulliparous adolescents with a history of IUC use are uniquely qualified to provide this information. In the current qualitative study, 20 nulliparous adolescents who had a history of IUC use and who were patients in a clinic serving a predominantly Latino and African-American population described their IUC adoption process. In particular, they identified the role of their medical provider in navigating this trajectory.
METHODS
Participants
A sample of 20 study participants was recruited between November 2010 and June 2011 from an adolescent family planning clinic in San Francisco. Clinic clients were eligible to participate if they were between 15-24 years of age, female, nulliparous, spoke English, and were a current or past user of IUC (LNG-IUS or Copper T) for at least one month within the previous two years. Most participants were recruited by provider referral. Several participants contacted the study’s lead investigator directly after reading flyers in the clinic. Participants received a $30 gift certificate upon completion. Study procedures were approved by the Institutional Review Boards at the University of California San Francisco and the University of California Berkeley.
Approximately half of those who were eligible for and contacted to be in the study ultimately participated. Those that did not participate primarily declined due to logistical barriers, such as transportation difficulties and scheduling conflicts. We did not collect data from those that declined participation.
Procedures
A qualitative approach was chosen because little is known about nulliparous adolescent IUC use or the context in which the method is adopted (18, 19). Participants gave written informed consent, participated in a one-hour in-person semi-structured interview with the lead author, and completed a brief demographic survey. The interview guide covered such topics as decision-making regarding IUC use (“Why did you get IUC?”), and clinical counseling experiences during this process (“What role did your provider play in helping you make your decision?”). Participants were also asked to provide counseling suggestions (“How should providers talk to young women about IUC?”). The interview guide is available upon request.
Analysis occurred in parallel with data collection, leading to iterative modification of the interview guide over time. Data collection ended when the study team felt they had reached saturation of dominant themes (20).
Data analysis
Facilitated by Atlas-TI software, the lead author used modified grounded theory to analyze the interviews (20). Through open coding (close reading of small segments of the first five transcripts), analytic categories were developed from which a preliminary codebook was made. Modifications to the codebook reflected emerging and changing codes that arose from the data. The development of the coding scheme was iterative and collaborative, with frequent meetings with the study team to review the interviews and coding structure and to discuss emerging categories. Summary memos regarding relationships between categories were drafted.
At the conclusion of preliminary analysis, a model to describe the process of IUC adoption emerged with a focus on the role of the medical provider. This preliminary model was derived primarily from participants’ experiences with IUC adoption and was also informed by Roger’s Diffusion of Innovations Model (21). The model was then tested using cross-case analysis, for which experiences described in individual interviews were compared to the provisional model (22). This comparison method allowed for a general understanding of the processes that occurred across cases while addressing the circumstances of each individual case (22). The process model is presented in the Results. Participants’ counseling recommendations are also reported.
RESULTS
Demographic Data
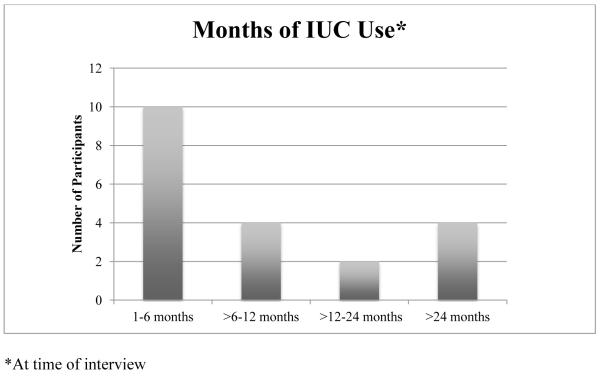
See Table 1 and Figure 1. All participants used IUC primarily for contraception.
Table 1.
Demographic Data (n=20), all participants nulliparous
| Participant Characteristics |
Percent of Participants |
Number of Participants |
|---|---|---|
| Age | ||
| 15-17 | 15 | 3 |
| 18-21 | 45 | 9 |
| 22-24 | 40 | 8 |
|
| ||
| Race/Ethnicity | ||
| Latina | 40 | 8 |
| African-American | 30 | 6 |
| Asian | 15 | 3 |
| White | 10 | 2 |
| Pacific Islander | 5 | 1 |
|
| ||
| IUC Type | ||
| LNG-IUS | 75 | 15 |
| Copper T | 25 | 5 |
|
| ||
| IUC Status | ||
| Current user | 80 | 16 |
| Past user | 20 | 4 |
|
| ||
|
Length of use
(months) |
17.5 (1-60) | |
| Mean (range) | ||
|
| ||
|
Number of prior
methods used |
||
| Mean (range) | 2.5 (0-5) | |
Figure 1.
Duration of IUC use
Qualitative Findings
Process Model
The process model for IUC adoption (Figure 2) includes the following stages: 1) first awareness, 2) initial reaction, 3) information gathering, 4) adoption, and 5) adjustment and reassessment. Each stage is described below.
Figure 2.
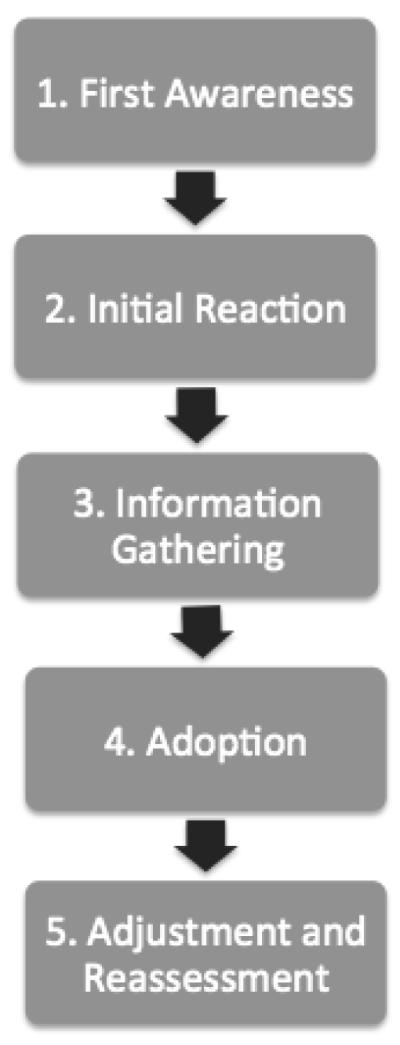
Process Model for IUC Adoption
1. First Awareness
Most participants first became aware of IUC after a conversation with their healthcare provider. Others heard about the method from a friend or family member, with a small minority being exposed to IUC from a media source. Many described a delayed awareness of the method. For example, providers rarely mentioned IUC during medical visits, friends and family members “never really talked about it” (Participant 4; 24-year-old LNG-IUS user) and the rare media source that advertised IUC presented it as inappropriate for nulliparous young women:
I think that it is a lack of media influence, and lack of information in these clinics that I was going to…. My gynecologist at that time was not really encouraging, or giving me information about [IUC]…I didn’t even know that it existed. Participant 19 (24-year-old Copper-T user)
Several participants stated that they would have used the method earlier had they known about it. Participant 8 (22-year-old LNG-IUS user) said: “[IUC] could have been talked about a little bit more. I had no clue about it and if I’d had a clue I would have chosen it back then over the shot.”
2. Initial reaction
After hearing about IUC, most participants described an initial negative reaction:
I felt like it would be really painful, hearing how it was inserted into your uterus. I thought, “Oh, I would not do that I couldn’t…cause it sounds so scary.” Participant 7 (18-year-old LNG-IUS user)
A minority of participants described a positive initial reaction. These tended to be adolescents who previously had negative experiences with other methods of birth control.
3. Information gathering
During the information-gathering phase, participants gathered information about IUC from three main sources: their social network (particularly friends and family), the Internet, and medical providers.
• Friends and family
Participants gathered information about IUC from current users, past users, and non-users of the method within their social network. Negative opinions of and experiences with IUC were commonly expressed, which discouraged some participants from using the method. For example, friends of participant 8 (22-year-old LNG-IUS user) told her “you’ll have a period forever.” Participant 9 (24-year-old former LNG-IUS user) said: “I’d heard of people’s [IUC] falling out or tearing their uteruses and that kind of just freaked me out.”
Conversely, several participants heard positive reviews of IUC, with some even being encouraged to use the method. Participant 10 (18-year-old former LNG-IUS user) said: “There wasn’t too much information on it. But the more I spoke to people, the more I saw that they were really happy with it.”
• Internet
Participants used the Internet to gather user reviews of the method and to verify what they had learned from other sources. Participant 17 (24-year-old Copper-T user) stated: “It was reassuring that everything I found on the Internet went with what the doctor and the [informational] pamphlet had said.”
• Medical providers Providers were cited as valuable resources for answering questions and addressing concerns about IUC. Many of these concerns arose following conversations with friends and family and some were based on misconceptions about the method. Participant 19 (24-year-old Copper-T user) named her healthcare provider as the “loudest voice of reason” among her information sources, while participant 11 (21-year-old LNG-IUS user) stated that her provider was an important influence because she was “really informed and knew about all the different types of birth control.”
In learning about IUC from their provider, study participants appreciated the use of visual materials and anatomical models, information on side effects, and reassurance that IUC discontinuation was an option. Counseling that was specifically tailored to each adolescent’s expressed preferences regarding method characteristics was also highly valued. See Table 2 for direct quotations regarding these aspects of counseling.
Table 2.
Helpful provider interactions in the information-gathering phase
| Interactions | Quote |
|---|---|
| Tailored counseling | “There was actually somebody listening to the things that I didn’t want and the things that I did want instead of just giving me a list of, you know, ‘generally this happens, generally this doesn’t.’ I didn’t wanna look at a spreadsheet of effectiveness… I needed to have like a dialogue and have it be more than just little facts.” Participant 9 (24-year-old former LNG-IUS user) |
| “I was talking to my clinician and I was just repeating my rant of ‘I hate hormones and they’re not for me.’ And she was just like, ‘well, you could try the [Copper- T]…Then my clinician explained it realistically and told me that my cramps might get worse…She knew I was concerned about that.” Participant 19 (24-year-old Copper-T user) |
|
| Used visuals and models | “Not every young person knows this is your vagina, this is what’s inside and this is how it is. They might be like ‘ok, yeah yeah’ and then they might be like, ‘what was she talking about?’ Being able to actually show a picture, I think that’s really helpful. Because whether or not you know the names of each part, you can’t go wrong with seeing it.” Participant 2 (19-year-old Copper-T user) |
| “I found out how small [IUC] was. That helped. Because I was wondering like, how does it stay there? How is it going to not get me pregnant? How is it going to stay there all the years? Like if I have sex, it’s not going to move? But they reassured me…and seeing it made it better.” Participant 16 (24-year-old LNG-IUS user) |
|
|
Gave information on a wide
range of side effects |
“I liked that [my provider] told me that I was gonna have more cramps and that my periods were gonna be heavier. So I knew what I was getting into.” Participant 1 (18- year-old Copper-T user) |
| “They tell you when you get [IUC] that sometimes your period may vary and sometimes you might not get your period at all. I went a few months before getting my period when I first got [IUC]. I was kind of scared at first, but I remembered that [my provider] explained this to me.” Participant 6 (22-year-old LNG-IUS user) |
|
|
Answered questions and
addressed concerns |
“I wanted to know everything. I was like, ‘Okay, so where’s that going to go, and for how long? And is it going to be okay?’ I was asking so many questions. [My provider] actually took the time to sit there and explain everything to me, like the side effects from it, the placement, and what he needed to do to implant it.” Participant 17 (24-year-old Copper-T user) |
| “My mom was on [IUC]…but she said she took it off because somebody told her that it was, like, a little machine…that made you have abortions or something…I heard that from her so that’s why I was kind of skeptical, you know? But [my provider] told me that it didn’t make you have abortions; it was just like any other birth control. So, I decided to get it.” Participant 5 (21-year-old former LNG-IUS user) |
|
|
Assured that discontinuation
was an option |
“It actually did [help to be told I could take IUC out]….You think, ‘well what if this is stuck in me forever? What if at a point I do want a child and I can’t get it out’? But [my provider] assured me that it would be able to be taken out when ready.” Participant 14 (16 year- old LNG-IUS user) |
| “If I did want to have children later on down the road, I liked the idea that it was pretty much freely my choice on when I could take it out. I really, really liked that.” Participant 13 (19-year-old LNG-IUS user) |
While providers were consistently valued for the informational role they played, some participants also found it helpful when their medical provider took on what they perceived as an almost friend-like role: “I’m comfortable with my doctor. I have this relationship with her and trust her not only as a doctor but, well, as a friend” (Participant 9; 24-year-old former LNG-IUS user). Some providers even self-disclosed that they used IUC themselves, which study participants cited as appropriate and comforting:
[Provider self-disclosure] actually made me feel better. To know that a person in the room also had what I was attempting to get made me feel more comfortable. Participant 14 (16-year-old LNG-IUS user)
On a related note, several participants wished that their provider had given them more subjective input about whether they should use IUC:
[I asked my provider], “could you please give your honest opinion about what to do? That doesn’t mean I’m gonna do it, but I will take it into consideration….Like, if you were my friend, what would you say?” Participant 2 (19-year-old Copper-T user)
Notably, the desire for subjective input from the medical provider was not expressed in every interview. Instead, participants voiced a wide range of preferences. For example, participant 18 (24-year-old LNG-IUS user) stated: “I want seriously unbiased, straight up information from my provider without opinions.”
4. Adoption
Participants decided to adopt IUC after integrating their personal preferences with the information they gathered from their social network, the Internet, and their medical provider. A strong preference to prevent pregnancy was a prominent theme in all of the interviews, with most participants seeing pregnancy as an obstacle to their future plans. Other preferences included a strong desire to avoid higher-dose hormonal methods and a preference for convenient and long-acting contraception.
In making the decision to adopt IUC, many participants overcame concerns about the method that had arisen during the information-gathering phase. This was facilitated by two factors:
• “The tipping point”
Many participants experienced a profound event—referred to by participant 19 (24-year-old Copper-T user) as the “tipping point”—which strengthened or changed their existing personal contraceptive preferences. This experience, such as a pregnancy scare or abortion, allowed them to overcome their concerns about IUC:
When I missed pills…I would kind of be scared and think ‘oh my god, I could get pregnant.’ You keep on stressing about it…. So, I figured [that] having [IUC] is better even though it seemed sort of scary at first. Participant 1 (18 year-old Copper-T user)
For others, personal preferences were modified after moving to a new location where access to or quality of family planning care was uncertain:
I’m going to college so I needed something more permanent...I don’t know how the clinics or healthcare system work there and I won’t know ‘til I get out there. Participant 8 (22-year-old LNG-IUS user)
• “Everyone is different”
The realization that contraception is “different for different people” (Participant 6; 22-year-old LNG-IUS user) was also key to helping participants overcome their concerns. Participants adopted IUC when they were able to conceptualize their own potential experiences with the method as distinct from the negative experiences that they had heard about in the information-gathering phase:
I know that every birth control method is not gonna be the same for every girl. That’s why there’s so many different types. You have to pick your own. I know my body is different…from a lot of my friends….So, I wanted to have my own experience, you know? Participant 12 (17-year-old Copper T-user)
5. Adjustment and Reassessment
Following IUC insertion, participants experienced IUC side effects and evaluated whether they would like to continue using the method. This period was influenced by motivation to use IUC, level of preparation for method use, and amount of external support received by the adolescent.
• Motivation
While the majority of participants experienced side effects, most were motivated to continue using IUC. This was partly due to a strong intention to prevent pregnancy and/or previous experience with other types of contraception. Copper-T users, in particular, expressed considerable motivation to continue using IUC due to dissatisfaction with previously used hormonal methods.
• Preparation
Participants stated that being prepared for potential side effects by their medical provider helped them to navigate the adjustment phase. Participant 18 (24-year-old LNG-IUS user) stated: “When I got [IUC], it took a month or two before my bleeding stopped. [My provider said] it takes a while, though… So, it was okay.” Friends with IUC experience were also a valuable resource: “[My friend] prepared me. And I guess if I hadn’t talked to her about it, I would’ve been freaking out right now” (Participant 12; 17-year-old Copper-T user).
• Support
Study participants appreciated receiving support from members of their social network during the adjustment and reassessment phase. For example, participant 4 (24-year-old LNG-IUS user) stated: “Between my friends who have it, we just encourage each other. We’re just like, ‘you’re doing great’” The Internet was also used as a source of reassurance. Participant 7 (18-year-old LNG-IUS user) said: “I googled it and some people had the same side effects. So, I wasn’t really tripping about it.”
Medical providers and clinic staff also played a supportive role. Participant 15 (21-year-old LNG-IUS user) explained: “If I have any question or concern, the clinic’s awesome. I just call them and…they answer my questions.” Participant 5 (21-year-old former LNG-IUS user) said: “At times I was scared ‘cause I’d heard it could fall out…I came [to the clinic] and they told me how to check for [IUC] and taught me more about it.”
Four participants in the study discontinued IUC due to concerns about side effects. These adolescents valued having their concerns validated by their medical provider:
I was like, “I think this [IUC] might be making me overly emotional and sensitive.” And the doctor said, “if you want, you can try and keep track of how you’re feeling to see…if it correlates to situations in your life or if you think it’s just [IUC].” I thought this was really nice. She wasn’t like “nope, not possible.” She said, “let’s try and pay attention to this and we’ll figure out if it’s [IUC] or if you think it’s something else.” Participant 9 (24-year-old former LNG-IUS user)
Two of the four participants who chose to remove IUC stated that their provider discouraged removal. These participants expressed a feeling of loss of control over the process and became disengaged in discussions with their medical provider. This was described by participant 10 (18-year-old former LNG-IUS user): “I just felt like [IUC removal] wasn’t my decision, it was more [my provider’s].”
Counseling Recommendations
Participants emphasized the importance of receiving comprehensive information during counseling, as well as reassurance regarding removal. Participant 16 (24 year-old LNG-IUS user) stated: “Providers should say, ‘you can take it out when you want to. It’s not permanent.’ They should also talk about side effects.” Participant 12 (17-year-old Copper-T user) recommended “providers use models to show where they place IUC…and give web [addresses] where you can get more information.” An expanded list of recommendations—based on both participant suggestions as well as those inferred from the process model—is included in the Discussion.
DISCUSSION
Through the use of qualitative methodology, participants in this study described their IUC adoption process and identified the role of the medical provider in this trajectory. While similar studies have developed models to describe adolescent adoption of the transdermal patch and vaginal ring (19, 23), none have focused specifically on IUC use or nulliparous adolescents. Our findings, therefore, add to the literature and can inform future efforts to support the use of an underutilized method that has the potential to address unintended pregnancy among young people.
Results from this study suggest that providers play prominent roles in the first awareness, information-gathering, and adjustment and reassessment phases of the IUC adoption process. The clinical implications for each of these stages are discussed below.
• First Awareness
Unlike past studies, which have identified the media as pivotal to spreading awareness of newly introduced contraceptive methods (19), participants in this study described a lack of IUC promotion in the media. This increases the onus on medical providers to introduce IUC relative to other methods that may be more heavily advertised. Given that some participants experienced a pregnancy scare, providers could also consider introducing Copper-T as a form of emergency contraception (14).
Although medical providers played a prominent role in spreading awareness of IUC, many study participants described a delay in introduction to the method. This may be related to providers’ misconceptions about the appropriateness of IUC for adolescents (10-12) and underscores the importance of educating providers about the method. This is particularly relevant because research shows that adolescents who hear about IUC from their medical provider are more likely to show interest in the method compared to those who first hear about it from other sources (7).
• Information Gathering
While conventional teaching holds that the medical provider should only offer information and not personal opinions regarding contraceptive selection (24), our results suggest that this philosophy may actually be a disservice to some adolescents, as many of them are still developing their decision-making skills and may benefit from more provider involvement in their adoption process (25). Results from this study and others (26) suggest that degree of provider input should vary based on each individual’s counseling preferences, with some desiring that their providers play a more active role in their decision-making process than others. Patient-centered counseling strategies, such as motivational interviewing, may offer a framework for medical providers to take on an active role with appropriate patients (27).
A related finding concerns provider self-disclosure of IUC use. There is a paucity of research on this topic in the family planning literature. Studies in other settings have yielded conflicting results regarding the utility of this type of information exchange (28, 29). A qualitative investigation of 100 primary care physicians found that self-disclosure was not useful to adult patients and, in some cases, disruptive (29). Conversely, Beach et al. (2004) found that physician self-disclosure was associated with increased patient satisfaction in surgical settings (28).
The fact that some adolescents in this study found self-disclosure appropriate and comforting may be partially explained by the perceived “friend-like” relationship that they had with their provider. Because younger participants (19 years of age and younger) primarily cited self-disclosure as helpful, developmental stage may also play a role in an adolescent’s perception of the usefulness of this interaction (30). More research is needed in this area, with attention to the likelihood that preferences may vary depending on the individual being counseled, the method being considered, and the relationship between the patient and provider.
Many study participants expressed concerns about IUC prior to insertion. These concerns typically arose after participants learned about negative experiences with and opinions of the method from within their social network. Previous qualitative research shows that adolescents, particularly those from non-white populations, rely heavily on their social networks when making decisions about contraceptive use and that some of this information is based on misconceptions (31, 32). Therefore, providers may better assist adolescent patients in making informed decisions regarding IUC use by directly inquiring about and addressing information received from social contacts in a respectful manner.
Finally, medical providers should be aware that, unlike the Copper-T, the prescribing information on the LNG-IUS manufacturer’s website has not been amended to include nulliparous women as acceptable candidates (33). This should be explained to nulliparous IUC candidates, as many study participants used the Internet to confirm the information they received from their provider.
• Adjustment and Reassessment
Study participants stated that being prepared for IUC and receiving external support facilitated their adjustment to IUC side effects. Though the actual impact of these influences cannot be conclusively demonstrated, past research has found that users of long-acting contraceptives who received comprehensive information on side effects were more satisfied with (34) and more likely to continue using these methods (35).
For four participants in the study, side effects became unacceptable, leading to removal of the device. Side effects are a commonly cited reason for IUC discontinuation (36, 37). While participants appreciated their providers’ validation of potential side effects, some felt that their autonomy was infringed upon when their medical provider resisted removal. Given that IUC is a provider-controlled method, it is important that nulliparous adolescent IUC users feel that removal of the device remains their decision.
Suggestions for IUC counseling appear in Table 3. An important qualification to implementing these recommendations is that IUC may not be the desired or appropriate contraceptive method for every nulliparous adolescent, even after counseling. This is a particularly relevant consideration when working with non-white populations. Up until the 1970’s, members of these groups were the target of coercive public health policies aimed at controlling population growth in the United States (38), which may be related to distrust of family planning programs among these populations (39).
Table 3.
Counseling suggestions, based on study results*
| BEFORE INSERTION |
| 1. Spread awareness of IUC |
| -Introduce IUC to nulliparous adolescent candidates during contraception counseling |
| -Educate about and offer Copper-T as a form of emergency contraception |
| -Stay up to date on current IUC medical eligibility criteria |
| 2. Prioritize individual needs |
| -Identify personal preferences for contraception and tailor counseling according to these preferences |
| -Discuss non-contraceptive benefits of IUC, such as lighter menstrual flow with the LNG-IUS |
| 3. Provide comprehensive information |
| -Give wide range of information on possible side effects |
| -Use visuals and models to explain where IUC is placed and how it works |
| -Consider offering personal experiences with IUC, when appropriate, or subjective advice when requested |
| -Develop a list of reputable Internet sites that adolescent can refer to throughout the adoption process |
| -After counseling, encourage adolescent to discuss IUC with members of her social network who have had positive experiences with the method |
| 4. Address and discuss concerns |
| -Remember that an adolescent may still use and be satisfied with IUC even if she has a negative initial reaction to the method |
| -Discuss the role of the social network in perpetuating concerns about IUC and dispel misconceptions that the adolescent may have about the method |
| -Remind adolescent that “everyone is different” and that the negative experiences of friends may not reflect her own experience |
| -Reassure adolescent that IUC discontinuation is an option |
| 5. Prepare adolescent for adjustment and reassessment phase |
| -Discuss sources of support in case of concerns |
| -Explain that clinic is available to answer questions after insertion |
| -Discuss motivation for using IUC and non-contraceptive benefits of the method |
| AFTER INSERTION |
| 1. Provide support |
| -Be available by text, email or phone to answer questions about side effects |
| -Validate and discuss concerns that may arise |
| -Remove IUC if requested by adolescent |
Given the limited amount of time available in a contraceptive counseling visit, it may be necessary to involve other clinic staff in the implementation of these recommendations
This study has several limitations. First, due to our focus on English-speaking, non-white urban adolescents, our results may not be generalizable to other populations. Only half of those who were recruited were ultimately interviewed, therefore, study participants may not have provided an inclusive representation of IUC experiences. Most of our sample was older than 17, which limits the generalizability of this study to younger adolescents. Second, because only IUC adopters were recruited, nothing can definitively be said about the counseling needs of non-users. Though we offer counseling suggestions, the specific experiences and preferences of non-users are not represented and may be different from those of the IUC users interviewed. Third, given that we recruited participants from a single youth-focused clinic, it is possible that the same medical provider(s) counseled multiple study participants. However, we believe that the degree of overlap is minimal, as participants described counseling experiences in multiple clinics throughout the California Bay Area. Finally, the counseling suggestions in this study are based on participants’ recommendations and/or have been inferred from the process model. Further studies are needed to confirm the actual impact of these suggestions on IUC use.
Our findings suggest that medical providers can influence a nulliparous adolescent’s IUC adoption process. Given the lack of understanding about the IUC (40), providers are ideally positioned to increase awareness and knowledge of the method. The role of provider self-disclosure and subjective input regarding IUC use warrants future investigation and suggests that the degree of provider participation into the decision-making process should be based on an individual’s preference rather than a standardized counseling practice. Medical providers should be aware, however, of the need for caution in encouraging IUC adoption and continuation, ensuring that the autonomy of the adolescent is not overshadowed by the clinical and public health implications of its use.
ACKNOWLEDGEMENTS
This project was supported by NIH/NCRR/OD UCSF-CTSI Grant Number KL2 RR024130. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. This project was also supported by the Association of Reproductive Health Professionals (ARHP) Gary Stewart Scholarship in Public Health, the Joint Medical Program Health & Medical Sciences Thesis Research Fellowship, and the UCSF School of Medicine Dean’s Research Fellowship.
A poster presentation of this research was given at the 2011 ARHP Annual Conference and was also given at the 2012 Society of Adolescent Health and Medicine Annual Conference. Abstracts associated with these poster presentations were published in special edition versions of Contraception and Journal of Adolescent Health, respectively.
We would like to extend our gratitude to Dr. Jody Steinauer and Dr. Tina Raine-Bennett for their support.
ABBREVIATIONS
- IUC
Intrauterine Contraception
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
There are no conflicts of interest for any of the authors.
REFERENCES
- 1.Chandra A, Martinez GM, Mosher WD, et al. Fertility, family planning, and reproductive health of US women: data from the 2002 National Survey of Family Growth. Vital Health Stat 23. 2005;(25):1–160. [PubMed] [Google Scholar]
- 2.Logan C, Holcombe E, Manlove J, et al. Child Trends. Inc and National Campaign to Prevent Teen Pregnancy; Washington, DC: 2007. The consequences of unintended childbearing. [Google Scholar]
- 3.Kost K, Singh S, Vaughan B, et al. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77(1):10–21. doi: 10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yen S, Saah T, Adams Hillard P. IUDs and Adolescents--An Under-Utilized Opportunity for Pregnancy Prevention. J Pediatr Adolesc Gynecol. 2009;23(3):123–8. doi: 10.1016/j.jpag.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Mosher WD, Jones J. Use of contraception in the United States: 1982-2008. Vital Health Stat 23. 2010;23(29):1–44. [PubMed] [Google Scholar]
- 6.Hubacher D, Lara-Ricalde R, Taylor D, et al. Use of copper intrauterine devices and the risk of tubal infertility among nulligravid women. N Engl J Med. 2001;345(8):561–7. doi: 10.1056/NEJMoa010438. [DOI] [PubMed] [Google Scholar]
- 7.Fleming K, Sokoloff A, Raine T. Attitudes and beliefs about the intrauterine device among teenagers and young women. Contraception. 2010;82(2):178–82. doi: 10.1016/j.contraception.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitaker A, Johnson L, Harwood B, et al. Adolescent and young adult women’s knowledge of and attitudes toward the intrauterine device. Contraception. 2008;78(3):211–7. doi: 10.1016/j.contraception.2008.04.119. [DOI] [PubMed] [Google Scholar]
- 9.Dehlendorf C, Levy K, Ruskin R, et al. Health care providers’ knowledge about contraceptive evidence: a barrier to quality family planning care? Contraception. 2010;81(4):292–8. doi: 10.1016/j.contraception.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dehlendorf C, Ruskin R, Darney P, et al. The effect of patient gynecologic history on clinician contraceptive counseling. Contraception. 2010;82(3):281–5. doi: 10.1016/j.contraception.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harper C, Blum M, de Bocanegra H, et al. Challenges in translating evidence to practice: the provision of intrauterine contraception. Obstet Gynecol. 2008;111(6):1359–69. doi: 10.1097/AOG.0b013e318173fd83. [DOI] [PubMed] [Google Scholar]
- 12.Stanwood N, Garrett J, Konrad T. Obstetrician-gynecologists and the intrauterine device: a survey of attitudes and practice. Obstet Gynecol. 2002;99(2):275–80. doi: 10.1016/s0029-7844(01)01726-4. [DOI] [PubMed] [Google Scholar]
- 13.Reproductive Health and Research. 4th Edition World Health Organization; 2009. Medical Eligibility Criteria for Contraceptive Use. [Google Scholar]
- 14.Long-acting reversible contraception: Implants and intrauterine devices: ACOG Practice Bulletin No. 121. Obstet Gynecol. 2011;118(1):184–196. doi: 10.1097/AOG.0b013e318227f05e. [DOI] [PubMed] [Google Scholar]
- 15.Lyus R, Lohr P, Prager S. Use of the Mirena LNG-IUS and Paragard CuT380A intrauterine devices in nulliparous women. Contraception. 2010;81(5):367–71. doi: 10.1016/j.contraception.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 16.Gold M, Johnson L. Intrauterine devices and adolescents. Curr Opin Obstet Gynecol. 2008;20(5):464–9. doi: 10.1097/GCO.0b013e32830a98f8. [DOI] [PubMed] [Google Scholar]
- 17.Hulton L. Adolescent Sexual Decision-Making; An Integrative Review. The Online Journal of Knowledge Synthesis for Nursing. 2001;8(1):48–60. [PubMed] [Google Scholar]
- 18.Rich M, Ginsburg KR. The reason and rhyme of qualitative research: Why, when, and how to use qualitative methods in the study of adolescent health. J Adolesc Health. 1999;25(6):371–8. doi: 10.1016/s1054-139x(99)00068-3. [DOI] [PubMed] [Google Scholar]
- 19.Sucato GS, Bhatt SK, Murray PJ, et al. Transdermal Contraception as a Model for Adolescent Use of New Methods. J Adolesc Health. 2011;49(2):357–62. doi: 10.1016/j.jadohealth.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 20.Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. Sage Publications; Thousand Oaks, California: 2006. [Google Scholar]
- 21.Rogers E. Diffusion of Innovations. 4th ed. The Free Press; New York: 1995. New York. [Google Scholar]
- 22.Miles MB, Huberman AM. Qualitative data analysis. Sage Publications; Thousand Oaks, California: 1994. [Google Scholar]
- 23.Epstein L, Sokal-Gutierrez K, Ivey S, et al. Adolescent experiences with the vaginal ring. J Adolesc Health. 2008;43(1):64–70. doi: 10.1016/j.jadohealth.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moskowitz E, Jennings B. Directive counseling on long-acting contraception. Am J Public Health. 1996;86:787–90. doi: 10.2105/ajph.86.6.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fonseca H, Greydanus DE. Sexuality in the child, teen, and young adult: Concepts for the clinician. Prime Care. 2007;34:275–92. doi: 10.1016/j.pop.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 26.Dehlendorf C, Diedrich J, Drey E, et al. Preferences for decision-making about contraception and general health care among reproductive age women at an abortion clinic. Patient Educ Couns. 2010;81(3):343–8. doi: 10.1016/j.pec.2010.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Petersen RPP, Albright J, Holland H, Cabral R, Curtis K. Applying motivational interviewing to contraceptive counseling: ESP for clinicians. Contraception. 2004;69(3):213–7. doi: 10.1016/j.contraception.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 28.Beach MC, Roter D, Rubin H, et al. Is Physician Self disclosure Related to Patient Evaluation of Office Visits? J Gen Intern Med. 2004;19(9):905–10. doi: 10.1111/j.1525-1497.2004.40040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McDaniel SH, Beckman HB, Morse DS, et al. Physician Self-disclosure in Primary Care Visits: Enough About You, What About Me? Arch Intern Med. 2007;167(12):1321–26. doi: 10.1001/archinte.167.12.1321. [DOI] [PubMed] [Google Scholar]
- 30.Papouchis N. Chapter: Self-disclosure and psychotherapy with children and adolescents. In: Stricker GFM, editor. Self-disclosure in the therapeutic relationship. Plenum Press; New York: 1990. pp. 157–74. [Google Scholar]
- 31.Gilliam M, Warden M, Goldstein C, et al. Concerns about contraceptive side effects among young Latinas: A focus-group approach. Contraception. 2004;70(4):299–305. doi: 10.1016/j.contraception.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 32.Yee L, Simon M. The Role of the Social Network in Contraceptive Decision-making among Young, African American and Latina Women. J Adolesc Health. 2010;47(4):374–80. doi: 10.1016/j.jadohealth.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. [Accessed online on September 22, 2011];Mirena: Highlights of Prescribing Information. Available at: http://berlex.bayerhealthcare.com/html/products/pi/Mirena_PI.pdf.
- 34.Backman T, Huhtala S, Luoto R, et al. Advance Information Improves User Satisfaction With the Levonorgestrel Intrauterine System. Obstet Gynecol. 2002;99(4):608–13. doi: 10.1016/s0029-7844(01)01764-1. [DOI] [PubMed] [Google Scholar]
- 35.Canto De Cetina TE, Canto P, Ordo ez Luna M. Effect of counseling to improve compliance in Mexican women receiving depot-medroxyprogesterone acetate. Contraception. 2001;63(3):143–6. doi: 10.1016/s0010-7824(01)00181-0. [DOI] [PubMed] [Google Scholar]
- 36.Alnakash A. Influence of IUD perceptions on method discontinuation. Contraception. 2008;78(4):290–3. doi: 10.1016/j.contraception.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 37.Toma A, Jamieson M. Revisiting the intrauterine contraceptive device in adolescents. J Pediatr Adolesc Gynecol. 2006;19(4):291–6. doi: 10.1016/j.jpag.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 38.Stern AM. Sterilized in the name of public health: race, immigration, and reproductive control in modern California. Am J Public Health. 2005;95(7):1128–38. doi: 10.2105/AJPH.2004.041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thorburn S, Bogart LM. Conspiracy Beliefs About Birth Control: Barriers to Pregnancy Prevention Among African Americans of Reproductive Age. Health Educ Behav. 2005;32(4):474–87. doi: 10.1177/1090198105276220. [DOI] [PubMed] [Google Scholar]
- 40.Stanwood N, Bradley K. Young Pregnant Women’s Knowledge of Modern Intrauterine Devices. Obstet Gynecol. 2006;108(6):1417–22. doi: 10.1097/01.AOG.0000245447.56585.a0. [DOI] [PubMed] [Google Scholar]